Abstract
Objective
To study patterns of antidepressant, anxiolytic, and hypnotic drug utilization in Denmark, Norway, and Sweden during the first year of the COVID-19 pandemic.
Methods
The monthly observed number of prescription fills of antidepressants, benzodiazepines and benzodiazepine-related hypnotics (BZ), and other anxiolytics and hypnotics (OAH) per population in 2020 were compared with predicted numbers based on analysis of covariance of prescription fills during 2015–2019.
Results
In March 2020, there was an increased number of prescription fills for antidepressants, anxiolytics, and hypnotics in youths and adults aged 20–59 years in Denmark, Norway, and Sweden. Antidepressant prescription fills increased between 13.5 % and 31.3 % at the end of 2020 in all age groups in Denmark and 17.4 % in youths in Norway. BZ drug prescription fills increased by 20.8 % at the end of 2020 in the 20–59 year age group in Denmark and decreased by 16.7 % in youths in Sweden. A general increase of prescription fills of OAH at the end of 2020 was observed in all countries (range 24.0–80.0 % in Denmark, 11.5–30.8 % in Norway, and 9.1–12.1 % in Sweden). Increases of prescription fills of OAH occurred earlier in Denmark.
Limitations
Aggregated data with lack of information on indications.
Conclusions
Peaks of utilization of antidepressants, anxiolytics, and hypnotics observed in March 2020 may reflect medication stock piling. Increased antidepressant drug utilization in Denmark and in Norwegian youths together with the general increase in OAH utilization in the Scandinavian countries in late 2020 may indicate an increase of symptoms of depression and anxiety, as well as disturbed sleep.
Keywords: Drug utilization, Antidepressants, Anxiolytics, Benzodiazepines, Hypnotics, COVID-19
1. Introduction
On 11 March 2020, WHO declared that the spread of the new coronavirus SARS-CoV-2 (Severe acute respiratory syndrome coronavirus 2) constituted a pandemic. During the first wave of viral spread most countries implemented lockdowns to reduce COVID-19 transmission (Lau et al., 2020; Pulla, 2020; Thornton, 2020). In Scandinavia, Norway and Denmark followed suit and imposed lockdowns and school closures. Sweden, however, remained comparatively open and schools were never closed, although upper secondary school education was held online during the initial pandemic phase (Ludvigsson, 2020). Lockdowns seem to affect mental health and increase symptoms of depression and anxiety in particular (Prati and Mancini, 2021). It is, however, difficult to disentangle the consequences of the lockdown from that of the pandemic itself, as associations between daily SARS-CoV-2 infection rates and prevalence of major depressive disorders and anxiety disorders have been reported (Covid- Mental Disorders Collaborators, 2021). Furthermore, poor sleep has been reported post COVID-19 infections (Ahmed et al., 2021). There is also a concern regarding psychiatric consequences of school closures on students (Meherali et al., 2021). Schools are seen as microsystems that provide an age adapted environment promoting development and mental health (Bronfenbrenner, 1977), which may be disrupted in case of school closure. Everyday life of children and adolescents has thus been particularly affected by COVID-19 mitigation measures, such as school closures in Denmark and Norway, and online education in upper secondary schools. Previous viral outbreaks have also demonstrated higher levels of psychological distress among health care workers exposed to affected patients (Kisely et al., 2020). Furthermore, as older age increases risk of serious outcomes of COVID-19 (Grasselli et al., 2020), recommendations of social distancing have been most strict for the elderly in all Scandinavian countries. Visits to nursery homes were restricted in the beginning of the pandemic, resulting in isolation of this group of the elderly.
It is evident that the COVID 19 pandemic has a profound effect on societies (Holmes et al., 2020), and that it therefore may lead to an increase in stress, and thereby potentially the risk of anxiety and depression in the population (Risch et al., 2009). Utilization of antidepressant and anxiolytic drugs can be seen as a proxy for the prevalence of depressive symptoms and anxiety in a population. Antidepressant drug utilization during national crisis such as economic recession has been examined (Kozman et al., 2012), but the impact of previous pandemics on prescription fills of antidepressants and anxiolytics has not been studied. During the COVID-19 pandemic, the number of first filled antidepressant prescriptions in primary care was reduced in the United Kingdom in April 2020 (Carr et al., 2021), and similarly in Germany a small reduction of antidepressant and benzodiazepine prescriptions for patients with anxiety disorder was noted during March till June 2020 (Jacob et al., 2020). By contrast, a small increase in prescriptions of selective serotonin reuptake inhibitors (SSRI) and tricyclic antidepressants was observed in England overall, compared to the previous year (Rabeea et al., 2021). Moreover, increased monthly prescribing of SSRI, serotonin and norepinephrine reuptake inhibitors, and benzodiazepine-related hypnotics in the United States of America during the time period between January and autumn 2020 has been reported (Milani et al., 2021). Thus, previous studies have not provided consistent patterns regarding the impact of the COVID-19 pandemic on utilization of drugs for treatment of depression, anxiety, and sleep disorders.
The purpose of this study was to examine the monthly utilization of antidepressants, anxiolytics, and hypnotics using nationwide population-based data from Denmark, Norway, and Sweden during 2020, the first year of the COVID-19 pandemic, compared to 2015–2019.
2. Materials and methods
Prescription fills were used as proxies for drug utilization. Aggregated data on pharmacy prescriptions, including number of prescription fills and volume dispensed (defined daily doses (DDD) per week in Sweden and per month in Denmark and Norway), were collected from January 1, 2015 to December 31, 2020 for the total populations of Sweden, Norway and Denmark and stratified into the following age groups: 0–19 years, 20–59 years, and from 60 years old and above. Data were collected from the Swedish National Board of Health and Welfare, the Norwegian Prescription Database, and the Danish National Prescription Registry. Data were provided with World Health Organization Anatomical Therapeutic Chemical (ATC) classification codes for three groups: antidepressants (ATC codes: N06AA, N06AB, N06AF, N06AG, N06AX), benzodiazepines and benzodiazepine-related hypnotics (BZ; ATC codes: N05BA, N05CD, N05CF), and other anxiolytics and hypnotics (OAH; ATC codes: N05BB, N05CM, N05CH, R06AD), see Supplementary table for more detailed information on the included ATC codes. The BZ group is a scheduled drug group, set apart from the other two groups by requiring special prescriptions as drugs of abuse potential.
