Abstract
Globally, diarrheal diseases and acute respiratory infections are the leading causes of morbidity and mortality in children under 5 years old. The benefits of exclusive breastfeeding in reducing the risk of gastrointestinal and respiratory infections are well documented. Optimal breastfeeding may potentially save the lives of about 800,000 children in low-income settings. Despite the evidence, around 63% of infants from birth to 6 months are not exclusively breastfed worldwide. We searched the literature published between 2010 and 2022 in Medline, Embase, and Scopus on the association between exclusive breastfeeding and infectious diseases. We selected and reviewed 70 relevant studies. Our findings expand and confirm the positive association between exclusive breastfeeding and reduced risk of a number of gastrointestinal, respiratory, and other infections in 60 out of 70 studies observed in both low- and high-income settings. Several studies analyzing exclusive breastfeeding duration reported that a longer exclusive breastfeeding duration is protective against many infectious diseases. This review also reported a lack of standardized definition for measuring exclusive breastfeeding in many studies. Overall, the results highlight the benefits of exclusive breastfeeding in many studies and suggests reporting exclusive breastfeeding in future studies using a consistent definition to enable better monitoring of exclusive breastfeeding rates.
Keywords: exclusive breastfeeding, diarrhea, acute respiratory infection, gastrointestinal infection, respiratory infection
1. Introduction
Infectious diseases are a leading cause of deaths in children below the age of 5 worldwide [1]. The most common infectious diseases affecting young children are diarrhea and acute respiratory infections [1]. Despite enormous efforts in the prevention of diarrheal morbidity and mortality, diarrhea is the second largest cause of mortality among children under 5 years old, and almost 1.7 billion children are experiencing diarrheal occurrences worldwide [2]. Globally, diarrhea leads to 525,000 deaths in children per year [2]. Furthermore, acute respiratory infection (ARI) is responsible for almost 20% of all deaths in children [3,4]. In 2016, almost 653,000 deaths were attributed to lower ARIs in children below 5 years old [3].
Research suggests that exclusive breastfeeding (EBF) is an important protective factor against infant morbidity and mortality from respiratory infections and gastrointestinal tract infections [5]. The World Health Organization (WHO) recommends EBF until the age of 6 months, and then continuation of breastfeeding along with complementary feeding until 2 years or more [6]. The WHO defines EBF as a practice, whereby the baby receives only breast milk in the first 6 months of life with no other foods or liquids, except for medications, vitamin and mineral supplements, and oral rehydration salts [6]. Approximately 11.6% of all deaths in children have been attributed to suboptimum breastfeeding in 2011 [7]. Despite the evidence supporting EBF, about 63% of babies aged less than 6 months in low- and middle-income countries (LMICs) do not receive EBF [8]. EBF has the potential to avert roughly 12% of deaths in children below 5 years old in LMICs [6]. The utilization of breastfeeding promotion programs and policies may be able the save the lives of millions of children, particularly in resource-limited areas where proper child nutrition and readily obtainable pediatric health services are not easily available [5,7]. However, suboptimum breastfeeding is an issue in both LMICs and high-income countries. High-income nations have a shorter breastfeeding duration compared to LMICs [8]. In 2012, the WHO adopted its Comprehensive Implementation Plan on Maternal, Infant, and Young Child Nutrition, which set six targets to lower mortality and mortality associated with nutrition [7]. One of the six objectives was to increase the rates of EBF during the first 6 months of life to 50% by 2025, which signifies the urgent need to address this issue [7,8]. A meta-analysis suggested that since 1993, EBF rates have increased by around 0.5 percentage points annually, reaching 35% in the year 2013 [8]. The meta-analysis indicates that an increase of greater than one percentage point is required every year to reach the target [8].
Thus, the purpose of this review is to critically analyze the published literature on the relationship between EBF and childhood morbidity, as very few studies have reviewed the current literature on EBF and a wide range of infections. The results of this review will build on an existing systematic review of breastfeeding and the risk of diarrhea morbidity in 2011, additionally investigate other infectious diseases such as ARI and provide recommendations for further research in this area [9].
2. Materials and Methods
2.1. Search Strategy
This review was undertaken by searching the following databases: Embase (OVID), Scopus, and Medline (OVID). Keywords and terms utilized in the searches included exclusive breastfeeding, morbidity, diarrhea, acute respiratory infection, fever, cough, and infectious diseases. Appropriate Boolean operators, truncations, and search features such as subject headings were used and adapted according to the database. The search was limited to papers published from January 2010 up to April 2022. Full details of the search strategy can be found in Appendix A.
2.2. Eligibility Criteria
The inclusion and exclusion criteria of studies are shown in Table 1.
Table 1.
Eligibility criteria of reviewed studies.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Studies that measured the association between EBF and childhood morbidity | Child age older than 5 years |
| Child age less than 5 years | Studies on HIV-exposed babies and children (reason: altered immune status of these children) |
| Study outcome of interest was diarrhea, respiratory tract infections, fever, and other infectious diseases | Studies with outcomes such as asthma, rhinitis, COVID-19, allergies, wheezing, gut microbiota, malaria, stunting, underweight, wasting, and mother’s morbidity |
| Published in a peer-reviewed journal | Sample size < 100 |
| Randomized controlled trials, observational studies, and meta-analysis | Case studies/reports, letters, conference abstracts, reviews, and nonhuman studies |
| Written in English language | No measurement of association/effect |
2.3. Selection of Studies
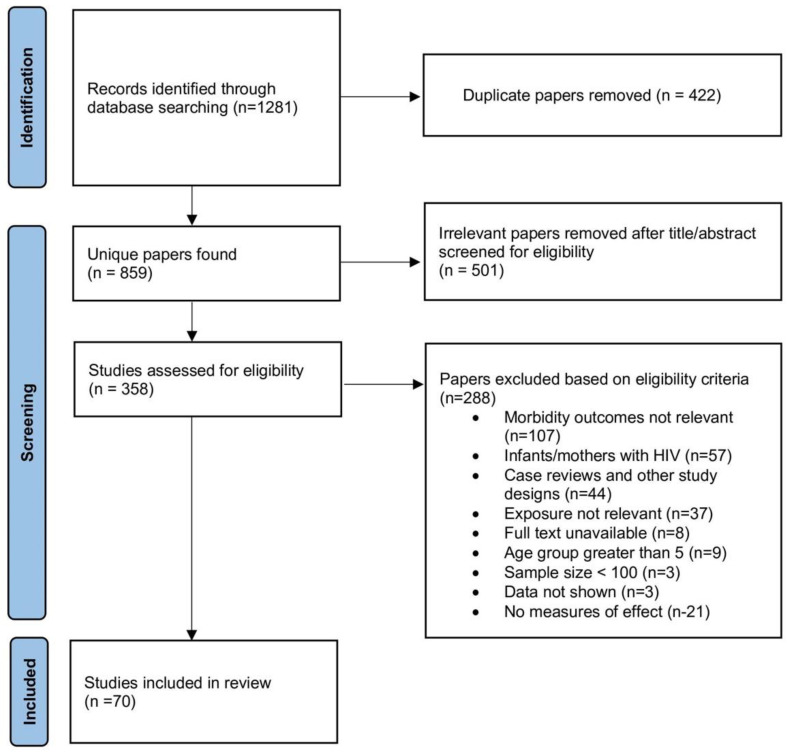
The articles found by using the search strategy were all exported to Endnote X9 for further screening. After duplicates were removed, as shown in Figure 1, a total of 859 studies were retrieved. After reviewing titles and abstracts, 70 papers were included in the review (Table 2). The quality assessment of each study involved an examination of the definitions of EBF and morbidity outcomes, study design, number of participants, and length of recall for the infant feeding practice. Studies were excluded if the children were older than 5 years of age at the time of interview/questionnaire as very long recall periods may result in inaccurate information about breastfeeding status. For example, a cohort study in Thailand involved 322 participants where it was found that children who were EBF for less than 6 months had lower odds of pneumonia [10]. However, the age of subjects ranged from 1 month to 15 years old, leading to a large recall length variability; therefore, they were excluded. A narrative review was conducted rather than a meta-analysis due to the heterogeneity of the definitions of exposures and morbidity outcomes, variability in the study methodologies, differing study settings, and categories of breastfeeding duration. Furthermore, this review assigned EBF status according to each author’s assigned category in the included studies, not the category based on the WHO’s definition of feeding practice, which further makes it unsuitable for a meta-analysis. Studies that provided no definition for EBF and EBF for infants beyond 6 months of age were also included.
Figure 1.
Flow diagram of study selection process.
Table 2.
