Abstract
Psychiatric disorders and substance abuse are barriers that limit access to timely treatment and can lead to Potentially Preventable Hospitalizations (PPH). The aim of this study is to identify the role played by gender in the association between mental health and PPH. Hospital discharge records (HDRs) from the Local Health Authority of Pescara (Italy) from 2015 to 2021 were examined and PPH were measured according to Prevention Quality Indicators (PQIs) provided by the Agency for Healthcare Research and Quality. In total, 119,730 HDRs were eligible for the study and 21,217 patients fell into the PQI categories. Mental health disorders and addictions were extracted from the HDRs through the Elixhauser Enhanced ICD-9-CM algorithm. The association between PQI hospitalization and some predictors considered was evaluated with multivariate logistic regression models. In males and females, alcohol abuse showed a protective role towards preventable admissions for PQI-90 (all types of conditions) and PQI-92 (chronic conditions). In contrast, there is a gender gap in accessibility to primary health care, especially for acute conditions leading to PPH. Indeed, in males, PQI-91 admissions for acute conditions were found to be positively associated with drug abuse, psychosis, and depression, whereas this was not the case for females.
Keywords: mental health, substance abuse, alcohol abuse, barriers, gender inequalities, preventable hospitalizations, public health
1. Introduction
Potentially Preventable Hospitalizations (PPH) for physical health conditions are used as a measure of health service access, integration, and effectiveness. PPH are specific hospital admissions that could potentially have been avoided through preventative health interventions and community care: long term studies found PPH elevated in patients with mental health conditions [1].
Barriers to primary care access lead to PPH. These barriers can be driven by psychological factors that can make it difficult for patients to prioritize their own health; in addition, primary care providers’ stigma on mental health and substance use can have an impact on the extent to which patients communicate their needs [2]. Analyzing PPH can indirectly help to define the determinants of the barriers to primary care access.
Gender roles can have an impact on generating differences in prevalence rates and determinants of mental health indicators between women and men [3]. In fact, the gender gap in mental health service use is caused not only by men’s negative attitudes toward help seeking, but also by structured social norms associated with masculinity [4]. For example, men are more likely to report barriers to care related to their perceptions of mental health issues and usefulness of health care services and are less likely to acknowledge the helpfulness of psychotherapy [4,5].
Using appropriate, inclusive, interprofessional models for mental health care is fundamental to enhance the delivery of mental health care in primary care settings and improve health outcomes for people with mental disorders [6,7,8]. In order to choose the proper model, to evaluate its efficacy and accessibility for psychiatric patients, local data inflow such as hospital discharge records can become an asset. Hospital discharge records (HDRs) allow estimates of the cost of hospitalizations that can be an indicator of the efficiency of primary health care: it can be used to identify PPH and orient programmatic decisions, both in hospital and primary care settings [9,10]. Prevention Quality Indicators (PQIs) created by the Agency for Healthcare Research and Quality (AHRQ) use data from HDRs to identify hospitalizations that could be preventable with access to quality primary health care and identify barriers to primary care access. PQIs result as a key tool to evaluate community health needs and primary health care services [11].
Current research on PPH still lacks focus on gender aspects, especially the one regarding mental health. The aim of the study is to identify gender disparities in the association between PPH and patients’ mental health state.
2. Materials and Methods
We carried out a retrospective observational study by analyzing the admissions that occurred in the Local Health Authority (LHA) of Pescara, the most populated city in Abruzzo, a region of Southern Italy. The LHA of Pescara serves a catchment area of about 320,000 inhabitants and is organized with a large hub hospital and two spoke hospitals [12]. Data were collected from hospital discharge records (HDRs) of all hospital admissions that occurred from 1 January 2015 to 31 December 2021. All the patients living in the LHA of Pescara were selected. The HDRs collected information on admission source and type, admission and discharge dates, patient baseline demographics (age, gender, citizenship, birthplace, and residence), the principal diagnosis and up to five additional diagnoses, the main procedure and up to five further procedures performed during the admission. Diagnoses and procedures were coded according to the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM, National Center for Health Statistics (NCHS), and the Centers for Medicare and Medicaid Services External, Atlanta, GE, USA). To compute the preventable admission rate, AHRQ definitions [13] were followed, including four different Prevention Quality Indicators: Prevention Quality Overall Composite (PQI-90), Prevention Quality Acute Composite (PQI-91), Prevention Quality Chronic Composite (PQI-92), Prevention Quality Diabetes Composite (PQI-93). Appendix A provides details on the definition, use, and composition of PQI Composite Measures (Table A1). Physical comorbidities and those specifically affecting mental health (depression and psychosis) and addictions (alcohol and drugs) were extracted from HDRs through the Elixhauser enhanced ICD-9-CM algorithm proposed by Quan et al. [14].
Statistical Analysis
Categorical variables were reported as frequency and percentage. Pearson’s Chi-square test was performed to compare baseline variables between gender for each of the PQIs examined. To evaluate the statistical association between PQI hospitalization and the various predictors taken into consideration, multivariate logistic regression models were implemented, one for the whole sample and one for the male and female sample. Statistical significance was set at p-value < 0.05. All analyses were performed with Stata® version 15 (StataCorp LLC, College Station, TX, USA).