The total population numbers of Denmark, Norway, and Sweden per year and age strata were obtained from the Statistics Denmark, Statistics Norway, and Statistics Sweden websites. In Sweden, the Medical Products Agency implemented a restriction in the amount medication that could be dispensed per patient on Wednesday April 1st, 2020, and therefore, weeks were started on a Wednesday in the Swedish data. The number of prescription fills and DDDs per 100,000 inhabitants and day in each month or 4-week period were calculated based on ATC codes.
2.1. Statistical analyses
The average number of prescription fills per 100,000 inhabitants by age group and drug group in Denmark, Norway, and Sweden during 2020 was compared with 2015–2019. An Analysis of Covariance (ANCOVA) model was used to predict the expected number of prescription fills and the volume of DDDs dispensed in 2020 based on data from 2015 to 2019. To achieve comparability between countries, the Swedish data was summed over 4 weeks, as the original data from Sweden were counts per week, while the data from Denmark and Norway were counts per month. The model included the following variables: 1) the date as a continuous variable to model linear change of drug use over time, 2) a categorical time period (month or 4-weeks period) variable to model seasonal patterns, and 3) a continuous variable for number of working days (including Saturdays) in each time period to model other holidays. This last element was included because in many non-metropolitan regions pharmacies are not open on Sundays and other holidays. Observations for each month/4-weeks period in 2020 were then compared to the predicted value based on data from 2015 to 2019, including 95 % confidence limits (CLs) for individual predictions. In the figures, multiplicity concerning the many 4-weekly and monthly comparisons within a drug group, but not across drug groups, is applied by dividing the standard significance limits by 12 or 13 (i.e., Bonferroni correction based on the number of months or four weeks periods of data in 2020). In the text, all p-values are Bonferroni corrected (multiplied by 12 or 13). All calculations were performed in SAS version 9.4 and SAS/STAT 14.3.
2.2. Ethics
