Abstract
Background
The transmission of monkeypox virus occurs through direct contact, but transmission through saliva or exhaled droplets and aerosols has not yet been investigated. We aimed to assess the presence of monkeypox virus DNA and infectious virus in saliva samples and droplets and aerosols exhaled from patients infected with monkeypox virus.
Methods
We did a cross-sectional study in patients with monkeypox confirmed by PCR who attended two health centres in Madrid, Spain. For each patient, we collected samples of saliva, exhaled droplets within a mask, and aerosols captured by air filtration through newly developed nanofiber filters. We evaluated the presence of monkeypox virus in the samples by viral DNA detection by quantitative PCR (qPCR) and isolation of infectious viruses in cell cultures.
Findings
Between May 18 and July 15, 2022, 44 patients with symptomatic monkeypox attended two health centres in Madrid and were included in the study. All were cisgender men, with a median age of 35·0 years (IQR 11·3). We identified high loads of monkeypox virus DNA by qPCR in 35 (85%) of 41 saliva samples. Infectious monkeypox virus was recovered from 22 (67%) of 33 saliva samples positive for monkeypox virus DNA. We also found a significant association between the number of affected cutaneous areas or general symptoms and the viral load present in saliva samples. Droplets exhaled from patients with monkeypox, detected inside a mask, contained monkeypox virus DNA in 32 (71%) of 45 samples, with two of the 32 positive samples showing the presence of the infectious virus. Monkeypox virus DNA in aerosols, collected from the medical consultation room, were detected in 27 (64%) of 42 samples, despite patients wearing an FFP2 mask during the visit. Infectious virus was not recovered from aerosol samples. High levels of monkeypox virus DNA were identified in aerosols collected from a hospital isolation room housing a patient with monkeypox.
Interpretation
The identification of high viable monkeypox virus loads in saliva in most patients with monkeypox and the finding of monkeypox virus DNA in droplets and aerosols warrants further epidemiological studies to evaluate the potential relevance of the respiratory route of infection in the 2022 monkeypox virus outbreak.
Funding
EU, Consejo Superior de Investigaciones Científicas, and Ciberinfec.
Introduction
Unprecedented outbreaks of monkeypox have been reported since May, 2022, in many countries around the world.1, 2, 3 The number of cases is increasing and has now surpassed the total number of cases ever reported outside monkeypox-endemic African countries since 1970, when the first case of monkeypox in humans was reported.4 This suggests a more efficient human-to-human transmission of the disease, which might have been spreading undetected, or that the introduction of the virus in the community of men who have sex with men (MSM) has led to more opportunities of contact transmission.5
Monkeypox is an emerging zoonotic disease caused by the monkeypox virus, a member of the Orthopoxvirus genus related to the variola virus, the causative agent of smallpox that was eradicated by 1980 as a result of the WHO Global Smallpox Eradication Campaign.6, 7 The clinical picture of monkeypox resembles that of smallpox, but it is less severe and shows a characteristic lymphoadenopathy not common in smallpox. The monkeypox virus is endemic in central and west Africa, where a natural reservoir in rodents has been identified that sporadically transmits to humans.8 Two clades of monkeypox virus have been identified: the central African clade, renamed clade I, and the west African clade, renamed clade IIa. The two clades are geographically separated and have defined epidemiological and clinical differences. Monkeypox virus clade I shows a higher case-fatality rate of up to 11%, with more human-to-human transmission reported. Clade II has a lower case-fatality rate and has been exported outside the African continent through travellers who were infected or exported animals (as occurred in the 2003 US outbreak). Phylogenetic analysis has shown that the monkeypox virus circulating in the 2022 outbreaks in several non-endemic countries belongs to clade II (subclade IIb).9, 10 The circulating virus has been mainly identified among close contact cases of MSM.2
Research in context.
Evidence before this study
We searched PubMed from inception to Sept 1, 2022, for studies published in English using the following terms, individually or combined: monkeypox infectious virus, saliva, droplets and monkeypox viable virus, airborne, and air transmission. The current evidence indicates that the main route of monkeypox virus transmission is by direct contact with skin lesions, which appears to be responsible for the current monkeypox virus outbreak identified mainly in men who have sex with men. Previous studies in Africa have identified human-to-human transmission in households, and infection by contact with contaminated surfaces or respiratory droplets were suggested as additional routes of transmission. A 2022 report identified monkeypox virus DNA in saliva samples. However, to our knowledge, the identification of infectious monkeypox virus in saliva or virus particles in droplets and aerosols exhaled from infected patients has not been documented.
Added value of this study
We did a study in patients with monkeypox to evaluate whether the virus is present in saliva and could be exhaled to the air as droplets or aerosols. We report high viral loads, detected by quantitative PCR, in saliva from most patients that correlated with the extent of skin lesions and symptoms suggestive of systemic disease. Viable infectious virus from many saliva samples was recovered in cell cultures. We also found that monkeypox virus is present in droplets exhaled by infected individuals, collected within a mask. We detected the presence of infectious virus in two of these samples. Lastly, we took advantage of nanofiber filters that we have recently developed to capture virus particles present in aerosols at longer distances from patients, and we showed for the first time the frequent presence of virus particles in the air collected in the consultation room, despite patients wearing a mask, and high levels of airborne virus in a hospital isolation room housing a patient.