3. Results
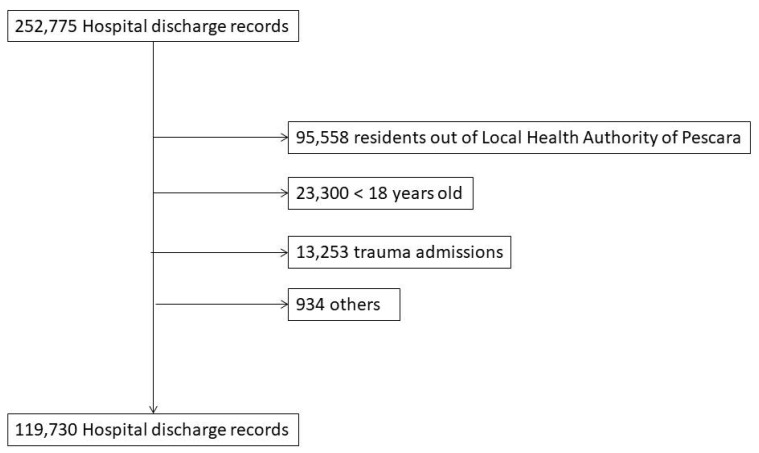
As showed in Figure 1, of the 252,755 hospital discharge records produced by the three hospitals in the Pescara LHA, 95,558 are excluded because residents out of the Pescara LHA. In total, 23,300 HDRs belonging to patients under the age of 18 and 13,253 HDRs related to trauma are excluded. Finally, 934 HDRs are excluded for other reasons such as coding errors. In total, 119,730 are eligible for our study and 21,217 patients fall into the PQIs categories.
Figure 1.
Flow chart of included HDRs.
The characteristics of the sample are summarized in Table 1. About the study population, 47.07% of included patients were males. The majority of patients are between 61 and 80 years of age (36.82%), followed by patients aged over 80 (22.26%), 41–60 (21.67%), and 18–40 (19.25%). In total, 50.27% of patients have one or more comorbidities.
Table 1.
Sex, age category, and physical comorbidities of the population under study and of the subjects considered in PQIs.
| N (%) | Total Population | PQI-90 Overall |
PQI-91 Acute |
PQI-92 Chronic | PQI-93 Diabetes |
|---|---|---|---|---|---|
| 119,730 | 9902 | 2429 | 7492 | 1394 | |
| Sex | |||||
| Males | 56,362 (47.07) | 5313 (53.66) | 1277 (52.57) | 4047 (54.02) | 910 (65.28) |
| Age category | |||||
| 18–40 | 23,045 (19.25) | 304 (3.07) | 220 (9.06) | 84 (1.12) | 19 (1.36) |
| 41–60 | 25,945 (21.67) | 1106 (11.17) | 412 (16.96) | 696 (9.29) | 170 (12.20) |
| 61–80 | 44,089 (36.82) | 4234 (42.76) | 917 (37.75) | 3330 (44.45) | 841 (60.33) |
| Over80 | 26,651 (22.26) | 4258 (43.00) | 880 (36.23) | 3382 (45.14) | 364 (26.11) |
| Physical comorbidities (Num) | |||||
| 0 | 59,545 (49.73) | 993 (10.03) | 857 (35.28) | 137 (1.83) | 6 (0.43) |
| 1 | 28,533 (23.83) | 2152 (21.73) | 725 (29.85) | 1430 (19.09) | 218 (15.64) |
| 2 | 19,594 (16.37) | 2977 (30.06) | 586 (24.13) | 2401 (32.05) | 482 (34.58) |
| 3+ | 12,058 (10.07) | 3780 (38.17) | 261 (10.75) | 3524 (47.04) | 688 (49.35) |
3+: more than three comorbidities.
In the overall sample, patients who have psychiatric or addiction problems under study are 3979 (3.32%). Of these, 2557 have at least one psychiatric diagnosis (2.14%), 1387 have at least one addiction diagnosis (1.16%), and 142 have both diagnoses (0.12%).
The hospital discharge records that fall into the PQIs categories are 21,217, of which 11,547 are about men (54.42%) and 9670 are about women (45.58%). Age of the population by gender and PQI are shown in Table 2. The majority of patients are between 61 and 80 years of age (9322, 43.94%), followed by the categories of over 80 (8884, 41.87%), 41–60 (2384, 11.24%), and 18–40 (627, 2.95%) years old. There are statistically significant differences between males and females by age: considering the PQI-90 overall and the PQI-91 acute hospitalizations, females are predominant in the 18–40 and over 80 age groups, while they are less represented in the 41–60 and 61–80 age groups. Females are always underrepresented in the PQI-93 diabetes hospitalization and overrepresented only in the over 80 age group considering the PQI-92 chronic hospitalization.
Table 2.
Age of the population by gender and by PQI.
| PQI-90 Overall | PQI-91 Acute | PQI-92 Chronic | PQI-93 Diabetes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Males | Females | p Value | Males | Females | p Value | Males | Females | p Value | Males | Females | p Value | |
| Total | 5313 | 4589 | 1277 | 1152 | 4047 | 3445 | 910 | 484 | ||||
| Age | ||||||||||||
| 18–40 | 135 (2.54) | 169 (3.68) | <0.001 | 79 (6.19) | 141 (12.24) | <0.001 | 56 (1.38) | 28 (0.81) | <0.001 | 11 (1.21) | 8 (1.65) | <0.001 ** |
| 41–60 | 737 (13.87) | 369 (8.04) | <0.001 | 238 (18.64) | 174 (15.10) | <0.001 | 501 (12.30) | 195 (5.66) | <0.001 | 130 (14.29) | 40 (8.26) | <0.001 ** |
| 61–80 | 2581 (48.58) | 1653 (36.02) | <0.001 | 537 (42.05) | 380 (32.99) | <0.001 | 2051 (50.68) | 1279 (37.13) | <0.001 | 570 (62.64) | 271 (55.99) | <0.001 ** |
| Over 80 | 1860 (35.01) | 2398 (52.26) | <0.001 | 423 (33.12) | 457 (39.67) | <0.001 | 1439 (35.56) | 1943 (56.40) | <0.001 | 199 (21.87) | 165 (34.09) | <0.001 ** |
The use of double asterisk (**) indicates that statistical significance was tested with Fisher’s exact test, since the sample size was small.
