Abstract
Background and Aims:
The utility of high-resolution anorectal manometry (HR-ARM) for diagnosing defecatory disorders (DDs) is unclear because healthy people may have features of dyssynergia. We aimed to identify objective diagnostic criteria for DD and to ascertain the utility of HR-ARM for diagnosing DD.
Methods:
Constipated patients were assessed with HR-ARM and rectal balloon expulsion test (BET), and a subset underwent defecography. Normal values were established by assessing 184 sex-matched healthy persons. Logistic regression models evaluated the association of abnormal HR-ARM findings with prolonged BET and reduced rectal evacuation (determined by defecography).
Results:
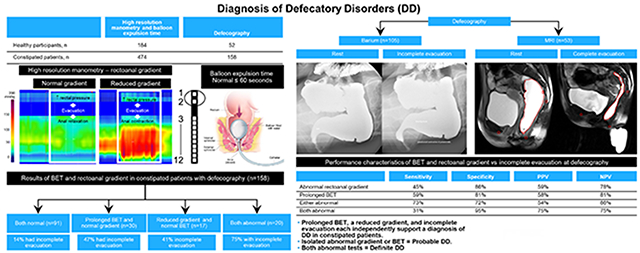
Four hundred seventy-four constipated persons (420 women) underwent HR-ARM and BET; 158 underwent defecography. BET was prolonged, suggesting a DD, for 152 patients (32%). Rectal evacuation was lower for patients with prolonged vs normal BET. A lower rectoanal gradient during evacuation, reduced anal squeeze increment, and reduced rectal sensation were independently associated with abnormal BETs; the rectoanal gradient was 36% sensitive and 85% specific for prolonged BET. A lower rectoanal gradient and prolonged BET were independently associated with incomplete evacuation. Among constipated patients, the probability of reduced rectal evacuation was 14% when gradient and BET were both normal, 45% when either was abnormal, and 75% when both variables were abnormal.
Conclusions:
HR-ARM, BET, and defecography findings were concordant for constipated patients, and reduced rectoanal gradient was the best HR-ARM predictor of prolonged BET or reduced rectal evacuation. Prolonged BET, reduced gradient, and incomplete evacuation each independently supported a diagnosis of DD in constipated patients. We propose the terms probable DD for patients with an isolated abnormal gradient or BET and definite DD for patients with abnormal results from both tests.
Keywords: defecography, dyssynergic defecation, pelvic floor dysfunction, Rome criteria
Graphical Abstract
Lay summary:
A reduced rectoanal gradient, as compared to age and sex-matched asymptomatic persons, was the most important parameter on anorectal manometry to predict impaired evacuation by either balloon expulsion test or defecography and should be considered probable evidence of a defecatory disorder.
Background
Many patients with laxative-refractory chronic constipation have defecatory disorders (DDs) that may be effectively treated with biofeedback.1, 2 Although thorough history and digital rectal examination findings may suggest a DD,3, 4 anorectal tests are necessary for the diagnosis.1, 2, 5–7 Nevertheless, consensus is limited about the selection of tests, sequence of testing, and the precise diagnostic criteria for DD. Most guidelines recommend beginning with anorectal manometry and balloon expulsion test (BET), possibly followed by barium or magnetic resonance (MR) defecography.1, 2 Others recommend beginning with manometry and defecography, to identify structural abnormalities that hinder defecation.8
Anorectal tests are limited by the fact that some asymptomatic, healthy people have features of dyssynergia.9–12 Hence, if results are not compared with sex- and age-matched normal values, which are not available for all tests, the diagnostic accuracy of the test is suboptimal. The Rome IV criteria recognized the potential for false-positive results and recommended that a DD diagnosis require abnormal results from 2 tests (ie, manometry or surface electromyography, BET, and defecography).13 But, confounding this approach, test results may be inconsistent for an individual.14–16 For example, among patients with dyssynergia by defecography, approximately 50% have normal findings with anal surface electromyography and BET.14
BET is arguably the preferred initial test for identifying DD because it is relatively sensitive, specific, and inexpensive.1 Among 106 patients with functional constipation and 24 patients with DD, BET was 88% sensitive and 89% specific for identifying a confirmed DD; positive and negative predictive values were 64% and 97%, respectively.17 However, the BET was performed by inflating a rectal balloon until patients wanted to defecate, rather than to 50 mL, which is the volume typically used in clinical practice.
In high-resolution anorectal manometry (HR-ARM), the optimal criteria for diagnosing DD are unclear.16 The rectoanal gradient during evacuation is the primary criterion used to diagnose DD, but the diagnostic utility of other abnormalities (eg, reduced rectal sensation, reduced anal squeeze function) is unknown.16 To date, only 2 small studies have investigated HR-ARM, BET, and defecography in constipated patients.11, 18 Hence, these 3 tests have not been rigorously compared in a large cohort of patients. We aimed to evaluate the diagnostic utility of HR-ARM, BET, and defecography for identifying a DD and clarify recommendations for anorectal testing in patients with suspected DDs.
Methods
Study Design and Participants
This retrospective cohort study was approved by the Mayo Clinic Institutional Review Board. Informed consent was waived for patients authorizing use of their health records for research. All authors had access to the study data and have reviewed and approved the final manuscript. Study participants were evaluated from January 1, 2008 through December 31, 2018 at Mayo Clinic (Rochester, Minnesota). Asymptomatic participants who had enrolled in previous clinical trials utilizing anorectal manometry9, 19, 20 were identified through public advertisements, and constipated participants were identified from our clinical practice.
Manometry
All participants underwent HR-ARM (Manoscan; Medtronic Inc) that included measurement of resting anal pressure, squeeze pressure, anorectal pressure during simulated defecation, and rectal sensory volume thresholds for first sensation, urge, and discomfort, as detailed previously.9, 21 During simulated defecation, the residual anal pressure, percent anal relaxation, rectal pressure increase above baseline, and rectoanal gradient were measured. Immediately after HR-ARM, the rectal BET was assessed as described;22 values greater than 60 seconds were considered abnormal.
