Abstract
Gastric cancer is the subject of clinical and basic studies due to its high incidence and mortality rates worldwide. Due to the diagnosis occurring in advanced stages and the classic treatment methodologies such as gastrectomy and chemotherapy, they are extremely aggressive and limit the quality of life of these patients. CRISPR/Cas9 is a tool that allows gene editing and has been used to explore the functions of genes related to gastric cancer, in addition to being used in the treatment of this neoplasm, greatly increasing our understanding of cancer genomics. In this mini-review, we seek the current status of the CRISPR/Cas9 gene-editing technology in gastric cancer research and clinical research.
Keywords: gastric cancer, CRISPR, gene editing
1. Introduction
Gastric cancer (GC) remains an important cancer worldwide, ranking fifth for incidence and fourth for mortality globally [1]. The high mortality rates of GC are mainly due to its detection at advanced stages, where it can no longer be treated with curative intent, and to the few available therapeutic options [2]. Currently, gastrectomy is the main option for locoregional GC treatment [3]. However, even after curative resection and adjuvant chemotherapy, the clinical outcome remains poor, with a recurrence rate of approximately 35% [4]. Despite some recent advances that have been made in the treatment of GC (e.g., systemic chemotherapy, radiotherapy, surgery, immunotherapy, and targeted therapy), only a subset of patients can benefit from these treatment options [5].
GC is a complex, heterogeneous, and multistep disease that involves environmental factors, mainly Helicobacter pylori infection, and several molecular alterations, such as genetic instability, the inactivation of tumor suppressor genes, and the activation of oncogenes.
Moreover, the molecular profiles may vary from patient to patient. Although many studies proposed a great number of diagnostic and prognostic markers, only a few of them are currently used in clinical practice [6]. Furthermore, different epigenetic alterations have been reported to activate oncogenes and inactivate tumor suppressor genes during gastric carcinogenesis [7]. Therefore, an understanding of the molecular aspects involved in gastric carcinogenesis and tumor heterogeneity is essential to providing new multidisciplinary treatments [8].
In this context, gene-editing technology has received increasing attention in GC, as it can adjust gene expression alterations and correct mutations. In addition, this technology can also reveal the roles of unknown genes in important pathways, and consequently can help in the identification of new biomarkers and therapeutic targets, as well as the mechanisms of GC responses to drug treatment [9].
Since Kim et. al.’s study, the methodologies for gene editing have involved the use of the zinc finger nuclease (ZFN) and the transcription activator effector nuclease (TALENs) by targeting DNA domain-binding proteins [10,11,12,13,14]. Currently, clustered regularly interspaced short palindromic repeat (CRISPR)-associated 9 is a gene-editing tool with a lower cost, higher efficiency, and less complexity in its application. In addition, the 2020 Nobel Prize in Chemistry was awarded to Emmanuelle Charpentier and Jennifer Doudna for the development of the CRISPR/Cas9 gene-editing technology [15].
In this mini-review, we first describe the mechanism and development of the CRISPR/Cas9 gene-editing system. Furthermore, we focus on the current applications of this technique for the basic research, diagnosis, and therapy of GC. The potential applications of CRISPR/Cas9 in GC therapy and the challenges are discussed.
2. The CRISPR/CAS9 Technology
The first hint of CRISPR was in 1987, when Japanese scientists studied the alkaline phosphatase gene in Escherichia coli and discovered an adjacent region of unknown function [16]. After two decades, it was discovered that these previously unknown regions were related to the adaptive immune systems of bacteria and prokaryotic organisms such as archaea [17,18,19]. This finding favored the discovery of the association of the catalytic enzyme Cas9 with the CRISPR system, providing the double-stranded DNA breaks [20]. In 2013, the CRISPR/Cas9 system was used for the first time as a gene-editing tool [21,22,23].
CRISPR/Cas9 works with a simplified system using a guide RNA (gRNA) that can recognize the genomic target through base complementarity according to the Watson–Crick theory, and also has the function of aggregating the endonuclease Cas9. Due to its simple system, greater specificity, and efficiency, the CRISPR/Cas9 system is a much more effective tool than the previous ZFN and TALENs methodologies [24].
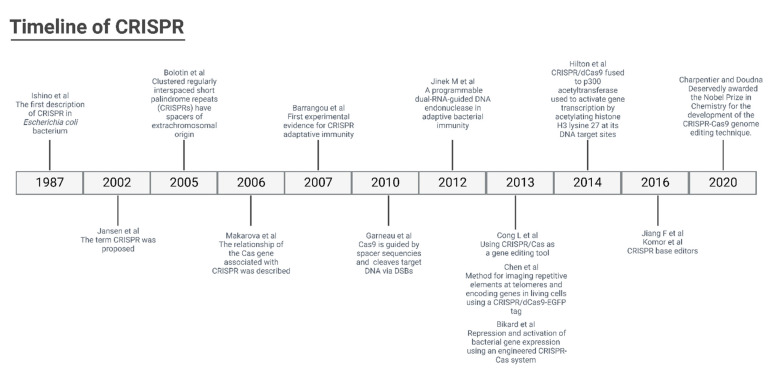
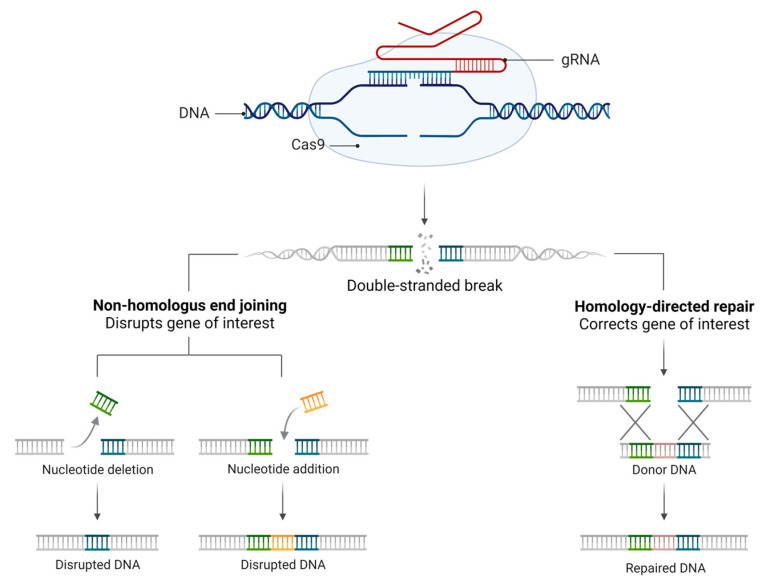
The CRISPR methodology has been improved over time (Figure 1), and to determine the specificity of the machinery connection, a PAM (protospacer-adjacent motif) primer sequence of 3 nucleotides (NGG) before the 20 nucleotides of the target is determined. In addition, the Cas type II protein from Streptococcus pyogenes (SpCas9) has been used for the break of the double strand of DNA. In response to DNA cleavage, the host cell can perform two different repair mechanisms. The non-homologous end joining (NHEJ) is a mechanism where the ends of the tape come together, which is subject to unwanted insertions or deletions. Another mechanism is homology-directed repair (HDR), which uses recombinations already determined from DNA models to reconstitute the cleaved DNA (Figure 2).
