Abstract
Objectives
The drug overdose crisis with shifting patterns from primarily opioid to polysubstance uses and COVID-19 infections are 2 concurrent public health crises in the United States, affecting the population of sizes in different magnitudes (approximately < 10 million for substance use disorder [SUD] and drug overdoses vs 80 million for COVID-19 within 2 years of the pandemic). Our objective is to compare the relative scale of disease burden for the 2 crises within a common framework, which could help inform policy makers with resource allocation and prioritization strategies.
Methods
We calculated disability-adjusted life-years (DALYs) for SUD (including opioids and stimulants) and COVID-19 infections, respectively. We collected estimates for SUD prevalence, overdose deaths, COVID-19 cases and deaths, disability weights, and life expectancy from multiple publicly available sources. We then compared age distributions of estimated DALYs.
Results
We estimated a total burden of 13.83 million DALYs for SUD and drug overdoses and 15.03 million DALYs for COVID-19 in 2 years since March 2020. COVID-19 burden was dominated by the fatal burden (> 95% of total DALYs), whereas SUD burden was attributed to both fatal (53%) and nonfatal burdens (47%). The highest disease burden was among individuals aged 30 to 39 years for SUD (27%) and 50 to 64 years for COVID-19 (31%).
Conclusions
Despite the smaller size of the affected population, SUD and drug overdoses resulted in comparable disease burden with the COVID-19 pandemic. Additional resources supporting evidence-based interventions in prevention and treatment may be warranted to ameliorate SUD and drug overdoses during both the pandemic and postpandemic recovery.
Keywords: COVID-19, disease burden, drug overdose, population health, substance use disorder
Introduction
Since the World Health Organization (WHO) declared the COVID-19 outbreak as a global pandemic in March 2020, the COVID-19 pandemic has taken 825 000 lives in the United States by the end of the year 2021 and close to 1 million lives as of April 2022.1 With > 2 years of vaccination, social distancing, and other public health measures, the cases, deaths, and hospitalizations in the United States have started to show a steady decline.1 , 2
Although the COVID-19 pandemic has been considered the pressing public health crisis over the past 2 years, it was not the only public health threat in this country. The drug overdose epidemic was highly publicized as a major public health crisis before the COVID-19 pandemic started and has remained to be a public health threat. More than 841 000 Americans have died of drug overdoses since 1999; the number of overdose deaths in 1 year increased to 71 000 in 2019 (ie, on average 8 deaths per hour).3 Although most of these overdose deaths were due to opioids, stimulant-related deaths have greatly increased in recent years. In 2017, 19.7% of drug overdose deaths involved cocaine and 14.7% involved psychostimulants,4 pointing to changing nature of the drug overdose crisis to a polysubstance landscape. When the response to the COVID-19 pandemic became the top public health priority in 2020, drug overdose deaths did not decline. On the contrary, numerous reports revealed that drug overdose deaths significantly increased during the pandemic.5 The total number of overdose deaths in the United States reached a record high of 92 000 in 2020, with the largest single-year percentage increase (29%) since 1999,6 and topped 100 000 drug overdose deaths during the 12-month period ending in April 2021.7
Not only are the death tolls by the 2 crises at different scales, the sizes of the affected population have also been presented at different magnitudes. The 2020 National Survey on Drug Use and Health (NSDUH) reported the past-year initiation of major illicit drug use (opioids and stimulants) to be 2.7 million and the past-year prevalence of substance use disorder (SUD) for illicit drugs except marijuana to be 6.1 million among people aged 12 or older.8 For COVID-19, within its first 2 years, 78 million people were infected with 90% of infected cases aged 12 or older1—an average of 35 million incidence for each year that is still substantially higher than that for illicit drug use.