Defecography
Constipated patients underwent MR or barium defecography using established approaches.23 Anorectal descent and rectal evacuation during defecation were measured with semiautomated, validated software (Pelvic Measures, Mayo Clinic); evacuation less than 25% was considered reduced.24, 25
Statistical Analysis
Categorical and continuous variables were compared with the χ2 and Wilcoxon rank sum tests. Multivariable logistic regression models evaluated the utility of HR-ARM findings, expressed as categorical or continuous variables, for predicting prolonged BET in constipated patients. Patients were sex- and age-matched to control groups with normal BET; groups were defined as male controls, female controls younger than 50 years, or female controls aged 50 years and older. The categorical models contained select anorectal variables; values were categorized as normal if they were within the 10th through 90th percentile range of values from the appropriate control group.9 These normal values differ slightly from our most recent paper because they include additional asymptomatic participants who were studied after that paper was published.9 Specifically, values for resting anal pressure, residual anal pressure during simulated defecation, and volume threshold for urge sensation exceeding the 90th percentile value were considered abnormal. Further, values for rectal pressure increase, anal relaxation, rectoanal gradient during simulated defecation, and squeeze increment (maximum squeeze vs anal resting pressure) less than the 10th percentile value were considered abnormal. The 10th-90th percentile ranges for these values in healthy volunteers with a normal BET are shown in Supplemental Table 1.
Separate logistic regression models were used to determine the odds ratio (OR) for abnormal BET by treating HR-ARM parameters as continuous variables. In these models, units were changed to 10 mm Hg or 10 mL to improve ease of interpretation.
Using the regression model with continuous parameters, the estimated odds and probability of abnormal BET for each participant were calculated with the following formulae:
Statistical analysis was performed with JMP Pro statistical software, version 13.0 (SAS Institute Inc). The α level was set at 0.05.
Results
Demographic Characteristics
The study included 658 persons (474 patients with constipation, 184 healthy participants). Table 1 details demographic characteristics and anorectal variables for the cohort. Of patients with constipation, 158 underwent defecography (MR, n=53; barium, n=105). Compared with healthy participants, constipated patients were older and a larger proportion were women (P<.001 for both). Among constipated patients, 369 satisfied symptom criteria for functional constipation and 105 met criteria for constipation-predominant irritable bowel syndrome. More constipated patients had a prolonged rectal BET than healthy participants (152 [32%] vs 20 [11%]; P<.001).
Table 1.
Demographic Characteristics and Anorectal Variables
| Characteristic | Clinical group | Balloon expulsion time | ||||
|---|---|---|---|---|---|---|
| Healthy participants (n=184) | Constipated patients (n=474) | P value | Normal (n=486) | Prolonged (n=172) | P value | |
| Demographic and clinical characteristics | ||||||
| Sex, No. (%) | <.001 | .44 | ||||
| Female | 134 (73) | 420 (89) | 412 (85) | 150 (87) | ||
| Male | 50 (27) | 54 (11) | 74 (15) | 22 (13) | ||
| Age, median (IQR), y | 35 (23-62) | 49 (26-73) | <.001 | 48 (24-72) | 45 (25-68) | .31 |
| Body mass index, median (IQR) | 25 (21-31) | 25 (20-34) | .49 | 25 (23-34) | 25 (22-29) | .67 |
| Symptoms | <.001 | |||||
| Functional constipation | N/A | 369 (78) | 250 (51) | 119 (69) | ||
| Constipation-predominant irritable bowel syndrome | N/A | 105 (22) | 72 (15) | 33 (19) | ||
| Healthy participants | N/A | N/A | 164 (34) | 20 (12) | ||
| Balloon expulsion test, abnormal result | 20 (11) | 152 (32) | <.001 | N/A | N/A | N/A |
| History of pregnancy | ||||||
| Yes | 64/134 (48) | 263/420 (63) | <.01 | 247/404 (61) | 80/150 (53) | .11 |
| No | 70/134 (52) | 116/420 (28) | 132/404 (33) | 54/150 (36) | ||
| Unknown | 0 (0) | 41/420 (10) | 25/404 (6) | 16/150 (11) | ||
| Number of births, median (IQR) | 0 (0-2) | 2 (0-3) | <.01 | 2 (0-2) | 1 (0-3) | .34 |
| Hysterectomy | ||||||
| Yes | 18 (13) | 133 (32) | <.01 | 115 (28) | 36 (24) | .29 |
| No | 116 (87) | 287 (68) | 289 (72) | 114 (76) | ||
| Anorectal variables | ||||||
| High anal resting pressure | 15 (8) | 34 (7) | .67 | 31 (6) | 18 (10) | .08 |
| Reduced anal squeeze increment | 20 (11) | 108 (23) | .001 | 83 (17) | 45 (26) | .01 |
| Evacuation | ||||||
| Reduced rectal pressure increase | 20 (11) | 37 (8) | .21 | 37 (8) | 20 (12) | .11 |
| High residual anal pressure | 18 (10) | 54 (11) | .55 | 44 (9) | 28 (16) | .01 |
| Reduced anal relaxation | 20 (11) | 71 (15) | .17 | 54 (11) | 37 (22) | .001 |
| Reduced rectoanal gradient | 21 (11) | 101 (21) | .003 | 63 (13) | 59 (34) | <.001 |
| Increased rectal sensory threshold for urgencya | 7/157 (4) | 39/459 (8) | .01 | 25/448 (6) | 21/168 (13) | .004 |
Abbreviation: N/A, not applicable.
Not evaluated for 42 patients.
HR-ARM vs BET
In the univariable analysis comparing constipated patients with healthy participants, a greater proportion of patients had a reduced anal squeeze increment (23% vs 11%; P=.01), an increased rectal sensory threshold for urgency (8% vs 4%; P=.01), and a reduced rectoanal gradient during evacuation (21% vs 11%; P=.003) (Table 1). Compared to those with normal BET, a greater proportion of participants with abnormal BET had reductions in anal squeeze increment, anal relaxation during evacuation, and rectoanal gradient during evacuation. Additionally, more participants with abnormal BET had increased residual anal pressure during evacuation and rectal sensory threshold for urgency.
For the 459 patients who had assessment of all HR-ARM variables, including rectal sensation, urge sensation, squeeze increment, and rectoanal gradient variables were normal for 252 patients (55%), and the rectoanal gradient was reduced for 97 patients (21%) (Supplemental Figure 1A). Among patients with normal rectoanal gradients but other abnormal findings, reductions also were observed for rectal sensation only (n=23 [5%]), the squeeze increment only (n=79 [17%]), or both variables (n=8 [2%]).
Does the Number of Abnormal Manometry Variables Predict an Abnormal BET?