Figure 1.
Timeline of CRISPR technology [16,17,18,19,21,25,26,27,28,29,30,31,32].
Figure 2.
CRISPR repair mechanism. Classic CRISPR mechanism comprising the guide RNA (gRNA), target DNA, and endonuclease (Cas9), which promotes DNA cleavage by DSBs induced by Cas9. DSBs can be repaired by two main mechanisms: the NHEJ mechanism, where the ends of the strands come together (this is subject to unwanted insertions or deletions), or by the HDR pathway, which uses the recombination donor DNA templates to reconstitute the DSB.
In addition, large chromosomal deletions, inversions, and translocations [33], as well as plasmid and retrotransposon insertions [34,35], have also been reported in the literature as a result of the DSBs induced by CRISPR/Cas9.
Accordingly, the ability of CRISPR/Cas9 to generate DNA double-stranded breaks at sites of interest, introducing a donor DNA template into the target cell, means it has been proven to be a useful tool for genome editing [36,37].
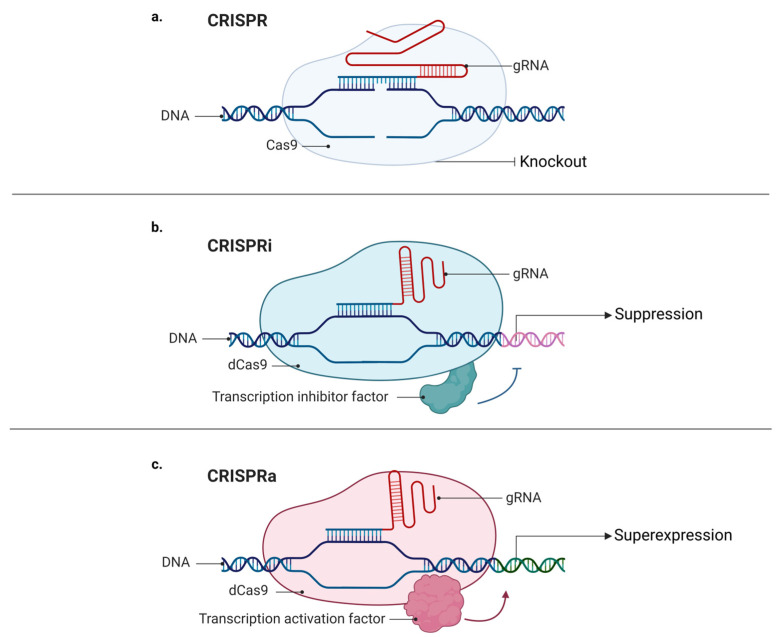
Moreover, using a modified version of the Cas9 protein, dCas9 (catalytic “dead” Cas9), it is possible to target desirable regions on the genome without cutting the DNA strands [25,38], which enables the possibility of adding many different proteins to dCas9, including fluorescent proteins. In 2013, Chen and collaborators described a method for the imaging of repetitive elements in telomeres and coding genes in living cells using a CRISPR/dCas9-EGFP tag [26]. Interestingly, regulatory factors such as modulators of gene expression can also be fused to dCas9. Like RNAi (RNA interference), CRISPRi (CRISPR interference) may be used to repress gene expression, although using a different mechanism. While RNAi uses a nucleotide base complementary to the desired sequence and the RNA-induced silencing complex (RISC) to suppress an mRNA target [39], CRISPRi uses a dCas9 linked to a transcription repressor domain to identify and bind to a specific DNA locus, and then to inhibit its transcription [40]. On the other hand, it is also possible to conjugate a dCas9 to a transcription activator and to create a CRISPR activation (CRISPRa) system [40]. Hilton and colleagues revealed that CRISPR/dCas9 fused to the human acetyltransferase p300 can be used to activate gene transcription by acetylating histone H3 lysine 27 at its DNA target sites (Figure 3) [27].
Figure 3.
Mechanisms of CRISPR, CRISPRa, and CRISPRi: (a) classic CRISPR mechanism comprising a guide RNA (gRNA), target DNA, and endonuclease (Cas9), which promotes DNA cleavage, resulting in a knockout; (b) CRISPR mechanism comprising a guide RNA (gRNA), sequence target (target DNA), and “dead” endonuclease (dCas9), without its catalytic domain, fused with inhibitory transcription factors favoring decreased expression and generating knockdown; (c) CRISPR mechanism comprising a guide RNA (gRNA), target sequence (target DNA), and “dead” endonuclease (dCas9), without its catalytic domain, fused with transcriptional activating factors, favoring increased expression and causing upregulation of a given gene.
Additionally, a dCas9 may be engineered to introduce point mutations to a specific DNA sequence without causing DSBs. Fusing a single-stranded DNA deaminase enzyme to dCas9 allows for single-nucleotide modifications at a genomic sequence of interest. Taking advantage of a segment of accessible single-stranded DNA formed by dCas9, gRNA, and target DNA, so far cytidine and adenine deaminases have been used to convert cytosine into uracil and adenosine into inosine, respectively [28,29,41].
In the context of gastric diseases, Krishnamurthy and collaborators studied gastric organoids derived from two individuals with homozygous mutations in PDX1 (pancreatic and duodenal homeobox 1), causing a loss of its expression. PDX1188delC/188delC organoids resulted in gastritis, a loss of antral identity, and gastric and intestinal metaplasia. Interestingly, the restoration of PDX1 protein expression via PDX1 point mutations using CRISPR/Cas9 also reversed these phenotypes. These results suggest that the CRISPR-mediated correction of point mutations has the potential to improve patient care in the future [42].
Garcia-Bloj et al. [43], by comparing the ZFN, TALENs, and CRISPR technologies for the overexpression of tumor suppressors in GC strains, demonstrated that CRISPR-dCas9 can restore the expression of the MASPIN/REPRIMO genes, being considered a transient, targeted, and efficient tool for restoring tumor suppressor functions.
3. Application of CRISPR/CAS9 in Basic GC Research
CRISPR/CAs9 is an extremely versatile tool that can be used in the study and understanding of cancer development mechanisms and in the diagnosis and treatment of several diseases, including GC [15].