Characteristics (physical comorbidities and mental health/substance use conditions) of the population by gender and PQI are shown in Table 3. In total, 90.61% (19,224) hospital discharge records considered in PQIs concern patients with one or more comorbidities and most have three or more comorbidities (38.90%).
Table 3.
Characteristics (physical comorbidities and mental health/substance use conditions) of the population by gender and by PQI.
| PQI-90 Overall | PQI-91 Acute | PQI-92 Chronic | PQI-93 Diabetes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Males | Females | p Value | Males | Females | p Value | Males | Females | p Value | Males | Females | p Value | |
| Total | 5313 | 4589 | 1277 | 1152 | 4047 | 3445 | 910 | 484 | ||||
| Physical comorbidities (Num) | ||||||||||||
| 0 | 496 (9.34) | 497 (10.83) | 0.056 | 408 (31.95) | 449 (38.98) | 0003 | 89 (2.20) | 48 (1.39) | 0.040 | 5 (0.55) | 1 (0.21) | 0.030 ** |
| 1 | 1172 (22.06) | 980 (21.36) | 0.056 | 393 (30.78) | 332 (28.82) | 0003 | 782 (19.32) | 648 (18.81) | 0.040 | 127 (13.96) | 91 (18.80) | 0.030 ** |
| 2 | 1629 (30.66) | 1348 (29.37) | 0.056 | 327 (25.61) | 259 (22.48) | 0003 | 1306 (32.27) | 1095 (31.79) | 0.040 | 308 (33.85) | 174 (35.95) | 0.030 ** |
| 3+ | 2016 (37.94) | 1764 (38.44) | 0.056 | 149 (11.67) | 112 (9.72) | 0003 | 1870 (46.21) | 1654 (48.01) | 0.040 | 470 (51.65) | 218 (45.04) | 0.030 ** |
| Drug abuse | 23 (0.43) | 2 (0.04) | <0.001 ** | 18 (1.41) | 2 (0.17) | 0.001 ** | 5 (0.12) | 0 (0.00) | 0.046 ** | 3 (0.33) | 0 (0.00) | 0.206 ** |
| Alcohol Abuse | 45 (0.85) | 5 (0.11) | <0.001 ** | 17 (1.33) | 3 (0.26) | 0.003 ** | 29 (0.72) | 2 (0.06) | <0.001 ** | 7 (0.77) | 1 (0.21) | 0.275 ** |
| Depression | 40 (0.75) | 56 (1.22) | 0018 | 21 (1.64) | 17 (1.48) | 0738 | 29 (0.72) | 2 (0.06) | <0.001 ** | 2 (0.22) | 3 (0.62) | 0.349 |
| Psychosis | 34 (0.64) | 21 (0.46) | 0.223 | 22 (1.72) | 7 (0.61) | 0.014 ** | 12 (0.30) | 14 (0.41) | 0420 | 5 (0.55) | 4 (0.83) | 0.508 ** |
| At least one psychiatric diagnosis | 73 (1.37) | 77 (1.68) | 0.217 | 42 (3.29) | 24 (2.08) | 0080 | 31 (0.77) | 53 (1.54) | 0001 | 7 (0.77) | 7 (1.45) | 0.263 |
| At least one addiction diagnosis | 68 (1.28) | 7 (0.15) | <0.001 ** | 35 (2.74) | 5 (0.43) | <0.001 | 34 (0.84) | 2 (0.06) | <0.001 ** | 10 (1.10) | 1 (0.21) | 0.110 |
| Both diagnoses | 2 (0.04) | 0 (0.00) | 0.503 ** | 1 (0.08) | 0 (0.00) | 1.000 ** | 1 (0.02) | 0 (0.00) | 1.000 ** | 0 (0.00) | 0 (0.00) | - |
The use of double asterisk (**) indicates that statistical significance was tested with Fisher’s exact test, since the sample size was small; 3+: more than three comorbidities
Considering all the hospital discharge records that fall into the PQIs categories, 53 (0.25%) of them concern drug-using patients, 109 (0.51%) alcohol users, 170 depressed patients, and 119 (0.80%) subjects with psychosis, 314 (1.48%) concern at least one psychiatric diagnosis, 162 (0.76%) at least one addiction diagnosis, and 4 (0.02%) both diagnoses.
In males, depression and having at least one psychiatric diagnosis were risk factors for PQI-90 overall hospitalization (OR = 1.69, 95% CI: 1.19–2.38 and OR = 1.37, 95% CI: 1.05–1.76). Drug abuse, psychosis, depression, having at least one psychiatric diagnosis, and having at least one addiction diagnosis were risk factors for PQI-91 acute hospitalization (OR = 2.02, 95% CI: 1.23–3.28, OR = 1.59, 95% CI: 1.02–2.45, OR = 2.44, 95% CI: 1.56–3.81, OR = 2.13, 95% CI: 1.53–2.93, OR = 1.64, 95% CI: 1.15–2.32, respectively). Data analysis also shows a growing positive association between the age of the patients and the increase of comorbidities. All the results are shown in Table 4.