Although the 2 concurrent crises seem to have drastically different scales, it is nontrivial to determine the relative order of magnitude of the disease burden that each has placed on society—the size of the affected population does not always necessarily reflect the true disease burden. Disease burden is a common measure used to inform public health policy makers about resource allocation and prioritization strategies for improving population health. Therefore, it is important to understand the burdens of the 2 crises—one being on a steady decline whereas the other one remaining stubbornly persistent and even worsening—retrospectively, to inform the health policies going forward. It is also important to understand the relative importance of the fatal versus nonfatal portions of the disease burden as this also informs the type of evidence-based interventions to prioritize. In this study, we aimed to estimate the disease burden of each by disability-adjusted life-years (DALYs), a standard measure used in the Global Burden of Disease (GBD) studies,9 and compare the resulting age distributions of the disease burden for the 2 public health crises.
Methods
We used DALYs to quantify the disease burden following the recommended methods by WHO.10 DALYs are calculated as the sum of (1) years lived with disability (YLDs) that are representing the nonfatal burden and (2) years of life lost (YLLs) because of premature death that are representing the fatal burden. Time discounting for future lost years of healthy life and age weighting to give less weight to YLLs at young and older ages were applied in earlier GBD studies, but their justification and interpretation have been debated.10 WHO adopted the approach of not applying time discounting and age weighting when calculating DALYs since 2012, and we followed the same approach in this analysis. We estimated the total DALYs of SUD representing the drug overdose crisis and those of COVID-19 infections among the population of age 12 and older during the 2 years of the COVID-19 pandemic starting from March 2020 in the United States. Our analysis focused on the population of age 12 and older because of the data availability for drug use estimates (consistent with the lowest age for the prevalence estimates reported by NSDUH,8 see more details below) and the very low risk of hospitalization and death from COVID-19 for this age group.11
Years Lived With Disabilities
We calculated the YLDs of SUD using a prevalence-based approach. In particular, we obtained prevalence estimates of SUD in the past year from the 2020 NSDUH12 for 3 major types of drugs, opioids, cocaine, and methamphetamine, separately (Appendix Table 1 in Supplemental Materials found at https://doi.org/10.1016/j.jval.2022.11.010). We chose these drug types primarily because they have been the key drugs involved in the changing drug overdose crisis, which has shifted from prescription opioids (wave 1) to heroin (wave 2) and synthetic opioids (wave 3)13 and now toward polysubstance uses, particularly with stimulants (wave 4).14 Furthermore, the overdose deaths involving these drugs contribute to 90% of the total overdose deaths from all drugs. The disability weight values were based on the estimates for heroin and other opioid dependence, cocaine dependence, and amphetamine dependence (as a surrogate for methamphetamine) from the 2019 GBD study.10 We multiplied the prevalence estimate by the disability weight for each drug and summed over the 3 drugs to calculate the total YLDs for 1 year. Given that the NSDUH reported the past-year SUD for each specific drug only by limited age groups of 12 to 17, 18 to 25, and 26+ years, we approximated the distribution of refined age categories within the 26+ age group based on the estimates of the past-month misuse of each drug by detailed age categories (Appendix Table 2 in Supplemental Materials found at https://doi.org/10.1016/j.jval.2022.11.010).
To calculate the COVID-19 related YLDs, we used the incidence-based approach following the recently published guide and studies.15, 16, 17 We considered YLDs of COVID-19 infections based on different health states including mild, severe (hospitalized), critical (admitted to intensive care unit), and postacute states. We did not consider the YLDs for asymptomatic infections of COVID-19. The YLD of each health state was calculated by multiplying the incidence, duration, and disability weight of the same health state. The proportion of asymptomatic, mild, and severe cases and postacute symptoms were estimated from the published studies18, 19, 20 (Appendix Table 1 in Supplemental Materials found at https://doi.org/10.1016/j.jval.2022.11.010). We assumed a duration of 21 days (equivalently, 21/365 years) as a conservative estimate for all symptomatic infections, given the reported values ranging widely but mostly below 3 weeks,21 and 90 days for the postacute state with prolonged symptoms.22 Given that the disability weight for each COVID-19 health state was not directly available from the GBD study, we used the disability weights of similar clinical conditions as a proxy, following the same approach in the literature (Appendix Table 1 in Supplemental Materials found at https://doi.org/10.1016/j.jval.2022.11.010).15 The total COVID-19 cases from March 2020 to February 2022 and the age distribution were obtained from the Centers for Disease Control and Prevention COVID Data Tracker (data accessed as of August 2022).1