Summary table of studies investigating the association between EBF and childhood infections arranged according to study design and country type (n = 70).
| Author(s), (year) | Country | Sample Size | Dataset | Exposure Variable | Outcome Variables | Main Results |
|---|---|---|---|---|---|---|
| Meta-analysis | ||||||
| Alamneh et al. (2020) [11] | Ethiopia | 4598 | EBF, during first 6 months | Pneumonia | Non-EBF group had a higher risk of developing pneumonia than EBF group (OR = 2.46; 95% CI 1.35, 4.47). | |
| Bowatte et al. (2015) [12] | Multi-country | 11,349 | EBF, first 6 months | Acute otitis media (AOM) | EBF was associated with lower odds of AOM (OR = 0.57; 95% CI 0.44, 0.75) than ‘ever vs. never’ BF (OR = 0.67; 95% CI 0.56, 0.80) and ‘more vs. less’ BF (OR = 0.67; 95% CI 0.59, 0.76). | |
| Jackson et al. (2013) [13] | Multi-country | n/a | EBF, only breast milk during first 4 months | Acute lower respiratory infections | Lack of EBF was associated with severe acute lower respiratory infection (OR = 2.34; 95% CI 1.42, 3.88) | |
| Khan et al. (2015) [14] | Multi-country | 70,976 | EBF, no definition | Morbidity—diarrhea, ARI, sepsis | Partially breastfed infants had a greater risk of diarrhea (RR = 2.97; 95% CI 1.38, 6.41), sepsis (RR = 3.46; 95% CI 2.41, 4.98), and ARI (RR = 1.69; 95% CI 1.08, 2.63) than EBF group. | |
| Krawczyk et al. (2016) [15] | Multi-country | 3466 | EBF, no definition | Rotavirus infection | EBF decreases risk of rotavirus infection (OR = 0.62; 95% CI 0.48, 0.81). | |
| Shen et al. (2018) [16] | LMICs | 10,811 | EBF, no definition | Rotavirus diarrhea | No significant relationship between case and control group. No correlation between rotavirus and EBF (OR = 0.86; 95% CI 0.63, 1.16). | |
| Cohort studies (developing countries) | ||||||
| Amour et al. (2016) [17] | Nepal, Peru, Pakistan, South Africa, India, Tanzania, Brazil, and Bangladesh | 1892 | MAL-ED study data | EBF, home surveillance twice a week categorized BF on day before as exclusive (no intake of other drinks or foods) | Campylobacter Infection | EBF group had decreased risk of Campylobacter detection than non-EBF group (RR = 0.57; 95% CI 0.47, 0.67) |
| Hanieh et al. (2015) [18] | Vietnam | 1049 | Ha Nam study data | EBF, only breast milk since birth with no other liquids or solids except medications, oral drops, and vitamins (questionnaire) | Diarrhea, pneumonia | EBF at 6 weeks since birth decreased the odds of inpatient admission for diarrhea (OR 0.37; 95% CI 0.15, 0.88) and suspected pneumonia (OR 0.39; 95% CI 0.20, 0.75) |
| Haque et al. (2019) [19] | Nepal, Peru, Pakistan, South Africa, India, Tanzania, Brazil, and Bangladesh | 1715 | MAL-ED birth cohort data | EBF, no definition | Campylobacter infection | Shorter duration of EBF (IRR = 0.98; 95% CI 0.95, 0.99; p = 0.035) was associated with Campylobacter infection. |
| Hassan et al. (2014) [20] | Egypt | 348 | Abu Homos study data | EBF, no definition | Diarrhea- ETEC | EBF decreased the risk of ETEC diarrhea (aRR = 0.51; 95% CI 0.3, 0.7, p < 0.001). |
| Henkle et al. (2013) [21] | Bangladesh | 331 | Mother’s Gift study data | EBF, only breast milk 1 week prior to each weekly assessment (interview) | Respiratory illness with fever | A significant protective effect of EBF was found for respiratory disease (aOR = 0.59; 95% CI 0.45, 0.77) for EBF group compared to non-EBF group. |
| Mansour et al. (2014) [22] | Egypt | 348 | Abu Homos study data | EBF, breast milk a sole source of nutrition (questionnaire) |
ETEC diarrhea- ETEC phenotypes- ST, LT | EBF was associated with a reduction in risk of ST (IRR = 0.47; 95% CI 0.24,0.91) and LT/ST-ETEC related diarrhea (IRR = 0.19; 95% CI 0.05, 0.67). |
| Panda et al. (2014) [23] | India | 696 | South-24 Parganas study data | EBF, no definition (questionnaire) | Rotavirus diarrhea | Non-EBF group less than 6 months of age had greater odds of diarrhea than non-EBF group (OR = 2.07; 95% CI 1.1, 3.82). |
| Richard et al. (2018) [24] | Nepal, Peru, Pakistan, South Africa, India, Tanzania, Brazil, and Bangladesh | 1731 | MAL-ED study data | EBF (questionnaire) | Acute lower respiratory infection, diarrhea | A significant protective effect of EBF during first 6 months was found against diarrhea (RR = 0.39; 95% CI 0.32, 0.49 for 0 to 2 months), (RR = 0.83; 95% CI 0.75, 0.93) and acute lower respiratory infection (RR = 0.81; 95% CI 0.68, 0.98 for 3 to 5 months). |
| Rogawski et al. (2017) [25] | (Stated above) | 2089 | MAL-ED study data | EBF, no definition |
Giardia Infection |
A significant protective effect of EBF was found against Giardia infection (HR = 0.46; 95% CI 0.28, 0.75). |
| Rogawski et al. (2017) [26] | (Stated above) | 2092 | MAL-ED study data | EBF, no definition | Enteroaggregative Escherichia coli (EAEC) infection | A significant protective effect of EBF was found against (EAEC) infection (RR = 0.72; 95% CI 0.65, 0.79). |
| Rogawski et al. (2015) [27] | India | 465 | Vellore slum data |
EBF, WHO definition (home visit data collection) | Diarrhea | In babies who stopped EBF prior to 6 months, antibiotic exposure was associated with higher risk of diarrhea (IRR = 1.48; 95% CI 1.23, 1.78). |
| Cohort studies (developed countries) | ||||||
| Ajetunmobi et al. (2015) [28] | Scotland | 502,948 | Hospital record linkage | EBF, main mode of feeding on day before data collection | Hospitalization due to GI, respiratory tract infections, etc. | Higher risk of hospitalization for upper respiratory tract (HR = 1.28; 95% CI 1.17, 1.40), lower respiratory tract (HR = 1.50; 95% CI 1.41–1.59), and GI infections (HR = 1.59; 95% CI 1.47, 1.73) among formula-fed babies relative to EBF-group. |
| Annamalay et al. (2012) [29] | Australia | 167 | The Kalgoorlie Otitis Media research Project (KOMrP) data | EBF at 6 to 8 weeks postpartum (Interview) |
Human rhinovirus infection | In non-Aboriginal babies, EBF was associated with a higher risk of HRV-a detection (OR = 3.08; 95% CI 1.09, 8.76). |
| Christensen et al. (2020) [30] | Denmark | 815 | Odense Child Cohort (OCC) data | EBF (WHO definition) (questionnaire) | Infections | Increased duration of EBF was associated with a decreased rate of hospitalization due to any infection (IRR: 0.88; 95% CI 0.80, 0.96; p = 0.006). |
| Diallo et al. (2020) [31] | USA | 1172 | Infant Feeding Practices Study II (IFPS II) data | EBF, only breast milk at every infant feeding session, without other foods (questionnaire) | Diarrhea | When compared to babies who got EBF for 3 months, the odds of diarrhea between 7–12 months greater in babies who discontinued EBF prior to 3 months (OR = 1.15; 95% CI 1.08, 1.22). |
| Duijts et al. (2010) [32] | Netherlands | 7116 | Generation R Study data |
EBF, only breast milk and no other solids, fluids, or milk (questionnaire) | GI, upper respiratory and lower respiratory infections | Babies who were EBF until 4 months of age and partially subsequently had reduced risk of GI (OR = 0.41; 95% CI 0.26, 0.64), upper respiratory (OR = 0.65; 95% CI 0.51, 0.83) and lower respiratory infections (OR = 0.50; 95% CI 0.32, 0.79) till 6 months of age than babies not breastfed. |
| Frank et al. (2019) [33] | USA, Germany, Finland, and Sweden | 6861 | The Environmental Determinants of Diabetes in the Young (TEDDY) data |
EBF, only breast milk with no other foods or formula before enrollment (questionnaire) | GI, respiratory infection, otitis media | The odds of respiratory infection (OR = 0.72; 95% CI 0.60, 0.87), GI infection OR = 0.45; 95% CI 0.32, 0.62), and otitis media (OR = 0.64; 95% CI 0.49, 0.84) were decreased among EBF-group compared to non-EBF group. |
| Gomez-Acebo et al. (2021) [34] | Spain | 969 | Marques de Valdecilla University Hospital data | EBF (WHO Definition) (feeding type at hospital discharge from medical records) | Bronchiolitis | EBF decreased the number of bronchiolitis episodes by 41% (IR = 0.59; 95% CI 0.46, 0.76) compared to infant formula. |
| Kawai et al. (2011) [35] | Japan | 1796 | Fukushima City data | EBF, no definition (questionnaire) | Lower respiratory tract infections | Girls who were EBF for a longer duration had a lower risk of lower respiratory infections hospitalization (HR = 0.45; 95% CI 0.19, 1.04 for 3 to 4 months) (HR = 0.38; 95% CI 0.15, 0.97 for >5 months). |
| Ladomenou et al. (2010) [36] | Greece | 926 | Crete study data | EBF, only breast milk with no other liquids, water and solids (questionnaire) | AOM, ARI | Babies who were EBF for 6 months had lower risk of AOM (OR = 0.37; 95% CI 0.13, 1.05) and ARI (OR = 0.58; 95% CI 0.36, 0.92) compared to babies not breastfed or partially breastfed. |
| Langer et al. (2022) [37] | Germany | 782 | LoewenKIDS study data | Duration of EBF, no definition (questionnaire) | ARI | EBF for less than 4 months is associated with a decreased risk of ARI compared to EBF for 4 to 6 months (RR = 0.78; 95% CI 0.69, 0.89). |