Table 4.
Logistic regression for PQI in males.
| PQI-90 Overall | PQI-91 Acute | PQI-92 Chronic | PQI-93 Diabetes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Odds Ratio (95%) | p Value | Odds Ratio (95%) | p Value | Odds Ratio (95%) | p Value | Odds Ratio (95%) | p Value | |||||
| Age | ||||||||||||
| 18–40 | Ref. | - | - | Ref. | - | - | Ref. | - | - | Ref. | - | - |
| 41–60 | 1.25 | (1.02–1.5) | 0.025 | 1.14 | (0.87–1.47) | 0.324 | 1.41 | (1.05–1.87) | 0.019 * | 1.50 | (0.8–2.8) | 0.203 |
| 61–80 | 1.46 | (1.21–1.75) | <0.001 * | 1.28 | (0.99–1.64) | 0.050 | 1.65 | (1.24–2.17) | <0.001 * | 1.74 | (0.94–3.18) | 0.076 |
| over 80 | 2.05 | (1.69–2.46) | <0.001 * | 2.15 | (1.65–2.77) | <0.001 * | 2.12 | (1.6–2.8) | <0.001 * | 1.01 | (0.54–1.87) | 0.971 |
| Physical comorbidities (Num) | ||||||||||||
| 0 | Ref. | - | - | Ref. | - | - | Ref. | - | - | Ref. | - | - |
| 1 | 3.54 | (3.17–3.95) | <0.001 * | 1.37 | (1.18–1.58) | <0.001 * | 12.91 | (10.33–16.11) | <0.001 * | 38.86 | (15.86–95.21) | <0.001 * |
| 2 | 7.45 | (6.69–8.28) | <0.001 * | 1.60 | (1.36–1.86) | <0.001 * | 32.15 | (25.83–40.01) | <0.001 * | 135.00 | (55.57–327.92) | <0.001 * |
| 3+ | 17.39 | (15.61–19.37) | <0.001 * | 1.10 | (0.9–1.34) | 0.326 | 87.39 | (70.24–108.71) | <0.001 * | 355.34 | (146.46–862.1) | <0.001 * |
| Alcohol abuse | 0.43 | (0.31–0.58) | <0.001 * | 1.05 | (0.64–1.7) | 0.853 | 0.33 | (0.22–0.48) | <0.001 * | 0.32 | (0.15–0.68) | 0.003 * |
| Drug abuse | 1.17 | (0.75–1.79) | 0.490 | 2.02 | (1.23–3.28) | 0.005 * | 0.42 | (0.17–1.02) | 0.056 | 1.22 | (0.38–3.9) | 0.734 |
| Psychoses | 1.08 | (0.75–1.54) | 0.686 | 1.59 | (1.02–2.45) | 0.038 * | 0.62 | (0.34–1.13) | 0.121 | 1.14 | (0.46–2.81) | 0.777 |
| Depression | 1.69 | (1.19–2.38) | 0.003 * | 2.44 | (1.56–3.81) | <0.001 * | 1.14 | (0.69–1.86) | 0.605 | 0.49 | (0.12–1.99) | 0.320 |
| At least one psychiatric diagnosis | 1.37 | (1.05–1.76) | 0.017 * | 2.13 | (1.53–2.93) | <0.001 * | 0.85 | (0.58–1.25) | 0.425 | 0.85 | (0.39–1.82) | 0.683 |
| At least one addiction diagnosis | 0.57 | (0.43–0.73) | <0.001 * | 1.64 | (1.15–2.32) | 0.006 * | 0.34 | (0.23–0.48) | <0.001 * | 0.43 | (0.22–0.8) | 0.008 * |
| Both diagnoses | 0.64 | (0.14–2.79) | 0.555 | 0.17 | (0.02–1.29) | 0.088 | 1.52 | (0.18–1.22) | 0.695 | 1.00 | (0–0) | |
The use of asterisk (*) indicates the statistical significance. 3+: more than three comorbidities
The categories “Alcohol abuse” and “At least one addiction diagnosis” seem to prevent PQIs hospitalization except for the PQI-91 acute one (OR = 0.43, 95% CI: 0.31–0.58 and OR = 0.57, 95% CI: 0.43–0.73, respectively, for the association of alcohol abuse and at least one addiction diagnosis with PQI-90 overall; OR = 0.33, 95% CI: 0.22–0.48 and OR = 0.34, 95% CI: 0.23–0.48, respectively, for the association of alcohol abuse and at least one addiction diagnosis with PQI-92 chronic; OR = 0.32, 95% CI: 0.15–0.68 and OR = 0.43, 95% CI: 0.22–0.80, respectively, for the association of alcohol abuse and at least one addiction diagnosis with PQI-93 diabetes).
In females (Table 5), the categories “Alcohol abuse” and “At least one addiction diagnosis” seem to prevent PQI-90 overall and PQI-92 chronic hospitalizations (OR = 0.39, 95% CI: 0.15–0.99 and OR = 0.44, 95% CI: 0.20–0.96, respectively, for the association of alcohol abuse and at least one addiction diagnosis with PQI-90 overall; OR = 0.19. 95% CI: 0.04–0.77 and OR = 0.16, 95% CI: 0.03–0.65, respectively, for the association of alcohol abuse and at least one addiction diagnosis with PQI-92 chronic). There is no evidence of risk factors for psychosis, depression, drug abuse, and addiction diagnosis. As for males, data analysis shows a growing positive association between the age of the patients and the increase in comorbidities.
Table 5.