This technique has helped studies in several areas, such as for gastric cancer, where in 2015 the study by Gannom and colleagues used the CRISPR/Cas9 technique for the first time in GC [44]. This pioneering study evaluated the knockdown effect of dual-specificity mitogen-activated protein kinase 1 (MAP2K1) and the relationship of MEK-inhibitory drugs with cancer cell lines, including gastric cancer. This study was important to evidence the RAS/MAPK activation driven by MAP2K1 depletion in gastric cancer.
CRISPR is an important tool that [9] helps us in a simple and practical way to understand the functions of genes that are still poorly described in GC. A collection of relevant GC studies that used CRISPR/Cas9 may be found in Table 1.
Table 1.
Studies performed in gastric cells using the CRISPR/Cas9 methodology.
| Gene | Cell Line | CRISPR Approach | Phenotype | Gene Classification | Functional Analyzes Performed |
Reference |
|---|---|---|---|---|---|---|
| FGFR | KATOIII, SNU16, AGS | Knockout | Cell proliferation, migration, differentiation, and cell death | Oncogene | Cell viability | [45] |
| PDIA3 | HFE145 e GES-1 | Knockout | Stress-resonant protein. | NE | Colony formation | [46] |
| ATG16L1 | AGS, HeLa | Knockout | Autophagy | NE | Cell viability | [47] |
| PDEF | GES, SGC, AGS | Knockout | Transcription factor | Oncogene | Proliferation, apoptosis, colony formation, migration, and invasion | [48] |
| GMAN | BGC-823, SGC-7901 e MKN45, GES-1 HGC-27, MGC-803, AGS | Knockout | Metastasis. | Oncogene | Invasion assay, Cell cycle, proliferation, and colony formation | [49] |
| PIWIL1 | AGP01 | Knockout | Cell proliferation | Oncogene | Proliferation, apoptosis, colony formation, migration, and invasion | [50] |
| MicroRNA-21 | TMK-1, AGS, KATO III, NCI-N87, MKN-1, MKN-28, MKN-45, SNU-1, SNU-5, SNU-216, SNU- 484, SNU-601, SNU-638, SNU-668 e SNU-719 | Knockout | Regulation of prostaglandins in carcinogenesis | Oncogene | Proliferation, apoptosis, colony formation | [51] |
| MRFAP1 | AGS, SGC-7901 | Knockout | Cell cycle | Tumor suppressor | Cell cycle, cell viability | [52] |
| LMX1A | AGS primary cells C-1/GC-2 | Knockout | Transcription factor | Tumor suppressor | Viability, colony formation, TUNEL (cell death) | [53] |
| CEACAM | AGS, KatoIII | Knockout | Cell adhesion related to the carcinoembryonic antigen | NE | NE | [54] |
| ASC | AGS, MKN1 | Knockout | Proinflammatory cytokine | Oncogene | Apoptosis, colony formation assay | [55] |
| PANDAR | AGS SNU-1 | Knockout | LNC RNA promoter of RNA activated by damage to antisense DNA CDKN1A | Oncogene | Cell viability, proliferation, and colony formation | [56] |
| GSDME | SGC-7901, MKN-45, HL-60 | Knockout | Cell death by pyroptosis | Tumor suppressor | Cell Viability, LDH Release Assay, Cell Death, and Apoptosis | [57] |
| REPRIMO | BGC-823, AGS GES-1 | Knockout | Cell cycle | Tumor suppressor | MTT | [58] |
| miR-30a | MKN45 SGC-7901 HEK293T | Knockout | Post-transcriptional regulation | Tumor suppressor | Proliferation, migration, colony formation, viability | [59] |
| SPOCD1 | BGC823, HGC27, MGC803, SGC7901, MKN28 GES1 | Knockout | Promotes migration and apoptosis reduction in CG | Oncogene | Proliferation, colony formation, migration, and invasion | [60] |
| BTN3A2 | BGC823, HGC27, MGC803, SGC7901, MKN28 GES1 | Knockout | Adaptive immune response | Oncogene | Proliferation, colony formation, migration, and invasion | [60] |
| AEP | HEK293T, MKN45 e SGC7901 | Knockout | Lysosomal protein | Oncogene | Cell viability | [61] |
| MASPIN | HEK293T, MCF7, SUM159, H157 | Knockin | Mammary protease serine inhibitor | Tumor suppressor | Cell viability, apoptosis, and proliferation | [43] |
| REPRIMO | HEK293T, MCF7, SUM159, H157 | Knockin | Cell cycle | Tumor suppressor | Cell viability, apoptosis, and proliferation | [43] |
| EphB2 | HGC27 | Knockin | Migration and invasion | Oncogene | Cell viability, apoptosis, and proliferation | [62] |
| SST | 293T and BGC823 | Knockout | Migration and invasion | Tumor suppressor | Cell viability, apoptosis, and proliferation | [63] |
NE: not evaluated.
3.1. Cell Viability and Proliferation
Needless to say, the ability of cells to proliferate rapidly and uncontrollably is a key factor in GC. Therefore, understanding these biological mechanisms and genes is extremely important for the identification of therapeutic targets. The CRISPR/Cas9-mediated knockout of apoptosis-associated speck-like protein containing a C-terminal caspase recruitment domain (ASC) blocked IL18 and augmented apoptosis in human GC cells, helping to reveal a novel pro-tumorigenic ASC/IL18 signaling axis in GC cell survival and a candidate therapeutic target in this disease [55].
Contributing to the findings of mir-21-induced loss of 15-hydroxyprostaglandin dehydrogenase (15-PGDH) in early GC and its phenotypic consequences, another study suppressed 15-PGDH in GC cells using CRISPR/Cas9, which demonstrated increased GC cell proliferation [51]. Therefore, the study suggested that maintaining the 15-PGDH enzyme activity could be a strategy for preventing GC, especially in tubular adenocarcinoma.
3.2. Cell Cycle Control
The study of genes that influence the cell cycle allows us to identify important cellular processes that differentiate a tumor cell from a healthy cell. Aspects such as unrestrained growth without the influence of external factors, the loss of programmed cell death capacity, and also the repression of tumor suppressor genes, among other properties, are important to identify specific biomarkers and potential therapeutic targets in GC.
To demonstrate the involvement of DNA hypermethylation on the regulation of the tumor suppressor gene REPRIMO and the TP53-dependent G2 arrest mediator homolog (RPRM) in GC, Lai and collaborators [58] used the CRISPR/Cas9 technology to first knockdown DNA methyltransferases (DNMTs). The knockdown of DNMT3A and DNMT3B resulted in a significant increase in RPRM mRNA by decreasing the RPRM promoter methylation in GC cells, suggesting an inverse correlation between DNMT functions and RPRM gene expression. To confirm the tumor suppression role of RPRM, the authors generated RPRM-deficient GC cell lines using CRISPR/Cas9, which were further inoculated in mice. The loss of RPRM enhanced the tumor formation in the in vivo model, confirming the role of RPRM as a tumor suppressor gene in GC. This study provided information regarding the role of RPRM and its regulatory methylation mechanism in GC development with potential application as a therapeutic target.
