Abstract
Introduction and importance
Rare presence of intra-articular osteoid osteoma may be difficult to diagnose due to the lack of typical radiographic features and clinical appearance similar to other articular pathologies. Additionally traditional treatment choices for osteoid osteoma may not suit the given environment of the shoulder joint area.
Case presentation
We presented a 50-year-old male with a prolonged history of anterior shoulder pain and shoulder stiffness after physical activity. Intra-articular joint pathology was suspected after initial clinical and radiographic assessment. Magnetic resonance imaging revealed an osteoid osteoma in the humeral bicipital groove.
Clinical discussion
The surgical goal is to resect the benign bony tumour. Though the established treatment by open surgery or radiological minimally invasive techniques may not be optimal since pathologies in the shoulder joint cannot be addressed without the risk of damage to articular structures and increased complications. In this case to avoid joint incision site morbidity and address adjacent pathology arthroscopic removal of the tumour with refixation of the biceps longus tendon was carried out. At follow up of 12 months post-surgery physical activity did not provoke stiffness and resting pain has subsided.
Conclusion
Arthroscopic intra-articular osteoma resection in shoulder joint was optimal to address adjacent osteoma induced pathology, achieve great visualization, reduce incision site complication rates and achieve good results. Additional synovectomy during arthroscopic treatment can be performed, due to concomitant synovitis causing joint stiffness in most reported intra-articular OO cases.
Keywords: Case report, Intra-articular osteoma, Osteoid osteoma, Arthroscopic osteoma resection, Shoulder osteoma, Osteoma mri
Highlights
-
•
MRI can be advantageous over CT in intra-articular OO cases to evaluate co-existing or osteoma induced joint pathology
-
•
Arthroscopic resection of intra-articular OO is ideal to directly visualise, treat adjacent pathology, reduce incision morbidity.
-
•
Synovitis causing joint stiffness reported in most intra-articular OO cases is adressed by arthroscopic synovectomy
1. Introduction and importance
Osteoid osteoma (OO) is a benign osteogenic tumour accounting for approximately 5 % of all bone tumours and 11 % of benign bone tumours [1]. OO usually occurs in the diaphyseal or metaphyseal cortices of the long bones and the spine, while less often in the medullary cavity or the periosteum. Around 13 % of all osteoid osteomas are intra-articular or near the joints [2]. Rare presence of intra-articular OO and non-specific symptoms may mimic other, more common articular pathologies. In example, osteoid osteoma in the shoulder joint may be misdiagnosed as rotator cuff tear, biceps longus tear or shoulder stiffness syndrome (frozen shoulder), which make the osteoid osteoma diagnosis challenging [3], [4]. Patients with intra-articular or close shoulder joint osteoma often lack typical radiographic features, like perifocal sclerosis, and commonly need tomography imaging to diagnose and accurately assess lesion localization for determining the correct surgical approach [5]. There is evidence that intra-articular osteoid osteoma may be associated with early osteoarthritis [6]. Though timely diagnosis and treatment is relevant.
The goal of the treatment is benign tumour resection. In the literature there are no specific guidelines regarding shoulder osteoma diagnosis and surgery. The treatment of osteoid osteoma can be performed either via open surgery or minimally invasive radiological techniques. Open surgical treatment involves removing the osteoma either through removing the whole intact tumour encased in healthy bone (en bloc) or by using a burr to reach the nidus and using a curette to scrape it out (burr down). While the results of open surgery are good and offer up to 85–100 % success rates, there is an increased risk of infection, nerve injury, tissue damage, postoperative hematomas and other complications related to open surgery [7]. Radiofrequency CT guided thermoablation has been the treatment of choice for smaller osteomas since 1990s, however ablation of intra-articular lesions possess certain challenges such as ablation of non-targeted tissue with articular cartilage damage and increased risk of infection [8]. Instrumental and technical improvement shifts surgical principles towards minimally invasive techniques, therefore there has been a surge in articles reporting arthroscopic removal of intra-articular bony tumours [9], [10], [11]. The arthroscopic approach has not only shown to have success rates up to 100 %, but it also reduces dangers posed by other techniques and offers the benefits of minimally invasive surgery.