| Nakamura et al. (2020) [38] | Japan | 31 578 | Longitudinal Survey of Babies data | EBF, breast milk and no formula milk (with or without other foods or fluids) (survey) |
Hospitalization due to GI infection | Late preterm babies who were EBF (OR = 1.13; 95% CI 0.36, 3.61) had lower risk of GI infection hospitalization compared to late preterm babies who were not EBF (wide CI). |
| Quigley et al. (2016) [39] | UK | 15,809 | Millennium Cohort Study data | EBF, no definition Pre-2001 WHO policy (EBF for 4–6 months, given solids without formula prior to 6 months, continuing BF at 6 months) |
Diarrhea, chest infection | Babies who were EBF for less than 4 months had a greater risk of diarrhea (RR = 1.42; 95% CI 1.06, 1.92) and chest infection (RR = 1.24; 95% CI 1.05, 1.45) than pre-2001 WHO policy babies. |
| Rosas-Salazar et al. (2022) [40] | USA | 1949 | INSPIRE study data | EBF, no definition (parental report) | Lower respiratory tract infection | A significant protective effect of EBF was found against lower respiratory tract infection (OR = 0.95; 95% CI 0.91, 0.99 for each 1 month of EBF) |
| Videholm et al. (2021) [41] | Sweden | 37,825 | Uppsala County data | EBF, WHO definition (Child Healthcare Quality database) | Respiratory, enteric infection | Non-EBF group had a greater risk of respiratory infections (IRR = 2.53; 95% CI 1.51, 4.24) and enteric infections (IRR = 3.32; 95% CI 2.14, 5.14) than babies who were EBF for 6 months or more. |
| Case–control studies (developing countries) | ||||||
| Baye et al. (2021) [42] | Ethiopia | 357 | Dessie city study data | EBF (recall period > 2 weeks before survey) | Acute diarrhea | The odds of acute diarrhea in non-EBF group during the first 6 months were higher EBF group (OR = 2.12; 95% CI 1.15, 3.70). |
| Delelegn et al. (2020) [43] | Ethiopia | 306 | Dessie referral hospital data | EBF (no definition) (questionnaire) | Acute diarrhea | Non-EBF group were more likely to experience acute diarrhea relative to EBF group (AOR = 3.32; 95% CI 1.206, 9.14). |
| Fahdiyani et al. (2016) [44] | Indonesia | 165 | Tamansari primary health care data | EBF, only breast milk during first 6 months or infant’s age during questionnaire if < 6 months | Upper respiratory tract infection (URI) | EBF was not associated with URI (OR = 0.76; 95% CI 0.38, 1.50, p = 0.425). |
| Lin et al. (2014) [45] | China | 937 | Guangdong Province study data | EBF, no foods or any other liquids and formula milk with exception of vitamins, minerals, and medication during first 6 months (questionnaire) | Hand, foot, and mouth disease (HFMD) | EBF was associated with decreased odds of HFMD (OR = 0.60; 95% CI 0.45, 0.79) compared to mixed feeding. |
| Mir et al. (2022) [46] | Pakistan | 3213 | Taluka Kotri study data |
EBF, no definition (questionnaire) | ARI | Infants who were EBF during the first 6 months had lower odds of ARI compared to non-EBF group (OR = 0.81; 95% CI 0.69, 0.96). |
| Nascimento et al. [47] | Brazil | 267 | Metropolitan Region of Recife (RMR) data | EBF, no definition (medical records) | Pertussis-like illness | Significant protective effect of EBF during first 6 months found against pertussis-like illness (OR = 0.26; 95% CI 0.11, 0.62) |
| Ngocho et al. (2019) [48] | Tanzania | 463 | Tanzania health centers data | EBF, WHO definition (interview) | Community-acquired pneumonia | Lack of EBF during the first 6 months was associated with higher risk of pneumonia (OR = 1.7; 95% CI 1.0, 2.9) |
| Rustam et al. (2019) [49] | Indonesia | 324 | Kampar District primary health care data | EBF, no definition (questionnaire) | Upper respiratory infection | Non-EBF group had increased odds of upper respiratory infection EBF group (OR = 1.69; 95% CI 1.02, 2.80). |
| Sutriana et al. (2021) [50] | Indonesia | 176 | Bojonegoro Regency health center data |
EBF, during 0 to 6 months, no definition (questionnaire) | Pneumonia | Non-EBF group had increased odds of pneumonia than EBF group (OR = 7.95; 95% CI 3.52, 17.94). |
| Yadav et al. (2013) [51] | Nepal | 200 | College of Medical Sciences Teaching Hospital data | EBF, no definition (recorded in proforma) | ARI | Difference between ARI in case and control group for EBF is not statistically significantly different (OR = 1.33; 95% CI 0.73, 2.44; p = 0.36). |
| Case–control studies (developed countries) | ||||||
| Pandolfi et al. (2017) [52] | Italy | 296 | Italian pediatric hospital data | EBF, no definition (questionnaire) | Pertussis | EBF was not statistically significantly associated with pertussis compared to partial BF and artificial feeding (OR = 1.2; 95% CI 0.31, 4.67; p = 0.779) |
| Cross-sectional studies (developing countries) | ||||||
| Abdulla et al. (2022) [53] | Bangladesh | 5724 | BDHS data | EBF (babies currently breastfed and no complementary foods) 24 h recall | Diarrhea, ARI, combination | Non-EBF group had higher risk of diarrhea (OR = 2.11; 95% CI 1.56, 2.85), acute respiratory infection (OR = 1.43; 95% CI 1.28, 1.60) or both (OR = 1.48; 95% CI 1.32, 1.66) compared to EBF group. |
| Adhiningsih et al. (2020) [54] | Indonesia | 116 | Primary health care records and standard questionnaire | History of EBF | Rotavirus infection | EBF group were less likely to have rotavirus diarrhea (OR = 0.67; 95% CI 0.26, 1.75) when compared to non-EBF group (Not statistically significantly different (p > 0.05)). |
| Ahmed et al. (2020) [55] | Ethiopia | 15,106 | EDHS data | EBF (24 h recall) | Diarrhea, ARI | EBF group were lower odds of diarrhea (OR = 0.51; 95% CI 0.39, 0.65). EBF group had lower odds of ARI (OR = 0.65; 95% CI 0.51, 0.83) |
| Cai et al. (2016) [56] | China | 1654 | Maternal Infant Nutrition and Growth (MING) study | EBF, breast milk as sole source of milk, with or without water, supplements, medication and food since birth (questionnaire) | Diarrhea, respiratory (bronchitis, cold, pneumonia) | Compared to EBF group, exclusive formula-feeding group had higher odds of respiratory illness (AOR = 1.44; 95% CI 1.04, 2.00). Compared to EBF group, mixed feeding group had higher odds of diarrhea (OR = 1.40; 95% CI 1.00, 1.96). |
| Dagvadorj et al. (2016) [57] | Mongolia | 1083 | Bulgan hospital data | EBF (no definition) (questionnaire) | Lower respiratory tract infection (LRTI) | EBF for >4 months was found to be a negative predictor of children’s hospitalization for LRTI (AOR = 0.43; 95% CI 0.24, 0.74). |
| Dairo et al. (2017) [58] | Nigeria | 630 | Primary health care centre data | EBF (no definition) |
Diarrhea | Compared to EBF group, babies who got partial BF (OR = 4.59; CI 3.20, 6.99) and predominant BF (OR = 2.78; CI 1.79, 4.29) had higher odds of diarrhea. |
| Demissie et al. (2021) [59] | Ethiopia | 414 | Wolaita Sodo University Teaching and Referral Hospital data | EBF, only breast milk for first 6 months or only breast milk until assessment time for babies aged < 6 months. (questionnaire) | Acute lower respiratory tract infection | Non-EBF group more likely to experience acute lower respiratory tract infections relative to EBF group (AOR = 1.85; 95 % CI 1.18, 2.91, p = 0.008). |
| Dhami et al. (2020) [60] | India | 90,596 | National Family Health Survey (NFHS-4)/India (DHS) | EBF (WHO definition) (24 h recall survey) | Diarrhea | EBF group aged 0–5 months had a lower risk of diarrhea in areas of North, East, and Central India, as well as nationally (AOR = 0.64; 95% CI 0.57, 0.72) compared to their counterparts. |
| Flores et al. (2021) [61] | Peru | 279 | The Parent Study data | EBF (WHO definition) (questionnaire) |
Tuberculosis | Children who were EBF for 6 months had a greater prevalence (PR = 1.6; 95% CI = 0.9, 2.7) of active tuberculosis compared to non-EBF group (not statistically significantly different (p > 0.05). |
| Gizaw et al. (2017) [62] | Ethiopia | 367 | Hadaleala district study data |
EBF, no definition (questionnaire) | Diarrhea | Odds of diarrhea was higher in infants aged <6 months and infants aged 6 to 24 months in non-EBF group during first 6 months (AOR = 13.33; 95% CI 1.59, 112.12) (AOR = 19.24; 95% CI 8.26, 44.82) compared to EBF group. |
| Hajeebhoy et al. (2014) [63] | Vietnam | 6068 | Alive & Thrive (A&T) program data | EBF (WHO definition) 24 h recall questionnaire) | Diarrhea, ARI | Compared to EBF group, babies predominantly (AOR = 1.52; 95% CI 1.05, 2.21) and partially breastfed (AOR = 1.55; 95% CI 1.07, 2.24) had higher odds of diarrhea. Compared to EBF group, babies partially breastfed (AOR = 1.24; 95% CI 1.03, 1.48) had higher odds of ARI. |
| Issa et al. (2019) [64] | Lebanon | 222 | Beirut study data | EBF (WHO definition) (questionnaire) | Urinary tract infection (UTI) | Infants who were EBF for a longer duration had lower odds of UTIs compared to infants who were not EBF for a longer duration (OR = 0.77; 95% CI 0.63, 0.95). |
| Kembo et al. (2011) [65] | Zimbabwe | 3220 | ZDHS data | EBF (24 h recall survey) | Diarrhea | EBF group had a lower risk of diarrhea compared to non-EBF group (OR = 0.27; 95% CI 0.09, 0.74) |