Considered individually, the HR-ARM variables were specific but relatively insensitive for predicting prolonged BET (Table 2). Reduced rectoanal gradient was the most useful variable for predicting prolonged BET, with sensitivity of 36% and specificity of 85%. Regardless of the exact abnormality, 1, 2, and 3 abnormal HR-ARM variables could predict prolonged BET with sensitivity of 72%, 37%, and 19%, respectively, and with specificity of 50%, 83%, and 95%, respectively. When the number of abnormal HR-ARM variables per patient increased from 3 to 4, the positive predictive value for prolonged BET increased from 64% to 92%. However, only 11 patients had 4 or more abnormal HR-ARM findings (Supplemental Figure 2).
Table 2.
Performance Characteristics of HR-ARM Findings vs Abnormal BET in Constipated Patients (n=474)
| Anorectal variable | Abnormal BET results, No. (%) | Sensitivity, % | Specificity, % | Positive predictive value, % | Negative predictive value, % | AUROC, % |
|---|---|---|---|---|---|---|
| High anal resting pressure | 18/34 (53) | 12 | 95 | 53 | 70 | 53 |
| Reduced anal squeeze increment | 43/108 (40) | 28 | 80 | 40 | 70 | 54 |
| Evacuation | ||||||
| Reduced rectal pressure increase | 16/37 (43) | 11 | 94 | 43 | 69 | 52 |
| High residual anal pressure | 26/54 (48) | 17 | 91 | 48 | 70 | 54 |
| Reduced anal relaxation | 31/71 (44) | 20 | 88 | 44 | 70 | 54 |
| Reduced rectoanal gradient | 54/101 (53) | 36 | 85 | 53 | 74 | 60 |
| Increased rectal sensory threshold for urgency | 20/39 (51) | 13 | 94 | 51 | 69 | 54 |
| Number of abnormal variables threshold | 65a | |||||
| 1 | 52/155 (34) | 72 | 50 | 41 | 79 | |
| 2 | 27/64 (42) | 37 | 83 | 51 | 73 | |
| 3 | 17/32 (53) | 19 | 95 | 64 | 71 | |
| 4 | 9/9 (100) | 7 | 99.7 | 92 | 69 | |
| 5 | 1/1 (100) | 1 | 100.0 | 100 | 68 | |
| 6 | 1/1 (100) | 1 | 100.0 | 100 | 68 |
Abbreviations: AUROC, area under the receiver operating curve; BET, balloon expulsion time; HR-ARM, high-resolution anal manometry; N/A, not applicable.
The AUROC was calculated for a model that included a threshold of 1 or more abnormal variables. Fifteen patients with missing data for sensation were excluded from the sensitivity and specificity analysis for the total number of abnormal variables.
Association of HR-ARM Variables and BET with Rectal Evacuation
Among 158 constipated patients who underwent defecography, prolonged BET, reduced rectoanal gradient, increased residual anal pressure, and increased rectal urge sensation threshold were each associated with reduced rectal evacuation measured with defecography (Table 3). Of the variables associated with reduced rectal evacuation, differences in rectal evacuation between participants with normal vs abnormal HR-ARM variables were considerable and statistically significant. For example, the median (IQR) for rectal evacuation was 78% (42%-93%) for patients with a normal BET and 18% (0%-65%) for patients with an abnormal BET (P<.001).
Table 3.
Comparison of Anorectal Manometry Findings and BET with Rectal Evacuation on Defecography in Constipated Patients (n=158)
| HR-ARM parameter abnormality | Evacuation, No. | P value | Evacuation, median, % | Sensitivity, % | Specificity, % | Positive predictive value, % | Negative predictive value, % | |
|---|---|---|---|---|---|---|---|---|
| Normal | Reduced | |||||||
| Prolonged BET | <.001 | |||||||
| Normal | 88 | 20 | 78 | N/A | N/A | N/A | N/A | |
| Abnormal | 21 | 29 | 18 | 59 | 81 | 58 | 81 | |
| Gradient | <.001 | |||||||
| Normal | 94 | 27 | 74 | N/A | N/A | N/A | N/A | |
| Abnormal | 15 | 22 | 16 | 45 | 86 | 59 | 78 | |
| Gradient and BET | <.001 | |||||||
| Both normal | 78 | 13 | 79 | N/A | N/A | N/A | N/A | |
| Either abnormal | 26 | 21 | 35 | 73 | 72 | 54 | 86 | |
| Both abnormal | 5 | 15 | 3 | 31 | 95 | 75 | 75 | |
| Resting anal pressure | .25 | |||||||
| Normal | 100 | 42 | 70 | N/A | N/A | N/A | N/A | |
| Abnormal | 9 | 7 | 33 | 14 | 92 | 44 | 70 | |
| Anal squeeze increment | .73 | |||||||
| Normal | 85 | 37 | 70 | N/A | N/A | N/A | N/A | |
| Abnormal | 24 | 12 | 60 | 24 | 78 | 33 | 70 | |
| Residual anal pressure | <.001 | |||||||
| Normal | 100 | 34 | 73 | N/A | N/A | N/A | N/A | |
| Abnormal | 9 | 15 | 12 | 31 | 92 | 63 | 75 | |
| Rectal pressure increase | .53 | |||||||
| Normal | 103 | 45 | 70 | N/A | N/A | N/A | N/A | |
| Abnormal | 6 | 4 | 37 | 8 | 94 | 40 | 70 | |
| Anal relaxation | .95 | |||||||
| Normal | 93 | 42 | 66 | N/A | N/A | N/A | N/A | |
| Abnormal | 16 | 7 | 70 | 14 | 85 | 30 | 69 | |
| Urge sensation | .013 | |||||||
| Normal | 101 | 40 | 70 | N/A | N/A | N/A | N/A | |
| Abnormal | 5 | 8 | 3 | 17 | 95 | 62 | 72 | |
Abbreviations: BE, balloon expulsion time; HR-ARM, high-resolution anorectal manometry; N/A, not applicable.
Incomplete rectal evacuation was defined as <25%. Prolonged BET was defined as >60 seconds.
Reduced rectoanal gradient plus prolonged BET (both characteristics present) was predictive of incomplete evacuation, as determined by defecography, for constipated patients. Figure 1A illustrates how the degree of rectal evacuation varied with BET and rectoanal gradient results. The median rectal evacuation also varied according to rectoanal gradient and BET status (79% if both variables were normal; 35% if either was abnormal; and 3% if both were abnormal [P<.001]). The sensitivities of a prolonged BET and reduced rectoanal gradient for incomplete evacuation by defecography were 59% and 45%, respectively; the specificities were 81% and 86%, respectively (Table 3). The sensitivity of either a prolonged BET or a reduced gradient compared with incomplete evacuation was 73%, whereas the specificity was 72%. Among patients with both a prolonged BET and a reduced gradient, the sensitivity compared with defecography was lower at 31%, but the specificity was higher at 95%.
