Abstract
Objectives:
The COVID-19 pandemic impacted the availability and accessibility of outpatient care following hospital discharge. Hospitalists (physicians) and hospital medicine advanced practice providers (HM-APPs) coordinate discharge care of hospitalized patients; however, it is unknown if they can deliver post-discharge virtual care and overcome barriers to outpatient care. The objective was to develop and provide post-discharge virtual care for patients discharged from hospital medicine services.
Methods:
We developed the Post-discharge Early Assessment with Remote video Link (PEARL) initiative for HM-APPs to conduct a post-discharge video visit (to review recommendations) and telephone follow-up (to evaluate adherence) with patients 2–6 days following hospital discharge. Participants included patients discharged from hospital medicine services at an institution’s hospitals in Rochester (May 2020–August 2020) and Austin (November 2020–February 2021) in Minnesota, US. HM-APPs also interviewed patients about their experience with the video visit and completed a survey on their experience with PEARL.
Results:
Of 386 eligible patients, 61.4% were enrolled (n=237/386) including 48.1% women (n=114/237). In patients with complete video visit and telephone follow-up (n=141/237), most were prescribed new medications (83.7%) and took them as prescribed (93.2%). Among five classes of chronic medications, patient-reported adherence ranged from 59.2% (narcotics) to 91.5% (anti-hypertensives). Patient-reported self-management of 12 discharge recommendations ranged from 40% (smoking cessation) to 100% (checking rashes). Patients reported benefit from the video visit (agree: 77.3%) with an equivocal preference for video visits over clinic visits. Among HM-APPs who responded to the survey (88.2%; n=15/17), 73.3% reported benefit from visual contact with patients but were uncertain if video visits would reduce emergency department visits.
Conclusion:
In this novel initiative, HM-APPs used video visits to provide care beyond their hospital role, reinforce discharge recommendations for patients, and reduce barriers to outpatient care. The effect of this initiative is under evaluation in a randomized controlled trial.
Keywords: hospital medicine, advanced practice providers, post-discharge care, telemedicine
Introduction
During the Coronavirus Disease-19 (COVID-19) pandemic, the care transition of hospitalized patients from the hospital to the community was disrupted by the reduced accessibility and availability of outpatient care. Hospitalists (physicians) and hospital medicine advanced practice providers (HM-APPs) coordinate discharge planning of patients hospitalized on general medical wards. However, it was unknown if hospital providers may expand beyond their hospital role, leverage virtual platforms, and provide post-discharge care.
Previous studies on post-discharge care and outcomes focused on reducing 30-day hospital readmission rates. A meta-analysis of 42 studies showed that interventions in the inpatient, outpatient, and both settings, had a pooled effect of 18% lower risk of 30-day hospital readmission. In 16 studies that improved patients’ self-care, there was a 32% lower risk of 30-day hospital readmission.1 In support, an observational study of 1000 general medical patients in 12 United States (US) academic medical centers showed that 26.9% of 30-day hospital readmissions were potentially preventable, and attributable to patient education, self-management, and medication safety, among other factors.2 Despite these studies, there is relatively less information on when and by whom the intervention(s) should be conducted. This was particularly relevant during the COVID-19 pandemic due to limited availability of outpatient visits with primary care providers and specialists following hospitalization.3-6 During the pandemic, HM-APPs (nurse practitioners and physician assistants) were uniquely situated to leverage their knowledge of the hospital discharge plan, expand beyond their traditional role in the hospital, and provide post-discharge virtual care.
Early in the COVID-19 pandemic, we developed the Post-discharge Early Assessment with Remote video Link (PEARL) initiative to address the reduced availability of outpatient care, reduced mobility of patients and caregivers, and to improve patient adherence to discharge recommendations. We describe the development of PEARL as well as patient and HM-APP perspectives. This initiative may be adapted at other institutions for the delivery of post-discharge virtual care.