| Khan et al. (2017) [66] | Bangladesh | 1918 | BDHS data | EBF (24 h recall survey) | ARI, diarrhea, fever | Odds of having diarrhea, ARI, and fever was greater if EBF was discontinued during 0 to 2 months (OR = 4.94; 95% CI 3.17, 10.23) (OR = 2.38; 95% CI 1.27, 3.26) (OR = 2.18; 95% CI 1.56, 3.04), 2 to 4 months (OR = 3.07; 95% CI 2.11, 5.03) (OR = 1.40; 95% CI 1.10, 1.76) (OR = 1.53; 95% CI 1.37, 2.10), and 4 to 6 months (OR = 2.30; 95% CI 1.89, 3.20) (OR = 1.19; 95% CI 1.04, 1.57) (OR = 1.23; 95% CI 1.06, 1.63) compared to infants who did not stop EBF up to 6 months. |
| Mulatu et al. (2021) [67] | Ethiopia | 1034 | EDHS data | EBF (24 h recall survey) | Diarrhea, fever | EBF group had reduced odds of diarrhea (OR = 0.33; 95% CI 0.13, 0.83) and fever (OR = 0.34; 95% CI 0.16, 0.75) relative to non-EBF group. |
| Mulatya et al. (2020) [68] | Kenya | 20,964 | KDHS data | EBF (24 h recall survey) | Diarrhea, ARI comorbidity | EBF did not have significant association with diarrhea and ARI comorbidity (OR = 2.73; 95% CI 0.80, 9.28; p = 0.107) |
| Nigatu et al. (2019) [69] | Ethiopia | 2433 | EDHS data | EBF, only breast milk in the 24 h before questionnaire | ARI, diarrhea, fever | Stopping EBF at 3 months (OR = 1.95; 95% CI 1.08, 3.53) and 4–6 months (OR = 3.5; 95% CI 2.19, 5.83) raised the odds of diarrhea compared to infants who were EBF for 6 months. Stopping EBF at 4–6 months raised the odds of ARI (OR = 2.74; 95% CI 1.61, 4.65) and fever (OR = 1.73; 95% CI 1.11, 2.68). |
| Ogbo et al. (2017) [70] | Uganda, Burkina Faso, Ethiopia, Mali, Nigeria, DR Congo, Tanzania, Niger, and Kenya | 83,100 | DHS data | EBF (aged 0–5 months), only breast milk (medicines, vitamins, ORS acceptable) | Diarrhea | EBF was associated with decreased risk of diarrhea (OR = 0.50; 95% CI 0.43, 0.57). |
| Ogbo et al. (2018) [71] | Tanzania | 10,139 | TDHS data | EBF (aged 0–5 months), only breast milk (medicines, vitamins, ORS acceptable) | Diarrhea | EBF group had reduced odds of diarrhea compared to non-EBF group (OR = 0.31; 95% CI 0.16, 0.59). |
| Ogbo et al. (2016) [72] | Nigeria | 88,152 | NDHS data | EBF (aged 0–5 months), only breast milk (medicines, vitamins, ORS acceptable) | Diarrhea | BEBF group had reduced odds of diarrhea compared to non-EBF group (RR = 0.61; 95% CI 0.44, 0.86). |
| Puspitasari et al. (2021) [73] | Indonesia | 16,555 | IDHS data | EBF (aged 0–6 months), with no complimentary foods | ARI | EBF group had reduced odds of ARI compared to non-EBF group (OR = 0.85; 95% CI 0.73, 0.99). |
| Saeed et al. (2020) [74] | Pakistan | 1033 | PDHS data | EBF (survey) | ARI, diarrhea, fever | EBF group had reduced odds of ARI (OR = 0.53; 95% CI 0.32, 0.90), fever (OR = 0.72; 95% CI 0.52, 0.99), and diarrhea (OR = 0.66; 95% CI 0.45, 0.98). |
| Santos et al. (2016) [75] | Brazil | 854 | Family Health Strategy data |
EBF, only breast milk, WHO definition (interview) | Diarrhea | Babies aged <6 months who were EBF had lower odds of diarrhea than babies who were mixed BF (OR = 10.8; 95% CI 2.3, 49.6) and complementary BF (OR = 14.1; 95% CI 3.3, 60.3). |
| Shumetie et al. (2018) [76] | Ethiopia | 553 | Bahir Dar study data | EBF, no definition (questionnaire) | Diarrhea | Non-EBF group had increased odds of diarrhea compared to EBF group (OR = 2.69; 95% CI 1.39, 5.19). |
| Srivastava et al. (2020) [77] | India | 94,144 | (NFHS-4) data | EBF, only breast milk (medication, vitamins, ORS, minerals acceptable) (aged 0–5 months) | Diarrhea, ARI | EBF group had reduced odds of diarrhea (OR = 0.78; 95% CI 0.72, 0.84; p < 0.01) and ARI (OR = 0.99; 95% CI 0.85, 1.15) than non-EBF group (result for ARI statistically significantly different (p > 0.1)). |
| Wibowo et al. (2021) [78] | Indonesia | 13,921 | IDHS data | EBF, no definition (questionnaire) | Diarrhea | EBF group were more likely to not experience diarrhea than non-EBF group (OR = 1.71; 95% CI 1.29, 1.07). |
| Cross-sectional studies (developed countries) | ||||||
| Alexandrino et al. (2016) [79] | Portugal | 152 | Porto day care center data | EBF (no definition) | Lower respiratory tract infection | Risk of lower respiratory tract infection was greater in non-EBF group compared to EBF group (OR = 24.61; 95% CI 1.11, 546.53). |
| Payne et al. (2017) [80] | UK | 30,760 | Infant Feeding Survey (IFS) data | EBF, WHO definition (questionnaire) | Hospitalization for infectious causes | Among babies breastfed at least 6 months, those who were EBF for 6 weeks or more had a lower risk for infectious causes (IR = 0.48; 95% CI 0.32, 0.72) compared to those not EBF for 6 weeks (IR = 0.72; 95% CI 0.48, 1.08). |
ARI—acute respiratory infection; BF—breastfeeding; CI—confidence interval; DHS—demographic health survey; ETEC—enterotoxigenic Escherichia coli; GI—gastrointestinal; HR—hazard ratio; ORS—oral rehydration solution; OR—odds ratio; PR—prevalence ratio; RR—risk ratio.
3. Results
3.1. Study Characteristics
Among the 70 included studies, there were six meta-analyses, 28 cross-sectional studies, 25 cohort studies, and 11 case–control studies, as detailed in Table 2. The sample size for each of the studies ranged from 116 to 502,948 participants. Data from these studies were mostly collected in developing countries (49 out of 70). A total of 42 out of the 49 identified studies in developing countries found that EBF was associated with a significant reduced risk of infection. A total of 14 out of the 17 papers in high-income countries reported decreased infectious disease risk in the EBF group. All four studies conducted in both LMICs and high-income countries (multi-country) indicated lower infection risk in the EBF group. Almost all studies that analyzed the duration of EBF reported the protective effects of a longer EBF duration. A total of 16 studies used the WHO definition of EBF for describing the explanatory variable, and two studies provided a slight variant of the WHO definition of EBF [56,75]. A total of 32 studies provided no specific definition for EBF. In terms of the methods of reporting EBF, 17 papers utilized the 24 h recall measure, and some papers used weekly or twice a week home visits, 2 week recall, and recall since birth measures. Most of the studies utilized self-administered questionnaires or surveys to measure EBF practices.
3.2. Diarrhea and Other Related Gastrointestinal Infections
Out of the 28 studies that included diarrhea as the outcome variable, nearly all studies (n = 27; one meta-analysis, 19 cross-sectional, five cohort, and two case–control studies) found a statistically significant decrease in the risk of diarrhea in children who were EBF [14,18,24,27,31,39,42,43,53,55,56,58,60,62,63,65,66,67,69,70,71,72,74,75,76,77,78]. Only one paper did not find a statistically significant association, and this analysis looked at diarrhea and ARI comorbidity [68]. Of the four studies with rotavirus as an outcome, two studies found a reduction in rotavirus infection and rotavirus diarrhea in children who were EBF, and two studies found no significant relationship [15,16,23,54]. All 11 papers that investigated ETEC (n = 2), EAEC (n = 1), giardia (n = 1), Campylobacter infections (n = 2), GI infections (n = 4), and enteric infections (n = 1) reported the protective effects of EBF [17,19,20,22,25,26,28,32,33,38,41].
3.3. ARI and Other Respiratory Infections
A total of 17 articles examined the relationship between ARI/acute lower respiratory infections and EBF, of which the majority of the articles noted a decrease in ARI in the EBF group (n = 13) [13,14,24,36,46,53,55,59,63,69,73,74]. A total of three papers found no significant relationship between EBF and ARI [50,68,77]. One paper from Germany reported that a longer duration of EBF led to a higher risk of ARI [37]. All studies assessing lower respiratory tract infections (n = 6), pneumonia (n = 5), bronchiolitis (n = 1), and broad respiratory/chest infections (n = 5) reported a protective association with EBF [11,18,21,28,32,33,34,35,39,40,41,48,49,50,56,57,79]. A few studies found that there was no significant association between EBF and tuberculosis (n = 1), upper respiratory tract infection (n = 1), and pertussis (n = 1) [44,52,61]. Three studies examining upper respiratory tract infection and pertussis found EBF as a protective factor [28,32,47]. One publication of a study conducted in Australia reported that EBF lead to increased risk of human rhinovirus infection; however, the sample size (n = 167) was small [29].
3.4. Fever and Infections
All papers that analyzed fever as the outcome factor reported a decrease in the risk of fever in children who were EBF (n = 5; 4 cross-sectional, 1 cohort) [21,66,67,69,74]. All articles that examined urinary tract infection (n = 1), sepsis (n = 1), acute otitis media (n = 3), HFMD infection (n = 1), and broad category of infections (n = 2) reported a reduced risk of these conditions in children who were EBF [12,14,30,33,36,45,64,80].