Logistic regression for PQI in females.
| PQI-90 Overall | PQI-91 Acute | PQI-92 Chronic | PQI-93 Diabetes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Odds Ratio (95%) | p Value | Odds Ratio (95%) | p Value | Odds Ratio (95%) | p Value | Odds Ratio (95%) | p Value | |||||
| Age | ||||||||||||
| 18–40 | Ref. | - | - | Ref. | - | - | Ref. | - | - | Ref. | - | - |
| 41–60 | 1.45 | (1.19–1.76) | <0.001 * | 1.55 | (1.23–1.94) | <0.001 * | 1.78 | (1.18–2.69) | 0.006 * | 0.89 | (0.4–1.91) | 0.756 |
| 61–80 | 2.56 | (2.14–3.06) | <0.001 * | 2.24 | (1.81–2.77) | <0.001 * | 3.60 | (2.42–5.34) | <0.001 * | 1.71 | (0.83–3.52) | 0.142 |
| Over 80 | 4.23 | (3.53–5.05) | <0.001 * | 3.39 | (2.73–4.2) | <0.001 * | 5.87 | (3.96–8.7) | <0.001 * | 0.99 | (0.47–2.05) | 0.979 |
| Physical comorbidities (Num) | ||||||||||||
| 0 | Ref. | - | - | Ref. | - | - | Ref. | - | - | Ref. | - | - |
| 1 | 3.57 | (3.17–4.02) | <0.001 * | 1.36 | (1.16–1.59) | <0.001 * | 22.17 | (16.34–30.06) | <0.001 * | 221.90 | (30.34–1622.45) | <0.001 * |
| 2 | 7.52 | (6.68–8.45) | <0.001 * | 1.50 | (1.26–1.78) | <0.001 * | 56.54 | (41.78–76.5) | <0.001 * | 630.16 | (86.34–4598.79) | <0.001 * |
| 3+ | 18.89 | (16.77–21.27) | <0.001 * | 0.99 | (0.78–1.23) | 0.901 | 163.63 | (120.93–221.39) | <0.001 * | 1326.64 | (181.6–9691.2) | <0.001 * |
| Alcohol abuse | 0.39 | (0.15–0.99) | 0.048 * | 1.40 | (0.44–4.44) | 0.565 | 0.19 | (0.04–0.77) | 0.021 * | 0.61 | (0.08–4.39) | 0.622 |
| Drug abuse | 0.47 | (0.11–1.95) | 0.303 | 1.14 | (0.28–4.64) | 0.853 | 1.00 | (0–0) | 1.00 | (0–0) | ||
| Psychoses | 0.87 | (0.54–1.37) | 0.541 | 0.87 | (0.41–1.84) | 0.720 | 0.85 | (0.47–1.49) | 0.566 | 1.43 | (0.52–3.91) | 0.485 |
| Depression | 1.03 | (0.77–1.38) | 0.825 | 1.24 | (0.76–2.01) | 0.392 | 0.94 | (0.65–1.33) | 0.716 | 0.45 | (0.14–1.4) | 0.169 |
| At least one psychiatric diagnosis | 0.99 | (0.77–1.26) | 0.933 | 1.13 | (0.75–1.7) | 0.553 | 0.91 | (0.67–1.23) | 0.556 | 0.74 | (0.34–1.58) | 0.443 |
| At least one addiction diagnosis | 0.44 | (0.2–0.96) | 0.040 * | 1.46 | (0.59–3.57) | 0.405 | 0.16 | (0.03–0.65) | 0.011 * | 0.49 | (0.06–3.54) | 0.482 |
| Both diagnoses | 1.00 | 1.00 | (0–0) | 1.00 | (0–0) | 1.00 | (0–0) | |||||
The use of asterisk (*) indicates the statistical significance. 3+: more than three comorbidities
4. Discussion
Our results show that, in males, there is a clear positive association between the four investigated psychiatric conditions/addictions and PQI-91 acute potentially preventable admissions, with the exception of alcohol abuse for which the association is not statistically significant. On the contrary, in females, having a mental health condition/addiction does not seem to increase the risk of undergoing an avoidable acute hospitalization.
Research has consistently found that men of different ages, nationalities, and social backgrounds are less likely than women to seek professional help for physical and mental health problems [15,16,17]. This means that men are more at risk of developing complications from their medical conditions leading to avoidable hospitalizations, as evidenced by our results for acute preventable hospitalizations. The social construction of masculinity, which requires a man to provide for his problems with his strengths, and the stigma of mental health conditions, with its feeling of shame and blame, are known to be some of the determinants that most affect men’s healthcare service use [4,18]. Furthermore, women tend to use preventive and diagnostic services more frequently, whereas men make greater use of emergency services [19,20]. It is assumed that these determinants could play a role even in our population. However, specific research about the use of non-psychiatric healthcare services by patients with psychiatric/addiction problems is needed to confirm this.
PQI-91 is a composite indicator that includes acute preventable admissions for urinary tract infections and bacterial pneumonia. Treating these diseases promptly when the first symptoms appear is certainly a primary goal. However, the prevention of these conditions is a more ambitious health goal even if not more difficult to achieve. Considering that streptococcus pneumoniae is the pathogen most responsible for bacterial pneumoniae, a strong campaign to promote pneumococcal vaccination, aimed specifically at male patients with these mental health conditions, is one of the possible ways to reduce acute avoidable hospitalizations in our Local Health Authority [21].