All data in this study are publicly available in Denmark, Norway, and Sweden, and approval from any data protection agency or ethical review board was therefore not required.
3. Results
Drug dispensation rates differed markedly between Denmark, Norway, and Sweden during the reference period 2015–2019 (Table 1 ), when the average number of prescription fills of antidepressants per 100,000 inhabitants per day was higher in Sweden (178, range in different age groups: 15–392) than in Denmark (110, range: 6–227) and Norway (94, range: 5–214). Daily BZ prescription fills per 100,000 inhabitants were higher in Norway (147, range: 4–395) and Sweden (159, range: 3–412) than in Denmark (59, range: 2–153). OAH prescription fills per 100,000 inhabitants per day were highest in Sweden (68, 28–93), followed by Norway (38, 16–64), while the lowest dispensation rates were found in Denmark (11, 8–18).
Table 1.
Demographic data and number of prescription fills per day.
| Age group | 2015–2019 |
2020 |
|||||
|---|---|---|---|---|---|---|---|
| Denmark | Norway | Sweden | Denmark | Norway | Sweden | ||
| Population size | All ages | 5,740,601 | 5,252,387 | 9,987,618 | 5,822,763 | 5,367,580 | 10,327,589 |
| 0–19 years | 1,309,228 | 1,259,752 | 2,289,467 | 1,296,400 | 1,248,749 | 2,403,730 | |
| 20–59 years | 2,997,244 | 2,820,794 | 5,158,372 | 3,026,001 | 2,869,792 | 5,290,102 | |
| >60 years | 1,434,129 | 1,171,841 | 2,539,780 | 1,500,362 | 1,249,039 | 2,633,757 | |
| Prescription fills per 100,000 inhabitants | |||||||
| Antidepressants | All ages | 110 | 94 | 178 | 106 | 98 | 195 |
| 0–19 years | 6 | 5 | 15 | 7 | 6 | 20 | |
| 20–59 years | 99 | 83 | 141 | 98 | 89 | 155 | |
| ≥60 years | 227 | 214 | 392 | 206 | 212 | 429 | |
| Benzodiazepines and benzodiazepine-related hypnotics | All ages | 59 | 147 | 159 | 44 | 143 | 141 |
| 0–19 years | 2 | 4 | 3 | 2 | 4 | 3 | |
| 20–59 years | 39 | 108 | 99 | 27 | 103 | 82 | |
| ≥60 years | 153 | 395 | 412 | 114 | 373 | 377 | |
| Other anxiolytics and hypnotics | All ages | 11 | 38 | 68 | 18 | 48 | 84 |
| 0–19 years | 8 | 16 | 28 | 14 | 26 | 43 | |
| 20–59 years | 10 | 37 | 73 | 16 | 45 | 93 | |
| ≥60 years | 18 | 64 | 93 | 25 | 75 | 104 | |
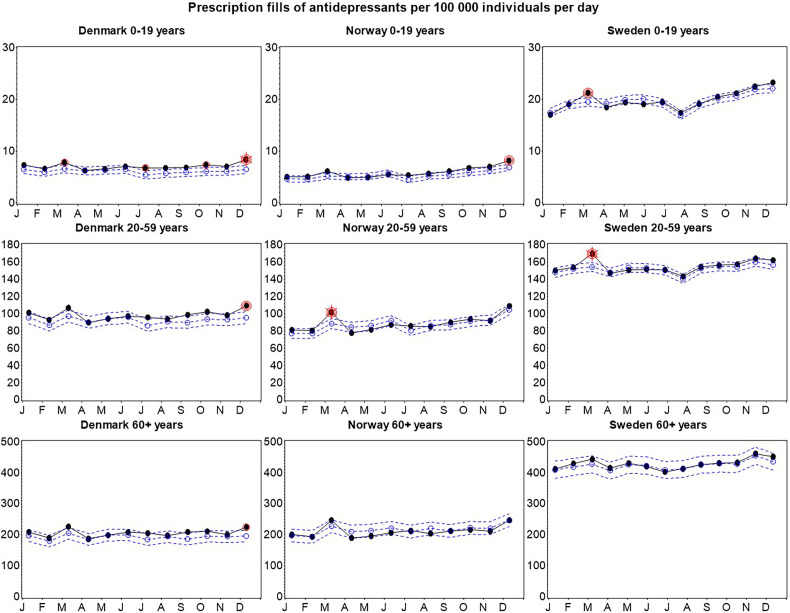
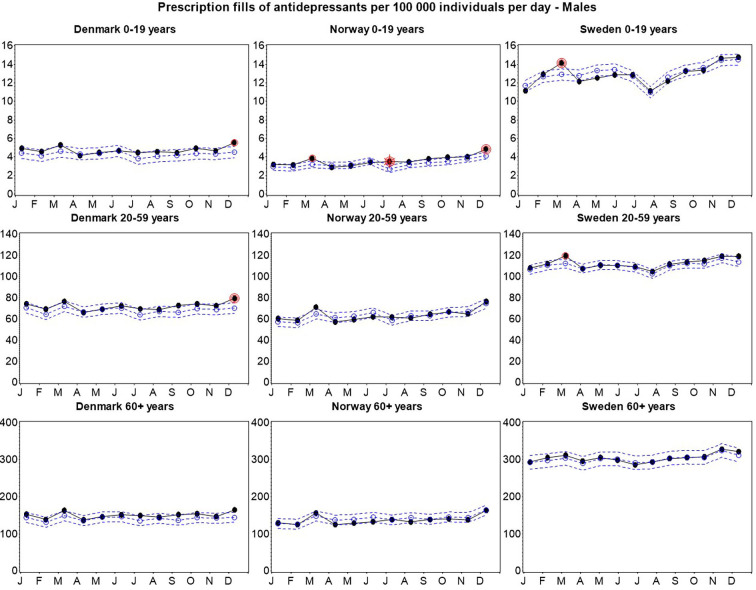
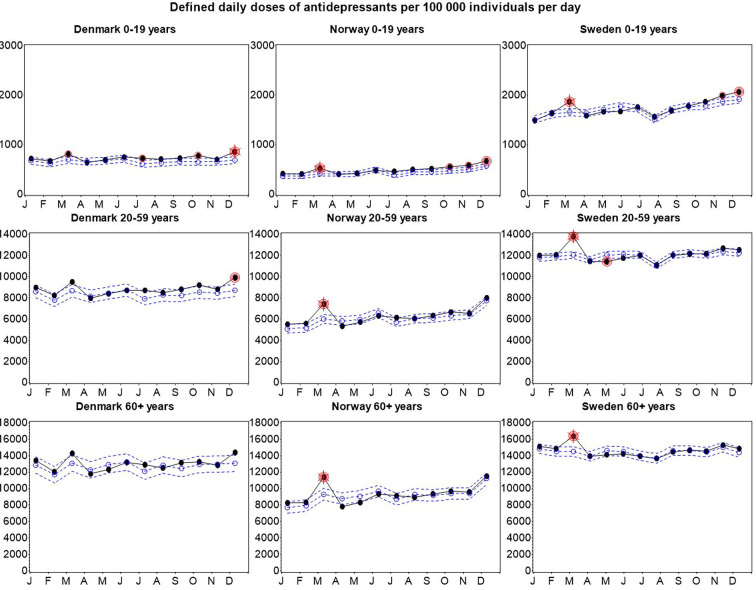