4. Discussion
4.1. Main Findings
This review updates and confirms the strong protective effects of EBF against childhood morbidity, which reaffirms the previous systematic reviews published by Lamberti et al. [9,81] and others [5,82,83]. It further expands upon the evidence base established by Lamberti et al. [9,81], who predominantly looked at diarrhea and pneumonia. This review highlights the beneficial association between EBF and the decreased risk of a larger number of gastrointestinal, respiratory, and other infections in both LMICs and high-income countries. Only 10 of these 70 studies found either no significant association or an increased risk of infections due to EBF. However, most of these results may be attributed to their small sample size of fewer than 300 participants [29,44,51,52,54,61]. Almost all studies in this review that looked at diarrhea and other gastrointestinal infections suggested the protective effects of EBF, which is in agreement with the paper by Lamberti et al. [9], where diarrhea mortality was greater in infants who were not breastfed relative to those who were EBF (RR = 10.52). In addition, most of the identified papers that examined the duration of EBF found that babies who were EBF for a longer duration experienced lower morbidity from many infectious diseases such as UTI, expanding on the review by Kramer et al. [5] that only noted its impact on gastrointestinal infections.
Another important finding from our review was the use of inconsistent definition for EBF. For instance, a study in Japan defined EBF as the infant’s consumption of breast milk as the only source of milk but may or may not include other foods and liquids [38]. There is a dearth of literature discussing the large variations in definitions of EBF used. Khanal et al. [84] and Binns et al. [85] reported this discrepancy in definition used to measure EBF in studies in Nepal and Australia. A few studies included in our review claimed to adopt the WHO definition of EBF; however, it was noted that the definition was not used accurately [56,75,85]. Consistency in the definition of EBF is crucial to appropriately detect and compare the changes and trends in EBF prevalence over time, across countries and within countries for development and progress of public health policies and interventions [84,86]. Additionally, there was also some variation in the definitions of morbidity outcomes. For example, Diallo et al. [31] in USA defined diarrhea as experiencing at least one episode of diarrhea, whereas the DHS studies defined this as three or more episodes of diarrhea per day [70]. Furthermore, surveys and questionnaires given to participating mothers was the most common measurement tool for collecting information on breastfeeding practices.
This review supports the current WHO recommendation of EBF for the first six months of life. Breastfeeding is influenced by sociocultural and economic factors, maternal factors such as age, education, work environment, birth, and postpartum circumstances, and perspectives on EBF; hence, initiatives must be taken according to the context of LMIC or high-income setting [83,87]. Breastfeeding requires support from families, communities, healthcare professionals, and the government; mothers are not responsible for this alone [74]. Sufficient breastfeeding counseling, lactation centers, education programs for both mothers and healthcare staff and other effective and integrated health policy interventions are vital for mothers in order to initiate and sustain optimal EBF practice [83].
4.2. Biological Plausibility
Numerous components in breast milk provide the biological basis that may explain its protective effects against gastrointestinal and respiratory diseases. It contains several bioactive elements that add to its total immunological activity, including antibodies such as immunoglobulin A (IgA), prebiotic oligosaccharides, lactoferrin, nonspecific anti-infective agents, lymphocytes, leucocytes, probiotics, and other immune cells and beneficial microbes [87,88]. Some of these beneficial components such as secretory antibodies, oligosaccharides, hormones, stem cells, enzymes, and immune cells are not present in formula milk [89]. Compared to formula milk, human milk also has a dynamic composition that varies over time to accommodate to the changing needs of the developing infant [89]. These elements offer the mechanism for infection prevention, especially during the first few months of life and during the breastfeeding phase [87,88]. Research shows that IgA stops the attachment of viruses and bacteria to the mucosal epithelial cells, which might lead to infections [88,89]. IgA antibodies defend against microbes that cause gastrointestinal infections such as Giardia, ETEC, and campylobacter [88,89]. Lactoferrin works as an antimicrobial agent, killing pathogens [88]. Oligosaccharides may block the attachment of pathogens such as pneumococci to the mucous membrane, thereby hindering the formation of respiratory and gastrointestinal infections [88,89]. Moreover, there is a possibility that breastmilk may cover the nasopharyngeal mucosa, thus safeguarding against the transmission of pathogens that cause respiratory diseases [90,91].
Another explanation is that babies who are not breastfed are more exposed to diarrheal-causing pathogens through feeding bottles, nonhuman milk, or other given foods to them, which prevents babies from receiving sufficient nutrition and, therefore, nonspecific immunity [84,92]. For instance, a study reported that typical weaning foods were infected with microbials that might induce gastrointestinal diseases in Gambian babies [92].
There is also evidence that breastfeeding may reduce the risk of sudden infant death syndrome (SIDS) with plausible biological mechanisms for this effect [93,94]. Cytokines and immunoglobulins may safeguard babies during the period when SIDS risk is greatest (2–4 months of age) [94]. Many babies who died from SIDS had a mild infection in the days before death; however, this is insufficient to account for the deaths [94]. It is probable that these infections may produce proinflammatory cytokines that could result in complications [94].
4.3. Strengths and Limitations
The current review was limited as we did not examine randomized controlled trials which would have provided high-quality evidence on the association between EBF and morbidity [87]. It is unethical to randomly assign infants to EBF; therefore, observational studies and reviews were examined [87]. However, it is ethically appropriate to promote EBF in communities compared to providing no EBF promotion [95]. For instance, in Bangladesh, the Shishu Pushti trial randomly allocated pregnant women to peer counseling for infant feeding practices (intervention) or to the control group [96]. Furthermore, most of the studies in this review did not account for reverse causality bias; that is, EBF might have been stopped or changed due to an occurrence of ARI, gastrointestinal, or other morbidity outcomes [9]. This may result in an overestimation of the protective effects of EBF against morbidity since the prevalence of EBF is underestimated in infants who develop the morbidity outcome [95]. Another limitation is that some of the studies in this review did not adjust for confounding factors such as poverty and maternal education [95]. Poverty has been associated with prolonged breastfeeding duration in LMICs; therefore, this may result in an inaccurate estimation of the protective effect of EBF [9,95]. Self-selecting mothers who breastfed for a greater duration may also have led to bias, especially in high-income countries, where breastfeeding mothers are more likely to be educated and health-conscious [95]. This review may also be limited by some studies with a longer length of recall, where mothers who breastfed for a shorter time may be more likely to overestimate EBF duration resulting in the possibility of misclassification. [95] Nevertheless, a major strength is that we carried out an inclusive and comprehensive approach to include a large number of studies with a wide geographic diversity from both LMICs and high-income countries, which makes it more generalizable to different populations.
5. Conclusions
Overall, our review confirms the results of previous reviews on the beneficial association between EBF and reduced childhood morbidity including gastrointestinal, respiratory, and other infections and fever in both LMICs and high-income countries. The measurement of EBF using a standardized and strict terminology is also critical in future research studies for reporting EBF levels and precisely comprehending the health benefits [84,86].
Acknowledgments
Not applicable.
Appendix A
Table A1.
Search strategy history.
| Database | Search Strategy History | Results |
|---|---|---|
| Medline via Ovid | 1. Breast Feeding/ 2. exclusive.tw. 3. 1 and 2 4. Morbidity/ 5. exp Respiratory Tract Infections/ 6. Otitis/ 7. Fever/ 8. Communicable Diseases/ 9. Diarrhea, Infantile/or Diarrhea/or diarrh?ea.tw. 10. Cough/ 11. 4 or 5 or 6 or 7 or 8 or 9 or 10 12. 3 and 11 13. limit 12 to (english language and yr = “2010-Current”) |
169 |
| Embase via Ovid | 1. Breast Feeding/ 2. exclusive.tw. 3. 1 and 2 4. Morbidity/ 5. exp Respiratory Tract Infections/ 6. Otitis/ 7. Fever/ 8. Communicable Diseases/ 9. Diarrhea, Infantile/or Diarrhea/or diarrh?ea.tw. 10. Cough/ 11. 4 or 5 or 6 or 7 or 8 or 9 or 10 12. 3 and 11 13. limit 12 to (english language and yr = “2010–Current”) 14. limit 13 to conference abstract 15. 13 not 14 |
340 |
| Scopus | (TITLE-ABS-KEY(“exclusive breast*”) AND TITLE-ABS-KEY(morbid* OR diarrh*ea OR “respiratory tract infection*” OR “infectious disease*” or “ear infection*” or fever or cough OR “acute respiratory infection*”)) AND PUBYEAR > 2009 AND (LIMIT-TO (LANGUAGE,”English”)) |
771 |
Author Contributions
Conceptualization, S.M.; methodology, S.M. and S.H.; validation, S.M.; formal analysis, S.H.; literature search, S.H.; writing—original draft preparation, S.H.; writing—review and editing, S.M.; supervision, S.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.UNICEF Under-Five Mortality. [(accessed on 15 May 2022)]. Available online: https://data.unicef.org/topic/child-survival/under-five-mortality/
- 2.World Health Organization Fact Sheets: Diarrhoeal Disease. 15 May 2021. [(accessed on 15 May 2022)]. Available online: https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease.