Arthroscopic treatment of osteoid osteoma located in the shoulder has been reported before but to our knowledge none with additional osteoma induced pathology or located in the bicipital groove (BG) [12], [13]. The diagnosis and treatment of intra-articular OO is non-specific to population and relevant globally. The rationale of this report is to describe a case of an intra-articular osteoma with osteoma induced adjacent intra-articular shoulder pathology. As well as present an arthroscopic treatment option, which is optimal to address both osteoma and following tendon injury. The manuscript is written according to SCARE 2020 guidelines [14].
2. Case presentation
The case is presented according to SCARE 2020 guidelines, though for the purpose of clean manuscript some information, such as income, education or marital status, as we believe in this case to be irrelevant was not mentioned [14]. A 50-year-old male was referred by a family physician with a prolonged history of dominant, right shoulder pain. The main complaint was shoulder stiffness after physical activity and pain in the anterior joint part. The otherwise healthy individual reported no previous surgical treatment or medication except non steroid anti-inflammatory drugs (NSAIDs) for shoulder pathology. No specific pathology in the family history was described. Social history of the patient revealed recreational smoking, which is not directly linked to osteoma formation, although there is a report of osteoma formation in pharynx of a heavy smoker [15].
The patient was consulted by orthopedic specialists several times before. Although the condition was treated as an overuse pathology with NSAIDs and rest. Since daily activities were not disturbed greatly, the patient did not actively seek additional treatment, which caused a delay to final diagnosis. Clinical findings on physical examination were tenderness in front of the shoulder joint, pain at the mentioned region during extreme external shoulder rotation in abduction with slight limitation of flexion and external rotation due to pain. X-ray radiographs appeared normal (not shown). Based on findings of later magnetic resonance imaging (MRI) osteoma in the BG was diagnosed (Fig. 1). Diagnosis was misleading due to shoulder pain in the anterior region during abduction and external rotation, which is specific for anterior glenoid labrum tear. MRI was appointed to confirm the former diagnosis and rule out co-existing intra-articular pathology, although different working diagnosis of osteoma in the BG was formed. At this point pathology of biceps longus tendon was not confirmed, though suspected since benign tumour was at the tendon tracking region and the tendon was dislocated and oedemic on MRI (Fig. 1).
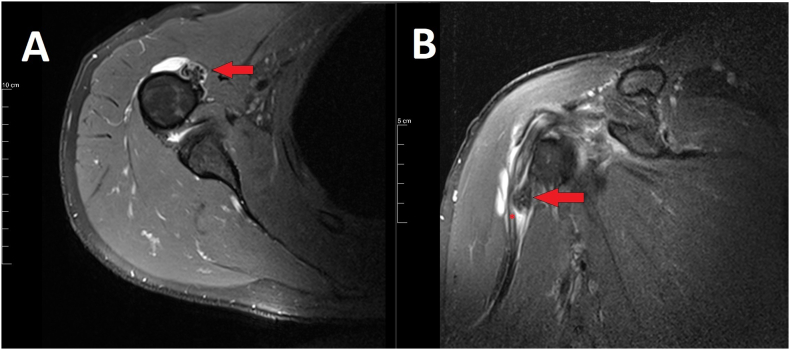
Fig. 1.
Right shoulder magnetic resonance images showing ossified intra-articular osteoma originating from the bicipital groove.
A) Axial proton density-weighted fat-suppressed right shoulder magnetic resonance image. Red arrow – bony formation. Red arrow indicates a well restricted intracortical ~ 0,8 × 0,7 × 1,2 cm formation with high intensity periphery and low intensity central nidus. The findings are typical to osteoid osteomas B) Coronal oblique T2 weighted right shoulder image. Red arrow – bony formation. * - tendon of biceps brachii muscle long head. The formation deforms and dislocates the tendon of m. biceps brachii long head laterally. The tendon is oedemic, fluid stretches are seen along it. The subdeltoid bursae has increased fluid.