Figure 1.
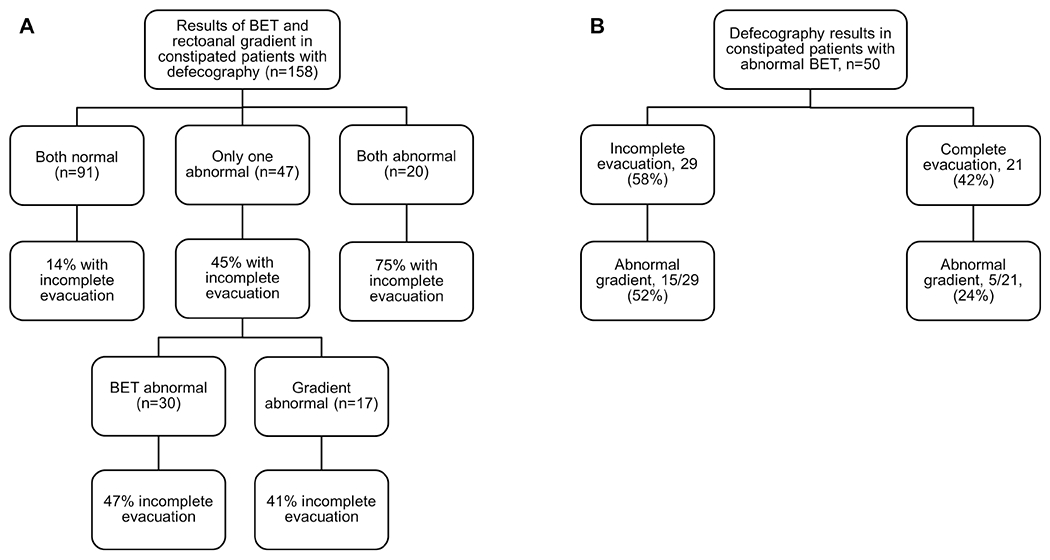
Relationship between rectoanal gradient, BET, and rectal evacuation in constipated patients. A, Rectal evacuation on defecography was associated with the results of HR-ARM and BET (P<.001). B, Among constipated patients with an abnormal BET, incomplete rectal evacuation on defecography was associated with an abnormal rectoanal gradient. BET indicates balloon expulsion test; HR-ARM, high-resolution anorectal manometry.
Of 50 constipated patients with abnormal BET who underwent defecography, 21 (42%) had normal evacuation and 29 (58%) had incomplete evacuation (Figure 1B). The rectoanal gradient was reduced for 15/29 patients (52%) with abnormal BET and incomplete evacuation and for 5/21 patients (24%) with abnormal BET and normal evacuation (P=.047).
Concurrent Consideration of Rectoanal Gradient, BET, and Defecography
Among 158 constipated patients who underwent defecography, all 3 variables (rectoanal gradient, BET, and rectal evacuation) were normal for 78 patients (49%) (Supplemental Figure 1B). Two or 3 variables showed abnormal results for 41 patients (26%). Hence, the results of these key variables were concurrent for 119 patients (75%). Of patients with only 1 abnormal test result, prolonged BET was noted for 16 (10%), incomplete evacuation for 13 (8%), and a reduced rectoanal gradient for 10 (6%).
Anorectal Descent During Evacuation
Anorectal descent during evacuation was assessed in 147 of 156 constipated patients who had clearly visible measurement landmarks. In the univariable analysis, anorectal descent during defecation was lower for patients with a prolonged vs normal BET (median, 21 vs 33 mm; P=.003), but it was not different between patients with reduced vs normal evacuation on defecography (median, 24 vs 31 mm; P=.10). No other defecography variables (eg, anorectal angle) distinguished between patients with normal vs reduced evacuation (data not shown). In the multivariable models for prolonged BET and incomplete evacuation, perineal descent during evacuation was not a significant variable; hence, it was not added to the multivariable models summarized in Tables 4 and 5.
Table 4:
Multivariable logistic regression models for predicting prolonged balloon expulsion test from HR-ARM variables
| Variable | Odds Ratios (95% CI) for abnormal BET | ||
|---|---|---|---|
| Among all participants with complete HR-ARM data (n=616) | Among constipated patients only (n=459) | Among constipated women only (n=405) | |
| Model 1 (HR-ARM categorical variables) | |||
| Reduced anal squeeze pressure increment | 1.79 (1.15-2.78)a | 1.67 (1.05-2.67)a | 2.07 (1.23-3.48)a |
| Increased volume for urge sensation | 2.45 (1.29-4.64)a | 2.53 (1.27-5.01)a | 2.61 (1.20-5.69)a |
| Reduced anal relaxation | 1.68 (1.01-2.78)a | Not significant, removed from model | Not significant, removed from model |
| Reduced rectoanal gradient during evacuation | 3.46 (2.23-5.37)a | 3.53 (2.20-5.65)a | 3.51 (2.13-5.78)a |
| Previous childbirth | N/A | N/A | 0.59 (0.37-0.91)a |
| Previous hysterectomy | N/A | N/A | 0.67 (0.41-1.11) |
| AUROC | 0.66 | 0.65 | 0.70 |
| Model 2 (HR-ARM continuous variables) | |||
| Anal squeeze pressure increment (mm Hg) | 0.93 (0.90-0.96)a | 0.95 (0.91-0.99)a | 0.92 (0.88-0.97)a |
| Volume for urge sensation | 1.04 (1.00-1.09)a | 1.05 (1.01-1.10)a | 1.05 (0.998-1.10) |
| Rectoanal gradient during evacuation | 0.77 (0.72-0.83)a | 0.76 (0.70-0.82)a | 0.75 (0.69-0.82)a |
| Previous childbirth | N/A | N/A | 0.65 (0.40-1.05) |
| Previous hysterectomy | N/A | N/A | 0.74 (0.44-1.24) |
| AUROC | 0.75 | 0.75 | 0.76 |
Abbreviations: AUROC, area under the receiver operating curve; HR-ARM, high-resolution anorectal manometry; N/A, not applicable.
Statistically significant predictor.
Table 5.