Compared with 2015–2019, the number of antidepressant prescription fills during 2020 was higher than predicted in the month of March for individuals aged 20–59 years in Norway (14.6 %, p < 0.001), and Sweden (9.7 %, p < 0.001) and in youths in Denmark (18.2 %, p = 0.040) and Sweden (5.0 %, p = 0.001) (Fig. 1 ). In December 2020, antidepressant prescription fills were higher in youths in Denmark (31.3 %, p < 0.001) and Norway (17.4 %, p = 0.001), and in Denmark prescription fills were also higher than predicted among 20–59 year-olds (13.5 %, p = 0.0026) and the 60+ year group (14.8 % increase, p = 0.037). Danish youths also had higher prescription rates in July (24.1 %, p = 0.013) and October (21.3 % increase, p = 0.018) 2020.
Fig. 1.
Observed versus predicted number of prescription fills per 100,000 population and day of antidepressants in Denmark, Norway, and Sweden 2020. Solid black line = observed values; dotted blue line with open circles = predicted values; dotted blue lines no marker = upper and lower 95 % confidence limits. p-Values that remain significant after Bonferroni correction are marked; single red circle = 5 % significance level; double red circle = 1 % significance level; double red circle with star = 0.1 % significance level. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
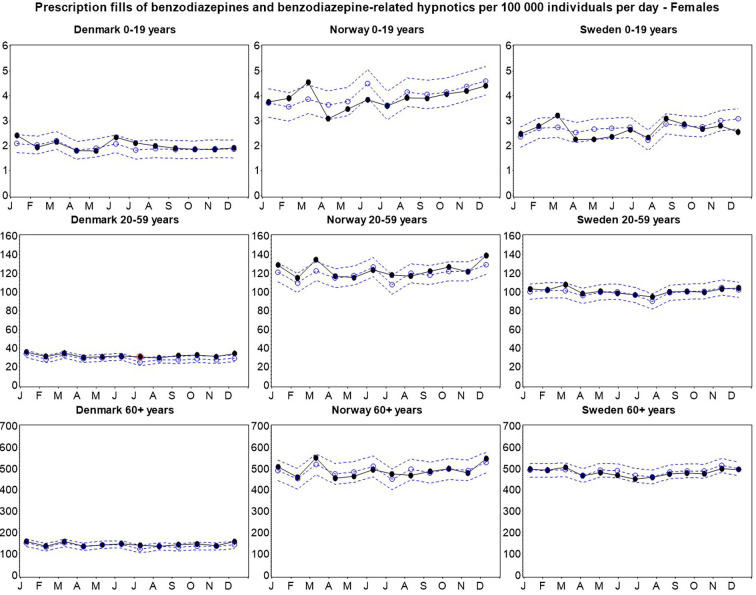
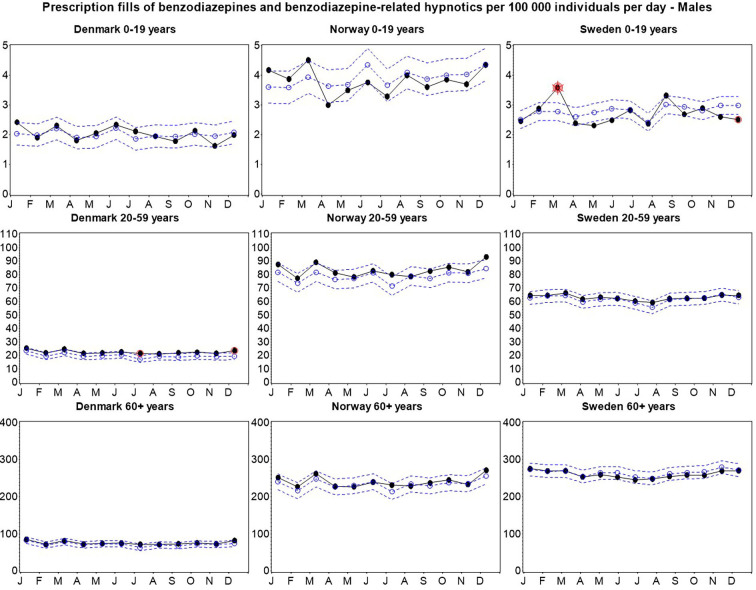
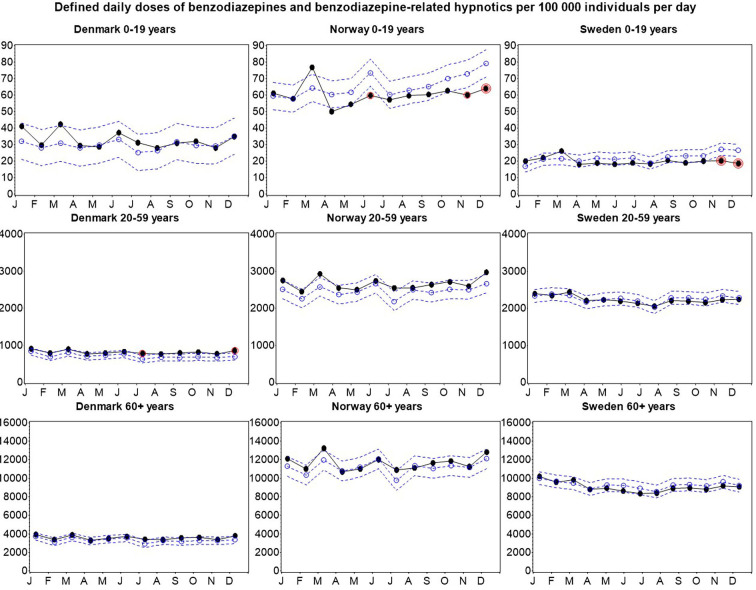
The number of BZ prescription fills were higher than predicted among Swedish youths (21.4 %, p = 0.0027) in March 2020, whereas the rates were lower than predicted for this group in December 2020 (16.7 %, p = 0.042) (Fig. 2 ). In Denmark, prescription fills were higher than predicted among individuals aged 20–59 years during July (23.8 %, p = 0.0276) and December 2020 (20.8 %, p = 0.043).
Fig. 2.
Observed versus predicted number of prescription fills per 100,000 population and day of BZ in Denmark, Norway, and Sweden 2020. Solid black line = observed values; dotted blue line with open circles = predicted values; dotted blue lines no marker = upper and lower 95 % confidence limits. p-Values that remain significant after Bonferroni correction are marked: single red circle = 5 % significance level; double red circle = 1 % significance level; double red circle with star = 0.1 % significance level. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