Implications of all the available evidence
Our results show the presence of high loads of infectious monkeypox virus in saliva of infected individuals, indicating that viable monkeypox virus might be present in the oral mucosa. The identification of monkeypox virus in droplets exhaled from patients with monkeypox, including viable viruses in two samples, and in aerosols collected at longer distances suggests that the virus can be found in air samples. Our results do not show transmission, and further investigations will be required to evaluate whether the levels of virus present in saliva, droplets, and aerosols are sufficient for disease transmission. This study has implications for preventive actions and health policies to control transmission in the 2022 monkeypox virus outbreak.
Respiratory viruses can spread through droplets that fall to the ground within a 1·5 m radius of the source and contaminate surfaces (fomites) or through airborne transmission, which involves the inhalation of infectious aerosols that travel longer distances (>1·5 m) suspended in the air.11 The aerosol size was traditionally defined as smaller than 5 μm, but it has been proposed that it should be defined as smaller than 100 μm because particles of this size can travel beyond 1 m and be inhaled. Defining the relative importance of droplet versus airborne transmission is complex because of technical limitations.11
Transmission of monkeypox virus is thought to occur through direct contact with lesion exudates or crust material, body fluids, and respiratory droplets of people who are infected.7 A 2022 report showed experimental evidence for the presence of monkeypox virus DNA in saliva samples12 but, to our knowledge, evidence of infectious virus in saliva or virus particles in droplets and aerosols has not been reported. To determine whether patients infected with monkeypox virus might expel it through respiratory tract secretions and whether the respiratory route of transmission might be relevant, we aimed to investigate the presence of monkeypox virus DNA and infectious virus in saliva samples and droplets and aerosols exhaled from patients infected with monkeypox virus.
Methods
Patients and variables
For this cross-sectional study, we recruited successive cases of individuals with suspected cutaneous lesions of monkeypox virus, which was confirmed by PCR, who attended two health centres in Madrid, Spain (Hospital Clínico San Carlos and Centro Sanitario Sandoval). Samples of the cutaneous lesion, saliva, mask filter, and air were obtained from each patient. We included these in the analysis if the cutaneous sample tested positive for monkeypox virus by PCR. Clinical and epidemiological information was recorded for each patient at the time of the visit, including the location of suspected lesions in one of the following cutaneous regions: face, perioral, upper limbs, lower limbs, trunk, and palms and soles. In patients with two sets of samples, we selected the most recent sample from the first visit when this information was used to associate clinical and laboratory data. Included patients provided written informed consent. The study protocol was approved by the Ethics Committee of the Hospital Clínico San Carlos (approval number 22/389-E).
Sample collection
Sample collection was done at the two participating health centres. Characteristics of the consultation and isolation rooms are described in the appendix (p 3). We collected a sample from the cutaneous lesion at the first visit and three additional types of non-invasive samples within the first week of infection for patients with a positive monkeypox PCR result (appendix p 15): phlegm-free saliva collected in a sterile vial in private; exhaled breath and respiratory tract secretions expelled through the nose and mouth, captured in two 25 mm nanofiber filters in the interior of an FPP2 mask (Bioinicia [Paterna, Spain] and Spanish National Research Council [CSIC]) worn by the patient during the medical visit (30–45 min, except for about 30 s when the mask was removed during exploration of the oral cavity and oropharynx); and two air samples filtered through 47 mm nanofiber filters (Bioinicia and CSIC) connected during the medical visit (30–45 min) to air pumps with an airflow of 30 L/min and placed at 2–3 m from the patient and at 1·5 m in height to collect aerosols that remained suspended in the air. Nanofiber filters were developed in 2021 and shown to capture SARS-CoV-2 from air samples.13, 14 The filter used, based on nanofiber technology developed by the Institute of Agrochemistry and Food Technology (CSIC) and Bioinicia, was composed of two protective spunbond polypropylene layers of 18 g/m2 sandwiching a polyvinylidene fluoride nanofiber layer of 0·9 g/m2, without antimicrobial components. The filtration efficiency for paraffin aerosols (0·14–5·00 μm in size) was a mean 99·29% (SD 0·11), and the pressure drop tested at 160 L/min in filter areas of 100 cm2 was a mean 317·03 Pa (SD 30·78). Filters were immersed into collection media (phosphate-buffered saline containing 0·1% bovine serum albumin and 25 μg/mL gentamycin) to test virus viability or cell lysis buffer from the Maxwell RSC Viral Total Nucleic Acid Purification kit (Promega; Madison, WI, USA) for quantitative PCR (qPCR) detection, and they were kept at 4°C until processed. Air samples from a patient with monkeypox housed in a hospital isolation room were collected with 47 mm nanofiber filters (Bioinicia and CSIC) connected to a 15 L/min air pump for 2–3 h and processed as indicated.