Multivariable logistic regression models of incomplete evacuation on defecography
| Variable | Odds ratio (95% CI) for incomplete evacuation | ||
|---|---|---|---|
| Among all participants with defecography and complete-HR-ARM data (n=204) | Among constipated patients with defecography (n=154) | Among constipated women with defecography (n=145) | |
| Anorectal HR-ARM parameter | |||
| High anal resting pressure | 0.82 (0.25-2.66) | 1.09 (0.30-3.99) | 1.13 (0.30-4.30) |
| Reduced anal squeeze increment | 1.02 (0.44-2.37) | 1.23 (0.49-3.12) | 1.31 (0.48-3.56) |
| Reduced anal relaxation | 0.58 (0.20-1.70) | 0.46 (0.13-1.55) | 0.42 (0.12-1.53) |
| Reduced rectoanal gradient | 4.19 (1.83-9.58)a | 4.35 (1.74-10.93)a | 4.44 (1.69-11.67)a |
| Increased rectal sensory threshold for urgency | 3.00 (0.86-10.50) | 2.69 (0.67-10.77) | 4.46 (0.95-20.83) |
| Abnormal balloon expulsion test | 4.32 (2.10-8.88)a | 4.57 (2.04-10.22)a | 5.06 (2.11-12.14)a |
| Previous childbirth | N/A | N/A | 0.90 (0.36-2.24) |
| Previous hysterectomy | N/A | N/A | 0.80 (0.31-2.06) |
| AUROC | 0.76 | 0.78 | 0.80 |
Abbreviations: AUROC, area under the receiver operating curve; HR-ARM, high-resolution anorectal manometry; N/A, not applicable.
Statistically significant predictor.
Using HR-ARM to Predict Abnormal BET and Rectal Evacuation During Defecography
Multivariable logistic regression models evaluated the utility of anorectal variables, childbirth, and hysterectomy for predicting a prolonged BET (Table 4) and reduced rectal evacuation on defecography (Table 5). Three HR-ARM parameters (reduced rectoanal gradient, increased rectal threshold volume for urgency, and reduced anal squeeze pressure increment) were independently associated with prolonged rectal BET whether expressed categorically (ie, normal or abnormal finding) or as continuous variables (Table 4). Among 459 constipated patients who had sensation assessed during HR-ARM, the OR of prolonged BET for reduced rectoanal gradient was 3.53 (95% CI, 2.20-5.65); for increased threshold of urgency sensation, the OR was 2.53 (95% CI, 1.27-5.01); and for reduced squeeze increment, the OR was 1.67 (95% CI, 1.05-2.67). Similar ORs were observed in the model that was limited to constipated women and also included childbirth and hysterectomy. The odds of a prolonged BET were lower (OR, 0.59; 95% CI, 0.37-0.91) in women with a history of childbirth.
Among constipated patients who underwent defecography, reduced rectoanal gradient during evacuation was also independently associated with incomplete rectal evacuation (OR, 4.35 [95% CI, 1.74-10.93]; P=.002) (Table 5). This association remained even after adjusting for prolonged BET (OR, 4.57 [95% CI, 2.04-10.22]; P<.001) and other HR-ARM abnormalities. Similar ORs were observed in the model that was limited to constipated women and also included childbirth and hysterectomy (Table 5).
The probability of prolonged BET for each constipated patient was calculated from the logistic regression model using continuous HR-ARM parameters and compared with degree of evacuation in patients who underwent defecography (excluding 4 patients who did not have rectal sensation assessed during HR-ARM). Of these 154 patients, the probability of prolonged BET was ≥60% for 19 patients, and these patients more commonly had incomplete evacuation on defecography (74% vs 25%; P<.001). This model estimated probability of normal BET ≥60% in 99/105 constipated patients who in fact had a normal BET. More patients with a higher probability (estimated ≥60%) of prolonged BET had reduced rectal evacuation on defecography compared with those who had a lower probability (estimated <60%) of prolonged BET (4/6 [67%] vs 16/99 [16%] patients; P=.002).
Discussion
Neither a criterion standard test nor an agreed-upon algorithm exists for diagnosing DD. The Rome IV criteria recommended diagnosing DD on the basis of at least 2 abnormal tests. However, this approach is challenging to implement because HR-ARM and BET may yield discordant findings and because access to defecography is limited. To date, only 2 small studies have evaluated HR-ARM, BET, and defecography in patients with suspected DD.11, 18 In a third study, among 188 patients who underwent HR-ARM and MR defecography but not a BET, there was considerable agreement in findings of dyssynergia between these tests.26
In this study, a cohort of constipated patients was evaluated by HR-ARM, BET, and defecography, and findings were analyzed with reference to appropriate controls. Overall, test results were significantly associated with each other, supporting their convergent validity. BET was prolonged, suggestive of a DD, in approximately one-third of the 474 constipated patients. Confirming some 27–28 but not all 29 earlier observations, prolonged BET was independently associated with reduced (more negative) rectoanal gradient during evacuation. A prolonged BET was also associated with other features (ie, lower anal squeeze increment,27, 28 greater rectal threshold for urgency29) that are not generally considered when diagnosing DD. This combined model had an optimal AUROC of 75% for distinguishing between constipated patients with normal vs abnormal BET (Supplemental Figure 3), whereas the AUROC was 72% for the isolated rectoanal gradient. The model’s accuracy was confirmed in a nested cohort of 158 constipated patients who underwent defecography. Among patients with an estimated abnormal BET probability <60% based on HR-ARM findings alone, 25% had reduced rectal evacuation on defecography; among patients with an estimated probability of ≥60%, 74% had incomplete evacuation. Even among patients with normal BET, patients with abnormal HR-ARM characteristics (probability of prolonged BET ≥60%) more commonly had incomplete evacuation, suggesting that even when HR-ARM and BET findings disagree, abnormal HR-ARM findings may be indicative of a DD.
Although HR-ARM is useful for diagnosing DD, approximately 30% of patients with abnormal BET have normal HR-ARM findings. Hence, when a DD is suspected, we emphasize that both tests must be performed. The rectoanal gradient during evacuation is the most useful HR-ARM variable for diagnosing DD (Table 6). For all anorectal variables including the gradient, values that were lower than the 10th percentile value in healthy asymptomatic persons studied in our laboratory (i.e., a gradient of −119, −74, and −67 mmHg respectively in men, women <50 years and ≥ 50 years) were considered abnormal (Supplemental Table 1). These normal values, which are derived from the largest cohort of asymptomatic healthy Caucasian persons studied with the Medtronic HR-ARM catheter, are probably also appropriate for Caucasian patients studied with this catheter at other centers. Studies performed with other catheters should be interpreted using age- and sex-appropriate normal values for those catheters 16. However, when normal values are unavailable, it is incorrect to interpret data against normal values obtained with a different catheter. Our data suggest that when interpreting HR-ARM studies, it is likely sufficient to consider a specific HR-ARM finding (ie, the rectoanal gradient during evacuation), rather than just the number of HR-ARM abnormalities. For example, the sensitivity and specificity of a reduced rectoanal gradient for predicting an abnormal BET were 36% and 85%, respectively, whereas they were 37% and 83%, respectively, for any 2 HR-ARM abnormalities.