Years of Life Lost
We computed YLLs by multiplying the number of deaths with the life expectancy of each age and summing over all ages. We estimated the life expectancy of each (single-year) age from the latest US life table.23 The latest mortality data were obtained from the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research Provisional Multiple Causes of Deaths (MCD) Data.3 We identified the COVID-19-related deaths by the International Classification of Diseases, Tenth Revision, MCD code U07.1. Overdose deaths from opioids and stimulants (to be consistent with the selected drug types for prevalence estimates and YLD calculation) were identified by the underlying cause of death code X40-44 (unintentional), X60-64 (suicide), X85 (homicide), or Y10-14 (undetermined intent) and MCD code T40.0-T40.4, T40.6 (opioids), T40.5 (cocaine), and T43.6 (psychostimulants with abuse potential). Due to the longer lag time for drug overdose deaths compared with other causes of death,24 the numbers of overdose deaths were deemed incomplete in January and February 2022. We imputed the values for these months using the past 6-month average (ie, from July to December of 2021) as a conservative estimate given its increasing trend.3 , 5 All counts of deaths were stratified by single-year age category. We replaced all suppressed values (counts below 10 were suppressed from the Wide-Ranging Online Data for Epidemiologic Research) with zero, which had minimal impact on the results given that suppressed values appeared in only a few of the very large age groups.
Results
During the period of 2 years since the pandemic from March 2020 to February 2022, the total direct impact of COVID-19 infections among the population of age 12 years and older in the United States was estimated to be 15.03 million (5363 per 100 000 population with ages 12 years and older) DALYs, consisting of 14.43 million YLLs (5148 YLLs per 100 000 population) as the fatal burden and 0.60 million YLDs (215 YLDs per 100 000 population) as the nonfatal burden (Table 1 ). The fatal burden contributed to most (96.0%) of the total direct burden of COVID-19. During the same period, SUD and drug overdoses resulted in a total burden of 13.83 million DALYs (4936 DALYs per 100 000 population), which comprised 6.48 million YLDs (2312 YLDs per 100 000 population) and 7.35 million YLLs (2624 YLLs per 100 000 population) from drug overdose deaths. The total YLLs and YLDs represented 53.2% and 46.8% of the total disease burden of SUD, respectively. Results for one-way sensitivity analysis by varying key parameters over uncertainty ranges are included in the Appendix Table 3 in Supplemental Materials found at https://doi.org/10.1016/j.jval.2022.11.010.
Table 1.
Disease burden for drug overdose crisis (substance use disorder and drug overdoses) and for COVID-19 infections, respectively, March 2020 to February 2022.
| Disease burden of public health crisis | YLLs (% of total) | YLDs (% of total) | DALYs (% of total) |
|---|---|---|---|
| Drug overdose crisis (substance use disorder and drug overdoses) | 7 353 334 | 6 477 988 | 13 831 322 |
| 12-17 years | 65 594 (0.89) | 158 756 (2.45) | 224 350 (1.62) |
| 18-29 years | 1 801 105 (24.49) | 1 425 364 (22) | 3 226 469 (23.33) |
| 30-39 years | 2 357 514 (32.06) | 1 383 586 (21.36) | 3 741 099 (27.05) |
| 40-49 years | 1 548 039 (21.05) | 1 493 407 (23.05) | 3 041 446 (21.99) |
| 50-64 years | 1 417 251 (19.27) | 1 392 751 (21.5) | 2 810 002 (20.32) |
| 65-74 years | 154 726 (2.1) | 624 123 (9.63) | 778 849 (5.63) |
| 75-84 years | 8319 (0.11) | (0) | 8319 (0.06) |
| 85+ years | 787 (0.01) | (0) | 787 (0.01) |
| COVID-19 infections | 14 426 389 | 602 459 | 15 028 849 |
| 12-17 years | 28 250 (0.2) | 50 633 (8.4) | 78 883 (0.52) |
| 18-29 years | 338 941 (2.35) | 142 859 (23.71) | 481 800 (3.21) |
| 30-39 years | 813 798 (5.64) | 113 068 (18.77) | 926 866 (6.17) |
| 40-49 years | 1 531 313 (10.61) | 95 994 (15.93) | 1 627 307 (10.83) |
| 50-64 years | 4 556 238 (31.58) | 122 167 (20.28) | 4 678 405 (31.13) |
| 65-74 years | 3 595 316 (24.92) | 44 781 (7.43) | 3 640 096 (24.22) |
| 75-84 years | 2 416 286 (16.75) | 21 971 (3.65) | 2 438 257 (16.22) |
| 85+ years | 1 146 248 (7.95) | 10 987 (1.82) | 1 157 235 (7.7) |
Note. All values are n (%) unless otherwise specified.