Detection of monkeypox virus DNA and infectivity
We inactivated saliva samples under biosafety level 3 (BSL3) containment by adding an equal volume of twice concentrated cell lysis buffer to the sample (Promega). For DNA extraction from mask filters, air filters, and saliva in cell lysis buffer, we used the Viral Total Nucleic Acid Purification kit (Promega) in combination with a Maxwell RSC 48 Instrument (Promega). To enhance the recovery of DNA, 100 ng of human DNA (from HeLa cells) were added to each sample from mask and air filters as a DNA carrier. We detected monkeypox virus DNA by qPCR using specific primers and fluorescent-labelled probes previously described.15 All measurements were made in triplicate, and a non-template control together with the standard curve (7-log standard curve of 10-fold dilutions of a plasmid containing an 85 bp insert of monkeypox virus DNA) were included in each plate. Samples with a cycle threshold (Ct) value lower than 35 and with a positive result for at least two of three replicates were considered positive by qPCR. After quantification by Ct interpolation in the calibration curve, data were converted to copies of monkeypox virus DNA/mL of saliva, copies per mask filter, or copies/m3 of captured air. We tested virus infectivity from clinical samples on BSC-1 cells (American Type Culture Collection [ATCC] CCL-26; ATCC, Mansassas, VA, USA), handled in BSL3 facilities. A detailed description of these methods is presented in the appendix (pp 4–5).
Transmission electron microscopy
Saliva samples were fixed in phosphate-buffered saline (PBS) with 4% paraformaldehyde for 30 min at room temperature in a BSL3 facility. Fixed samples were adsorbed to ionised collodion-carbon coated grids for 5 min, washed with PBS, and exposed for 30 s at 37°C to a drop of 2% uranyl acetate. We analysed specimens using a Jeol 1400 Flash transmission electron microscope.
Statistical analysis
We compared baseline clinical and epidemiological characteristics of the patients in terms of test positivity, viability, and viral load in each sample with the Fisher's exact test, χ2 test, Wilcoxon test, Kruskal Wallis test, Cochran Armitage test, and univariate linear models as appropriate. For the analysis, viral load was logarithmically transformed to increase the linearity of this measure. In the linear models, the assumptions of linearity, homoscedasticity, independence, and normality were tested in each model. All measures are shown in terms of median (IQR), with range also provided when indicated. Statistical analysis was done with R, version 4.1, considering 2-sided values of p<0·05 as statistically significant. No subgroup or sensitive analyses were done. Missing values from viral load (undetermined or not available) were excluded for the analysis.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
During the 2022 monkeypox outbreak, between May 18 and July 15, Madrid was one of the areas with the highest incidence in the world, with 2249 confirmed cases by Aug 23, 2022.16 Of these, patients with symptomatic disease from two health centres in Madrid were assessed from June 7 to 26 (appendix pp 7–8). 44 cisgender men, of whom 41 (94%) self-identified as MSM, were included in the study; only one patient required hospitalisation. The median age was 35·0 years (IQR 11·3). 23 (52%) patients were positive for HIV on treatment, all with undetectable HIV. 11 (25%) patients reported having received a smallpox vaccine, and six (14%) did not know whether they had been vaccinated. The median time from symptom onset to sample collection was 5 days (IQR 4–7, range 1–9). Fever was reported as first symptom in 18 (41%) patients, with 33 (75%) patients having reported fever at any time during the disease duration. Most patients (40 [91%]) developed general symptoms such as asthenia, myalgia, headache, odynophagia, or fever. Additionally, 26 (59%) of 44 patients had inguinal adenopathies, of which 14 (54%) were classified as painful, and 16 (36%) had adenopathies in other locations, especially cervical (ten [63%) of 16). All patients had characteristic vesicular-umbilicated and pseudo-pustular skin lesions, most frequently located on the anogenital region (33 [75%]), face (31 [70%]), trunk (25 [57%]), and upper limbs (24 [55%]). 12 (27%) patients had a concomitant sexually transmitted infection other than HIV (appendix pp 7–8).