Table 6.
Summary of Key Findings and Recommendations
| Finding | Recommendation |
|---|---|
| Reduced rectoanal gradient, reduced squeeze increment, and increased threshold for urge sensation independently predicted prolonged BET in constipated patients. | HR-ARM variables must be interpreted relative to normal values measured with the same technique in the corresponding sex and age (Supplementary Table 1). Reduced squeeze and sensation should be considered as supportive criteria for a DD. |
| In a multivariable model adjusting for HR-ARM findings, only prolonged BET and reduced rectoanal gradient were associated with incomplete evacuation on defecography. | Abnormal rectoanal gradient and prolonged BET are the most useful non-defecography findings for predicting a DD. The presence of either abnormality in the setting of typical symptoms should be considered a sign of a probable DD, but 2 abnormal anorectal test results are suggested to confirm the diagnosis. |
| The sensitivity of individual HR-ARM parameters for abnormal BET ranged from 11% to 35%, whereas the specificity ranged from 80% to 95%. The sensitivity of a single abnormal HR-ARM parameter was 72%, whereas the specificity was 50%. Requiring at least 2 abnormal HR-ARM parameters reduced sensitivity to 37% but increased specificity to 83%. | A single HR-ARM parameter has low sensitivity but high specificity for an abnormal BET, but the finding of at least 1 HR-ARM abnormality (of any type) is more sensitive. Increasing the number of abnormalities increases specificity but reduces sensitivity. |
| Most constipated patients with abnormal results for both BET and rectoanal gradient had reduced rectal evacuation (75% of patients), whereas those with normal results for both BET and gradient less commonly had reduced evacuation (14% of patients). Patients with only 1 abnormality (either an abnormal gradient or an abnormal BET) had an intermediate frequency of reduced evacuation (41% and 47%, respectively). | Patients with 1 abnormality (gradient or BET) should be considered to have a probable DD; patients with 2 abnormalities (gradient and BET)should be considered to have a definite DD. When either gradient or BET alone is abnormal, defecography can provide useful supportive evidence; however, it may not be required because the specificity of abnormal BET and abnormal gradient for reduced rectal evacuation was 81% and 86%, respectively. When BET and rectoanal gradient findings agree, defecography is likely unnecessary unless clinical suspicion exists for structural abnormalities, such as rectocele. |
Abbreviations: BET, balloon expulsion time; DD, defecatory disorder; HR-ARM, high-resolution anorectal manometry.
The Rome IV criteria for DD require meeting symptom criteria for constipation-predominant irritable bowel syndrome or functional constipation and having “features of impaired evacuation as demonstrated by 2 of the following 3 tests: abnormal BET, anorectal evacuation pattern with manometry or anal surface EMG [electromyography], or impaired rectal evacuation by imaging.”13 Regardless of HR-ARM and BET results, defecography should be used to assess patients with suspected structural abnormalities (eg, a large rectocele) that may promote the development of a DD. Although HR-ARM findings may suggest selected structural abnormalities (eg, rectal intussusception or a large rectocele), imaging is required to document such findings.11
Our findings suggest that when the index of suspicion for structural abnormalities is low, defecography is unnecessary when the HR-ARM and BET are both normal or both abnormal because these combinations are associated with a low (14%) or high (75%) prevalence of reduced rectal evacuation, respectively. When the gradient and BET were both abnormal, the specificity compared with reduced evacuation was 95%. Hence, such patients almost certainly have a DD and would require pelvic floor biofeedback therapy. However, the sensitivity of 2 abnormal test results (ie, HR-ARM and BET) compared with reduced evacuation was only 31%. Consequently, if 2 abnormal test results are required to diagnose a DD, some patients with a DD that manifests with only 1 abnormal test result might not be referred for, (and thus would not benefit from) biofeedback therapy. Barring concern for clinically relevant structural abnormalities, our impression is that most experts would concur with a DD diagnosis and the need for biofeedback therapy for patients with typical clinical features and an abnormal BET. By comparison, we suspect that fewer clinicians would be comfortable diagnosing a DD for a patient with a reduced rectoanal gradient but a normal BET.
However, our findings suggest that the probability of reduced rectal evacuation is similar, ie, 41% and 47% in patients who have an isolated reduced gradient or a prolonged BET. Moreover, a reduced gradient was independently associated with reduced rectal evacuation, even after adjusting for the BET; both variables had similar ORs for predicting incomplete evacuation (4.35 for abnormal gradient and 4.57 for prolonged BET). In patients with at least 1 abnormal finding (ie, abnormal gradient and/or BET), the sensitivity and specificity compared with reduced evacuation were 73% and 72%, respectively. Currently, for such patients, the decision to pursue defecography depends on the clinical index of suspicion for a DD or for structural abnormalities and whether 1 or 2 abnormal test results are deemed necessary to diagnose a DD. Also, defecography is not widely available, it may be embarrassing for some patients, and barium defecography entails radiation exposure. Hence, taking these factors into consideration, we propose the term probable DD to characterize those patients who have 1 abnormal result from the 3 tests (ie, HR-ARM, BET, and defecography) and the term definite DD to characterize those with 2 abnormal test results. Although a single abnormal finding may be a false-positive result, it may be reasonable to pursue a trial of biofeedback therapy for patients with a probable DD, especially when defecography is not feasible. However, this approach should be confirmed by prospective studies that assess the response to anorectal biofeedback therapy in patients with probable and definite DD, as defined above.
In the analyses, the BET and rectal evacuation measured with defecography were the dependent variables because they are arguably the best available outcome variables for rectal evacuation. Nevertheless, no “gold standard” test exists for DD, partly because patients may be reluctant to expel in a test environment and/or may experience a variable desire to defecate during these tests. Thus, the extent to which these tests approximate normal defecation likely varies among individuals. We also acknowledge differences in the nature and volume of rectal contents among these tests, ie, barium paste (180 mL, 454 g) during defecography, a balloon (50 mL) during a BET, and no rectal distention during HR-ARM. Therefore, it is not surprising that different tests yield different answers for some patients. For example, 13 of 91 patients (14%) with an abnormal BET and rectoanal gradient had normal rectal evacuation during defecography. Compared with defecography, HR-ARM and BET may be associated with less rectal distention and urgency and thus more strain during evacuation, with excessive strain unmasking the abdominoanal dyscoordination in patients with DD.30 These variables (ie, nature of rectal contents and the rate of rectal distention) affect the outcome of anorectal tests and the ease of defecation 28,31. Hence, differences among test findings are perhaps not true inconsistencies; rather, they underscore that defecation is a nuanced somatovisceral process that is influenced by several factors.