To regain the tumor suppression gene function, a study reactivated the RPRM expression using CRISPR/dCas9 linked to VP64 and SAM effector domains in GC cell lines, showing a hypermethylated RPMR promoter and expressing very low basal levels of the gene [43]. As a result, a marked reduction in GC proliferation was observed. This result outlined the advantage of this combinatorial epigenome editing approach to reactivate highly methylated tumor suppressor genes as a promising therapy for GC.
Another promising tumor suppressor was described in the study by Hu and collaborators [52], with the knockout of the Morf4-family-associated protein 1 (MRFAP1) gene using CRISPR/Cas9 from the CG human cell lines. The researchers observed that the knockout promoted an interaction of this MLN4924 subtract with suppressed tumor proteins, such as p27, which promoted a decrease in vitality, increased cell cycle arrest, and apoptosis, data that are important to relate the gene–subtract interaction to favor improvements in cancer treatment. The study by Liu et al. [56] used the CRISPR/Cas9-mediated knockout of promoter of CDKN1A antisense DNA damage-activated RNA (PANDAR) and evaluated its effects on the phenotype of GC cell lines. The knockout of PANDAR suppressed the proliferative activity and colony formation in the GC cell line. It was also observed by flow cytometry that the PANDAR knockout blocks the progression of the cell cycle at the G1/S checkpoint. Through this unique pattern of transcriptional modification, PANDAR remarkably facilitated the proliferation of cancer cells, the formation of clones, and resistance to chemotherapy. Another study developed by Zhang and colleagues [53] used the CRISPR/Cas9-mediated knockout of LIM homeobox transcription factor 1 α (LMX1A) in GC cell lines to identify LMX1A as a primary target of miR-9. The authors that demonstrated the knockout of LMX1A increased the cell viability and cell proliferation, reinforcing the role of LMX1A as a tumor suppressor in GC.
3.3. Invasion and Migration
The basic mechanism of metastasis development involves several important characteristics, such as the ability of cells to detach themselves from the primary tumor site and migrate to colonize more distant sites in the organism [64]. Due to the lack of early diagnosis and effective therapy options for GC, a better understanding of the mechanisms involved in the metastatic process of GC is necessary. In this sense, Zhou and colleagues [49] used the CRISPR/Cas9-mediated knockout of gastric cancer metastasis-associated long non-coding RNA (GMAN) IncRNA and evaluated the phenotype of GC cells. The knockout of the GMAN lncRNA delayed the invasive activity of these cells. This study also showed the overlapping relationship between GMAN and ephrin A1, in which the GMAN knockout induced an ephrin A1 expression reduction. Assessing the effect of ephrin A1 knockout in GC cell lines, it reduced the ability for invasion and metastasis in in vivo experiments. Another important study was developed by Zhu and colleagues [60], in which a GWAS analysis was used to find low-frequency genetic variants associated with the risk of GC. The authors found two genes that contained a variant associated with GC risk, SPOC-domain-containing 1 (SPOCD1) and Butyrophilin subfamily 3 member A2 (BTN3A), and eliminated these genes using CRISPR/Cas9 in GC cell lines. The knockout of SPOCD1 and BTN3A2 inhibited cell proliferation and colony formation. To investigate the effects of SPOCD1 and BTN3A2 knockout on migration and invasion, the authors performed xenograft assays and observed a tumor growth reduction in a rat model associated with SPOCD1 knockout. On the other hand, BTN3A2 was suggested as a susceptibility gene, although no significant changes in the xenograft model were observed. Zhang et al. [48] demonstrated that the CRISPR/Cas9-mediated deletion of SAM-pointed domain-containing Ets transcription factor (PDEF) inhibited the apoptosis, colony formation, migration, and invasion of GC cell lines. These results confirm the involvement of PDEF in the different stages of GC development. The study by Araújo et al. [50] demonstrated that the CRISPR/Cas9-mediated elimination of the Piwi-like protein 1 (PIWIL1) gene decreased GC cell migration and invasion abilities, demonstrating the oncogenic role of PIWIL1. On the other hand, Chen Wei’s study [63] demonstrated that the CRISPR/Ca9-mediated knockout of Somatostatin (SST) significantly promoted the migration and invasion capabilities of GC cell lines. These data are essential for characterizing SST as a potential tumor suppressor in GC.
Another interesting study used the CRISPR/Cas9-mediated knockin of ephrin type-B receptor 2 (EphB2) and evaluated its functions as an independent prognostic marker in patients with GC [62]. The results indicated that the activation of EphB2 in GC cells increased the malignant properties of GC cells, reducing the adhesion but accelerating the migration and invasion capabilities. These results indicate that EphB2 plays a pro-tumor role in GC and has therapeutic potential to be used in this neoplasia.
3.4. Tumorigenesis Models
Helicobacter pylori is a Gram-negative spiral bacterium that is present in 58% of the global population [65]. Most individuals infected with H. pylori are asymptomatic, and the presence of this bacterium increases the risk of developing ulcers and gastric adenocarcinoma [66]. An interesting study was carried out by Hu and collaborators [49], who sought to demonstrate the mechanisms in which vitamin D3 can assist in the defense of the host by promoting an autophagic reaction in the fight against H. pylori. The results showed that there is a new pathogenic mechanism that H. pylori can survive by hiding inside the autophagosomes in the GC cells by using the CRISPR/Cas9-mediated knockout of protein disulfide-isomerase A3 (PDIA3). From this study, a new vitamin D3 signaling pathway activates the PDIA3-STAT3-MCOLN3-Ca 2+ axis to reactivate the lysosome.