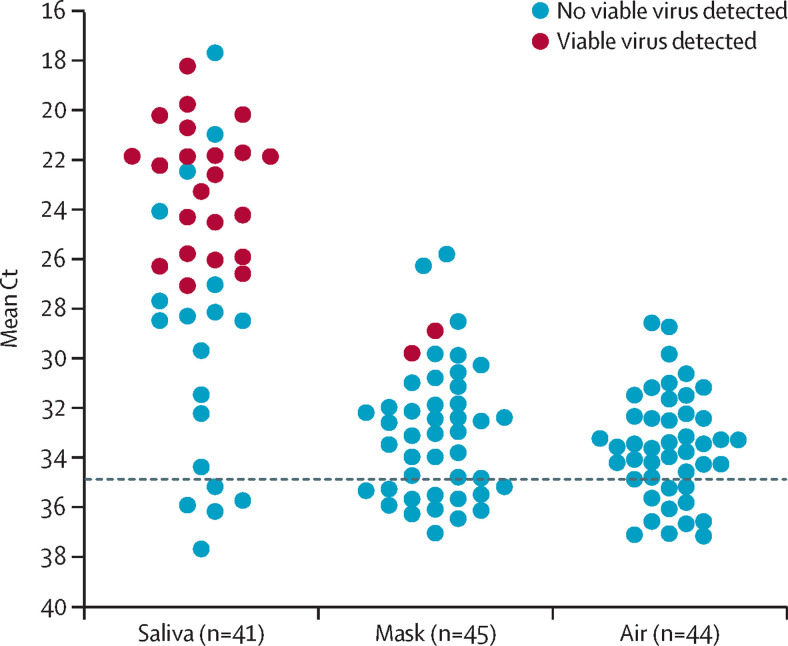
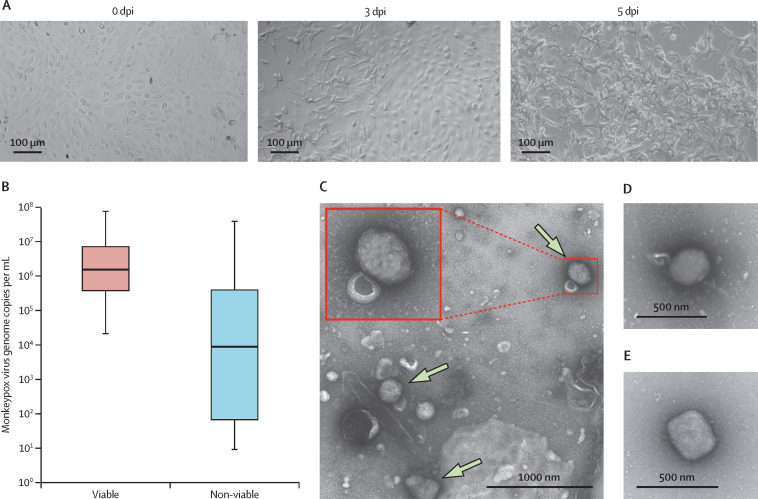
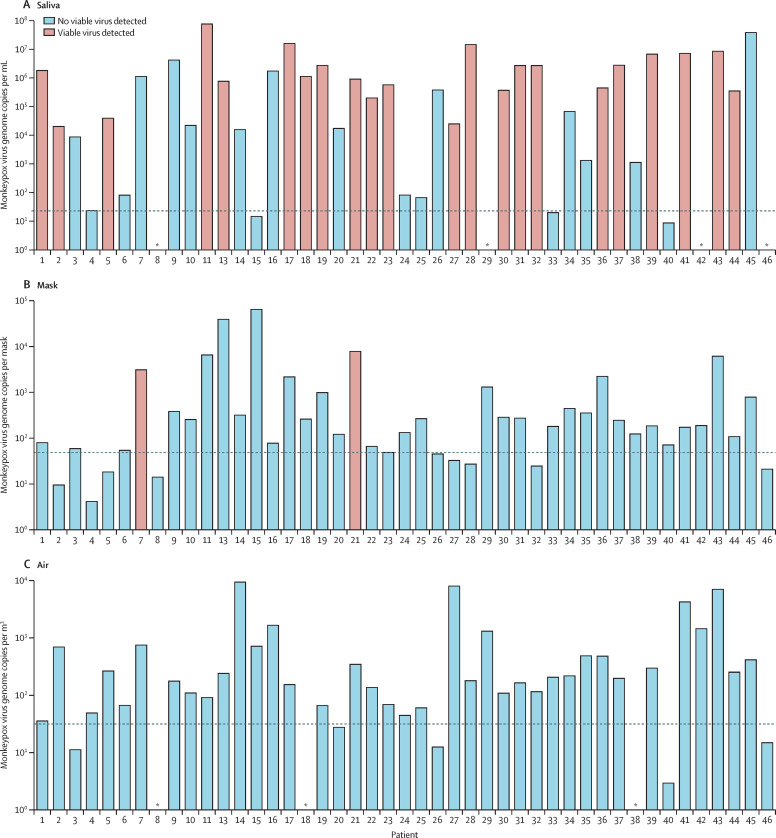
Analysis by qPCR revealed that 35 (85%) of 41 saliva samples tested positive for monkeypox virus. The Ct values obtained from positive samples were unexpectedly low (lowest Ct value was 18) and most ranged from 20 to 26 (figure 1 ). These low Ct values indicate an elevated viral load and raise the possibility that viable monkeypox virus could remain in the saliva of patients with monkeypox. Indeed, cells inoculated with saliva samples showed the typical monkeypox virus-induced cytopathic effect at the first attempt in 22 (67%) of the 33 positive samples (figure 1, appendix pp 9–10). The fact that the cytopathic effect rapidly spread through the cell culture within the first 5 days after inoculation indicates the presence of infectious virus in saliva (figure 2A ). The presence of monkeypox virus was further confirmed by qPCR in cell cultures in which the cytopathic effect was observed (appendix p 11). We found a relationship between the viral load estimated by qPCR and the detection of viable virus, indicating that recovering infectious viruses was more likely in samples with Ct lower than 26 or with a viral load higher than 104 monkeypox virus genomes per mL of saliva (Figure 2, Figure 3 , appendix p 12). Consistently, monkeypox virus particles were identified by transmission electron microscopy in saliva samples with high viral loads (figure 2), similar to virions identified in patient pustules (figure 2E).
Figure 1.