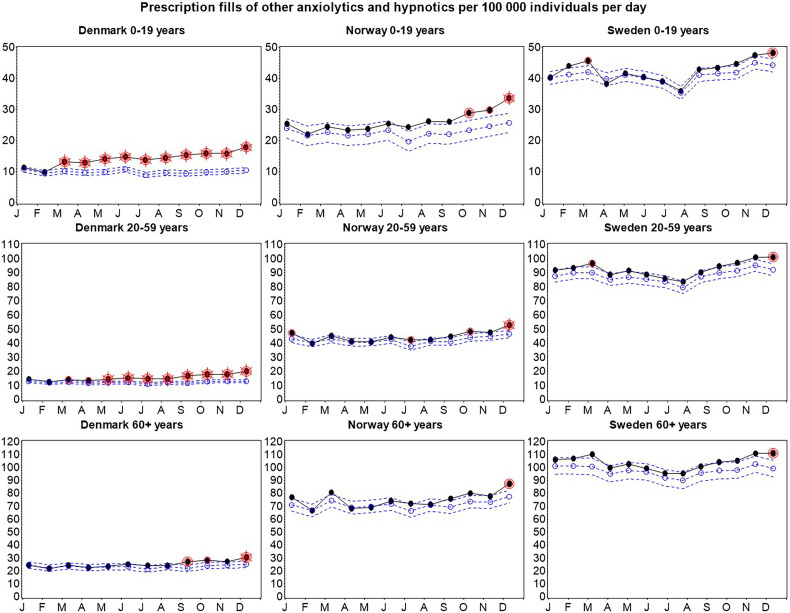
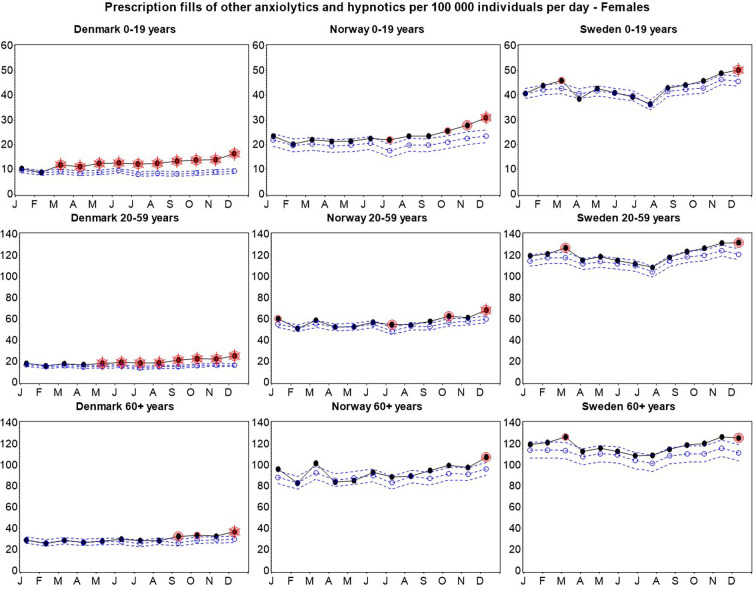
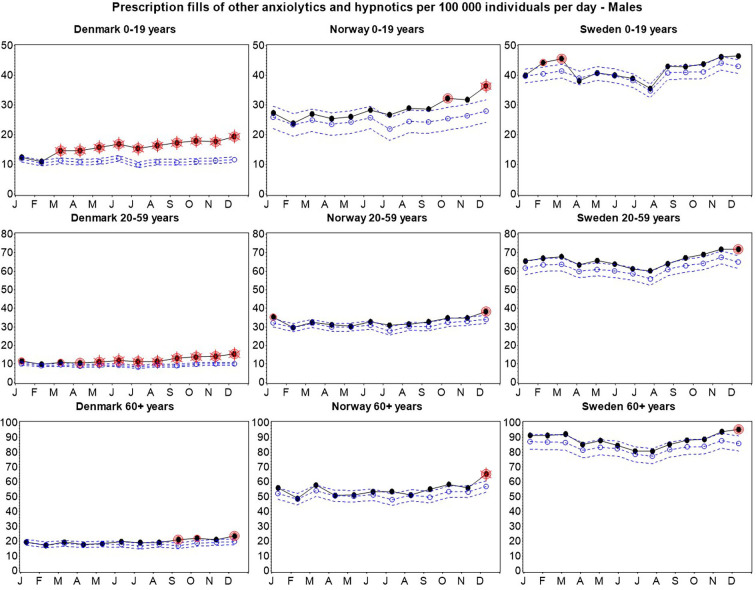
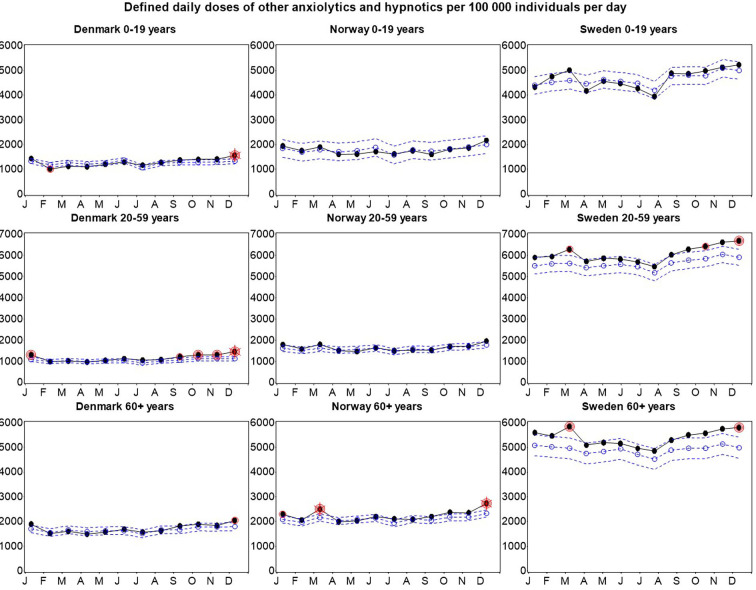
Prescription fills of other anxiolytics and hypnotics (OAH) were higher than predicted in March 2020 among Swedish youths (9.5 %, p = 0.013) and Swedish individuals aged 20–59 years (with 7.8 %, p = 0.034) (Fig. 3 ). A similar pattern was observed in Denmark, with higher numbers of prescription fills among youths (30.0 %, p < 0.001) and individuals aged 20–59 years (7.7 %, p = 0.034) in March 2020. Furthermore, in these age groups in Denmark, an incremental increase in the number of OAH prescription fills was found during the rest of 2020 with distinctly higher numbers of prescription fills in December 2020 (80 %, p < 0.001, and 53.8 %, p < 0.001, respectively). In all age groups and countries, OAH prescription fills increased at the end of 2020, reaching the highest number of prescription fills of the year in December (ranges of increase in December 2020: Denmark: 24.0–80.0 %, Norway: 11.5–30.8 %, Sweden: 9.1–12.1 %).
Fig. 3.
Observed versus predicted number of prescription fills per 100,000 population and day of OAH in Denmark, Norway, and Sweden 2020. Solid black line = observed values; dotted blue line with open circles = predicted values; dotted blue lines no marker = upper and lower 95 % confidence limits. p-Values that remain significant after Bonferroni correction are marked: single red circle = 5 % significance level; double red circle = 1 % significance level; double red circle with star = 0.1 % significance level. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
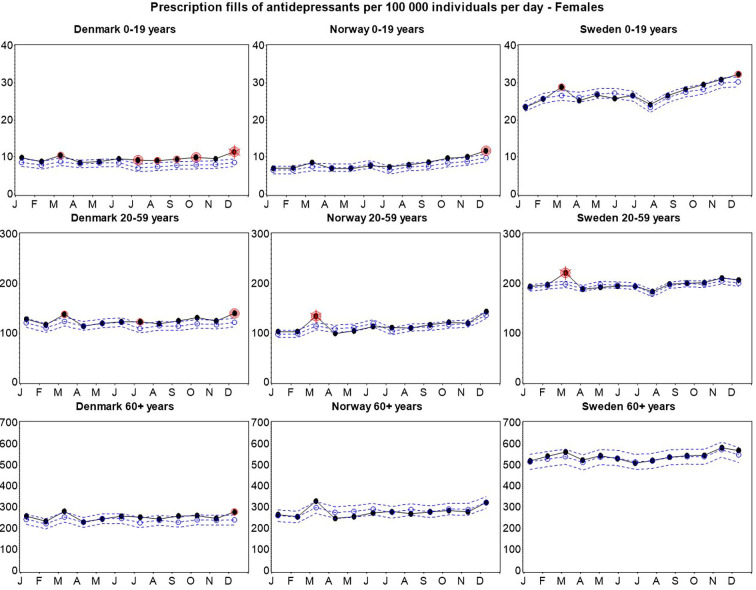
Overall, prescription fills for antidepressants and OAH in 2020 followed the same patterns for males and females as in the combined groups for each country (Fig. S1). However, there was a 6.7 % increase in antidepressant prescriptions among Swedish female youths in December 2020 (p = 0.044), which was not observed among males. The statistically significant differences in BZ prescription fills during 2020 on the other hand, were only found among males.