The molecular mechanism by which H. pylori induces peptic ulcers or gastritis cancer is not understood, but it probably involves a combination of host genetic predisposition and bacterial virulence factors (e.g., VacA and CagA proteins) [65]. The vacuolating cytotoxin (VacA) is responsible for several cellular responses, such as cell vacuolization, as well as other processes such as autophagy and necrosis [67]. Foegeding and collaborators [47] inhibited autophagy by using the CRISPR/Cas9-mediated knockout of autophagy-related 16-like 1 (ATG16L1) in HeLa cells. The results showed increased VacA levels or increased vacuolization compared with the control and that the VacA degradation is independent of the autophagic activity. CagA is a virulence factor used for the detection of H. pylori and is considered an important risk factor for severe gastric diseases, including GC. Zhao and coauthors [54] evaluated the effects of integrin receptors and the function of cell adhesion molecule 1 receptors (CEACAM) through the cag-type IV secretion system (cag-T4SS) on the CagA translocation process through a multiple knockout of CEACAM receptors in the GC cell line. The results showed that neither the direct interaction of the components of cag-T4SS with the integrins nor any signaling event mediated by the integrin is necessary for the translocation of CagA. Furthermore, the CRISPR/Cas9 mediated the deletion of miR-30a in H. pylori infected mice, the knockout mice demonstrated that genetic editing did not affect the growth and development of the mice, and little effect was observed on the H. pylori colonization rates of the mice. Increased incidence rates of chronic gastritis, chronic atrophic gastritis, atypical hyperplasia, and other precancerous lesions and manifestations of adenocarcinoma in the antral or gastric mucosa of rats have also been reported. These data demonstrate that miR-30a plays the role of a tumor suppressor in GC [59].
3.5. Chemotherapy Response
From the development of tumor cells to create resistance to chemotherapeutic-induced cell death, the CRISPR tool has been used to discover new therapeutic targets and drugs for the treatment of GC. Wang and colleagues [57] used CRISPR/Cas9 to mediate the knockout of the gasdermin E (GSDME) gene in a GC cell line to assess the effect of 5-fluoracil on the induction of pyroptosis in these cells. The authors found that the GSDME deficiency changed the pyroptosis induced by 5-FU to apoptosis, characterized by shrinkage, fragmentation in apoptotic bodies, and cell death without lysis. The study by Cui and collaborators [61] used the CRISPR/Cas9-mediated knockout of the legumain (AEP) gene to assess the proliferative capacity of these cells in the presence of different chemotherapeutic agents. This gene has previously been shown to be an oncogene related to invasiveness and metastasis in GC. The authors demonstrated that AEP knockout GC cells caused significantly decreased proliferation after treatment with 5-FU, paclitaxel, docetaxel, and T-DM1. These data demonstrate that AEP is a potential therapeutic target for GC.
4. Application of CRISPR/CAS9 in GC Clinical Research
Due to the ease of use that CRISPR/Cas9 has brought to gene editing, the chances of treating diseases previously defined as “incurable” has greatly increased. However, this technology is a challenge in the field of clinical studies related to GC, due to the difficulties in finding a delivery system that is specific enough and capable of targeting only the cells of interest inside a given tissue.
There are currently two clinical trials where CRISPR/Cas9 is being used for the treatment of patients with GC via different approaches. The “Phase I/II Trial in Patients with Metastatic Gastrointestinal Epithelial Cancer Administering Tumor-Infiltrating Lymphocytes in which the Gene Encoding CISH was Inactivated using the CRISPR/Cas9 System” (NCT04426669) is one of the pioneers in this type of study, which is a clinical trial to evaluate the safety and efficacy of genetically modified neoantigen-specific tumor-infiltrating lymphocytes (TILs), in which the intracellular immune checkpoint CISH (cytokine-induced SH2 protein) will be inhibited using CRISPR/Cas9 gene editing for the treatment of gastrointestinal (GI) cancer [68].
Another interesting ongoing clinical trial is “PD-1 Knockout EBV-CTLs for Advanced-Stage Epstein–Barr Virus (EBV)-Associated Malignancies”. This clinical trial seeks to collect peripheral blood lymphocytes from patients with advanced stage Epstein–Barr virus (EBV) GC to generate PD-1 (programmed cell death protein 1) knockout cytotoxic T-lymphocytes (CTL). After the reintroduction of PD-1 knockout EBV-CTL, the patients are expected to show increased GC progression-free survival (PFS) and overall survival (OS) rates [69].
These studies are important for understanding the administration of CRISPR in humans and establishing this technique as a future personalized treatment in patients with GC.
5. Conclusions and Future Perspectives
Over the years, CRISPR technology has given us new perspectives that were previously unattainable in the scientific world. In the context of GC, CRISPR has been an ally in the discovery of new mechanisms and genes that play key roles in this neoplasm. In addition to helping to understand the molecular mechanisms involved in the emergence of GC, CRISPR is a promising tool with the potential to modify specific genes important for gastric carcinogenesis and reverse processes as we have never been able to before. CRISPR technology has proved to be such an advantageous tool, as we can see its potential via in vitro, in vivo, and clinical studies, proving it to be a technology that is applicable for several approaches, including in cancer, but we still have not identified the complete domain of CRISPR, so there is still a lot of work to be done to refine this technology and make it applicable.
Acknowledgments
Figures were created with biorender.com.
Author Contributions