3. Intervention
Surgical treatment of OO has great success rates of 85–100 % [13]. Since the OO was located in the shoulder joint, direct visualization during arthroscopy was possible. Additionally during joint examination at the start of every arthroscopy other joint structures can be evaluated, in this case biceps longus tendon, which was potentially damaged. Former mentioned advantages and less risk of joint incision site morbidity was considered, therefore arthroscopic resection of the osteoma was planned.
4. Surgical technique
The surgery was performed by a senior sports trauma and arthroscopy surgeon with a great procedural volume at our University hospital. No specific patient optimization prior to the procedure was required. Shoulder arthroscopy was done under general anesthesia in a beach-chair position, prior to surgery prophylactic dose of 2 g of Cefazolin 30 min before incision was administered. Standard posterior, posterolateral and additional low anterolateral portals were used. Diagnostic arthroscopic findings included a longitudinal tear and dislocation of the biceps longus tendon, which we believe is an outcome of long lasting mechanically induced inflammation at the area of the osteoma (Fig. 4). Additionally, moderate shoulder capsulitis and a partial subscapularis tendon tear were found. Initially the tear of subscapularis was addressed by fixing it to the lesser tubercle with a suture anchor (Corkscrew 5.5 mm) Later on the biceps tendon was inspected from the proximal attachment at the glenoid to the distal bicipital groove (Fig. 2A). At the BG, after the biceps longus tendon was inspected, a longitudinal tear inside the groove was found. Complete separation to a smaller and main part of the tendon was noted (Fig. 2B). Around the area moderate synovitis of the sheet of the tendon was present, most likely due to inflammation caused by mechanical irritation in the osteoma region (Fig. 2C). Facing the tendon with the help of mechanically pushing the instrument a bony spur was felt, which was the MRI verified osteoma (Fig. 3A). After detaching the connective tissue from the bone with electrocautery and an unaggressive shaver a clear vision of the osteoma was established (Fig. 3B–D). Using an arthroscopic burr the bony excrescence was removed extensively (Fig. 4A). At the former site of the osteoma an anchor with two sutures (Corkscrew 5.5 mm) was placed to fix long head of the biceps tendon into the BG (Fig. 4B). The biceps longus tendon was fixed with a knot pusher using standard suture knot technique (Fig. 4C). One end of the blue suture was passed through the lateral side of the main part of the tendon and locked, while the other one was left free, same with the white suture just medial. The tendon was pressed pushing down 7 knots each (Fig. 4D). Afterwards the biceps tendon was cut at the glenoid insertion proximally. No major deviation from initial plan of surgery took place, since biceps longus tendon tear was suspected, except for additional fixation of subscapularis tendon, which did not alter post-operative protocol. Surgical technique alone is not new, though the novelty of the procedure arises from combination of techniques and approach under the main osteoid osteoma diagnosis.
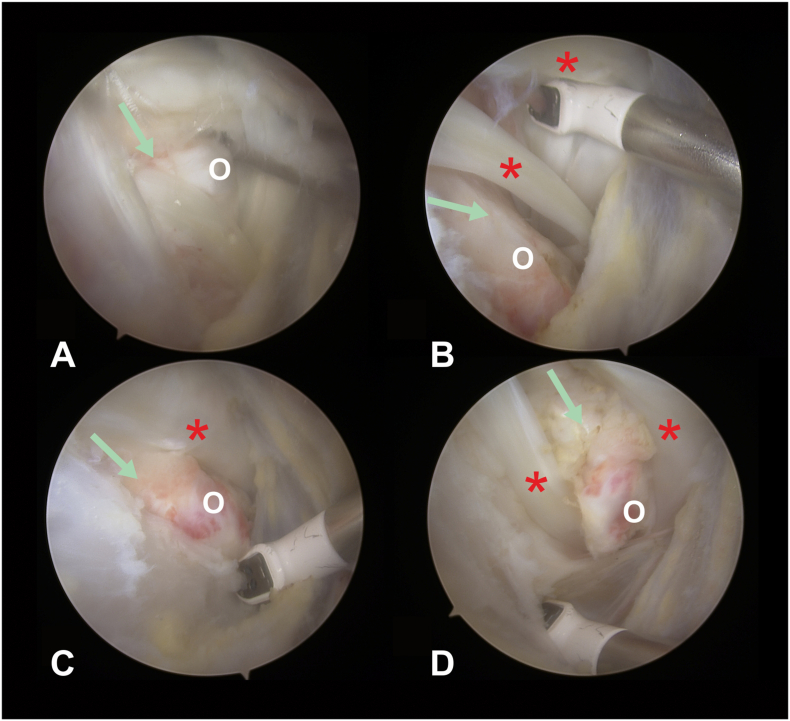
Fig. 4.