- 3.Troeger C., Blacker B., Khalil I.A., Rao P.C., Cao J., Zimsen S.R., Albertson S.B., Deshpande A., Farag T., Abebe Z., et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 2018;18:1191–1210. doi: 10.1016/S1473-3099(18)30310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams B.G., Gouws E., Boschi-Pinto C., Bryce J., Dye C. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect. Dis. 2002;2:25–32. doi: 10.1016/S1473-3099(01)00170-0. [DOI] [PubMed] [Google Scholar]
- 5.Kramer M.S., Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst. Rev. 2012:CD003517. doi: 10.1002/14651858.CD003517.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agho K.E., Ezeh O.K., Ghimire P.R., Uchechukwu O.L., Stevens G.J., Tannous W.K., Fleming C., Ogbo F.A., Global Maternal and Child Health Research collaboration Exclusive Breastfeeding Rates and Associated Factors in 13 “Economic Community of West African States” (ECOWAS) Countries. Nutrients. 2019;11:3007. doi: 10.3390/nu11123007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu H., Zhao M., Magnussen C.G., Xi B. Global prevalence of WHO infant feeding practices in 57 LMICs in 2010–2018 and time trends since 2000 for 44 LMICs. EClinicalMedicine. 2021;37:100971. doi: 10.1016/j.eclinm.2021.100971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Victora C.G., Bahl R., Barros A.J., França G.V., Horton S., Krasevec J., Murch S., Sankar M.J., Walker N., Rollins N.C., et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387:475–490. doi: 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 9.Lamberti L.M., Fischer Walker C.L., Noiman A., Victora C., Black R.E. Breastfeeding and the risk for diarrhea morbidity and mortality. BMC Public Health. 2011;11:S15. doi: 10.1186/1471-2458-11-S3-S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sunkonkit K., Ruangkijpaisal N., Reungrongrat S. Factors associated with severe community-acquired pneumonia in thai children. Southeast Asian J. Trop. Med. Public Health. 2020;51:928–936. [Google Scholar]
- 11.Alamneh Y.M., Adane F. Magnitude and Predictors of Pneumonia among Under-Five Children in Ethiopia: A Systematic Review and Meta-Analysis. J. Environ. Public Health. 2020;2020:1606783. doi: 10.1155/2020/1606783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bowatte G., Tham R., Allen K.J., Tan D.J., Lau M.X.Z., Dai X., Lodge C.J. Breastfeeding and childhood acute otitis media: A systematic review and meta-analysis. Acta Paediatr. 2015;104:85–95. doi: 10.1111/apa.13151. [DOI] [PubMed] [Google Scholar]
- 13.Jackson S., Mathews K.H., Pulanić D., Falconer R., Rudan I., Campbell H., Nair H. Risk factors for severe acute lower respiratory infections in children—A systematic review and meta-analysis. Croat. Med. J. 2013;54:110–121. doi: 10.3325/cmj.2013.54.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khan J., Vesel L., Bahl R., Martines J.C. Timing of Breastfeeding Initiation and Exclusivity of Breastfeeding During the First Month of Life: Effects on Neonatal Mortality and Morbidity—A Systematic Review and Meta-analysis. Matern. Child Health J. 2015;19:468–479. doi: 10.1007/s10995-014-1526-8. [DOI] [PubMed] [Google Scholar]
- 15.Krawczyk A., Lewis M.G., Venkatesh B.T., Nair S.N. Effect of Exclusive Breastfeeding on Rotavirus Infection among Children. Indian J. Pediatr. 2016;83:220–225. doi: 10.1007/s12098-015-1854-8. [DOI] [PubMed] [Google Scholar]
- 16.Shen J., Zhang B.M., Zhu S.G., Chen J.J. No direct correlation between rotavirus diarrhea and breast feeding: A meta-analysis. Pediatr. Neonatol. 2018;59:129–135. doi: 10.1016/j.pedneo.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Amour C., Gratz J., Mduma E., Svensen E., Rogawski E.T., McGrath M., Seidman J.C., McCormick B.J.J., Shrestha S., Samie A., et al. Epidemiology and Impact of Campylobacter Infection in Children in 8 Low-Resource Settings: Results from the MAL-ED Study. Clin. Infect. Dis. 2016;63:1171–1179. doi: 10.1093/cid/ciw542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hanieh S., Ha T.T., Simpson J.A., Thuy T.T., Khuong N.C., Thoang D.D., Tran T.D., Tuan T., Fisher J., Biggs B.-A. Exclusive breast feeding in early infancy reduces the risk of inpatient admission for diarrhea and suspected pneumonia in rural Vietnam: A prospective cohort study Global health. BMC Public Health. 2015;15:1166. doi: 10.1186/s12889-015-2431-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haque M.A., Platts-Mills J.A., Mduma E., Bodhidatta L., Bessong P., Shakoor S., Kang G., Kosek M.N., Lima A.A.M., Shrestha S.K., et al. Determinants of Campylobacter infection and association with growth and enteric inflammation in children under 2 years of age in low-resource settings. Sci. Rep. 2019;9:17124. doi: 10.1038/s41598-019-53533-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hassan K.E., Mansour A., Shaheen H., Amine M., Riddle M.S., Young S.Y.N., Sebeny P., Levin S. The impact of household hygiene on the risk of bacterial diarrhea among egyptian children in rural areas, 2004–2007. J. Infect. Dev. Ctries. 2014;8:1541–1551. doi: 10.3855/jidc.4539. [DOI] [PubMed] [Google Scholar]
- 21.Henkle E., Steinhoff M.C., Omer S.B., Roy E., Arifeen S.E., Raqib R., Breiman R.F., Caulfield L.E., Moss W.J., Zaman K. The effect of exclusive breast-feeding on respiratory illness in young infants in a maternal immunization trial in Bangladesh. Pediatr. Infect. Dis. J. 2013;32:431–435. doi: 10.1097/INF.0b013e318281e34f. [DOI] [PubMed] [Google Scholar]
- 22.Mansour A., Shaheen H.I., Amine M., Hassan K., Sanders J.W., Riddle M.S., Armstrong A.W., Svennerholm A.M., Sebeny P.J., Klena J.D., et al. Diarrhea burden due to natural infection with Enterotoxigenic Escherichia coli in a birth cohort in a rural Egyptian community. J. Clin. Microbiol. 2014;52:2595–2603. doi: 10.1128/JCM.00215-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Panda S., Deb A.K., Chawla-Sarkar M., Ramamurthy T., Ganguly S., Pradhan P., Chakraborty A., Desai S., Gupte M.D., Dhere R. Factors associated with diarrhoea in young children and incidence of symptomatic rotavirus infection in rural West Bengal, India. Epidemiol. Infect. 2014;142:1848–1858. doi: 10.1017/S0950268814000831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richard S.A., McCormick B.J.J., Seidman J.C., Rasmussen Z., Kosek M.N., Rogawski E.T., Petri W., Bose A., Mduma E., Maciel B.L.L., et al. Relationships among Common Illness Symptoms and the Protective Effect of Breastfeeding in Early Childhood in MAL-ED: An Eight-Country Cohort Study. Am. J. Trop. Med. Hyg. 2018;98:904–912. doi: 10.4269/ajtmh.17-0457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rogawski E.T., Bartelt L.A., Platts-Mills J.A., Seidman J.C., Samie A., Havt A., Babji S., Trigoso D.R., Qureshi S., Shakoor S., et al. Determinants and Impact of Giardia Infection in the First 2 Years of Life in the MAL-ED Birth Cohort. J Pediatr. Infect. Dis. Soc. 2017;6:153–160. doi: 10.1093/jpids/piw082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rogawski E.T., Guerrant R.L., Havt A., Lima I.F.N., Medeiros P.H.Q.S., Seidman J.C., McCormick B.J.J., Babji S., Hariraju D., Bodhidatta L., et al. Epidemiology of enteroaggregative Escherichia coli infections and associated outcomes in the MAL-ED birth cohort. PLoS Negl. Trop. Dis. 2017;11:e0005798. doi: 10.1371/journal.pntd.0005798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rogawski E.T., Westreich D., Becker-Dreps S., Adair L.S., Sandler R.S., Sarkar R., Kattula D., Ward H.D., Meshnick S.R., Kang G. The effect of early life antibiotic exposures on diarrheal rates among young children in Vellore, India. Pediatr. Infect. Dis. J. 2015;34:583–588. doi: 10.1097/INF.0000000000000679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ajetunmobi O.M., Whyte B., Chalmers J., Tappin D.M., Wolfson L., Fleming M., MacDonald A., Wood R., Stockton D.L., Glasgow Centre for Population Health Breastfeeding Project Steering Group Breastfeeding is associated with reduced childhood hospitalization: Evidence from a Scottish Birth Cohort (1997–2009) J. Pediatr. 2015;166:620–625. doi: 10.1016/j.jpeds.2014.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Annamalay A.A., Khoo S.K., Jacoby P., Bizzintino J., Zhang G., Chidlow G., Lee W.-M., Moore H.C., Harnett G.B., Smith D.W., et al. Prevalence of and risk factors for human rhinovirus infection in healthy aboriginal and non-aboriginal western australian children. Pediatr. Infect. Dis. J. 2012;31:673–679. doi: 10.1097/INF.0b013e318256ffc6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Christensen N., Bruun S., Sondergaard J., Christesen H.T., Fisker N., Zachariassen G., Sangild P.T., Husby S. Breastfeeding and Infections in Early Childhood: A Cohort Study. Pediatrics. 2020;146:11. doi: 10.1542/peds.2019-1892. [DOI] [PubMed] [Google Scholar]
- 31.Diallo A.F., McGlothen-Bell K., Lucas R., Walsh S., Allen C., Henderson W.A., Cong X., McGrath J. Feeding modes, duration, and diarrhea in infancy: Continued evidence of the protective effects of breastfeeding. Public Health Nurs. 2020;37:155–160. doi: 10.1111/phn.12683. [DOI] [PubMed] [Google Scholar]
- 32.Duijts L., Jaddoe V.W.V., Hofman A., Moll H.A. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics. 2010;126:e18–e25. doi: 10.1542/peds.2008-3256. [DOI] [PubMed] [Google Scholar]