Supplementary Fig. 1.
Prescription fills of antidepressants, benzodiazepines and benzodiazepine-related hypnotics, and other anxiolytics and hypnotics per 100,000 individuals per day in females and males.
3.1. Defined daily doses
Prescription patterns in terms of DDDs dispensed for antidepressants and other anxiolytics and hypnotics during 2020 were similar to that of the prescription fills (Fig. S2). DDDs of the BZ drug groups were lower than predicted at the end of 2020 among youths in Norway (19.0 %, p = 0.0068) and Sweden (33.3 %, p = 0.001), whereas BZ DDDs were higher than predicted among Danish individuals aged 20–59 years in July (24.7 %, p = 0.035) and December (22.7 %, p = 0.026).
Supplementary Fig. 2.
Defined daily doses of antidepressants, benzodiazepines and benzodiazepine-related hypnotics, and other anxiolytics and hypnotics per 100,000 individuals per day.
4. Discussion
During the first year of the COVID-19 pandemic, we observed an increased utilization of drugs for treatment of depression, anxiety, and sleep disorders in Scandinavia compared to what was predicted based on the preceding five-year period. Firstly, we observed increases in prescription fills in all drug groups in March 2020. Secondly, there was a general increase in utilization of OAH drugs by the end of 2020, which started earlier in Denmark. Finally, antidepressant drug utilization increased at the end of 2020 in Denmark and in Norwegian youths.
In March 2020, we observed local peaks of antidepressant, BZ, and OAH prescription fills. March 2020 was in many ways the first month of the COVID-19 pandemic in Scandinavia. Similar local peaks of dispensations have been observed in Sweden for a wide variety of drugs at that time, with distinct increases particularly in the second week of March 2020 (Karlsson et al., 2021). For comparison, an increase of dispensed defined daily doses of drugs of ATC class C, including antihypertensives, during mid-February to mid-March 2020 was observed in Sweden, indicating hoarding of medications (Karlsson et al., 2021). During the rest of 2020 class C-drugs were dispensed as predicted in Sweden. Furthermore, the number of primary health care and psychiatric emergency visits in Sweden was reduced in Spring 2020 (Flygare et al., 2020; National Board of Health and Welfare, 2020). With this reduced health care utilization together with a general trend of hoarding of drugs during March 2020, the high numbers of antidepressant, BZ and OAH prescription fills during this month most likely reflect medication stock piling (Karlsson et al., 2021).
While the high numbers of prescription fills in March normalized in April 2020 for most groups, AOH prescription fills in Danish youths and individuals aged 20–59 years continued to increase over the rest of this year. There was no introduction of new OAH drugs or national guidelines in Denmark during 2020 that could possibly explain the increase in OAH prescription fills. It is worth noting that the increases in OAH drug prescription fills started earlier the lower the country's prepandemic dispensation rates, which was lowest in Denmark, higher in Norway and highest in Sweden. With lower prepandemic rates of prescriptions fills, any changes in prescription patterns may have relatively larger impact, although our model adjusted for the trend based on the number of prescription fills per population during the preceding five year period in each group. The reason for these prepandemic differences in prescription patterns is not clear. A previous finding of differences in health care between countries is the larger number of child psychiatrists per population in Sweden compared with Denmark (Signorini et al., 2017), which could have an impact on the number of drug prescriptions. Interestingly, larger use of antipsychotics per population, predominantly of the sedative quetiapine, in Denmark compared to Norway and Sweden has been reported (Halfdanarson et al., 2017; Hojlund et al., 2019). However, there may also be an effect of lockdowns on depressive symptoms, anxiety, and sleep. Denmark stands out among the Scandinavian countries with repeated lockdowns during 2020, implemented in March as well as in December, while the only lockdown in Norway was in the spring of 2020, and Sweden did not impose any lockdown during 2020. Even though the long term effects of lockdowns on sleep and anxiety are not known, higher prevalence of anxiety, insomnia, and poor sleep quality has been reported in online surveys during lockdown in Italy (Casagrande et al., 2020; Cellini et al., 2020; Gualano et al., 2020) and China (Liu et al., 2020). However, with the exception of patients aged 20–59 years in Denmark, utilization of BZ drugs, also used to alleviate anxiety and poor sleep, did not increase from April to December 2020, and among youths in Sweden BZ drug utilization was even reduced in December 2020. A possible explanation for this may be that in contrast to OAH prescriptions, BZ drugs require special prescriptions in Denmark, Norway, and Sweden, meaning that to a larger extent visiting a prescriber is necessary, while OAH drugs may more easily be prescribed after remote consultations. Thus, with reduced utilization of in person health care during the COVID-19 pandemic, the limited BZ utilization changes do not necessarily contradict the observed increases in OAH drug utilization during 2020.
Denmark also stands out as the only country with a general increase in antidepressant utilization at the end of 2020, while increased antidepressant utilization was confined to children and adolescents in Norway, and there was no significant antidepressant utilization increase in Sweden. However, prepandemic antidepressant drug utilization in Sweden was roughly twice as high in Sweden than in Denmark and Norway. Still, it is possible that lockdowns may have led to increased antidepressant drug utilization. From what we know so far into the current pandemic, there appears to be a certain increased risk of depressive symptoms in people experiencing lockdowns (Prati and Mancini, 2021). The increase in antidepressant drug utilization observed in Denmark and in Norwegian youths at the end of 2020 could possibly reflect a part of the population suffering from a deteriorating mental health over time following nationwide lockdown, as have been observed in the UK Household Longitudinal study (Pierce et al., 2021). However, the knowledge on the mental health impact of repeated lockdowns is limited, although reports on weariness of restrictions to limit viral spread, known as pandemic fatigue, are becoming more frequent (Reicher and Drury, 2021). Moreover, there may also be a direct impact of SARS-CoV-2 infections on depressive symptoms (Renaud-Charest et al., 2021).