Materials and Methods
Study Design and Sites
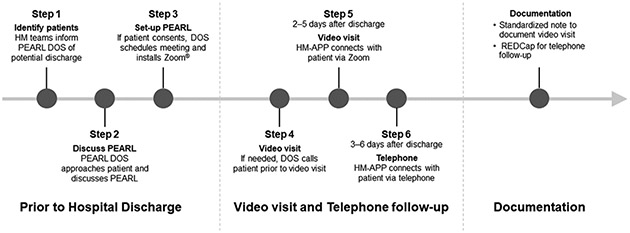
PEARL was designed by multidisciplinary stakeholders (hospitalists, HM-APPs, desk operations specialists [DOS], division administrators and operations managers) with expertise in hospital medicine, health administration, patient flow and logistics, survey methods, and clinical research (Figure 1). DOS are integral members of hospital teams and provide logistic support (e.g., obtain outside records, carry team pager, update treatment plan in patient rooms, and schedule post-discharge appointments). PEARL had a dedicated DOS to manage daily logistics for PEARL and maintain study documents. PEARL was deemed to be ‘Exempt’ by the Mayo Clinic Institutional Review Board.
Figure 1: PEARL workflow for patient identification, enrollment, and completion of video visits and telephone follow-up.
Abbreviations: HM-APP: Hospital Medicine Advanced Practice Provider; DOS: Desk Operations Specialist; HM: Hospital Medicine; MCHS-AU: Mayo Clinic Health System-Austin; PEARL: Post-Discharge Early Assessment with Remote video Link; REDCap: Research Electronic Data Capture.
Used with permission of Mayo Foundation for Medical Education and Research, all rights reserved.
The study sites were Mayo Clinic Hospital, Saint Marys Campus, Rochester, MN and Mayo Clinic Health System in Austin, MN (MCHS-AU). Mayo Clinic Hospital in Rochester, MN is a large academic hospital with 1,265 beds at two campuses–Saint Marys Campus and Rochester Methodist Hospital. In 2020, the hospital had 52,778 admissions, of which, 22% were managed by hospital medicine. The Division of Hospital Internal Medicine is comprised of approximately 50 physicians and 50 APPs. MCHS-AU has 82 beds and is part of MCHS, which is a network of 16 community hospitals in southern Minnesota, western Wisconsin, and northern Iowa. In 2020, MCHS-AU had 4,932 admissions, of which, 61% were managed by hospital medicine. At both sites, hospital medicine services provided care to adults hospitalized in general medical wards.
PEARL was developed from April 14, 2020–May 3, 2020, and conducted at Saint Marys Campus (May 4, 2020–August 9, 2020) and MCHS-AU (November 16, 2020–February 15, 2021) (Supplementary Figure 1). PEARL involved steps prior to hospital discharge (steps 1–3), video visit and telephone follow-up after hospital discharge (steps 4–6), and documentation of video visits and telephone follow-up (Figure 1).
Steps 1–3: Prior to Hospital Discharge
Patient Eligibility
The inclusion criteria were: (i) age ≥18 years and discharged from hospital medicine services managed by a physician and HM-APP, (ii) oral consent from patient or legally authorized representative; and (iii) discharge home or to assisted living facility. The exclusion criteria were: (i) current elective admission (i.e., hospitalized for a planned intervention or procedure), (ii) non-English speaking patient or legally authorized representative who could not provide oral consent, (iii) discharge from hospital against medical advice, (iv) no access to mobile technology, laptop, or computer, (v) active COVID-19 diagnosis, or (vi) scheduled re-admission for intervention or procedure.
Patients were not charged or remunerated for the virtual service.
Study Staff and Workspace
PEARL required additional staffing and support for virtual technology. PEARL had a dedicated workroom for the DOS and APPs. Computer workstations were fitted with dual monitors, web cameras, and Zoom® software. At Saint Marys Campus, a DOS or HM-APP obtained patient consent and provided logistic support. At MCHS-AU, APPs obtained patient consent. All video-visits and telephone follow-up were conducted by APPs at Saint Marys Hospital Campus.