Monkeypox virus detection in 45 samples from patients with confirmed infection
Individual mean Ct values determined by a specific quantitative PCR for monkeypox virus DNA from every patient's saliva, mask filter, and air filter are shown. A mean Ct value of 35 was established as threshold for positivity (dotted line). Each sample was tested in triplicate, and at least two of three wells needed to be positive for the sample to be considered positive. Red colour indicates samples in which infectious viruses were detected after inoculation of cell monolayers. Ct=cycle threshold.
Figure 2.
Infectious monkeypox virus detected in saliva samples from patients
(A) Representative cytopathic effect in BSC-1 cells inoculated with a fraction of saliva sample from a patient and examined daily for cytopathic effect; images show viral spreading through the cell culture at 0, 3, and 5 days after infection. (B) Box and whisker plot showing the distribution of monkeypox virus loads from saliva samples containing (red) or not containing (blue) viable virus (n=41). (C, D) Identification of monkeypox virus particles (green arrows) in saliva samples by electron microscopy after negative staining; the inset shows the magnification of the indicated virion. (E) Monkeypox virus particle from a pustular lesion identified by electron microscopy after negative staining.
Figure 3.
Monkeypox virus load determination from samples
Estimated monkeypox virus genome copies per mL of saliva (A) and mask filter (B) or m3 of captured air (C) from every patient. We interpolated cycle thresholds in the calibration curve (range of linearity from 106 to 1 copy per μL, with a slope of –3·10, intercept 35·82; R2=0·997 and amplification efficiency of 110%). Red bars indicate samples in which infectious monkeypox virus was detected. Dotted lines indicate the baseline of the assay in every sample; values below this line were considered negative. n=41 for saliva, n=45 for mask filters, and n=42 for air samples. Patient 12 was not confirmed positive for monkeypox virus infection by PCR of the cutaneous lesion, and was excluded from the study. *Not available.
In the assessment of exhaled breath samples, 32 (71%) of 45 mask filters were positive for monkeypox virus by qPCR (baseline Ct of 35), with a lowest Ct value of 26 (figure 1). Viral loads detected in positive mask filters were lower than those estimated for saliva samples, ranging from 70 to about 6 × 104 monkeypox virus genomes per mask (figure 3B, appendix pp 9–10). Consequently, the number of positive mask filter samples in which infectious viruses could be recovered was limited to patient number 7 (3 × 103 monkeypox virus genomes per mask filter) and number 21 (8 × 103 monkeypox virus genomes per mask filter). Both samples with infectious viruses were in the 85th percentile of viral load.
In the assessment of air samples, 27 (64%) of 42 air filters tested positive for monkeypox virus by qPCR (baseline Ct of 35), despite patients wearing an FFP2 mask for almost the whole visit. The distribution of Ct values was similar to that of Ct values obtained for mask filters (lowest Ct value of 29; figure 1), and the viral loads calculated ranged from 40 to about 9 × 103 monkeypox virus genomes per m3 (figure 3C, appendix pp 9–10). Moreover, air samples collected with the nanofiber filters from a hospital isolation room housing a single patient with monkeypox with respiratory symptoms tested positive for monkeypox virus on two consecutive days. The viral load in the saliva of this patient was lower than others (3·7 × 105 monkeypox virus genomes per mL) but infectious in cell culture, and it could be detected in the mask filter but not in the air filter during the medical visit (appendix pp 9–10). Despite these low levels of monkeypox virus in the patient's samples, high levels of monkeypox virus DNA were identified in two air samples taken during 2–3 h from the isolation room (Cts of 30 and 29, corresponding to 4·4 × 103 viral genomes per m3 for the first sample and 1·3 × 103 viral genomes per m3 for the second). We could not recover infectious viruses from any of the air samples.
We found that systemic symptoms, such as non-inguinal lymphoadenopathy, asthenia, and myalgia, as well as skin lesions located in the face, upper limbs, and trunk, were associated with higher monkeypox virus loads in saliva (appendix pp 12–13). The presence of headache (16 [76%] of 20 with the symptom vs seven [41%] of 17 without; p=0·04) and non-inguinal adenopathies (13 [93%] of 14 with the symptom vs ten [43%] of 23 without; p=0·008) were associated with the identification of viable monkeypox virus in saliva. We observed an association between the presence of oral symptoms (odynophagia or perioral lesions) at the time of evaluation and the viability of monkeypox virus in saliva samples (18 [75%] of 24 vs five [38%] of 13; p=0·039), but we could not find this association in samples collected from masks (two [7%] of 28 vs 0 [0%] of 15; p=0·54) or ambient air (0 [0%] of 26 vs 0 [0%] of 14; p=1·0). We did not find an association between respiratory symptoms, such as cough, nasal congestion, or dyspnoea, and the presence of monkeypox virus DNA in masks, although the number of patients with respiratory symptoms was very low (six [14%]).