Increased antidepressant drug utilization in youths was observed by the end of 2020, both in Denmark and Norway. The higher than predicted antidepressant drug utilization during late 2020 could reflect increases in depressive and anxiety symptoms in children and adolescents, which has been demonstrated in a meta-analysis of the global mental health impact of the COVID-19 pandemic (Racine et al., 2021). In this study, elapsed time since onset of the pandemic affected the results, with more pronounced increases of depressive and anxiety symptoms the further into the pandemic each individual study was conducted (Racine et al., 2021). This could support the explanation that the increased antidepressant drug utilization we observed in youths in Denmark and Norway at the end of 2020 reflects increased depressive symptoms in these groups. In Denmark, Norway, and Sweden upper secondary school education has been affected by mitigation measures, but only Denmark and Norway implemented full scale school closures. Poorer mental health has been reported in older children in remote schooling compared with in-person schooling (Hawrilenko et al., 2021). Moreover, increased depressive symptoms after school closing related to COVID-19 has been observed in Chinese primary school children (Zhang et al., 2020).
An important question that needs to be addressed with longitudinal clinical studies is whether the increase in antidepressant and OAH prescription fills at the end of 2020 is an early predictor of an increase in anxiety, depression, and sleep disorders in the wake of the pandemic or reflects a temporary mental health impact of the lockdown or similar mitigation measures, which will subside after lockdown. Longitudinal studies comparing the prevalence of depressive, anxiety, and sleep disorders before the pandemic with the other half of 2020 are needed to understand whether the increases in OAH and antidepressant drug prescription fills late 2020 are related to deteriorated mental health in the Scandinavian populations.
4.1. Strengths and limitations
In the included Scandinavian countries, nation-wide data on prescription fills are available, as sales must be regularly reported to the authorities according to law, which is a major strength of the study. The availability of data from 2015 to 2019 for comparisons also strengthens the study. In the statistical analyses we were able to take into account underlying time trends for the use of the respective drugs over the six year period, although a potential limitation is that the model applied was based on the assumption that prescription fills over time can be described as a linear function. Moreover, prescription fills were used as proxies for medication use and we lacked information on treatment indication and to what degree the increases seen were due to drugs dispensed to new (incident) users or to patients who already had a prescription. Filled prescriptions are considered superior to medical record and questionnaire information (Furu et al., 2010) and are more indicative of use than prescriptions alone as there may be a considerable proportion of primary non-adherence to class-N drugs (Pottegard et al., 2014), but they are only a proxy for actual consumption. Furthermore, antihistamines in the OAH group are also prescribed for other indications, such as itching and hives. Finally, data on drugs dispensed in institutions (e.g. hospitals) were not included in the study.
5. Conclusions
The main findings in this drug utilization study are the increasing use of other anxiolytics and hypnotics towards the end of 2020 (earlier and most pronounced in Denmark, where the pre-pandemic use was very low) as well as a similar, but less pronounced increase for antidepressants in Denmark and in youths in Norway. The early local peaks in prescription fills are likely due to stockpiling behavior, which has been described for a wide variety of drugs in March 2020. Baseline differences may have influenced prescription pattern changes during the study period. Longitudinal studies are needed to examine if the increases of anxiolytic, hypnotic, and antidepressant drugs at the end of 2020 are early markers for an increased level of anxiety, depression or sleep problems during the COVID-19 pandemic.
The following are the supplementary data related to this article.
Study drug groups.
CRediT authorship contribution statement
Mikael Tiger and Johan Reutfors designed the study. Carolyn Cesta and Pär Karlsson acquired the data. Pär Karlsson analyzed the data. All authors interpreted the data. Pär Karlsson performed the statistical analysis. Mikael Tiger and Johan Reutfors supervised the study. Mikael Tiger drafted the manuscript. All authors revised the manuscript for important intellectual content and approved the final version of the manuscript.
Conflict of interest
CEC, PK, and JR are employed at the Centre for Pharmacoepidemiology, Karolinska Institutet, which receives grants from several entities (pharmaceutical companies, regulatory authorities, and contract research organizations) for performance of drug safety and drug utilization studies, with no relation to the work reported in this paper. MT, MB, SS, RW, and MH declare no conflict of interest.
Acknowledgements
The Centre for Pharmacoepidemiology, Karolinska Institutet, provided financial support for this project.
References
- Ahmed G.K., Khedr E.M., Hamad D.A., Meshref T.S., Hashem M.M., Aly M.M. Long term impact of Covid-19 infection on sleep and mental health: a cross-sectional study. Psychiatry Res. 2021;305 doi: 10.1016/j.psychres.2021.114243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. Toward an experimental ecology of human-development. Am. Psychol. 1977;32:513–531. [Google Scholar]
- Carr M.J., Steeg S., Webb R.T., Kapur N., Chew-Graham C.A., Abel K.M., Hope H., Pierce M., Ashcroft D.M. Effects of the COVID-19 pandemic on primary care-recorded mental illness and self-harm episodes in the UK: a population-based cohort study. Lancet Public Health. 2021;6:e124–e135. doi: 10.1016/S2468-2667(20)30288-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casagrande M., Favieri F., Tambelli R., Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the italian population. Sleep Med. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020;29 doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covid- Mental Disorders Collaborators Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flygare O., Ivanov V.Z., Säll R., Malaise H., Rück C., Jayaram-Lindström N., Martinsson L. 2020. Subjective Mental Health and Need for Care Among Psychiatric Outpatients During the COVID-19 Pandemic: Results From an Outreach Initiative in Sweden. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furu K., Wettermark B., Andersen M., Martikainen J.E., Almarsdottir A.B., Sorensen H.T. The nordic countries as a cohort for pharmacoepidemiological research. Basic Clin. Pharmacol. Toxicol. 2010;106:86–94. doi: 10.1111/j.1742-7843.2009.00494.x. [DOI] [PubMed] [Google Scholar]