Patient Enrollment
The PEARL workflow was developed with multidisciplinary input. Hospital medicine services informed the PEARL DOS of potential patient discharges. The DOS and/or HM-APP screened and scheduled eligible patients for a video visit (2–5 days after discharge) and telephone follow-up (3–6 days after discharge). If requested, the DOS or HM-APP installed Zoom® on the patients’ electronic (iPAD or similar) device.
Steps 4–6: Video visit and Telephone follow-up
Post-discharge Video Visit and Telephone Follow-up
During video visits, APPs used a standardized script to review discharge recommendations for four domains: (1) new medications or changes to existing medications, (2) chronic medications, (3) self-management and action plan, and (4) home supports (Supplement 1). The video visit provided opportunities to review discharge recommendations and barriers to adherence. Based on acuity, APPs resolved issues through discussion with the patient, follow-up with the physician/HM-APP from the discharging hospital medicine service, or referral to the primary care provider or emergency department. Video visits were documented in the electronic medical record using a standardized note template (not shown).
During telephone follow-up, APPs used a standardized script to evaluate patient adherence to discharge recommendations (yes; no) or address questions/concerns. At the end of the telephone follow-up, APPs surveyed patients on their experience with the video visits (Supplement 2). The responses were documented using the Research Electronic Data Capture (REDCap®) portal.7,8
Additional Information
Patient demographics (e.g., name, date of birth) and hospitalization characteristics (e.g., date of admission, date of discharge) were captured at enrollment in PEARL. Additional information (e.g., race, marital status) was obtained from the electronic medical record and entered in REDCap®.
HM-APP Survey
HM-APPs who conducted ≥1 video visit and/or telephone follow-up received a REDCap® electronic survey on demographics and experience with PEARL (interpersonal communication, technical quality of care, efficacy, and technology) (Supplement 3). HM-APPs received a unique survey link at their work email address with up to two weekly reminders. The survey was conducted from July 13, 2020–July 27, 2020. HM-APPs were not remunerated for participating in the survey.
Statistical Analysis
Patient demographics and hospital characteristics were summarized using frequency (percentage) or median (range). Statistical analysis was completed using SAS 9.4 (SAS Institute Inc., Cary, NC) and statistical significance was established at two-tailed P<0.05.
Results
Patient Characteristics
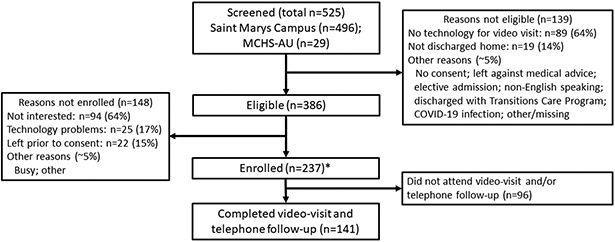
Of 525 patients screened, 73.5% met eligibility criteria (n=386/525) and the main reason for not meeting eligibility was absence of technology (n=89/139) (Figure 2). Of eligible patients, 61.4% were enrolled (n=237/386) and the main reason for not enrolling was lack of interest (64%; n=94/148).
Figure 2: Schematic to screen and enroll patients for post-discharge video visit and telephone follow-up.
*Of eligible patients (n=386), consent for enrollment was received from 238 patients, and 1 patient was not enrolled for administrative reasons.
Abbreviations: COVID-19 Coronavirus Disease 2019; MCHS-AU Mayo Clinic Health System-Austin
The enrolled patients had a median age (range) of 63 (19–98) years and included 48.1% women and 88.6% White adults (Table 1). The median interval (range) between hospital discharge and video visit was 3 (0–7) days and between video visit and telephone follow-up was 1 (1–5) days.