Conception and design, R.S.A., F.W. and M.A.C.S.; writing, review and revision, R.S.A., F.W., B.T.R.K. and M.A.C.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This study was funded by the São Paulo Research Foundation (FAPESP) under grant numbers 2016/25562-0 and 2019/20592-6; the National Council for Scientific and Technological Development (CNPq) under grant number 2018/301127-2; and the Coordination for the Improvement of Higher Education Personnel (CAPES) under grant numbers 23038051640/2009-01 and 88882.430350/2019-01. M.A.C.S. was funded by FAPESP grant number 2016/25562-0; CNPq grant number 2018/301127-2; and CAPES 23038051640/2009-01. B.T.R.K. was funded by FAPESP grant number 2019/20592-6. R.S.A. was funded by CAPES Doctoral Fellowship 88882.430350/2019-01.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 3.Dikken J.L., van de Velde C.J., Coit D.G., Shah M.A., Verheij M., Cats A. Treatment of resectable gastric cancer. Therap. Adv. Gastroenterol. 2012;5:49–69. doi: 10.1177/1756283X11410771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ito S., Ohashi Y., Sasako M. Survival after recurrence in patients with gastric cancer who receive S-1 adjuvant chemotherapy: Exploratory analysis of the ACTS-GC trial. BMC Cancer. 2018;18:449. doi: 10.1186/s12885-018-4341-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Joshi S.S., Badgwell B.D. Current treatment and recent progress in gastric cancer. CA Cancer J. Clin. 2021;71:264–279. doi: 10.3322/caac.21657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matsuoka T., Yashiro M. Biomarkers of gastric cancer: Current topics and future perspective. World J. Gastroenterol. 2018;24:2818–2832. doi: 10.3748/wjg.v24.i26.2818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leal M.F., Wisnieski F., de Oliveira Gigek C., do Santos L.C., Calcagno D.Q., Burbano R.R., Smith M.C. What gastric cancer proteomic studies show about gastric carcinogenesis? Tumour Biol. 2016;37:9991–10010. doi: 10.1007/s13277-016-5043-9. [DOI] [PubMed] [Google Scholar]
- 8.La Russa M.F., Qi L.S. The New State of the Art: Cas9 for Gene Activation and Repression. Mol. Cell. Biol. 2015;35:3800–3809. doi: 10.1128/MCB.00512-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang S.-W., Gao C., Zheng Y.-M., Yi L., Lu J.-C., Huang X.-Y., Cai J.-B., Zhang P.-F., Cui Y.-H., Ke A.-W. Current applications and future perspective of CRISPR/Cas9 gene editing in cancer. Mol. Cancer. 2022;21:57. doi: 10.1186/s12943-022-01518-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim Y.G., Cha J., Chandrasegaran S. Hybrid restriction enzymes: Zinc finger fusions to Fok I cleavage domain. Proc. Natl. Acad. Sci. USA. 1996;93:1156–1160. doi: 10.1073/pnas.93.3.1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christian M., Cermak T., Doyle E.L., Schmidt C., Zhang F., Hummel A., Bogdanove A.J., Voytas D.F. Targeting DNA double-strand breaks with TAL effector nucleases. Genetics. 2010;186:757–761. doi: 10.1534/genetics.110.120717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller J.C., Tan S., Qiao G., Barlow K.A., Wang J., Xia D.F., Meng X., Paschon D.E., Leung E., Hinkley S.J., et al. A TALE nuclease architecture for efficient genome editing. Nat. Biotechnol. 2011;29:143–148. doi: 10.1038/nbt.1755. [DOI] [PubMed] [Google Scholar]
- 13.Carroll D. Genome engineering with zinc-finger nucleases. Genetics. 2011;188:773–782. doi: 10.1534/genetics.111.131433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang W., Marraffini L.A. CRISPR-Cas: New Tools for Genetic Manipulations from Bacterial Immunity Systems. Annu. Rev. Microbiol. 2015;69:209–228. doi: 10.1146/annurev-micro-091014-104441. [DOI] [PubMed] [Google Scholar]
- 15.Zhang H., Qin C., An C., Zheng X., Wen S., Chen W., Liu X., Lv Z., Yang P., Xu W., et al. Application of the CRISPR/Cas9-based gene editing technique in basic research, diagnosis, and therapy of cancer. Mol. Cancer. 2021;20:126. doi: 10.1186/s12943-021-01431-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ishino Y., Shinagawa H., Makino K., Amemura M., Nakata A. Nucleotide sequence of the iap gene, responsible for alkaline phosphatase isozyme conversion in Escherichia coli, and identification of the gene product. J. Bacteriol. 1987;169:5429–5433. doi: 10.1128/jb.169.12.5429-5433.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barrangou R., Fremaux C., Deveau H., Richards M., Boyaval P., Moineau S., Romero D.A., Horvath P. CRISPR provides acquired resistance against viruses in prokaryotes. Science. 2007;315:1709–1712. doi: 10.1126/science.1138140. [DOI] [PubMed] [Google Scholar]
- 18.Bolotin A., Quinquis B., Sorokin A., Ehrlich S.D. Clustered regularly interspaced short palindrome repeats (CRISPRs) have spacers of extrachromosomal origin. Microbiology. 2005;151:2551–2561. doi: 10.1099/mic.0.28048-0. [DOI] [PubMed] [Google Scholar]
- 19.Makarova K.S., Grishin N.V., Shabalina S.A., Wolf Y.I., Koonin E.V. A putative RNA-interference-based immune system in prokaryotes: Computational analysis of the predicted enzymatic machinery, functional analogies with eukaryotic RNAi, and hypothetical mechanisms of action. Biol. Direct. 2006;1:7. doi: 10.1186/1745-6150-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koonin E.V., Makarova K.S. CRISPR-Cas: Evolution of an RNA-based adaptive immunity system in prokaryotes. RNA Biol. 2013;10:679–686. doi: 10.4161/rna.24022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jinek M., Chylinski K., Fonfara I., Hauer M., Doudna J.A., Charpentier E. A programmable dual-RNA-guided DNA endonuclease in adaptive bacterial immunity. Science. 2012;337:816–821. doi: 10.1126/science.1225829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tröder S.E., Zevnik B. History of genome editing: From meganucleases to CRISPR. Lab. Anim. 2022;56:60–68. doi: 10.1177/0023677221994613. [DOI] [PubMed] [Google Scholar]
- 23.Wang T., Wei J.J., Sabatini D.M., Lander E.S. Genetic screens in human cells using the CRISPR-Cas9 system. Science. 2014;343:80–84. doi: 10.1126/science.1246981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pellagatti A., Dolatshad H., Valletta S., Boultwood J. Application of CRISPR/Cas9 genome editing to the study and treatment of disease. Arch. Toxicol. 2015;89:1023–1034. doi: 10.1007/s00204-015-1504-y. [DOI] [PubMed] [Google Scholar]