Additionally, we found an association between monkeypox virus load in saliva and the extent of skin involvement, defined by the number of affected body regions; these areas were the face, upper extremities, trunk, lower extremities, palms and soles, and anal and genital area (appendix pp 14, 16). We used a linear model to predict the logarithm of monkeypox virus load in saliva as a function of the number of skin lesions. For each new area affected, viral load was increased by a mean of 48% (IQR 16–88, p=0·002; appendix p 16). When we calculated the percentage of viral positivity and viability in cumulative subgroups of patients with increasing number of skin areas affected, we found that subgroups of patients with more areas affected had higher viability (p<0·01) and positivity (p=0·01) in saliva samples than subgroups with fewer areas affected, as well as higher positivity in mask samples (p<0·01; appendix p 14). In terms of monkeypox virus PCR positivity in saliva, we observed a gradual increase in positivity for saliva samples (p=0·05), mask samples (p<0·001), and air samples (p=0·01) when more affected regions were considered (appendix p 14). In terms of monkeypox virus load or viability in saliva, we found no differences between people living with HIV, those with a concurrent sexually transmitted infection, or those previously vaccinated against smallpox, although vaccination was not confirmed by serology and was unlikely considering the age of the patients.
Discussion
The identification of monkeypox virus DNA in saliva by qPCR was reported in 12 patients in 2022.12 Our study in 44 patients with monkeypox, assessed less than a week after onset of symptoms, extends this observation by identifying monkeypox virus DNA in a high proportion (85%) of saliva samples. We also provide, to our knowledge, the first experimental evidence for the presence of infectious monkeypox virus in human saliva. We found the viral load detected by qPCR to be high in most cases, reaching values of up to 106–107 viral genomes per mL. Moreover, the finding of viable virus in 66% of qPCR-positive saliva samples suggests that monkeypox virus present in oral mucosa is infectious. The finding of high viral loads in saliva that can be ejected from the mouth as spittle droplets suggests that saliva might contribute, together with respiratory droplets, aerosols, and shedding of skin lesions, to surface contamination with the infectious virus. Monkeypox virus DNA has been detected by qPCR on various surfaces in hospital rooms occupied by patients with monkeypox, and the infectious virus was found in some of these samples, as described in three publications.17, 18, 19
Human-to-human transmission of monkeypox virus has been reported in the past in Africa, but the number of studies is low.6, 7, 20 Several studies showed transmission within a household, and transmission routes other than direct contact might occur under these circumstances, perhaps through saliva contaminating surfaces, droplets, or aerosols. However, these studies have not addressed the relative contribution of different routes of transmission, and these should be investigated. Our finding of high viral loads in saliva in people infected with monkeypox virus with general symptoms and more affected skin areas suggests that, in this initial phase of the disease (a median of 5 days of symptoms), a systemic infection is evolving that can affect the oral mucosa. A limitation of our study is that we have not determined viraemia to assess a systemic infection. Prolonged upper respiratory tract viral DNA shedding after skin lesion resolution was reported in some patients.21 Similarly, it will be of interest to investigate whether monkeypox virus might be present in saliva for longer periods.
We have developed new nanofiber filters that allowed us to capture monkeypox virus particles from aerosols that can travel long distances in the air. A limitation of this study is the fact that we did not recover infectious monkeypox virus from air samples, which contrasts with the recovery of viable virus from most saliva samples. This might be due to the low levels of virus captured from the air, not reaching the viral load that might be required to recover the virus in cell cultures. Additionally, the use of filters to capture airborne viruses might not preserve viral infectivity due to desiccation of the sample. Similar technical limitations have been found in studies of SARS-CoV-2, a virus that transmits through aerosols: the use of a gentle vapour condensation VIVAS sampler allowed researchers to show the presence of viable virus in aerosols.11, 22 A 2022 study reported the identification of five air samples positive for monkeypox virus DNA, taken at a distance of 1·0–2·5 m from patient beds in a hospital, with low levels of viral DNA detected (generally Ct of about 36).19 Three of the positive samples, one of them with replication-competent viruses taken at less than 1 m from the patient (Ct 32·7), were collected during bed linen changes, suggesting that the viruses detected in the air sample might correspond to viruses in fomites re-aerosolised rather than aerosols generated by the patient's breathing. Our detection of higher levels of monkeypox virus DNA in air samples (Ct 28·5–35·0) might be due to the use of nanofiber filters instead of gelatine filters, together with the sampling of larger air volumes. We should note that high levels of monkeypox virus DNA in air samples were detected in this study despite patients wearing an FFP2 mask, suggesting that even higher levels might be exhaled when masks are not used.