Table 1:
Characteristics of Patients Enrolled in PEARL
| Completed Video visit and Telephone Follow-up |
||||
|---|---|---|---|---|
| Overall N = 237 |
Yes N = 141 |
No N = 96 |
P value | |
| Demographics | ||||
| Age, years | 63 (19–98) | 66 (20–87) | 56 (19–98) | <0.001 |
| Women | 114 (48.1) | 68 (48.2) | 46 (47.9) | 0.96 |
| Race | 0.19 | |||
| American Indian or Alaska Native | 2 (0.8) | 1 (0.7) | 1 (1.0) | |
| Asian | 1 (0.4) | 0 (0) | 1 (1.0) | |
| Black or African American | 17 (7.2) | 6 (4.3) | 11 (11.5) | |
| Native Hawaiian or Other Pacific Islander | 1 (0.4) | 1 (0.7) | 0 (0) | |
| White | 210 (88.6) | 128 (90.8) | 82 (85.4) | |
| Other | 3 (1.3) | 2 (1.4) | 1 (1.0) | |
| Unknown | 3 (1.3) | 3 (2.1) | 0 (0) | |
| Marital status | 0.003 | |||
| Married | 133 (56.1) | 91 (64.5) | 42 (43.8) | |
| Single, separated, or divorced | 97 (40.5) | 45 (31.9) | 52 (54.2) | |
| Widowed | 7 (3.0) | 5 (3.5) | 2 (2.1) | |
| Enrollment site | ||||
| Saint Marys Campus | 223 (94.1) | 133 (94.3) | 90 (93.8) | |
| MCHS-AU | 14 (5.9) | 8 (5.7) | 6 (6.3) | |
| Video visit and telephone follow-up | ||||
| Interval between hospital discharge and video visit, days* | N/A | 3 (0–7) | N/A | |
| No-show for video visit† | N/A | 72 (30.4) | N/A | |
| Video visit converted to telephone call | N/A | 42 (17.7) | N/A | |
| Interval between video visit and telephone follow-up, days | N/A | 1 (1–5) | N/A | |
| Interval between hospital discharge and telephone follow-up, days | N/A | 5 (1–8) | N/A | |
| Completed telephone follow-up‡ | N/A | 141 (85.5) | N/A | |
Data presented as median (range) and frequency (%).
Video visit conducted on same day as discharge per patient request (n=1).
No-show for video visit and telephone follow-up based on unsuccessful contact with patient on two calendar days.
Based on completed video visits.
Abbreviations: MCHS-AU Mayo Clinic Health System-Austin; N/A: Not applicable; PEARL Post-discharge Early Assessment with Remote video Link
HM-APP Characteristics
Among HM-APPs, the survey response rate was 88.2% (n=15/17). Most respondents were women, nurse practitioners, and had completed 1-5 PEARL shifts (Supplementary Table 1).
Patient Management of Discharge Recommendations
The video visit and telephone follow-up were completed by 59.5% of patients (n=141/237). Patients who did not complete the video visit and telephone follow-up, compared with those that did, were younger and less likely to be married (Table 1). In patients with complete video visit and telephone follow-up, 83.7% were prescribed new medications (n=118/141), 94.9% collected medications from the pharmacy and 93.2% took the medications as prescribed (Table 2). Patient-reported adherence to chronic medications ranged from 91.5% for anti-hypertensives to 59.2% for narcotics with intermediate adherence of 63.2%–80.8% for diuretics, inhalers, and antibiotics.