- 25.Bikard D., Jiang W., Samai P., Hochschild A., Zhang F., Marraffini L.A. Programmable repression and activation of bacterial gene expression using an engineered CRISPR-Cas system. Nucleic Acids Res. 2013;41:7429–7437. doi: 10.1093/nar/gkt520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen B., Gilbert L.A., Cimini B.A., Schnitzbauer J., Zhang W., Li G.W., Park J., Blackburn E.H., Weissman J.S., Qi L.S., et al. Dynamic imaging of genomic loci in living human cells by an optimized CRISPR/Cas system. Cell. 2013;155:1479–1491. doi: 10.1016/j.cell.2013.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hilton I.B., D’Ippolito A.M., Vockley C.M., Thakore P.I., Crawford G.E., Reddy T.E., Gersbach C.A. Epigenome editing by a CRISPR-Cas9-based acetyltransferase activates genes from promoters and enhancers. Nat. Biotechnol. 2015;33:510–517. doi: 10.1038/nbt.3199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Komor A.C., Kim Y.B., Packer M.S., Zuris J.A., Liu D.R. Programmable editing of a target base in genomic DNA without double-stranded DNA cleavage. Nature. 2016;533:420–424. doi: 10.1038/nature17946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jiang F., Taylor D.W., Chen J.S., Kornfeld J.E., Zhou K., Thompson A.J., Nogales E., Doudna J.A. Structures of a CRISPR-Cas9 R-loop complex primed for DNA cleavage. Science. 2016;351:867–871. doi: 10.1126/science.aad8282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jansen R., Embden J.D., Gaastra W., Schouls L.M. Identification of genes that are associated with DNA repeats in prokaryotes. Mol. Microbiol. 2002;43:1565–1575. doi: 10.1046/j.1365-2958.2002.02839.x. [DOI] [PubMed] [Google Scholar]
- 31.Garneau J.E., Dupuis M.È., Villion M., Romero D.A., Barrangou R., Boyaval P., Fremaux C., Horvath P., Magadán A.H., Moineau S. The CRISPR/Cas bacterial immune system cleaves bacteriophage and plasmid DNA. Nature. 2010;468:67–71. doi: 10.1038/nature09523. [DOI] [PubMed] [Google Scholar]
- 32.Cong L., Ran F.A., Cox D., Lin S., Barretto R., Habib N., Hsu P.D., Wu X., Jiang W., Marraffini L.A., et al. Multiplex genome engineering using CRISPR/Cas systems. Science. 2013;339:819–823. doi: 10.1126/science.1231143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu M., Zhang W., Xin C., Yin J., Shang Y., Ai C., Li J., Meng F.L., Hu J. Global detection of DNA repair outcomes induced by CRISPR-Cas9. Nucleic Acids Res. 2021;49:8732–8742. doi: 10.1093/nar/gkab686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Skryabin B.V., Kummerfeld D.M., Gubar L., Seeger B., Kaiser H., Stegemann A., Roth J., Meuth S.G., Pavenstädt H., Sherwood J., et al. Pervasive head-to-tail insertions of DNA templates mask desired CRISPR-Cas9-mediated genome editing events. Sci. Adv. 2020;6:eaax2941. doi: 10.1126/sciadv.aax2941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tao J., Wang Q., Mendez-Dorantes C., Burns K.H., Chiarle R. Frequency and mechanisms of LINE-1 retrotransposon insertions at CRISPR/Cas9 sites. Nat. Commun. 2022;13:3685. doi: 10.1038/s41467-022-31322-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kosicki M., Tomberg K., Bradley A. Repair of double-strand breaks induced by CRISPR-Cas9 leads to large deletions and complex rearrangements. Nat. Biotechnol. 2018;36:765–771. doi: 10.1038/nbt.4192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shibata E., Dutta A. A human cancer cell line initiates DNA replication normally in the absence of ORC5 and ORC2 proteins. J. Biol. Chem. 2020;295:16949–16959. doi: 10.1074/jbc.RA120.015450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qi L.S., Larson M.H., Gilbert L.A., Doudna J.A., Weissman J.S., Arkin A.P., Lim W.A. Repurposing CRISPR as an RNA-guided platform for sequence-specific control of gene expression. Cell. 2013;152:1173–1183. doi: 10.1016/j.cell.2013.02.022. Erratum in Cell 2021, 184, 844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elbashir S.M., Martinez J., Patkaniowska A., Lendeckel W., Tuschl T. Functional anatomy of siRNAs for mediating efficient RNAi in Drosophila melanogaster embryo lysate. EMBO J. 2001;20:6877–6888. doi: 10.1093/emboj/20.23.6877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gilbert L., Larson M.H., Morsut L., Liu Z., Brar G.A., Torres S.E., Stern-Ginossar N., Brandman O., Whitehead E.H., Doudna J.A., et al. CRISPR-mediated modular RNA-guided regulation of transcription in eukaryotes. Cell. 2013;154:442–451. doi: 10.1016/j.cell.2013.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gaudelli N.M., Komor A.C., Rees H.A., Packer M.S., Badran A.H., Bryson D.I., Liu D.R. Programmable base editing of A•T to G•C in genomic DNA without DNA cleavage. Nature. 2017;551:464–471. doi: 10.1038/nature24644. Erratum in Nature 2018, 559, E8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Krishnamurthy M., Kechele D.O., Broda T., Zhang X., Enriquez J.R., McCauley H.A., Sanchez J.G., McCracken K., Palermo J., Bernieh A., et al. Using Human Induced Pluripotent Stem Cell-Derived Organoids to Identify New Pathologies in Patients With PDX1 Mutations. Gastroenterology. 2022;163:1053–1063.e7. doi: 10.1053/j.gastro.2022.06.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Garcia-Bloj B., Moses C., Sgro A., Plani-Lam J., Arooj M., Duffy C., Thiruvengadam S., Sorolla A., Rashwan R., Mancera R.L., et al. Waking up dormant tumor suppressor genes with zinc fingers, TALEs and the CRISPR/dCas9 system. Oncotarget. 2016;7:60535–60554. doi: 10.18632/oncotarget.11142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gannon H.S., Kaplan N., Tsherniak A., Vazquez F., Weir B.A., Hahn W.C., Meyerson M. Identification of an "Exceptional Responder" Cell Line to MEK1 Inhibition: Clinical Implications for MEK-Targeted Therapy. Mol. Cancer Res. 2016;14:207–215. doi: 10.1158/1541-7786.MCR-15-0321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen J., Bell J., Lau B.T., Whittaker T., Stapleton D., Ji H.P. A functional CRISPR/Cas9 screen identifies kinases that modulate FGFR inhibitor response in gastric cancer. Oncogenesis. 2019;8:33. doi: 10.1038/s41389-019-0145-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hu W., Zhang L., Li M.X., Shen J., Liu X.D., Xiao Z.G., Wu D.L., Ho I.H.T., Wu J.C.Y., Cheung C.K.Y., et al. Vitamin D3 activates the autolysosomal degradation function against Helicobacter pylori through the PDIA3 receptor in gastric epithelial cells. Autophagy. 2019;15:707–725. doi: 10.1080/15548627.2018.1557835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Foegeding N.J., Raghunathan K., Campbell A.M., Kim S.W., Lau K.S., Kenworthy A.K., Cover T.L., Ohi M.D. Intracellular Degradation of Helicobacter pylori VacA Toxin as a Determinant of Gastric Epithelial Cell Viability. Infect. Immun. 2019;87:e00783-18. doi: 10.1128/IAI.00783-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang Y.-Q., Pei J.-H., Shi S.-S., Guo X.-S., Cui G.-Y., Li Y.-F., Zhang H.-P., Hu W.-Q. CRISPR/Cas9-mediated knockout of the PDEF gene inhibits migration and invasion of human gastric cancer AGS cells. Biomed. Pharmacother. 2018;111:76–85. doi: 10.1016/j.biopha.2018.12.048. [DOI] [PubMed] [Google Scholar]