The identification of high viral loads of infectious monkeypox virus in saliva and the emission of viral particles from nose and mouth (from spittle, respiratory droplets, or aerosols) that can be captured in mask filters might represent a potential route of transmission. Moreover, the frequent identification of the virus in the air suggests that monkeypox virus is also present in aerosols that travel longer distances. Reports have shown the presence of monkeypox virus DNA detected by qPCR in nose and throat swabs, suggesting shedding from the upper respiratory tract3, 12, 21 that would be compatible with our identification of viral DNA in droplets and aerosols. Viable monkeypox virus has been recovered from laboratory-controlled aerosols after up to 90 h, suggesting that the virus might remain infectious for long periods in the environment.23 Human-to-human aerosol transmission has not been documented for monkeypox virus. However, evidence of human infections from prairie dogs in the 2003 US outbreak, in which individuals who were in the same room with a prairie dog without handling the animals or who entered the room after the prairie dog was removed became infected with monkeypox, suggests indirect contact (fomites) or aerosol transmission.24, 25 This evidence supports the potential of monkeypox virus to transmit through the respiratory route, as shown in the prairie dog model of infection.26 Similarly, transmission of variola virus, a related virus that caused human smallpox, is thought to occur by direct contact and droplets, but evidence also exists of airborne transmission.27
Our understanding of monkeypox virus human-to-human transmission is scarce. Most cases in the 2022 outbreak of monkeypox are in MSM, and close contact with skin lesions and possibly sexual transmission plays a major role in transmission in this context, consistent with the finding of monkeypox virus DNA in skin lesions and semen.12, 28, 29 The high loads of infectious monkeypox virus in saliva suggest that salivary transmission might also contribute to transmission during sexual activity and should be investigated. Community transmission is likely to occur and, as monkeypox spreads to other social groups, alternative types of transmission other than direct skin contact during sexual activity might become more relevant and warrant further investigation. Asymptomatic infections are likely to occur in this monkeypox virus outbreak, which can contribute to viral spread in the community,30, 31 and we hypothesise that the presence of the virus in respiratory droplets and aerosols might be relevant in monkeypox transmission.
Further investigations are required to determine whether the viral loads present in saliva, droplets, and aerosols are sufficient for efficient transmission of monkeypox virus and to evaluate the relevance of salivary and respiratory routes of transmission in the spread of the disease in the community. Our results have implications for prevention and control measurements of the 2022 monkeypox virus outbreak, which should consider the presence of monkeypox virus in saliva and air samples.
Data sharing
Deidentified participant data collected for the study will be made available from the corresponding authors on reasonable request.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
This study was funded by the EU (Nextgeneration EU), Consejo Superior de Investigaciones Científicas (PTI Salud Global), and Ciberinfec (Acción estratégica MKPXV22). We thank Milagros Guerra and the Electron Microscopy Service at CBMSO for their support. We thank the contribution of Grupo Viruela Simio Madrid ISCIII/HCSC/Sandoval.
Contributors
AA and VE conceived and led the study and raised funding. AA, BH, AS, AM-G, EO, and VE were responsible for study design and writing of the manuscript. BH, AS, and RM did the laboratory analysis of the samples, including the growth of monkeypox virus in BSL3 conditions. IS, OA, TP, MV, NC, JV, AN, JdR, and VE were responsible for recruitment and clinical care of the patients. AM-G and EO were involved in clinical data collection. AV-C did the statistical analysis. CP, MP-F, AS, AA, and JML developed the nanofiber filters. All authors reviewed and approved the final version of the manuscript.
Supplementary Material
References
- 1.Zumla A, Valdoleiros SR, Haider N, et al. Monkeypox outbreaks outside endemic regions: scientific and social priorities. Lancet Infect Dis. 2022;22:929–931. doi: 10.1016/S1473-3099(22)00354-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Orviz E, Negredo A, Ayerdi O, et al. Monkeypox outbreak in Madrid (Spain): clinical and virological aspects. J Infect. 2022;85:412–417. doi: 10.1016/j.jinf.2022.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tarín-Vicente EJ, Alemany A, Agud-Dios M, et al. Clinical presentation and virological assessment of confirmed human monkeypox virus cases in Spain: a prospective observational cohort study. Lancet. 2022;400:661–669. doi: 10.1016/S0140-6736(22)01436-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO Multi-country outbreak of monkeypox, external situation report #9. 2022. https://www.who.int/publications/m/item/multi-country-outbreak-of-monkeypox--external-situation-report--9---2-november-2022
- 5.Kozlov M. Monkeypox outbreaks: 4 key questions researchers have. Nature. 2022;606:238–239. doi: 10.1038/d41586-022-01493-6. [DOI] [PubMed] [Google Scholar]