DALY indicates disability-adjusted life-year; YLD, year lived with disability; YLL, year of life lost.
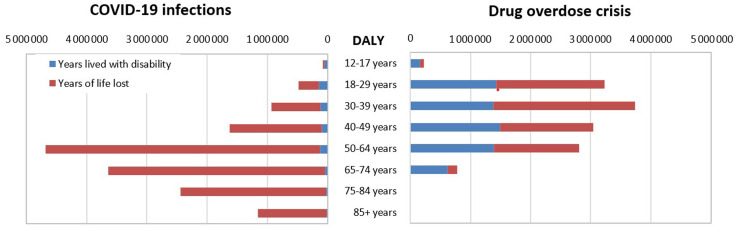
Figure 1 compares the age distribution of the disease burdens. For COVID-19 infections, most of the burden was attributed to the age groups 50 years and older, with the highest DALYs between ages 50 and 64 years (31% of total DALYs). Furthermore, the YLDs of COVID-19 infections were nearly negligible compared with the YLLs, especially in the elderly population of age 50 years and older. For SUD and drug overdose, the disease burden was primarily concentrated between ages 18 and 64 years, contributing to 93% of the total burden, with the highest burden among ages 30 to 39 years (27% of total DALYs). Unlike COVID-19 infections, for SUD and drug overdoses, the nonfatal burden (YLDs) represented a substantial portion of the total disease burden in most age groups; the fatal burden (YLLs) constituted most of total DALYs (50%-63%) across different age groups between 18 and 64 years.
Figure 1.
Comparison of years lived with disability and years of life lost for drug overdose crisis (substance use disorder and drug overdoses) and for COVID-19 infections by age groups, March 2020 to February 2022.
DALY indicates disability-adjusted life-year.
Discussion
We estimated a total of 15.03 million DALYs resulted from SUD and drug overdoses and 13.83 million DALYs from COVID-19 infections in the United States from March 2020 to February 2022, 2 years into the pandemic. Our results imply that the disease burdens of these 2 public health crises are close with comparable order of magnitude despite the disproportionately smaller population affected by SUD and drug overdoses. The burden of COVID-19 was predominately attributable to deaths in the elderly population of age 50 years and older, given that the disability from COVID symptoms was mostly mild and temporary with a relatively short duration. In contrast, the burden of drug use and overdose was borne primarily by the younger population, driven by the long-term disability and the greater YLLs because of overdose deaths at younger ages.
Despite the time-varying patterns of multiple COVID-19 waves and the continuing increase in drug overdose deaths, each contributed approximately 7 million DALYs per year. In fact, according to the estimates of disease burden by disease categories from the 2019 GBD study,9 , 25 there were only a few broad disease categories resulting in > 7 million DALYs in 2019, which were cardiovascular diseases (17.3 million DALYs), neoplasms (16.7 million DALYs), musculoskeletal disorders (14.0 million DALYs), mental disorders (7.3 million DALYs), and chronic respiratory diseases (7.0 million DALYs). The disease burden of specific illnesses, such as diabetes, stroke, chronic obstructive pulmonary diseases, chronic kidney diseases, and Alzheimer’s diseases, were all well below 7 million DALYs annually. This comparison clearly illustrated the significance of the disease burden attributed to these 2 public health crises in the past 2 years.