In males, there are no other significant associations of mental illness neither with preventable hospitalizations for chronic conditions nor specifically for hospitalizations related to diabetes. Chronic conditions such as those included in PQI-92 and PQI-93 (diabetes, COPD, asthma, hypertension, and heart failure) offer a longer period between the onset of symptoms and the occurrence of complications worthy of hospitalization [12]. This means that there is more time for the general practitioner or for other specialists to intercept the disease and take care of the patient, even with mental health comorbidities. Otherwise, acute conditions, included in PQI-91 composite indicator, such as bacterial pneumonia and urinary tract infections tend to evolve quickly, leading in a short time to complications and hospitalizations. One hypothesis to explain our findings is that males with mental health conditions face barriers that prevent access to general medical care in a short time.
Many general practitioners in Italy, even before the COVID-19 pandemic, had abandoned the organization of the open-access clinic in favor of the organization of an appointment diary [22]. This is one of the reasons that could explain why accessing care for acute problems could be so challenging for this group of patients. Making and meeting an appointment is not an easy task for a patient with mental health problems or addictions, because of the mental disease symptoms but also for the socioeconomic factors that usually match these conditions [2,23]. Creating specific agendas for access to medical care for this fragile population group is one of the possible solutions.
The protective role of alcohol abuse (and more generally of the category “At least one diagnosis of addiction”) towards PQI-90 overall and PQI-92 chronic preventable hospitalizations in females is peculiar [23]. However, this result could be influenced by the low number of women with addictions included in PQI groups. On the contrary, in men, whose numerical representativeness is greater in PQI groups, the protective role of alcohol abuse is even stronger and extends to PQI-93 diabetes-related preventable admissions [12,24].
Studies have showed that certain mental health conditions lead the patient to refer to the general practitioner more often. This is the case of generalized anxiety disorder, post-traumatic stress disorder, and panic disorder [25]. However, when focusing on alcohol abuse, many studies highlight how this condition is linked with fewer primary health care visits and more non-psychiatric hospitalizations [26]. Further investigations should be carried out to understand these results, which could arise from study limits but also, for example, from a particular and as yet undefined characteristic of the population under study or from a good functioning of the territorial services for alcohol addiction.
In our study, we performed a logistic regression to assess the association of mental conditions to preventable association correcting for age and physical comorbidities. Further elements, such as socioeconomic condition and consumption of medications, may be considered to further correct our findings for a more in-depth study.
The overall number of patients in the PQI categories represents a limit to the understanding of the phenomenon, especially in females for whom drug and alcohol abuse are less frequent even if in sharp growth [27,28]. Extending the observation period of our study can bring out associations that cannot be highlighted with the current sample. However, the overall number of patients in PQI groups is also linked to the coding of the hospital discharge records (HDRs). Although the coding of HDRs has been regulated by ministerial guidelines and the reproducibility has significantly improved over the years, there is still a fair amount of variability among healthcare professionals in the choice of the ICD-9-CM codes to be identified as the main and secondary diagnosis [29]. The main diagnosis code is fundamental, for our study and according to the indications of the AHRQ, to identify or exclude a preventable hospitalization. The secondary diagnoses codes, on the other hand, are equally important to identify patients with mental health conditions or addiction. It is documented that in Italy, mental health conditions are clearly underdiagnosed and, therefore, not coded (especially when it comes to comorbidities) among the hospital discharge record diagnoses.
The AHRQ definitions are one of the possibilities to identify potentially preventable hospitalizations. Although well-validated and provided with exclusion criteria for comorbidities that would make them not preventable, there could be some hospitalizations identified that are not preventable. Conversely, hospitalizations for other diagnoses not identified by AHRQ criteria may have been potentially preventable.
Finally, our data concern a limited population of a Local Health Authority and may not be generalizable.
5. Conclusions
Gender can have an impact on the accessibility of primary care for patients with psychiatric pathologies or addictions. Quality prevention for patients with mental health conditions or addictions and improved access to psychiatric and non-psychiatric services may limit potentially preventable hospitalizations.
The gender lens we applied to our population may be a successful approach to health inequalities: women and men respond to different diagnostic-prescriptive appropriateness, which depends both on biology and on social, cultural, psychological, and economic differences.
In a public health system where equity of access to care is one of the dimensions of quality, research in this area can help identify the most vulnerable population subgroups and guide targeted health policies.
Acknowledgments
This study arises from a scientific collaboration within the Working Group on Public Mental Health of the medical residents’ Assembly of the Italian Society of Hygiene and Preventive Medicine, of which some of the authors are members and/or coordinators.
Appendix A
What Are the PQI Composites?
Although they rely on hospital discharge data, the Prevention Quality Indicators (PQI) are measures of potentially avoidable hospitalizations for Ambulatory Care Sensitive Conditions (ACSCs) that are meant to reflect issues with access to and the quality of ambulatory care in a specific geographic area. The PQI composites are designed to increase the statistical accuracy of the individual PQI, enabling better performance differentiation across areas and increased capacity to recognize potential performance-determining factors.
An overall composite, which connects the several PQI measures—all of which are rates at the local level—captures the overall idea of possibly avoidable hospitalization. To examine various factors affecting hospitalization rates for each ailment, several composite measures for acute and chronic conditions were developed. The measurements that make up each of the four PQI composites are listed in Table A1.
Table A1.