- 33.Frank N.M., Lynch K.F., Uusitalo U., Yang J., Lonnrot M., Virtanen S.M., Hyöty H., Norris J.M. The relationship between breastfeeding and reported respiratory and gastrointestinal infection rates in young children. BMC Pediatr. 2019;19:339. doi: 10.1186/s12887-019-1693-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gómez-Acebo I., Lechosa-Muñiz C., Paz-Zulueta M., Sotos T.D., Alonso-Molero J., Llorca J., Cabero-Perez M.J. Feeding in the first six months of life is associated with the probability of having bronchiolitis: A cohort study in Spain. Int. Breastfeed. J. 2021;16:82. doi: 10.1186/s13006-021-00422-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kawai T., Goto A., Watanabe E., Nagasawa M., Yasumura S. Lower respiratory tract infections and gastrointestinal infections among mature babies in Japan. Pediatr. Int. 2011;53:431–445. doi: 10.1111/j.1442-200X.2010.03285.x. [DOI] [PubMed] [Google Scholar]
- 36.Ladomenou F., Moschandreas J., Kafatos A., Tselentis Y., Galanakis E. Protective effect of exclusive breastfeeding against infections during infancy: A prospective study. Arch. Dis Child. 2010;95:1004–1008. doi: 10.1136/adc.2009.169912. [DOI] [PubMed] [Google Scholar]
- 37.Langer S., Horn J., Gottschick C., Klee B., Purschke O., Caputo M., Dorendorf E., Meyer-Schlinkmann K.M., Raupach-Rosin H., Karch A., et al. Symptom Burden and Factors Associated with Acute Respiratory Infections in the First Two Years of Life—Results from the LoewenKIDS Cohort. Microorganisms. 2022;10:111. doi: 10.3390/microorganisms10010111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nakamura K., Matsumoto N., Nakamura M., Takeuchi A., Kageyama M., Yorifuji T. Exclusively Breastfeeding Modifies the Adverse Association of Late Preterm Birth and Gastrointestinal Infection: A Nationwide Birth Cohort Study. Breastfeed. Med. 2020;15:509–515. doi: 10.1089/bfm.2020.0064. [DOI] [PubMed] [Google Scholar]
- 39.Quigley M.A., Carson C., Sacker A., Kelly Y. Exclusive breastfeeding duration and infant infection. Eur. J. Clin. Nutr. 2016;70:1420–1427. doi: 10.1038/ejcn.2016.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rosas-Salazar C., Shilts M.H., Tang Z.Z., Hong Q., Turi K.N., Snyder B.M., Wiggins D.A., Lynch C.E., Gebretsadik T., Peebles R.S., Jr., et al. Exclusive breast-feeding, the early-life microbiome and immune response, and common childhood respiratory illnesses. J. Allergy Clin. Immunol. 2022;3:612–621. doi: 10.1016/j.jaci.2022.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Videholm S., Wallby T., Silfverdal S.A. Breastfeeding practice, breastfeeding policy and hospitalisations for infectious diseases in early and later childhood: A register-based study in Uppsala County, Sweden. BMJ Open. 2021;11:e046583. doi: 10.1136/bmjopen-2020-046583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baye A., Adane M., Sisay T., Hailemeskel H.S. Priorities for intervention to prevent diarrhea among children aged 0–23 months in northeastern Ethiopia: A matched case-control study. BMC Pediatr. 2021;21:155. doi: 10.1186/s12887-021-02592-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Delelegn M.W., Endalamaw A., Belay G.M. Determinants of acute diarrhea among children under-five in Northeast Ethiopia: Unmatched case-control study. Pediatr. Health Med. Ther. 2020;11:323–333. doi: 10.2147/PHMT.S256309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fahdiyani R., Raksanagara A.S., Sukandar H. Influence of household environment and maternal behaviors to upper respiratory infection among toddlers. Kesmas. 2016;10:120–126. doi: 10.21109/kesmas.v10i3.589. [DOI] [Google Scholar]
- 45.Lin H., Sun L., Lin J., He J., Deng A., Kang M., Zeng H., Ma W., Zhang Y. Protective effect of exclusive breastfeeding against hand, foot and mouth disease. BMC Infect. Dis. 2014;14:645. doi: 10.1186/s12879-014-0645-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mir F., Ariff S., Bhura M., Chanar S., Nathwani A.A., Jawwad M., Hussain A., Rizvi A., Umer M., Memon Z., et al. Risk Factors for Acute Respiratory Infections in Children Between 0 and 23 Months of Age in a Peri-Urban District in Pakistan: A Matched Case–Control Study. Front. Pediatr. 2022;9:704545. doi: 10.3389/fped.2021.704545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nascimento R.M.D., Baptista P.N., Lopes K.A.M., Pimentel A.M., Cruz F., Ximenes R.A.A. Protective effect of exclusive breastfeeding and effectiveness of maternal vaccination in reducing pertussis-like illness. J. Pediatr. 2021;97:500–507. doi: 10.1016/j.jped.2020.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ngocho J.S., de Jonge M.I., Minja L., Olomi G.A., Mahande M.J., Msuya S.E., Mmbaga B.T. Modifiable risk factors for community-acquired pneumonia in children under 5 years of age in resource-poor settings: A case-control study. Trop. Med. Int. Health. 2019;24:484–492. doi: 10.1111/tmi.13211. [DOI] [PubMed] [Google Scholar]
- 49.Rustam M., Mahkota R., Kodim N. Exclusive breastfeeding and upper respiratory infection in infants aged 6-12 months in Kampar district, Riau Province. Kesmas. 2019;13:117–123. doi: 10.21109/kesmas.v13i3.1892. [DOI] [Google Scholar]
- 50.Sutriana V.N., Sitaresmi M.N., Wahab A. Risk factors for childhood pneumonia: A case-control study in a high prevalence area in Indonesia. Clin. Exp. Pediatr. 2021;64:588–595. doi: 10.3345/cep.2020.00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yadav S., Khinchi Y., Pan A., Gupta S.K., Shah G.S., Baral D.D., Poudel P. Risk factors for acute respiratory infections in hospitalized under five children in central Nepal. J. Nepal Paediatr. Soc. 2013;33:39–44. doi: 10.3126/jnps.v33i1.7358. [DOI] [Google Scholar]
- 52.Pandolfi E., Gesualdo F., Carloni E., Villani A., Midulla F., Carsetti R., Stefanelli P., Fedele G., Tozzi A.E. Does Breastfeeding Protect Young Infants from Pertussis? Case-control Study and Immunologic Evaluation. Pediatr. Infect. Dis. J. 2017;36:e48–e53. doi: 10.1097/INF.0000000000001418. [DOI] [PubMed] [Google Scholar]
- 53.Abdulla F., Hossain M., Karimuzzaman M., Ali M., Rahman A. Likelihood of infectious diseases due to lack of exclusive breastfeeding among infants in Bangladesh. PLoS ONE. 2022;17:e0263890. doi: 10.1371/journal.pone.0263890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Adhiningsih Y.R., Athiyyah A.F. Identification of acute rotavirus diarrhea and analysis of its risk factors in children under-5 years in Surabaya, Indonesia. Indian J. Public Health Res. Dev. 2020;11:1499–1505. doi: 10.37506/ijphrd.v11i6.10021. [DOI] [Google Scholar]
- 55.Ahmed K.Y., Page A., Arora A., Ogbo F.A., Global Maternal and Child Health Research collaboration Associations between infant and young child feeding practices and acute respiratory infection and diarrhoea in Ethiopia: A propensity score matching approach. PLoS ONE. 2020;15:e0230978. doi: 10.1371/journal.pone.0230978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cai L., Yu P., Zhang Y., Yang X., Li W., Wang P. Effect of feeding pattern on infant illness in Chinese cities. Public Health Nutr. 2016;19:1252–1259. doi: 10.1017/S1368980015002633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dagvadorj A., Ota E., Shahrook S., Olkhanud P.B., Takehara K., Hikita N., Bavuusuren B., Mori R., Nakayama T. Hospitalization risk factors for children’s lower respiratory tract infection: A population-based, cross-sectional study in Mongolia. Sci. Rep. 2016;6:24615. doi: 10.1038/srep24615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dairo M.D., Ibrahim T.F., Salawu A.T. Prevalence and determinants of diarrhoea among infants in selected primary health centres in kaduna north local government area, nigeria. Pan Afr. Med. J. 2017;28:109. doi: 10.11604/pamj.2017.28.109.8152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Demissie B.W., Amele E.A., Yitayew Y.A., Yalew Z.M. Acute lower respiratory tract infections and associated factors among under-five children visiting Wolaita Sodo University Teaching and Referral Hospital, Wolaita Sodo, Ethiopia. BMC Pediatr. 2021;21:413. doi: 10.1186/s12887-021-02888-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dhami M.V., Ogbo F.A., Diallo T.M., Agho K.E., Global Maternal and Child Health Research Collaboration (GloMACH) Regional analysis of associations between infant and young child feeding practices and diarrhoea in indian children. Int. J. Environ. Res. Public Health. 2020;17:4740. doi: 10.3390/ijerph17134740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Flores J.A., Coit J., Mendoza M., Leon S.R., Konda K., Lecca L., Franke M.F. Is exclusive breastfeeding for six-months protective against pediatric tuberculosis? Glob. Health Action. 2021;14:1861922. doi: 10.1080/16549716.2020.1861922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gizaw Z., Woldu W., Bitew B.D. Child feeding practices and diarrheal disease among children less than two years of age of the nomadic people in Hadaleala District, Afar Region, Northeast Ethiopia. Int. Breastfeed. J. 2017;12:24. doi: 10.1186/s13006-017-0115-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hajeebhoy N., Nguyen P.H., Mannava P., Nguyen T.T., Mai L.T. Suboptimal breastfeeding practices are associated with infant illness in Vietnam. Int. Breastfeed. J. 2014;9:12. doi: 10.1186/1746-4358-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Issa C., Hobeika M., Salameh P., Zeidan R.K., Mattar L. Longer durations of both exclusive and mixed breastfeeding are associated with better health in infants and toddlers. Breastfeed. Rev. 2019;27:17–27. doi: 10.3316/informit.674686961104750. [DOI] [Google Scholar]