Arthroscopic images of the right shoulder in the bicipital groove. All images have been made through posterolateral portal
A) After the bony spur was removed, the site for the suture anchor is prepared B) Two suture Corkscrew 5.5 mm is inserted in the bicipital groove. C) One end of the blue suture was passed through the lateral side of the main part of the tendon and locked, while the other one was left free, same with the white suture just medial. D) The tendon was pressed pushing down 7 knots each. * - tendon of biceps brachii muscle long head, green arrow – direction of the bicipital groove.
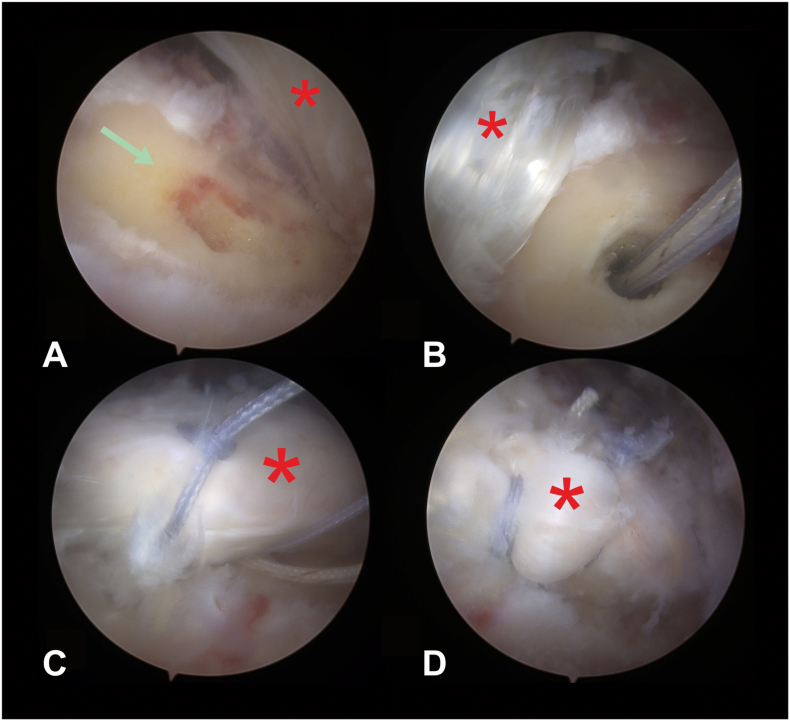
Fig. 2.
Arthroscopic images of the right shoulder with partially injured biceps longus tendon. All images have been made through posterolateral portal.
A) An injured biceps longus tendon is seen. B) An injured and bi-parted biceps tendon is revealed distally. C) Synovitis and inflammation around the area of bony spur is found. * - tendon of biceps brachii muscle long head, HH – humeral head, Ssc – subscapularis muscle tendon. S – Synovitis and inflammation.
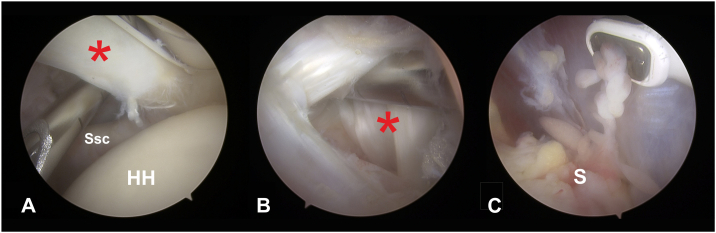
Fig. 3.