Table 2:
Patient-reported Management of Discharge Medications
| Patients N = 141 no. (%) |
|
|---|---|
| New medications | |
| Prescribed at discharge | 118 (83.7) |
| Understood instructions | |
| Fully understood | 117 (99.2) |
| Partially understood | 1 (0.8) |
| Picked up new medications prescribed at discharge from pharmacy | 112 (94.9) |
| Reasons did not pick up new medication | |
| Could not afford | 3 (2.1) |
| Did not think medication was needed | 1 (0.7) |
| Worried about side-effects | 1 (0.7) |
| Other | 2 (1.4) |
| New medications taken as prescribed | |
| Yes | 110 (93.2) |
| Not exactly | 4 (3.4) |
| No | 4 (3.4) |
| Reason not taking new medications as prescribed* | |
| Felt sick | 1 (0.7) |
| Worried about side-effects | 1 (0.7) |
| Other | 2 (1.4) |
| Chronic medications, if applicable † | |
| Took anti-hypertensives (e.g., ACE-inhibitor, calcium blockers, β-blockers) | |
| Yes | 86 (91.5) |
| No | 8 (8.5) |
| Took diuretics (e.g., furosemide, spironolactone, torsemide, HCTZ) | |
| Yes | 42 (80.8) |
| No | 10 (19.2) |
| Took inhalers (e.g., inhalers, nebulizers, steroids) | |
| Yes | 37 (74.0) |
| No | 13 (26.0) |
| Took antibiotics | |
| Yes | 36 (63.2) |
| No | 21 (36.8) |
| Took narcotic pain medications (e.g., oxycodone, hydromorphone)‡ | |
| Yes | 29 (59.2) |
| No | 20 (40.8) |
Based on responding ‘No’ to previous question (n=4).
Responses: yes (took as prescribed); no (did not take as prescribed). Other patients were not prescribed these chronic medications.
Missing data (n=2 patients).
Percentages may not add to 100 due to rounding.
Abbreviations: ACE angiotensin converting enzyme; HCTZ hydrochlorothiazide.
HM-APPs evaluated patients’ self-management of 12 discharge recommendations (Table 3). Adequate self-management ranged from 100% for checking rashes to 40% for smoking cessation with intermediate management of 87.9%–97.7% for other recommendations. Patients receipt of post-discharge supplies ranged from 97.6% for walkers to 40.0% for bedside commode with intermediate responses of 72.7%–91.3% for other supplies (Table 3).
Table 3:
Advanced Practice Provider Evaluation of Patient-reported Self-Care
| Patients N = 141 no. (%) |
|
|---|---|
| As evaluated by HM-APPs, patient met expectations for * | |
| Checking weight | |
| Yes | 45 (90.0) |
| No | 5 (10.0) |
| Checking blood pressure | |
| Yes | 51 (87.9) |
| No | 7 (12.1) |
| Checking leg swelling | |
| Yes | 43 (97.7) |
| No | 1 (2.3) |
| Checking rashes | |
| Yes | 24 (100) |
| No | 0 |
| Using supplemental oxygen | |
| Yes | 13 (92.9) |
| No | 1 (7.1) |
| Using CPAP/BiPAP† | |
| Yes | 25 (92.6) |
| No | 2 (7.4) |
| Fluid restriction | |
| Yes | 16 (88.9) |
| No | 2 (11.1) |
| Salt restriction‡ | |
| Yes | 31 (93.9) |
| No | 2 (6.1) |
| Diet restriction† | |
| Yes | 51 (92.7) |
| No | 4 (7.3) |
| Checking blood sugar | |
| Yes | 41 (95.3) |
| No | 2 (4.7) |
| Smoking cessation† | |
| Yes | 6 (40.0) |
| No | 9 (60.0) |
| Alcohol consumption† | |
| Yes | 27 (93.1) |
| No | 2 (6.9) |
| If prescribed, patients received post-discharge supplies | |
| Supplemental oxygen† | |
| Yes | 12 (80.0) |
| No | 3 (20.0) |
| Walker | |
| Yes | 41 (97.6) |
| No | 1 (2.4) |
| Cane | |
| Yes | 21 (91.3) |
| No | 2 (8.7) |
| Wheelchair | |
| Yes | 14 (87.5) |
| No | 2 (12.5) |
| Bedside commode | |
| Yes | 2 (40.0) |
| No | 3 (60.0) |
| Intravenous medication | |
| Yes | 8 (72.7) |
| No | 3 (27.3) |
Responses: yes (met expectations/received supplies), no (did not meet expectations/did not receive supplies).