Our analysis could have underestimated the disease burden of SUD and overdoses. For estimating the morbidity of SUD, we only included the prevalence of opioids, cocaine, and methamphetamines from the NSDUH reports, given that these 3 drug categories contributed to most of total drug overdose deaths and have well-defined disability weight parameters from the GBD report. Although it is possible that the SUD from these 3 drugs were not necessarily mutually exclusive, the summation of their estimated prevalence value remained lower than the prevalence for “illicit drugs other than marijuana” from the NSDUH report, implying that our approach still likely underestimated the total morbidity burden of SUDs. Furthermore, although the NSDUH 2020 has revised its survey question and criteria for determining SUD,26 the long-criticized issue of underestimating SUD prevalence may still persist because of the stigmatized drug use behavior among the hard-to-reach population.27 In addition, underestimating SUD prevalence is particularly common for older adults.28 Despite the probable underestimation, our estimates were still higher than the GBD estimates in 2019 with a total of 6.12 million DALYs (2.98 million YLDs and 3.13 million YLLs)25 attributed to drug use disorders (excluding alcohol), highlighting the pressing need of actions in response to the worsening SUD and drug overdose crisis.
Our estimate of the COVID-19 mortality burden also merits some further discussion. We used the incidence-based approach to estimate YLDs for COVID-19 and the prevalence-based approach for the drug overdose crisis. Historically, the GBD study has transitioned from the incidence-based to the prevalence-based approach considering that disease incidence rates and duration were more difficult to obtain from conventional epidemiological studies,10 which, nevertheless, are mostly straightforward estimates in the context of COVID-19. One limitation of our COVID-19 disease burden estimate is that there was a lack of exact estimates of disability weights for COVID-19. We followed the approach in recent studies15, 16, 17 where the disability weights for COVID-19 states were inferred from other similar conditions of respiratory diseases. In fact, our sensitivity analysis implied that the uncertainty in the estimates of these disability weights may have a very limited impact on the results of the total disease burden given that asymptomatic cases constituted a substantial portion of all infections. Furthermore, research for fully understanding the long COVID is still in progress. The parameters—frequency, duration, and disability weight—of the long COVID will affect the estimation of the nonfatal burden of COVID-19. Given that the follow-up lengths and definitions of long COVID in existing studies varied substantially,29, 30, 31, 32 we used a gross proxy of the disability weight for the postacute COVID state and very conservative assumptions of its frequency and duration in our analysis. Future research is needed to standardize the definition and to refine the evaluation of its impact on health measured with disability weight and quality of life.
We also acknowledge that the YLLs for COVID-19 deaths could be overestimated because of preexisting chronic conditions, given that roughly 84% of individuals who died of COVID had at least one chronic comorbidity including cardiovascular diseases, diabetes, hypertension, or chronic obstructive pulmonary disease.33 Thus, these patients would likely not have achieved the life expectancy of the general population. In contrast, several studies have argued that the full impact of the pandemic on mortality in society could be greater than the reported COVID-19 deaths, given that the changes in other social, economic, and behavioral aspects during the pandemic may also affect overall mortality.34 , 35 A global analysis predicted the cumulative excess mortality because of the COVID-19 pandemic in the United States to be 1.13 million for 2020 to 2021, which is more than one-third higher than the 825 000 reported deaths during the same period.1 In our calculation, we chose to use the reported deaths from the same mortality data source to make the comparison between the 2 epidemics more meaningful. Considering the variations in the estimates, our results demonstrated that the disease burden of SUD has been qualitatively comparable in the order of magnitude with that of COVID-19 infections.
Given the sharp increases in overdose deaths during the pandemic, there are understudied interactive effects between the COVID-19 pandemic and the SUD epidemic. The interplay is bidirectional. On the one hand, SUD is a risk factor associated with increased disease severity and mortality of COVID-19.36, 37, 38 That is, the preexisting drug overdose crisis had increased the COVID-19 burden disproportionately among the population with SUD. In contrast, increases in drug use have been observed since the COVID-19 pandemic.5 The pandemic presented numerous challenges, barriers, and disruptions for people with SUD and those in recovery. Job loss, social isolation, and neglected illness may have negatively affected individuals with SUDs and destabilized patients in otherwise sustained recovery during this time period. Mitigation efforts such as vaccination that could effectively reduce the stress of COVID-19 on society would help to reduce social restrictions and promote economic recovery sooner, which will enable more individuals to access treatment and avoid premature death because of overdose.