Study Strengths and Limitations
In this study, 658 participants (including 184 healthy controls and 104 men) underwent HR-ARM and BETs; 210 also underwent defecography (including 158 constipated patients). Healthy controls were used to generate 10th through 90th percentile normal ranges, and these values were used to determine whether constipated patients had normal or abnormal HR-ARM parameters (after adjusting for age and sex). However, the analysis was retrospective. There were differences in demographic features, parity, and hysterectomy status between constipated and healthy participants. Although the decision to pursue defecography was based on clinical judgment and likely representative of the clinical practice at our institution, this decision may be affected by selection bias.
Conclusion
In summary, we suggest that HR-ARM and BET should be performed first for patients with a suspected DD. Reduced rectoanal gradient and prolonged BET were independently associated with incomplete evacuation on defecography, which suggests that abnormal rectoanal gradient is indicative of a DD, even when BET is normal. In addition to the rectoanal gradient during defecation (the most useful HR-ARM variable for diagnosing DD), low anal squeeze increment and high sensory threshold for urgency were also independently associated with abnormal BET. Although multiple abnormal findings provide the strongest evidence of a DD, an abnormal rectoanal gradient alone in patients with typical symptoms likely represents pelvic floor dysfunction, and it may be reasonable to pursue biofeedback therapy with such patients.
Supplementary Material
Supplemental Figure 1. Proportion of all constipated patients (left panel) and constipated patients who also underwent defecography (right panel) who had anorectal manometry abnormalities (ie, reduced rectoanal gradient during evacuation and/or reduced anal squeeze increment and/or reduced rectal sensation). All 3 manometry variables were normal in 55% (left panel) or 49% of patients (right panel).
Supplemental Figure 2. Proportion of constipated patients with a prolonged balloon expulsion time stratified by the number of anorectal manometry abnormal findings. The balloon expulsion time was prolonged in all patients with 4 or more abnormal manometry findings.
Supplemental Figure 3: Receiver operating characteristic curve to predict a prolonged rectal balloon expulsion time from selected anorectal manometry variables (ie, rectoanal gradient, anal squeeze increment, and rectal volume threshold for urgency) in all participants with complete HR_ARM data.
Box. What You Need to Know.
Background and Context:
Defecatory disorders (DDs) are a common cause of chronic constipation, but the diagnostic criteria for DD and the utility of high-resolution anorectal manometry (HR-ARM) for diagnosing DD are unclear.
New Findings:
Among constipated patients (n=474), reduced rectoanal gradient, squeeze increment, and urge sensation were the most useful HR-ARM predictors of prolonged balloon expulsion test, while only reduced rectoanal gradient and prolonged balloon expulsion test were independent predictors of incomplete evacuation on defecography.
Limitations:
Not all patients underwent defecography, and the number of male participants was limited.
Impact:
In patients with suggestive history and physical exam, a prolonged BET or reduced rectoanal gradient alone suggests probable DD, whereas the presence of both is diagnostic.
Acknowledgment:
June Oshiro, PhD, ELS, Mayo Clinic, substantively edited the manuscript. The Scientific Publications staff at Mayo Clinic provided proofreading, administrative, and clerical support.
Grant Support:
This study was supported by US Public Health Service National Institutes of Health grant R01DK078924.
Abbreviations
- AUROC
area under the receiver operating curve
- BET
balloon expulsion test, balloon expulsion time
- DD
defecatory disorder
- HR-ARM
high-resolution anorectal manometry
- MR
magnetic resonance
- OR
odds ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: All authors report that they have no conflicts of interest.
Portions of this manuscript were presented at Digestive Diseases Week 2022.
Contributor Information
John W. Blackett, Resident in the Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota.
Gautam Misha, Research Fellow in the Enteric Physiology and Imaging Facility, Mayo Clinic, Rochester, Minnesota.
Rahul Mishra, Research Fellow in the Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota.
Nicholas R. Oblizajek, Resident in the Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota.
Shivabalan Kathavarayan Ramu, Research Fellow in the Enteric Neuroscience Program, Mayo Clinic, Rochester, Minnesota.
Kent R. Bailey, Mayo Clinic School of Graduate Medical Education, Mayo Clinic College of Medicine and Science, Rochester, Minnesota, and Division of Clinical Trials and Biostatistics, Mayo Clinic, Rochester, Minnesota.
Adil E. Bharucha, Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota.
Data availability:
Data are available from the corresponding author upon reasonable request.