Arthroscopic images of the right shoulder at the bicipital groove revealing the osteoid osteoma. All images have been made through posterolateral portal.
A) Bony spur (o) is palpated with electrocautery. B) After detaching the soft tissue, the bony spur (o) is exposed and the bi-parted biceps longus tendon is shown (*). C) Bony spur is further exposed. D) The arthroscopic image indicates the localization of the osteoma relative to biceps tendon. Green arrow – direction of the bicipital groove, * - tendon of biceps brachii muscle long head, O – bony spur, osteoid osteoma.
5. Follow-up and outcomes
The patient was discharged second day after surgery after redressing the surgical wounds and confirming the suture anchor position on X-ray radiographs. After surgery shoulder brace was applied for 4 weeks. From 2 weeks post-operative passive shoulder motion was started to prevent adhesive capsulitis, from 3 weeks active assisted motion was allowed after every session putting the hand back in to the brace. Supervised out-patient physiotherapy was started at 4 weeks after surgery. During the postoperative period NSAIDs were used, cryotherapy was recommended first week after surgery and after every motion session. Follow-up consultation plan consisted of one primary care consultation 2 weeks after surgery to evaluate wound healing and remove sutures, primary physiotherapist consultation at 4 weeks and continuous out-patient physiotherapy for 10 days. Orthopedic consultations at University hospital were scheduled 3 months after surgery and 12 months after surgery to evaluate the course of treatment. The outcome of OO treatment was evaluated based on clinical findings, since X-ray radiographs initially did not reveal the disease it was not informative for outcome as well, except for confirming the desired position of suture anchors early and later after surgery. MRI was not covered by the state health insurance, therefore not performed. We conclude that the patient adherence to recommendations was good based on adherence to follow-up consultations, participation in physiotherapy program and shoulder brace wear. At follow-up 12 months after surgery no complications or adverse outcomes were noted. Clinical outcome was concluded as good based on subsided resting pain or pain in extreme motion, no tenderness in the anterior shoulder and symptom free physical activity. The outcome fulfilled our good expectations, although the patient was informed of a possible recurrence up to 4.5 % even after more than a year after surgery [13].
6. Clinical discussion
The present diagnostic and treatment options for intra-articular osteoid osteoma are relevant. There is research reporting the difficulty of identifying OO as a shoulder pain cause [13]. Malignant shoulder tumours were misdiagnosed as shoulder stiffness in 26 % of cases [3]. Osteoid osteoma is a rare pathology, while intra-articular osteomas consist of even a lesser part of it. Diagnosis is complicated due to indistinctive symptoms which may mimic other articular pathologies and delay the correct diagnosis. An analysis of 140 patients with shoulder stiffness syndrome revealed an incidence of 2.1 % of tumours as a primary stiffness cause [16]. In our presented case not only stiffness was reported after physical activity, but articular pathology induced by osteoma was found, which contributes to the confusing nature of OO diagnosis. MRI and CT scans are considered the optimum methods for diagnosing intra-articular OO, with evidence suggesting computed tomography superior to magnetic resonance imaging [2]. Although MRI enables to evaluate joint structures and in a case of intra-articular osteoma we believe to be superior to rule out other or osteoma induced articular pathologies. The treatment of choice is important as well. Minimally invasive techniques have an advantage due to soft tissue morbidity. Arthroscopic resection of OO provides smaller incision size, less morbidity of surrounding soft tissue and reduces the risk of compromising adjacent neurovascular structures [9], [10], [17]. Endoscopic technique also promotes less scarring with reduced risk of adhesive capsulitis, rapid functional recovery, decreases postoperative morbidity rates and length of hospital stay when compared to open surgery [11], [18], [19]. The success rates of other minimally invasive techniques such as radiofrequency CT guided thermoablation are lower when compared to open surgery or arthroscopic approaches, at 80 % to 90 % [20]. Additionally CT guided ablation poses a risk to damage the cartilage and surrounding joint structures. In a series of case reports only in arthroscopic case group there were no limitation of motion after the surgery [13]. This we believe is related not only to incision site, but to almost a routine procedure of joint synovectomy during arthroscopy. Since adjacent synovitis causing stiffness is reported in multiple case reports with osteoid osteoma [13]. In the particular case the bony spur was localized at the bicipital groove, an accessible place by shoulder arthroscopy. Adjacent pathologies, such as a suspected tear of the biceps longus tendon in this case and ability to evaluate articular structures made arthroscopic treatment ideal. Direct visualization of the tumour is an advantage, to help the surgeon ensure that the entire lesion is thoroughly removed, consequently minimizing recurrence rates [10], [20]. In this case, as we believe osteoid osteoma at the bicipital groove induced mechanical inflammation and damage to the biceps longus tendon, which could not have been subtly addressed without arthroscopic treatment.