As the COVID-19 pandemic recedes with increased vaccination rates and other mitigation efforts, we expect that the increased barriers to substance abuse services and the exacerbated burden of drug overdoses induced by the COVID-19 pandemic would be hopefully alleviated, which, nevertheless, by no means implies the resolution of the drug overdose crisis. SUD and overdose deaths will stubbornly remain and will demand the necessary attention and investment to address them. SUD and overdose deaths have been prevalent for decades and show little sign of abatement. After 2 years of consistent decline, overdose deaths increased by 30% during the COVID-19 pandemic.6 Effective medications and treatments are available; nevertheless, too many individuals with SUD lack health insurance or access to quality evidence-based intervention programs.39 , 40 Evidence-based medications with psychosocial services for SUD remain deeply stigmatized41 and hard to access in many rural locations.42
Although the fatal burden from overdose deaths constitutes most of the disease burden of SUD, its nonfatal burden is substantial. This implies that policies that solely focus on overdose death reductions, such as naloxone, fentanyl strip distribution, and other harm reduction interventions, are not sufficient to achieve sustained reductions of the disease burden in the long run. Policy changes will also be necessary to increase prevention efforts, access to behavioral health services, medication for the treatment of SUDs, and recovery services. Moreover, legislative efforts to decriminalize drug use and divert individuals to treatment may help destigmatize treatment and create new avenues for treatment introduction, such as various Law Enforcement Assisted Diversion programs throughout the country.43 , 44 Implementing evidence-based interventions of prevention and treatment will be an effective solution to reduce both the nonfatal and fatal burden of SUD and drug overdoses.
Overall, our analysis found that despite the smaller size of the affected population, SUD and drug overdoses resulted in a comparable disease burden with the COVID-19 infections in the United States during the 2 years of the pandemic. Substantial resources and continued endeavors are warranted to ameliorate the ongoing drug overdose crisis.
Article and Author Information
Author Contributions:Concept and design: Chen, Griffin, Kawasaki
Acquisition of data: Chen
Analysis and interpretation of data: Chen, Griffin
Drafting of the manuscript: Chen, Griffin, Kawasaki
Critical revision of the paper for important intellectual content: Chen, Griffin, Kawasaki
Statistical analysis: Chen
Conflict of Interest Disclosures: The authors reported no conflicts of interest.
Funding/Support: Dr Kawasaki was supported by the National Institutes of Health under award number grant AT010118, the National Institute on Drug Abuse under award number AWD0000584 (135723-1), the and Substance Abuse and Mental Health Services Administration under award number TI081432.
Role of theFunder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Acknowledgment
The authors sincerely thank Dr Susan Griffin for suggesting the initial conceptual ideas and constructive comments on the manuscript.
Footnotes
Supplementary data associated with this article can be found in the online version at https://doi.org/10.1016/j.jval.2022.11.010.
Supplemental Material
References
- 1.COVID data tracker. Centers for Disease Control and Prevention. https://covid.cdc.gov/covid-data-tracker/#datatracker-home. Accessed August 27, 2022.
- 2.Willingham L, Mattise J. US virus cases, hospitalizations continue steady decline. US News. February 21. https://apnews.com/article/coronavirus-pandemic-health-new-york-infectious-diseases-buffalo-1a11bbba3693c38a3ac6d7069496244f, 2022. Accessed April 20, 2022.
- 3.Mattson C.L., Tanz L.J., Quinn K., Kariisa M., Patel P., Davis N.L. Trends and geographic patterns in drug and synthetic opioid overdose deaths - United States, 2013-2019. MMWR Morb Mortal Wkly Rep. 2021;70(6):202–207. doi: 10.15585/mmwr.mm7006a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kariisa M., Scholl L., Wilson N., Seth P., Hoots B. Drug overdose deaths involving cocaine and psychostimulants with abuse potential - United States, 2003-2017. MMWR Morb Mortal Wkly Rep. 2019;68(17):388–395. doi: 10.15585/mmwr.mm6817a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Issue brief: Nation’s drug-related overdose and death epidemic continues to worsen. American Medical Association. https://www.ama-assn.org/system/files/issue-brief-increases-in-opioid-related-overdose.pdf. Accessed August 20, 2021.