AHRQ PQI Composite Measures, v2021.
| PQI 90 PREVENTION QUALITY OVERALL COMPOSITE |
|---|
| PQI 01 Diabetes Short-Term Complications Admission Rate |
| PQI 03 Diabetes Long-Term Complications Admission Rate |
| PQI 05 Chronic Obstructive Pulmonary Disease (COPD) or Asthma in Older Adults Admission Rate |
| PQI 07 Hypertension Admission Rate |
| PQI 08 Heart Failure Admission Rate |
| PQI 11 Community Acquired Pneumonia Admission Rate |
| PQI 12 Urinary Tract Infection Admission Rate |
| PQI 14 Uncontrolled Diabetes Admission Rate |
| PQI 15 Asthma in Younger Adults Admission Rate |
| PQI 16 Lower-Extremity Amputation among Patients with Diabetes Rate |
| PQI 91 PREVENTION QUALITY ACUTE COMPOSITE |
| PQI 11 Bacterial Pneumonia Admission Rate |
| PQI 12 Urinary Tract Infection Admission Rate |
| PQI 92 PREVENTION QUALITY CHRONIC COMPOSITE |
| PQI 01 Diabetes Short-Term Complications Admission Rate |
| PQI 03 Diabetes Long-Term Complications Admission Rate |
| PQI 05 Chronic Obstructive Pulmonary Disease (COPD) or Asthma in Older Adults Admission Rate |
| PQI 07 Hypertension Admission Rate |
| PQI 08 Heart Failure Admission Rate |
| PQI 14 Uncontrolled Diabetes Admission Rate |
| PQI 15 Asthma in Younger Adults Admission Rate |
| PQI 16 Lower-Extremity Amputation among Patients with Diabetes Rate |
| PQI 93 PREVENTION QUALITY DIABETES COMPOSITE |
| PQI 01 Diabetes Short-Term Complications Admission Rate |
| PQI 03 Diabetes Long-Term Complications Admission Rate |
| PQI 14 Uncontrolled Diabetes Admission Rate |
| PQI 16 Lower-Extremity Amputation among Patients with Diabetes Rate |
This table is sourced from Quality Indicator User Guide: Prevention Quality Indicators (PQI) Composite Measures, v2022 with permission from the Agency for Healthcare Research and Quality [30].
Author Contributions
Conceptualization, methodology, formal analysis, investigation, supervision, and project administration, F.C. and A.C.; software, F.C.; validation, L.S., N.B., M.C., G.M., C.C. and C.M.; writing—original draft preparation, F.C., A.C., N.B. and M.C.; writing—review and editing, C.M., C.C., G.M., L.S. and G.D.M.; visualization, F.C., A.C., G.M., G.D.M., C.M. and C.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Ethical review and approval was waived due to retrospective protocol conducted on perfectly anonymized clinical records.
Informed Consent Statement
Patient consent was waived due to retrospective protocol conducted on perfectly anonymized clinical records.
Data Availability Statement
Authors can be contacted for information about dataset.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sara G., Chen W., Large M., Ramanuj P., Curtis J., McMillan F., Mulder C.L., Currow D., Burgess P. Potentially preventable hospitalisations for physical health conditions in community mental health service users: A population-wide linkage study. Epidemiol. Psychiatr. Sci. 2021;30:e22. doi: 10.1017/S204579602100007X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ross L.E., Vigod S., Wishart J., Waese M., Spence J.D., Oliver J., Chambers J., Anderson S., Shields R. Barriers and facilitators to primary care for people with mental health and/or substance use issues: A qualitative study. BMC Fam. Pract. 2015;16:135. doi: 10.1186/s12875-015-0353-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Otten D., Tibubos A.N., Schomerus G., Brähler E., Binder H., Kruse J., Ladwig K.-H., Wild P.S., Grabe H.J., Beutel M.E. Similarities and differences of mental health in women and men: A systematic review of findings in three large german cohorts. Front. Public Health. 2021;9:553071. doi: 10.3389/fpubh.2021.553071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pattyn E., Verhaeghe M., Bracke P. The gender gap in mental health service use. Soc. Psychiatry Psychiatr. Epidemiol. 2015;50:1089–1095. doi: 10.1007/s00127-015-1038-x. [DOI] [PubMed] [Google Scholar]
- 5.Slaunwhite A.K. The role of gender and income in predicting barriers to mental health care in canada. Community Ment. Health J. 2015;51:621–627. doi: 10.1007/s10597-014-9814-8. [DOI] [PubMed] [Google Scholar]
- 6.Gillies D., Buykx P., Parker A.G., Hetrick S.E. Consultation liaison in primary care for people with mental disorders. Cochrane Database Syst. Rev. 2015;2016:CD007193. doi: 10.1002/14651858.CD007193.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eghaneyan B.H., Sanchez K., Mitschke D.B. Implementation of a collaborative care model for the treatment of depression and anxiety in a community health center: Results from a qualitative case study. J. Multidiscip. Health. 2014;7:503–513. doi: 10.2147/JMDH.S69821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huxley P. Mental illness in the community: The Goldberg-Huxley model of the pathway to psychiatric care. Nord. J. Psychiatry. 1996;50:47–53. doi: 10.3109/08039489609099730. [DOI] [Google Scholar]
- 9.Martin C., Hinkley N., Stockman K., Campbell D. Potentially preventable hospitalizations-The “pre-hospital syndrome”: Retrospective observations from the MonashWatch self-reported health journey study in Victoria, Australia. J. Eval. Clin. Pract. 2021;27:228–235. doi: 10.1111/jep.13460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnston J., Longman J., Ewald D., King J., Das S., Passey M. Study of potentially preventable hospitalisations (PPH) for chronic conditions: What proportion are preventable and what factors are associated with preventable PPH? BMJ Open. 2020;10:e038415. doi: 10.1136/bmjopen-2020-038415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manzoli L., Flacco M.E., De Vito C., Arcà S., Carle F., Capasso L., Marzuillo C., Muraglia A., Samani F., Villari P. AHRQ prevention quality indicators to assess the quality of primary care of local providers: A pilot study from Italy. Eur. J. Public Health. 2014;24:745–750. doi: 10.1093/eurpub/ckt203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Di Martino G., Di Giovanni P., Cedrone F., D’Addezio M., Meo F., Scampoli P., Romano F., Staniscia T. The Burden of Diabetes-Related Preventable Hospitalization: 11-Year Trend and Associated Factors in a Region of Southern Italy. Healthcare. 2021;9:997. doi: 10.3390/healthcare9080997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agency for Healthcare Research and Quality AHRQ QualityIndicators Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions. [(accessed on 12 September 2022)]; Available online: http://www.ahrq.gov.