- Grasselli G., Greco M., Zanella A., Albano G., Antonelli M., Bellani G., Bonanomi E., Cabrini L., Carlesso E., Castelli G., Cattaneo S., Cereda D., Colombo S., Coluccello A., Crescini G., Forastieri Molinari A., Foti G., Fumagalli R., Iotti G.A., Langer T., Latronico N., Lorini F.L., Mojoli F., Natalini G., Pessina C.M., Ranieri V.M., Rech R., Scudeller L., Rosano A., Storti E., Thompson B.T., Tirani M., Villani P.G., Pesenti A., Cecconi M., Network C.-L.I. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern. Med. 2020;180:1345–1355. doi: 10.1001/jamainternmed.2020.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gualano M.R., Lo Moro G., Voglino G., Bert F., Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halfdanarson O., Zoega H., Aagaard L., Bernardo M., Brandt L., Fuste A.C., Furu K., Garuoliene K., Hoffmann F., Huybrechts K.F., Kalverdijk L.J., Kawakami K., Kieler H., Kinoshita T., Litchfield M., Lopez S.C., Machado-Alba J.E., Machado-Duque M.E., Mahesri M., Nishtala P.S., Pearson S.A., Reutfors J., Saastamoinen L.K., Sato I., Schuiling-Veninga C.C.M., Shyu Y.C., Skurtveit S., Verdoux H., Wang L.J., Yahni C.Z., Bachmann C.J. International trends in antipsychotic use: a study in 16 countries, 2005–2014. Eur. Neuropsychopharmacol. 2017;27:1064–1076. doi: 10.1016/j.euroneuro.2017.07.001. [DOI] [PubMed] [Google Scholar]
- Hawrilenko M., Kroshus E., Tandon P., Christakis D. The association between school closures and child mental health during COVID-19. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.24092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hojlund M., Pottegard A., Johnsen E., Kroken R.A., Reutfors J., Munk-Jorgensen P., Correll C.U. Trends in utilization and dosing of antipsychotic drugs in Scandinavia: comparison of 2006 and 2016. Br. J. Clin. Pharmacol. 2019;85:1598–1606. doi: 10.1111/bcp.13945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob L., Smith L., Koyanagi A., Oh H., Tanislav C., Shin J.I., Konrad M., Kostev K. Impact of the coronavirus 2019 (COVID-19) pandemic on anxiety diagnosis in general practices in Germany. J. Psychiatr. Res. 2020;143:528–533. doi: 10.1016/j.jpsychires.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson P., Nakitanda A.O., Lofling L., Cesta C.E. Patterns of prescription dispensation and over-the-counter medication sales in Sweden during the COVID-19 pandemic. PLoS One. 2021;16 doi: 10.1371/journal.pone.0253944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369 doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozman D., Graziul C., Gibbons R., Alexander G.C. Association between unemployment rates and prescription drug utilization in the United States, 2007–2010. BMC Health Serv. Res. 2012;12:435. doi: 10.1186/1472-6963-12-435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau H., Khosrawipour V., Kocbach P., Mikolajczyk A., Schubert J., Bania J., Khosrawipour T. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J. Travel Med. 2020;27 doi: 10.1093/jtm/taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y.T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludvigsson J.F. The first eight months of Sweden's COVID-19 strategy and the key actions and actors that were involved. Acta Paediatr. 2020;109:2459–2471. doi: 10.1111/apa.15582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meherali S., Punjani N., Louie-Poon S., Abdul Rahim K., Das J.K., Salam R.A., Lassi Z.S. Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18073432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milani S.A., Raji M.A., Chen L., Kuo Y.F. Trends in the use of benzodiazepines, Z-hypnotics, and serotonergic drugs among US women and men before and during the COVID-19 pandemic. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.31012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Board of Health and Welfare Analys av första covid-19-vågen – produktion, köer och väntetider i vården 2020-11-11. 2020. https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2020-11-7065.pdf
- Pierce M., McManus S., Hope H., Hotopf M., Ford T., Hatch S.L., John A., Kontopantelis E., Webb R.T., Wessely S., Abel K.M. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry. 2021;8:610–619. doi: 10.1016/S2215-0366(21)00151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pottegard A., Christensen R., Houji A., Christiansen C.B., Paulsen M.S., Thomsen J.L., Hallas J. Primary non-adherence in general practice: a danish register study. Eur. J. Clin. Pharmacol. 2014;70:757–763. doi: 10.1007/s00228-014-1677-y. [DOI] [PubMed] [Google Scholar]
- Prati G., Mancini A.D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021;51:201–211. doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulla P. Covid-19: India imposes lockdown for 21 days and cases rise. BMJ. 2020;368 doi: 10.1136/bmj.m1251. [DOI] [PubMed] [Google Scholar]
- Rabeea S.A., Merchant H.A., Khan M.U., Kow C.S., Hasan S.S. Surging trends in prescriptions and costs of antidepressants in England amid COVID-19. Daru. 2021;29:217–221. doi: 10.1007/s40199-021-00390-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine N., McArthur B.A., Cooke J.E., Eirich R., Zhu J., Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175(11):1–10. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reicher S., Drury J. Pandemic fatigue? How adherence to covid-19 regulations has been misrepresented and why it matters. BMJ. 2021;372 doi: 10.1136/bmj.n137. [DOI] [PubMed] [Google Scholar]
- Renaud-Charest O., Lui L.M.W., Eskander S., Ceban F., Ho R., Di Vincenzo J.D., Rosenblat J.D., Lee Y., Subramaniapillai M., McIntyre R.S. Onset and frequency of depression in post-COVID-19 syndrome: a systematic review. J. Psychiatr. Res. 2021;144:129–137. doi: 10.1016/j.jpsychires.2021.09.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risch N., Herrell R., Lehner T., Liang K.Y., Eaves L., Hoh J., Griem A., Kovacs M., Ott J., Merikangas K.R. Interaction between the serotonin transporter gene (5-HTTLPR), stressful life events, and risk of depression: a meta-analysis. JAMA. 2009;301:2462–2471. doi: 10.1001/jama.2009.878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Signorini G., Singh S.P., Boricevic-Marsanic V., Dieleman G., Dodig-Curkovic K., Franic T., Gerritsen S.E., Griffin J., Maras A., McNicholas F., O'Hara L., Purper-Ouakil D., Paul M., Santosh P., Schulze U., Street C., Tremmery S., Tuomainen H., Verhulst F., Warwick J., de Girolamo G., Consortium M. Architecture and functioning of child and adolescent mental health services: a 28-country survey in Europe. Lancet Psychiatry. 2017;4:715–724. doi: 10.1016/S2215-0366(17)30127-X. [DOI] [PubMed] [Google Scholar]
- Thornton J. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ. 2020;369 doi: 10.1136/bmj.m1401. [DOI] [PubMed] [Google Scholar]
- Zhang L., Zhang D., Fang J., Wan Y., Tao F., Sun Y. Assessment of mental health of chinese primary school students before and after school closing and opening during the COVID-19 pandemic. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.21482. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Study drug groups.