- 6.Ahmad F, Rossen L, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics, Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed August 27, 2022.
- 7.Drug overdose deaths in the U.S. Top 100,000 annually. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm. Accessed April 20, 2022.
- 8.Results from the 2020 National Survey on Drug Use and Health: detailed tables. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. https://www.samhsa.gov/data/report/2020-nsduh-detailed-tables. Accessed August 27, 2022.
- 9.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO methods and data sources for global burden of disease estimates 2000-2019. World Health Organization. https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/ghe2019_daly-methods.pdf. Accessed September 1, 2021.
- 11.Risk for COVID-19 infection, hospitalization, and death by age group. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html. Accessed August 25, 2022.
- 12.National Survey of Drug Use and Health (NSDUH) releases. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/release/2020-national-survey-drug-use-and-health-nsduh-releases. Accessed April 1, 2022.
- 13.Ciccarone D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy. 2019;71:183. doi: 10.1016/j.drugpo.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ciccarone D. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr Opin Psychiatry. 2021;34(4):344–350. doi: 10.1097/YCO.0000000000000717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wyper G., Assunção R., Colzani E., et al. Burden of disease methods: a guide to calculate COVID-19 disability-adjusted life years. Int J Public Health. 2021;66 doi: 10.3389/ijph.2021.619011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cuschieri S., Calleja N., Devleesschauwer B., Wyper G.M.A. Estimating the direct Covid-19 disability-adjusted life years impact on the Malta population for the first full year. BMC Public Health. 2021;21(1):1827. doi: 10.1186/s12889-021-11893-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh B.B., Devleesschauwer B., Khatkar M.S., et al. Disability-adjusted life years (DALYs) due to the direct health impact of COVID-19 in India, 2020. Sci Rep. 2022;12(1):2454. doi: 10.1038/s41598-022-06505-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oran D.P., Topol E.J. Prevalence of asymptomatic SARS-CoV-2 infection : a narrative review. Ann Intern Med. 2020;173(5):362–367. doi: 10.7326/M20-3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oran D.P., Topol E.J. The proportion of SARS-CoV-2 infections that are asymptomatic : a systematic review. Ann Intern Med. 2021;174(5):655–662. doi: 10.7326/M20-6976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stokes E.K., Zambrano L.D., Anderson K.N., et al. Coronavirus disease 2019 case surveillance - United States, January 22-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(24):759–765. doi: 10.15585/mmwr.mm6924e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nguyen N.T., Chinn J., Nahmias J., et al. Outcomes and mortality among adults hospitalized with COVID-19 at US medical centers. JAMA Netw Open. 2021;4(3) doi: 10.1001/jamanetworkopen.2021.0417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greenhalgh T., Knight M., A’Court C., Buxton M., Husain L. Management of post-acute COVID-19 in primary care. BMJ. 2020;370:m3026. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- 23.Arias E., Xu J. United States life tables, 2018. Natl Vital Stat Rep. 2020;69(12):1–45. [PubMed] [Google Scholar]
- 24.Spencer M, Ahmad F. Timeliness of death certificate data for mortality surveillance and provisional estimates. National Center for Health Statistics, Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data/vsrr/report001.pdf. Accessed February 1, 2022.
- 25.GBD results tool. Institute for Health Metrics and Evaluation. https://ghdx.healthdata.org/gbd-results-tool. Accessed April 1, 2022.
- 26.National Survey on Drug Use and Health (NSDUH). methodological summary and definitions. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. 2020. https://www.samhsa.gov/data/report/2020-methodological-summary-and-definitions. Accessed August 27, 2022.