- 14.Quan H., Sundararajan V., Halfon P., Fong A., Burnand B., Luthi J.-C., Saunders L.D., Beck C.A., Feasby T.E., Ghali W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 15.Husaini B.A., Moore S.T., Cain V.A. Psychiatric Symptoms and Help-Seeking Behavior Among the Elderly. J. Gerontol. Soc. Work. 1994;21:177–196. doi: 10.1300/J083V21N03_12. [DOI] [Google Scholar]
- 16.D’Arcy C., Schmitz J.A. Sex differences in the utilization of health services for psychiatric problems in Saskatchewan. Can. J. Psychiatry. 1979;24:19–27. doi: 10.1177/070674377902400106. [DOI] [PubMed] [Google Scholar]
- 17.Neighbors H.W., Howard C.S. Sex differences in professional help seeking among adult black Americans. Am. J. Community Psychol. 1987;15:403–417. doi: 10.1007/BF00915210. [DOI] [PubMed] [Google Scholar]
- 18.Addis M.E., Mahalik J.R. Men, masculinity, and the contexts of help seeking. Am. Psychol. 2003;58:5–14. doi: 10.1037/0003-066X.58.1.5. [DOI] [PubMed] [Google Scholar]
- 19.Vaidya V., Partha G., Karmakar M. Gender differences in utilization of preventive care services in the United States. J. Women’s Health. 2012;21:140–145. doi: 10.1089/jwh.2011.2876. [DOI] [PubMed] [Google Scholar]
- 20.Anson O., Carmel S., Levin M. Gender differences in the utilization of emergency department services. Women Health. 1991;17:91–104. doi: 10.1300/J013v17n02_05. [DOI] [PubMed] [Google Scholar]
- 21.Cilloniz C., Martin-Loeches I., Garcia-Vidal C., San Jose A., Torres A. Microbial etiology of pneumonia: Epidemiology, diagnosis and resistance patterns. Int. J. Mol. Sci. 2016;17:2120. doi: 10.3390/ijms17122120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.FIMMG (Federazione Italiana Medici di Medicina Generale) Protocollo per gli Ambulatori Medici per la Gestione Post-Emergenza COVID-19. [(accessed on 12 September 2022)]. Available online: https://www.fimmg.org/index.php?action=pages&m=view&p=30877&lang=it.
- 23.Di Giovanni P., Di Martino G., Zecca I.A.L., Porfilio I., Romano F., Staniscia T. The Revolving Door Phenomenon: Psychiatric Hospitalization and Risk of Readmission Among Drug-Addicted Patients. Clin. Ter. 2020;171:e421–e424. doi: 10.7417/CT.2020.2252. [DOI] [PubMed] [Google Scholar]
- 24.Di Martino G., Di Giovanni P., Cedrone F., Michela D., Meo F., Scampoli P., Romano F., Staniscia T. The Impact of COPD on Hospitalized Patients with Diabetes: A Propensity Score Matched Analysis on Discharge Records. Healthcare. 2022;10:885. doi: 10.3390/healthcare10050885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fogarty C.T., Sharma S., Chetty V.K., Culpepper L. Mental health conditions are associated with increased health care utilization among urban family medicine patients. J. Am. Board Fam. Med. 2008;21:398–407. doi: 10.3122/jabfm.2008.05.070082. [DOI] [PubMed] [Google Scholar]
- 26.Miquel L., Manthey J., Rehm J., Vela E., Bustins M., Segura L., Vieta E., Colom J., Anderson P., Gual A. Risky alcohol use: The impact on health service use. Eur. Addict. Res. 2018;24:234–244. doi: 10.1159/000493884. [DOI] [PubMed] [Google Scholar]
- 27.White A.M. Gender differences in the epidemiology of alcohol use and related harms in the United States. Alcohol Res. 2020;40:1. doi: 10.35946/arcr.v40.2.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Center for Behavioral Health Statistics and Quality 2016 National Survey on Drug Use and Health: Detailed Tables. [(accessed on 12 September 2022)]; Available online: https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf.
- 29.Ministero della Salute Aggiornamento delle Linee Guida per la Codifica delle Informazioni Cliniche della Scheda di Dimissione Ospedaliera (SDO). 2010. [(accessed on 6 November 2022)]; Available online: https://www.salute.gov.it/portale/temi/p2_6.jsp?lingua=italiano&id=1232&area=ricoveriOspedalieri&menu=vuoto.
- 30.“Quality Indicator User Guide: Prevention Quality Indicators (PQI) Composite Measures, v2022” [serial online] Published July 2022. [(accessed on 6 November 2022)]; Available online: https://qualityindicators.ahrq.gov/Downloads/Modules/PQI/V2022/PQI_Composite_Measures.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Authors can be contacted for information about dataset.