- 65.Kembo J. Factors associated with the risk of diarrhoeal morbidity among under-3 children in zimbabwe. J. Soc. Dev. Afr. 2011;26:9–38. doi: 10.4314/JSDA.V26I2. [DOI] [Google Scholar]
- 66.Khan M.N., Islam M.M. Effect of exclusive breastfeeding on selected adverse health and nutritional outcomes: A nationally representative study. BMC Public Health. 2017;17:889. doi: 10.1186/s12889-017-4913-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mulatu T., Yimer N.B., Alemnew B., Linger M., Liben M.L. Exclusive breastfeeding lowers the odds of childhood diarrhea and other medical conditions: Evidence from the 2016 Ethiopian demographic and health survey. Ital. J. Pediatr. 2021;47:166. doi: 10.1186/s13052-021-01115-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mulatya D.M., Mutuku F.W. Assessing Comorbidity of Diarrhea and Acute Respiratory Infections in Children Under 5 Years: Evidence from Kenya’s Demographic Health Survey 2014. J. Prim. Care Community Health. 2020;11:2150132720925190. doi: 10.1177/2150132720925190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nigatu D., Azage M., Motbainor A. Effect of exclusive breastfeeding cessation time on childhood morbidity and adverse nutritional outcomes in Ethiopia: Analysis of the demographic and health surveys. PLoS ONE. 2019;14:e0223379. doi: 10.1371/journal.pone.0223379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ogbo F.A., Agho K., Ogeleka P., Woolfenden S., Page A., Eastwood J., Global Child Health Research Interest Group Infant feeding practices and diarrhoea in sub-Saharan African countries with high diarrhoea mortality. PLoS ONE. 2017;12:e0171792. doi: 10.1371/journal.pone.0171792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ogbo F.A., Nguyen H., Naz S., Agho K.E., Page A. The association between infant and young child feeding practices and diarrhoea in Tanzanian children. Trop. Med. Health. 2018;46:2. doi: 10.1186/s41182-018-0084-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ogbo F.A., Page A., Idoko J., Claudio F., Agho K.E. Diarrhoea and Suboptimal Feeding Practices in Nigeria: Evidence from the National Household Surveys. Paediatr. Perinat. Epidemiol. 2016;30:346–355. doi: 10.1111/ppe.12293. [DOI] [PubMed] [Google Scholar]
- 73.Puspitasari M.D., Rahardja M.B. Family health behavior: Preventive measures against acute respiratory infections in under-5 children. Int. J. Prev. Med. 2021;12:99. doi: 10.4103/ijpvm.IJPVM_580_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Saeed O.B., Haile Z.T., Chertok I.A. Association between Exclusive Breastfeeding and Infant Health Outcomes in Pakistan. J Pediatr. Nurs. 2020;50:e62–e68. doi: 10.1016/j.pedn.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 75.Santos F.S., dos Santos L.H., Saldan P.C., Santos F.C.S., Leite A.M., Demello D.F. Breastfeeding and acute diarrhea among children enrolled in the family health strategy. Texto Contexto Enfermagem. 2016;25:e0220015. doi: 10.1590/0104-070720160000220015. [DOI] [Google Scholar]
- 76.Shumetie G., Gedefaw M., Kebede A., Derso T. Exclusive breastfeeding and rotavirus vaccination are associated with decreased diarrheal morbidity among under-five children in Bahir Dar, northwest Ethiopia Fred Paccaud. Public Health Rev. 2018;39:28. doi: 10.1186/s40985-018-0107-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Srivastava S., Mishra P.S., Sinha D., Kumar P. Population attributable risk for breastfeeding practices on diarrhea and acute respiratory infections among children aged 0–23 months in India—What we know and we do not know? Child. Youth Serv. Rev. 2020;119:105531. doi: 10.1016/j.childyouth.2020.105531. [DOI] [Google Scholar]
- 78.Wibowo: T.P., Melaniani S., Salim L.A. Modeling of binary logistic regression in the event of childhood diarrhea in Indonesia. Indian J. Forensic Med. Toxicol. 2021;15:4631–4639. doi: 10.37506/ijfmt.v15i3.16020. [DOI] [Google Scholar]
- 79.Alexandrino A.S., Santos R., Melo C., Bastos J.M. Risk factors for respiratory infections among children attending day care centres. Fam. Pract. 2016;33:161–166. doi: 10.1093/fampra/cmw002. [DOI] [PubMed] [Google Scholar]
- 80.Payne S., Quigley M.A. Breastfeeding and infant hospitalisation: Analysis of the UK 2010 Infant Feeding Survey. Matern. Child Nutr. 2017;13:e12263. doi: 10.1111/mcn.12263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lamberti L.M., Zakarija-Grković I., Fischer Walker C.L., Theodoratou E., Nair H., Campbell H., Black R.E. Breastfeeding for reducing the risk of pneumonia morbidity and mortality in children under two: A systematic literature review and meta-analysis. BMC Public Health. 2013;13:S18. doi: 10.1186/1471-2458-13-S3-S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Binns C.W., Lee M.K. Exclusive breastfeeding for six months: The WHO six months recommendation in the Asia Pacific region. Asia Pac. J. Clin. Nutr. 2014;23:344–350. doi: 10.6133/apjcn.2014.23.3.21. [DOI] [PubMed] [Google Scholar]
- 83.Santos F.S., Santos F.C., Santos L.H., Leite A.M., Mello D.F. Breastfeeding and protection against diarrhea: An integrative review of literature. Einstein. 2015;13:435–440. doi: 10.1590/S1679-45082015RW3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Khanal V., Lee A.H., Scott J.A., Karkee R., Binns C.W. Implications of methodological differences in measuring the rates of exclusive breastfeeding in Nepal: Findings from literature review and cohort study. BMC Pregnancy Childbirth. 2016;16:389. doi: 10.1186/s12884-016-1180-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Indicators For Assessing Infant and Young Child Feeding Practices: Part 1: Definitions: Conclusions of a Consensus Meeting Held 6–8 November 2007 in Washington, DC, USA. [(accessed on 19 June 2022)]. Available online: https://apps.who.int/iris/handle/10665/43895.
- 86.Binns C.W., Fraser M.L., Lee A.H., Scott J. Defining exclusive breastfeeding in Australia. J. Paediatr. Child Health. 2009;45:174–180. doi: 10.1111/j.1440-1754.2009.01478.x. [DOI] [PubMed] [Google Scholar]
- 87.Lee M.K., Binns C. Breastfeeding and the risk of infant illness in Asia: A review. Int. J. Environ. Res. Public Health. 2020;17:186. doi: 10.3390/ijerph17010186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Story L., Perish T. Breastfeeding helps prevent two major infant illnesses. Internet J. Allied Health Sci. Pract. 2008;6:10. doi: 10.46743/1540-580X/2008.1207. [DOI] [Google Scholar]
- 89.Morrow A.L., Rangel J.M. Human milk protection against infectious diarrhea: Implications for prevention and clinical care. Semin. Pediatr. Infect. Dis. 2004;15:221–228. doi: 10.1053/j.spid.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 90.Borg B., Gribble K., Courtney-Haag K., Parajuli K.R., Mihrshahi S. Association between early initiation of breastfeeding and reduced risk of respiratory infection: Implications for nonseparation of infant and mother in the COVID-19 context. Matern. Child Nutr. 2022;18:e13328. doi: 10.1111/mcn.13328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Schlaudecker E.P., Steinhoff M.C., Omer S.B., McNeal M.M., Roy E., Arifeen S.E., Dodd C.N., Raqib R., Breiman R.F., Zaman K. IgA and neutralizing antibodies to influenza a virus in human milk: A randomized trial of antenatal influenza immunization. PLoS ONE. 2013;8:e70867. doi: 10.1371/journal.pone.0070867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rowl M.G., Barrell R.A., Whitehead R.G. Bacterial contamination in traditional Gambian weaning foods. Lancet. 1978;311:136–138. doi: 10.1016/s0140-6736(78)90432-4. [DOI] [PubMed] [Google Scholar]
- 93.McKenna J.J., Ball H.L., Gettler L.T. Mother–infant cosleeping, breastfeeding and sudden infant death syndrome: What biological anthropology has discovered about normal infant sleep and pediatric sleep medicine. Am. J. Phys. Anthropol. Off. Publ. Am. Assoc. Phys. Anthropol. 2007;134:133–161. doi: 10.1002/ajpa.20736. [DOI] [PubMed] [Google Scholar]
- 94.Hauck F.R., Thompson J.M., Tanabe K.O., Moon R.Y., Vennemann M.M. Breastfeeding and reduced risk of sudden infant death syndrome: A meta-analysis. Pediatrics. 2011;128:103–110. doi: 10.1542/peds.2010-3000. [DOI] [PubMed] [Google Scholar]
- 95.Horta B.L., Victora C.G. A Systematic Review on the Benefits of Breastfeeding on Diarrhoea and Pneumonia Mortality. World Health Organization; Geneva, Switzerland: 2013. [Google Scholar]
- 96.Mihrshahi S., Ara G., Khanam M., Rasheed S., Agho K.E., Kabir A.I., Roy S.K., Haider R., Hamadani J.D., Tofail F., et al. The Shishu Pushti Trial–Extended Peer Counseling for Improving Feeding Practices and Reducing Undernutrition in Children Aged 0-48 Months in Urban Bangladesh: Protocol for a Cluster-Randomized Controlled Trial. JMIR Res. Protoc. 2022;11:e31475. doi: 10.2196/31475. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.