Currently only around 6.3 % of intra-articular osteoid osteomas are treated arthroscopically [21]. Emphasis on treating intra-articular OO arthroscopically in the hip, ankle and knee joints has already been established and report excellent outcomes [10], [11], [20]. Successful arthroscopic treatment of shoulder intra-articular OO have been reported, although none with osteoma induced articular pathology or located at BG [12], [13] Presented case report supports arthroscopic osteoid osteoma treatment with description of various advantages and good clinical results. Strengths and weaknesses of the case are presented in Table 1.
Table 1.
Strengths and Weaknesses of the presented case.
| Strengths |
|
| Weaknesses and limitations |
|
7. Conclusion
In this particular case MRI has been advantageous in discovering co-existing intra-articular structural damage to intra-articular osteoid osteoma. Arthroscopic intra-articular osteoma resection in shoulder joint was optimal to address adjacent osteoma induced pathology, reduce incision site complication rates, achieve great visualization and good results. Additional synovectomy during arthroscopic treatment can be performed, due to concomitant synovitis causing joint stiffness in most reported intra-articular OO cases.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Case report studies are exempt of ethical approval at our institution.
Funding
The study received no funding.
Guarantor
All authors have given the final approval of the version to be published and agree to be accountable for all aspects of the work.
Research registration number
N/a.
CRediT authorship contribution statement
R.G. – study design, operating surgeon, revision of manuscript. M.S., A.R. – acquisition of data, drafting the manuscript., A.S. – intellectual data interpretation, revision of manuscript.
Conflicts of interest
Authors declare to have no conflict of interest. Each author confirms to have no commercial relations regarding the subject presented.
References
- 1.Noordin S., Allana S., Hilal K., Nadeem N., Lakdawala R., Sadruddin A., Uddin N. Osteoid osteoma: contemporary management. Orthop. Rev. (Pavia) 2018;10:108–119. doi: 10.4081/or.2018.7496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allen S.D., Saifuddin A. Imaging of intra-articular osteoid osteoma. Clin. Radiol. 2003;58:845–852. doi: 10.1016/S0009-9260(03)00213-7. [DOI] [PubMed] [Google Scholar]
- 3.Sano H., Hatori M., Mineta M., Hosaka M., Itoi E. Tumors masked as frozen shoulders: a retrospective analysis. J. Shoulder Elb. Surg. 2010;19:262–266. doi: 10.1016/j.jse.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 4.Rosenthal D.I., Springfield D.S., Gebhardt M.C., Rosenberg A.E., Mankin H.J. Osteoid osteoma: percutaneous radio-frequency ablation. Radiology. 1995;197:451–454. doi: 10.1148/radiology.197.2.7480692. [DOI] [PubMed] [Google Scholar]
- 5.Weber K.L., Morrey B.F. Osteoid osteoma of the elbow: a diagnostic challenge. J. Bone Jt. Surg. 1999;81:1111–1119. doi: 10.2106/00004623-199908000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Cohen M.D., Harrington T.M., Ginsburg W.W. Osteoid osteoma: 95 cases and a review of the literature. Semin.Arthritis Rheum. 1983;12:265–281. doi: 10.1016/0049-0172(83)90010-0. [DOI] [PubMed] [Google Scholar]