- 6.Weaver JR, Isaacs SN. Monkeypox virus and insights into its immunomodulatory proteins. Immunol Rev. 2008;225:96–113. doi: 10.1111/j.1600-065X.2008.00691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reynolds MG, Damon IK. Outbreaks of human monkeypox after cessation of smallpox vaccination. Trends Microbiol. 2012;20:80–87. doi: 10.1016/j.tim.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Beer EM, Rao VB. A systematic review of the epidemiology of human monkeypox outbreaks and implications for outbreak strategy. PLoS Negl Trop Dis. 2019;13 doi: 10.1371/journal.pntd.0007791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakazawa Y, Mauldin MR, Emerson GL, et al. A phylogeographic investigation of African monkeypox. Viruses. 2015;7:2168–2184. doi: 10.3390/v7042168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Isidro J, Borges V, Pinto M, et al. Phylogenomic characterization and signs of microevolution in the 2022 multi-country outbreak of monkeypox virus. Nat Med. 2022;28:1569–1572. doi: 10.1038/s41591-022-01907-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang CC, Prather KA, Sznitman J, et al. Airborne transmission of respiratory viruses. Science. 2021;373 doi: 10.1126/science.abd9149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peiró-Mestres A, Fuertes I, Camprubí-Ferrer D, et al. Frequent detection of monkeypox virus DNA in saliva, semen, and other clinical samples from 12 patients, Barcelona, Spain, May to June 2022. Euro Surveill. 2022;27 doi: 10.2807/1560-7917.ES.2022.27.28.2200503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lagaron JM, Pardo-Figurez MM, Chiva A, Teno J. WO2021005258—multilayer filter with antimicrobial properties and use thereof in industrial filtration applications and protective masks. 2021. https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2021005258
- 14.Pardo-Figuerez M, Chiva-Flor A, Figueroa-Lopez K, Prieto C, Lagaron JM. Antimicrobial nanofiber based filters for high filtration efficiency respirators. Nanomaterials (Basel) 2021;11:900. doi: 10.3390/nano11040900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Y, Zhao H, Wilkins K, Hughes C, Damon IK. Real-time PCR assays for the specific detection of monkeypox virus West African and Congo Basin strain DNA. J Virol Methods. 2010;169:223–227. doi: 10.1016/j.jviromet.2010.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centro de Coordinación de Alertas y Emergencias Sanitarias Informe de situación del 23/08/22. Alerta sobre infección de viruela de los monos en España y otros países no endémicos. 2022. https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/alertaMonkeypox/docs/Informe_de_situacion_MPX_20220823.pdf
- 17.Nörz D, Pfefferle S, Brehm TT, et al. Evidence of surface contamination in hospital rooms occupied by patients infected with monkeypox, Germany, June 2022. Euro Surveill. 2022;27 doi: 10.2807/1560-7917.ES.2022.27.26.2200477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Atkinson B, Burton C, Pottage T, et al. Infection-competent monkeypox virus contamination identified in domestic settings following an imported case of monkeypox into the UK. Environ Microbiol. 2022;24:4561–4569. doi: 10.1111/1462-2920.16129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gould S, Atkinson B, Onianwa O, et al. Air and surface sampling for monkeypox virus in a UK hospital: an observational study. Lancet Microbe. 2022 doi: 10.1016/S2666-5247(22)00257-9. published online Oct 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bunge EM, Hoet B, Chen L, et al. The changing epidemiology of human monkeypox—a potential threat? A systematic review. PLoS Negl Trop Dis. 2022;16 doi: 10.1371/journal.pntd.0010141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adler H, Gould S, Hine P, et al. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect Dis. 2022;22:1153–1162. doi: 10.1016/S1473-3099(22)00228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lednicky JA, Lauzard M, Fan ZH, et al. Viable SARS-CoV-2 in the air of a hospital room with COVID-19 patients. Int J Infect Dis. 2020;100:476–482. doi: 10.1016/j.ijid.2020.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Verreault D, Killeen SZ, Redmann RK, Roy CJ. Susceptibility of monkeypox virus aerosol suspensions in a rotating chamber. J Virol Methods. 2013;187:333–337. doi: 10.1016/j.jviromet.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reynolds MG, Yorita KL, Kuehnert MJ, et al. Clinical manifestations of human monkeypox influenced by route of infection. J Infect Dis. 2006;194:773–780. doi: 10.1086/505880. [DOI] [PubMed] [Google Scholar]
- 25.Hammarlund E, Lewis MW, Carter SV, et al. Multiple diagnostic techniques identify previously vaccinated individuals with protective immunity against monkeypox. Nat Med. 2005;11:1005–1011. doi: 10.1038/nm1273. [DOI] [PubMed] [Google Scholar]
- 26.Hutson CL, Gallardo-Romero N, Carroll DS, et al. Transmissibility of the monkeypox virus clades via respiratory transmission: investigation using the prairie dog-monkeypox virus challenge system. PLoS One. 2013;8 doi: 10.1371/journal.pone.0055488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Milton DK. What was the primary mode of smallpox transmission? Implications for biodefense. Front Cell Infect Microbiol. 2012;2:150. doi: 10.3389/fcimb.2012.00150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Antinori A, Mazzotta V, Vita S, et al. Epidemiological, clinical and virological characteristics of four cases of monkeypox support transmission through sexual contact, Italy, May 2022. Euro Surveill. 2022;27 doi: 10.2807/1560-7917.ES.2022.27.22.2200421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Noe S, Zange S, Seilmaier M, et al. Clinical and virological features of first human monkeypox cases in Germany. Infection. 2022 doi: 10.1007/s15010-022-01874-z. published online July 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferré VM, Bachelard A, Zaidi M, et al. Detection of monkeypox virus in anorectal swabs from asymptomatic men who have sex with men in a sexually transmitted infection screening program in Paris, France. Ann Intern Med. 2022;175:1491–1492. doi: 10.7326/M22-2183. [DOI] [PubMed] [Google Scholar]
- 31.De Baetselier I, Van Dijck C, Kenyon C, et al. Retrospective detection of asymptomatic monkeypox virus infections among male sexual health clinic attendees in Belgium. Nat Med. 2022 doi: 10.1038/s41591-022-02004-w. published online Aug 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Deidentified participant data collected for the study will be made available from the corresponding authors on reasonable request.