- 27.Nesoff E.D., Martins S.S., Palamar J.J. Caution is necessary when estimating treatment need for opioid use disorder using national surveys. Am J Public Health. 2022;112(2):199–201. doi: 10.2105/AJPH.2021.306624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Han B., Gfroerer J.C., Colliver J.D., Penne M.A. Substance use disorder among older adults in the United States in 2020. Addiction. 2009;104(1):88–96. doi: 10.1111/j.1360-0443.2008.02411.x. [DOI] [PubMed] [Google Scholar]
- 29.Yong S.J. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis (Lond) 2021;53(10):737–754. doi: 10.1080/23744235.2021.1924397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thompson E.J., Williams D.M., Walker A.J., et al. Long COVID burden and risk factors in 10 UK longitudinal studies and electronic health records. Nat Commun. 2022;13(1):3528. doi: 10.1038/s41467-022-30836-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ballering A.V., van Zon S.K.R., Olde Hartman T.C., Rosmalen J.G.M., Lifelines Corona Research Initiative Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. Lancet. 2022;400(10350):452–461. doi: 10.1016/S0140-6736(22)01214-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sudre C.H., Murray B., Varsavsky T., et al. Attributes and predictors of long COVID. Nat Med. 2021;27(4):626–631. doi: 10.1038/s41591-021-01292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bajgain K.T., Badal S., Bajgain B.B., Santana M.J. Prevalence of comorbidities among individuals with COVID-19: a rapid review of current literature. Am J Infect Control. 2021;49(2):238–246. doi: 10.1016/j.ajic.2020.06.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.COVID-19 Excess Mortality Collaborators Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet. 2022;399(10334):1513–1536. doi: 10.1016/S0140-6736(21)02796-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stokes A.C., Lundberg D.J., Elo I.T., Hempstead K., Bor J., Preston S.H. COVID-19 and excess mortality in the United States: a county-level analysis. PLoS Med. 2021;18(5) doi: 10.1371/journal.pmed.1003571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang Q.Q., Kaelber D.C., Xu R., Volkow N.D. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry. 2021;26(1):30–39. doi: 10.1038/s41380-020-00880-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baillargeon J., Polychronopoulou E., Kuo Y.F., Raji M.A. The impact of substance use disorder on COVID-19 outcomes. Psychiatr Serv. 2021;72(5):578–581. doi: 10.1176/appi.ps.202000534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Allen B., El Shahawy O., Rogers E.S., Hochman S., Khan M.R., Krawczyk N. Association of substance use disorders and drug overdose with adverse COVID-19 outcomes in New York City: January-October 2020. J Public Health (Oxf) 2021;43(3):462–465. doi: 10.1093/pubmed/fdaa241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ali M.M., Teich J., Woodward A., Han B. The implications of the Affordable Care Act for behavioral health services utilization. Admin Policy Ment Health. 2016;43(1):11–22. doi: 10.1007/s10488-014-0615-8. [DOI] [PubMed] [Google Scholar]
- 40.Ali M.M., Teich J.L., Mutter R. Reasons for not seeking substance use disorder treatment: variations by health insurance coverage. J Behav Health Serv Res. 2017;44(1):63–74. doi: 10.1007/s11414-016-9538-3. [DOI] [PubMed] [Google Scholar]
- 41.Allen B., Nolan M.L., Paone D. Underutilization of medications to treat opioid use disorder: what role does stigma play? Subst Abus. 2019;40(4):459–465. doi: 10.1080/08897077.2019.1640833. [DOI] [PubMed] [Google Scholar]
- 42.Joudrey P.J., Edelman E.J., Wang E.A. Drive times to opioid treatment programs in urban and rural counties in 5 US states. JAMA. 2019;322(13):1310–1312. doi: 10.1001/jama.2019.12562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Collins S.E., Lonczak H.S., Clifasefi S.L. Seattle’s Law Enforcement Assisted Diversion (LEAD): program effects on recidivism outcomes. Eval Program Plann. 2017;64:49–56. doi: 10.1016/j.evalprogplan.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 44.Anderson E., Shefner R., Koppel R., Megerian C., Frasso R. Experiences with the Philadelphia police assisted diversion program: a qualitative study. Int J Drug Policy. 2022;100 doi: 10.1016/j.drugpo.2021.103521. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.