- 7.Lee E.H., Shafi M., Hui J.H.P. Osteoid osteoma: a current review. J. Pediatr. Orthop. 2006;26:695–700. doi: 10.1097/01.bpo.0000233807.80046.7c. [DOI] [PubMed] [Google Scholar]
- 8.Motamedi D., Learch T.J., Ishimitsu D.N., Motamedi K., Katz M.D., Brien E.W., Menendez L. Thermal ablation of osteoid osteoma: overview and step-by-step guide. Radiogr. a Rev. Publ. Radiol. Soc. North Am. Inc. 2009;29:2127–2141. doi: 10.1148/rg.297095081. [DOI] [PubMed] [Google Scholar]
- 9.Gudas R., Pocius A. Endoscopic removal of the osteochondroma of the fibular head. Medicina (Kaunas) 2013;49:191–194. [PubMed] [Google Scholar]
- 10.Furukawa M., Anazawa U., Horiuchi K., Yabe H., Morioka H., Mukai M., Toyoda T., Chiba K., Shiraishi T., Toyama Y. Arthroscopic removal of intra-articular osteoid osteoma in the knee: case report and review of the literature. J. Orthop. Sci. 2011;16:321–325. doi: 10.1007/s00776-011-0060-4. [DOI] [PubMed] [Google Scholar]
- 11.Marwan Y.A., Abatzoglou S., Esmaeel A.A., Alqahtani S.M., Alsulaimani S.A., Tanzer M., Turcotte R.E. Hip arthroscopy for the management of osteoid osteoma of the acetabulum: a systematic review of the literature and case report. BMC Musculoskelet. Disord. 2015;16:1–7. doi: 10.1186/s12891-015-0779-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kelly A.M., Selby R.M., Lumsden E., O’Brien S.J., Drakos M.C. Arthroscopic removal of an osteoid osteoma of the shoulder. Arthrosc. J. Arthrosc. Relat. Surg. 2002;18:801–806. doi: 10.1053/JARS.2002.35268. [DOI] [PubMed] [Google Scholar]
- 13.Glanzmann M.C., Imhoff A.B., Schwyzer H.K. Osteoid osteoma of the shoulder and elbow: from diagnosis to minimally invasive removal. Int. Orthop. 2013;37:2403–2408. doi: 10.1007/s00264-013-2060-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 15.Angelillo M., Mazzone S., Costa G., Mazzone A., Barillari U. The first case of osteoma in the false vocal fold. Auris Nasus Larynx. 2009;36:235–238. doi: 10.1016/j.anl.2008.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Demazière A., Wiley A.M. Primary chest wall tumor appearing as frozen shoulder. Review and case presentations. J. Rheumatol. 1991;18:911–914. [PubMed] [Google Scholar]
- 17.Goyal S., Said H.G. Osteoid osteoma (OO) of the coracoid: a case report of arthroscopic excision and review of literature. Sicot-J. 2015;1:1–5. doi: 10.1051/sicotj/2015016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bojanić I., Rogošić S., Mahnik A., Smoljanović T. Removal of osteoid osteoma of the tibia using two-portal posterior ankle arthroscopy. J. Foot Ankle Surg. 2012;51:103–105. doi: 10.1053/j.jfas.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 19.David P., Legname M., Dupond M. Arthroscopic removal of an osteoid osteoma of the talar neck. Orthop. Traumatol. Surg. Res. 2009;95:454–457. doi: 10.1016/j.otsr.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Ge S.M., Marwan Y., Addar A., Algarni N., Chaytor R., Turcotte R.E. Arthroscopic Management of Osteoid Osteoma of the ankle joint: a systematic review of the literature. J. Foot Ankle Surg. 2019;58:550–554. doi: 10.1053/j.jfas.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 21.Jordan R.W., Koç T., Chapman A.W.P., Taylor H.P. Osteoid osteoma of the foot and ankle-a systematic review. Foot Ankle Surg. 2015;21:228–234. doi: 10.1016/j.fas.2015.04.005. [DOI] [PubMed] [Google Scholar]