- 49.Zhuo W., Liu Y., Li S., Guo D., Sun Q., Jin J., Rao X., Li M., Sun M., Jiang M., et al. Long Noncoding RNA GMAN, Up-regulated in Gastric Cancer Tissues, Is Associated with Metastasis in Patients and Promotes Translation of Ephrin A1 by Competitively Binding GMAN-AS. Gastroenterology. 2019;156:676–691.e11. doi: 10.1053/j.gastro.2018.10.054. [DOI] [PubMed] [Google Scholar]
- 50.Araújo T., Khayat A., Quintana L., Calcagno D., Mourão R., Modesto A., Paiva J., Lima A., Moreira F., Oliveira E., et al. Piwi like RNA-mediated gene silencing 1 gene as a possible major player in gastric cancer. World J. Gastroenterol. 2018;24:5338–5350. doi: 10.3748/wjg.v24.i47.5338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Park Y.S., Lee J.H., Jung D.-B., Kim H.-B., Jung J.-H., Pak S., Ryu Y.-M., Park H.J., Park Y.-Y., Jung H.-Y., et al. MicroRNA-21 induces loss of 15-hydroxyprostaglandin dehydrogenase in early gastric tubular adenocarcinoma. Sci. Rep. 2018;8:17717. doi: 10.1038/s41598-018-36139-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hu L., Bai Z.G., Ma X.M., Bai N., Zhang Z.T. MRFAP1 plays a protective role in neddylation inhibitor MLN4924-mediated gastric cancer cell death. Eur. Rev. Med. Pharmacol. Sci. 2018;22:8273–8280. doi: 10.26355/eurrev_201812_16524. [DOI] [PubMed] [Google Scholar]
- 53.Zhang X., Qian Y., Li F., Bei S., Li M., Feng L. microRNA-9 selectively targets LMX1A to promote gastric cancer cell progression. Biochem. Biophys. Res. Commun. 2018;505:405–412. doi: 10.1016/j.bbrc.2018.09.101. [DOI] [PubMed] [Google Scholar]
- 54.Zhao Q., Busch B., Jiménez-Soto L.F., Ishikawa-Ankerhold H., Massberg S., Terradot L., Fischer W., Haas R. Integrin but not CEACAM receptors are dispensable for Helicobacter pylori CagA translocation. PLoS Pathog. 2018;14:e1007359. doi: 10.1371/journal.ppat.1007359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Deswaerte V., Nguyen P., West A., Browning A.F., Yu L., Ruwanpura S.M., Balic J., Livis T., Girard C., Preaudet A., et al. Inflammasome Adaptor ASC Suppresses Apoptosis of Gastric Cancer Cells by an IL18-Mediated Inflammation-Independent Mechanism. Cancer Res. 2018;78:1293–1307. doi: 10.1158/0008-5472.CAN-17-1887. [DOI] [PubMed] [Google Scholar]
- 56.Liu J., Ben Q., Lu E., He X., Yang X., Ma J., Zhang W., Wang Z., Liu T., Zhang J., et al. Long noncoding RNA PANDAR blocks CDKN1A gene transcription by competitive interaction with p53 protein in gastric cancer. Cell Death Dis. 2018;9:168. doi: 10.1038/s41419-017-0246-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang Y., Yin B., Li D., Wang G., Han X., Sun X. GSDME mediates caspase-3-dependent pyroptosis in gastric cancer. Biochem. Biophys. Res. Commun. 2018;495:1418–1425. doi: 10.1016/j.bbrc.2017.11.156. [DOI] [PubMed] [Google Scholar]
- 58.Lai J., Wang H., Luo Q., Huang S., Lin S., Zheng Y., Chen Q. The relationship between DNA methylation and Reprimo gene expression in gastric cancer cells. Oncotarget. 2017;8:108610–108623. doi: 10.18632/oncotarget.21296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liu X., Ji Q., Zhang C., Liu X., Liu Y., Liu N., Sui H., Zhou L., Wang S., Lihong Z. miR-30a acts as a tumor suppressor by double-targeting COX-2 and BCL9 in H. pylori gastric cancer models. Sci. Rep. 2017;7:7113. doi: 10.1038/s41598-017-07193-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhu M., Yan C., Ren C., Huang X., Zhu X., Gu H., Wang M., Wang S., Gao Y., Ji Y., et al. Exome Array Analysis Identifies Variants in SPOCD1 and BTN3A2 That Affect Risk for Gastric Cancer. Gastroenterology. 2017;152:2011–2021. doi: 10.1053/j.gastro.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 61.Cui Y., Li Q., Li H., Wang Y., Wang H., Chen W., Zhang S., Cao J., Liu T. Asparaginyl endopeptidase improves the resistance of microtubule-targeting drugs in gastric cancer through IQGAP1 modulating the EGFR/JNK/ERK signaling pathway. OncoTargets Ther. 2017;10:627–643. doi: 10.2147/OTT.S125579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yin J., Li Z., Ye L., Birkin E., Li L., Xu R., Chen G., Ji J., Zhang Z., Jiang W., et al. EphB2 represents an independent prognostic marker in patients with gastric cancer and promotes tumour cell aggressiveness. J. Cancer. 2020;11:2778–2787. doi: 10.7150/jca.38098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen W., Ding R., Tang J., Li H., Chen C., Zhang Y., Zhang Q., Zhu X. Knocking Out SST Gene of BGC823 Gastric Cancer Cell by CRISPR/Cas9 Enhances Migration, Invasion and Expression of SEMA5A and KLF2. Cancer Manag. Res. 2020;12:1313–1321. doi: 10.2147/CMAR.S236374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Machlowska J., Baj J., Sitarz M., Maciejewski R., Sitarz R. Gastric Cancer: Epidemiology, Risk Factors, Classification, Genomic Characteristics and Treatment Strategies. Int. J. Mol. Sci. 2020;21:4012. doi: 10.3390/ijms21114012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang F., Meng W., Wang B., Qiao L. Helicobacter pylori-induced gastric inflammation and gastric cancer. Cancer Lett. 2014;345:196–202. doi: 10.1016/j.canlet.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 66.Hooi J.K.Y., Lai W.Y., Ng W.K., Suen M.M.Y., Underwood F.E., Tanyingoh D., Malfertheiner P., Graham D.Y., Wong V.W.S., Wu J.C.Y., et al. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology. 2017;153:420–429. doi: 10.1053/j.gastro.2017.04.022. [DOI] [PubMed] [Google Scholar]
- 67.Foegeding N.J., Caston R.R., McClain M.S., Ohi M.D., Cover T.L. An Overview of Helicobacter pylori VacA Toxin Biology. oxins. 2016;8:173. doi: 10.3390/toxins8060173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Masonic Cancer Center UdM A Study of Metastatic Gastrointestinal Cancers Treated with Tumor Infiltrating Lymphocytes in Which the Gene Encoding the Intracellular Immune Checkpoint CISH Is Inhibited Using CRISPR Genetic Engineering. [(accessed on 31 October 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT04426669?term=CRISPR&cond=Gastric+Cancer&draw=2&rank=1.
- 69.Yang Y. PD-1 Knockout EBV-CTLs for Advanced Stage Epstein-Barr Virus (EBV) Associated Malignancies. [(accessed on 31 October 2022)];2020 Available online: https://clinicaltrials.gov/ct2/show/NCT03044743?term=CRISPR&cond=Gastric+Cancer&draw=2&rank=2.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.