References
- 1.Bharucha AE, Lacy BE. Mechanisms, Evaluation, and Management of Chronic Constipation. Gastroenterology 2020;158:1232–1249.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wald A, Bharucha AE, Limketkai B, et al. ACG Clinical Guidelines: Management of Benign Anorectal Disorders. Am J Gastroenterol 2021;116:1987–2008. [DOI] [PubMed] [Google Scholar]
- 3.Tantiphlachiva K, Rao P, Attaluri A, et al. Digital rectal examination is a useful tool for identifying patients with dyssynergia. Clinical Gastroenterology & Hepatology 2010;8:955–60. [DOI] [PubMed] [Google Scholar]
- 4.Rao SSC. Rectal Exam: Yes, it can and should be done in a busy practice! Am J Gastroenterol 2018;113:635–638. [DOI] [PubMed] [Google Scholar]
- 5.Carrington EV, Heinrich H, Knowles CH, et al. Methods of anorectal manometry vary widely in clinical practice: Results from an international survey. Neurogastroenterology & Motility 2017;29:e13016. [DOI] [PubMed] [Google Scholar]
- 6.Ortengren AR, Ramkissoon RA, Chey WD, et al. Anorectal manometry to diagnose dyssynergic defecation: Systematic review and meta-analysis of diagnostic test accuracy. Neurogastroenterology & Motility 2021;33:e14137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scott SM, Carrington EV. The London Classification: Improving Characterization and Classification of Anorectal Function with Anorectal Manometry. Curr Gastroenterol Rep 2020;22:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grossi U, Di Tanna GL, Heinrich H, et al. Systematic review with meta-analysis: defecography should be a first-line diagnostic modality in patients with refractory constipation. Alimentary pharmacology & therapeutics 2018;48:1186–1201. [DOI] [PubMed] [Google Scholar]
- 9.Oblizajek NR, Gandhi S, Sharma M, et al. Anorectal pressures measured with high-resolution manometry in healthy people—Normal values and asymptomatic pelvic floor dysfunction. Neurogastroenterology and Motility : the official journal of the European Gastrointestinal Motility Society 2019:e13597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grossi U, Carrington EV, Bharucha AE, et al. Diagnostic accuracy study of anorectal manometry for diagnosis of dyssynergic defecation. Gut 2016;65:447–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prichard DO, Lee T, Parthasarathy G, et al. High-resolution Anorectal Manometry for Identifying Defecatory Disorders and Rectal Structural Abnormalities in Women. Clinical Gastroenterology & Hepatology 2017;15:412–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raza N, Bielefeldt K. Discriminative value of anorectal manometry in clinical practice. Digestive Diseases & Sciences;54:2503–11. [DOI] [PubMed] [Google Scholar]
- 13.Rao S, Bharucha AE, Chiarioni G, et al. Functional anorectal disorders. Gastroenterology 2016;150:1430–1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bordeianou L, Savitt L, Dursun A. Measurements of pelvic floor dyssynergia: which test result matters? Diseases of the Colon & Rectum 2011;54:60–5. [DOI] [PubMed] [Google Scholar]
- 15.Palit S, Thin N, Knowles CH, et al. Diagnostic disagreement between tests of evacuatory function: a prospective study of 100 constipated patients. Neurogastroenterology and Motility 2016;28:1589–98. [DOI] [PubMed] [Google Scholar]
- 16.Bharucha AE, Basilisco G, Malcolm A, et al. Review of the indications, methods, and clinical utility of anorectal manometry and the rectal balloon expulsion test. Neurogastroenterol Motil 2022:e14335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Minguez M, Herreros B, Sanchiz V, et al. Predictive value of the balloon expulsion test for excluding the diagnosis of pelvic floor dyssynergia in constipation. Gastroenterology 2004;126:57–62. [DOI] [PubMed] [Google Scholar]
- 18.Deb B, Sharma M, Fletcher JG, et al. Inadequate Rectal Pressure and Insufficient Relaxation and Abdominopelvic Coordination in Defecatory Disorders. Gastroenterology 2022;162:1111–1122.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma M, Muthyala A, Feuerhak K, et al. Improving the Utility of High Resolution Manometry for the Diagnosis of Defecatory Disorders in Women with Chronic Constipation. Neurogastroenterol and Motility 2020. Jul 01;32:e13910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ratuapli S, Bharucha AE, Harvey D, et al. Comparison of rectal balloon expulsion test in seated and left lateral positions. Neurogastroenterology and Motility 2013;25:e813–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oblizajek NR, Deb B, Kathavarayan Ramu S, et al. Optimizing Techniques for Measuring Anal Resting and Squeeze Pressures with High Resolution Manometry Neurogastroenterol and Motility 2022;In press. [DOI] [PMC free article] [PubMed]
- 22.Carrington EV, Heinrich H, Knowles CH, et al. The international anorectal physiology working group (IAPWG) recommendations: Standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol Motil 2020;32:e13679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tirumanisetty P, Prichard D, Fletcher JG, et al. Normal values for assessment of anal sphincter morphology, anorectal motion, and pelvic organ prolapse with MRI in healthy women. Neurogastroenterology & Motility 2018;30:e13314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Puthanmadhom Narayanan S, Sharma M, Fletcher JG, et al. Comparison of changes in rectal area and volume during MR evacuation proctography in healthy and constipated adults. Neurogastroenterology & Motility 2019;31:e13608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Noelting J, Bharucha AE, Lake DS, et al. Semi-automated vectorial analysis of anorectal motion by magnetic resonance defecography in healthy subjects and fecal incontinence. Neurogastroenterol Motil 2012;24:e467–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heinrich H, Sauter M, Fox M, et al. Assessment of Obstructive Defecation by High-Resolution Anorectal Manometry Compared With Magnetic Resonance Defecography. Clinical Gastroenterology & Hepatology 2015;13:1310–1317.e1. [DOI] [PubMed] [Google Scholar]
- 27.Bharucha AE, Fletcher JG, Seide B, et al. Phenotypic Variation in Functional Disorders of Defecation. Gastroenterology 2005;128:1199–1210. [DOI] [PubMed] [Google Scholar]
- 28.Bharucha AE, Croak AJ, Gebhart JB, et al. Comparison of rectoanal axial forces in health and functional defecatory disorders. American Journal of Physiology - Gastrointestinal & Liver Physiology 2006;290:G1164–9. [DOI] [PubMed] [Google Scholar]
- 29.Vasudevan SP, Scott SM, Gladman MA, et al. Rectal hyposensitivity: evaluation of anal sensation in female patients with refractory constipation with and without faecal incontinence. Neurogastroenterology & Motility 2007;19:660–7. [DOI] [PubMed] [Google Scholar]
- 30.Srinivasan SG, Muthyala A, Sharma M, et al. Abdomino-anal Dyscoordination in Defecatory Disorders. Clinical Gastroenterology & Hepatology 2021;08:08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heitmann PTVP, Knowles CH, Lunniss PJ, Dinning PD, Scott SM. The physiology of human defaecation: a prerequisite to understanding disorders of evacuation and continence. Nat Rev Gastroenterol Hepatol 2021;18:751–769. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Proportion of all constipated patients (left panel) and constipated patients who also underwent defecography (right panel) who had anorectal manometry abnormalities (ie, reduced rectoanal gradient during evacuation and/or reduced anal squeeze increment and/or reduced rectal sensation). All 3 manometry variables were normal in 55% (left panel) or 49% of patients (right panel).
Supplemental Figure 2. Proportion of constipated patients with a prolonged balloon expulsion time stratified by the number of anorectal manometry abnormal findings. The balloon expulsion time was prolonged in all patients with 4 or more abnormal manometry findings.
Supplemental Figure 3: Receiver operating characteristic curve to predict a prolonged rectal balloon expulsion time from selected anorectal manometry variables (ie, rectoanal gradient, anal squeeze increment, and rectal volume threshold for urgency) in all participants with complete HR_ARM data.
Data Availability Statement
Data are available from the corresponding author upon reasonable request.