Other patients were not provided this discharge recommendation.
Missing data for (n=2)† and (n=3)‡ patients.
Percentages may not add to 100 due to rounding.
Abbreviations: HM-APP hospital medicine advanced practice provider; BiPAP bilevel positive airway pressure; CPAP continuous positive airway pressure.
Patient Perspective on Video visit
Patients connected easily (agree: 74.0%) and understood the provider (agree: 93.0%) during the video visit (Table 4). Patients reported benefit from the video visit (agree: 77.3%) and recommending to friends or family (agree: 82.3%) but were equivocal in preferring video visits over clinic visits (agree: 34.6%).
Table 4:
Patient Perspective on Video visits
| Agree | Neutral | Disagree | |
|---|---|---|---|
| Patients (n=131) | no. (%) | ||
| Easy to connect to video visit | 97 (74.0) | 16 (12.2) | 18 (13.7) |
| Understood provider during video visit* | 119 (93.0) | 6 (4.7) | 3 (2.3) |
| Provider understood you during video visit* | 121 (94.5) | 6 (4.7) | 1 (0.8) |
| Benefited from video visit* | 99 (77.3) | 27 (21.1) | 2 (1.6) |
| Interested in future video visits† | 91 (70.0) | 19 (14.6) | 20 (15.4) |
| Prefer video visit over clinic visit† | 45 (34.6) | 51 (39.2) | 34 (26.2) |
| Video visit felt less connected to provider compared to in-person visit‡ |
23 (17.8) | 28 (21.7) | 78 (60.5) |
| Would recommend video visit to friends or family† | 107 (82.3) | 19 (14.6) | 4 (3.1) |
Missing data for (n=3)*, (n=1)†, and (n=2) ‡ patients.
Survey questions in Supplement 2.
HM-APP Perspective on PEARL
Among HM-APP respondents (n=15) including nurse practitioners (66.7%; n=10/15) and physician assistants (33.3%; n=5/15), 66.7% of HM-APPs had completed 1–5 PEARL shifts and 33.3% had completed 6–15 shifts (Supplementary Table 1). HM-APPs saw ~4–10 patients per shift. HM-APPs benefited from visual contact with patients (agree: 73.3%), used the video visit software easily (agree: 80.0%) and had adequate time for video visits (agree: 93.3%) but were uncertain if video visits would reduce emergency department visits (neutral: 46.7%), hospital length of stay or hospital readmission rates (both, neutral: 53.3%) (Supplementary Table 2).
Discussion
During the COVID-19 pandemic, we developed PEARL to improve post-discharge care following hospitalization on a hospital medicine service. Of 237 patients enrolled, 59.5% completed the video visit and telephone follow-up. Post-discharge adherence ranged from 59.2%–91.5% (chronic medications) and 40%–100% (self-management) with 40%–97.6% of patients receiving the prescribed discharge supplies. Most patients and HM-APPs reported benefit from the video visit. This study reports the development and results of a novel post-discharge initiative that may be replicated at other institutions. To our knowledge, this is the first study on expanding the role of HM-APPs to deliver post-discharge care during the COVID-19 pandemic.
In a study of 12 US academic centers, factors associated with potentially preventable 30-day readmission (adjusted odds ratio [95% CI]) in general medical patients included inadequate medication safety (2.41 [1.18–4.90]), suboptimal patient education and self-management (2.33 [1.64–3.30]), and lack of post-discharge disease monitoring (1.75 [1.37–2.24]) among other factors.2 In support, a meta-analysis of 19 clinical trials showed that communication interventions at hospital discharge resulted in 24% higher adherence to treatment regimen, 31% lower 30-day hospital readmission but no association with emergency department visits (relative risk 0.86; 95% CI, 0.67–1.10).9 In the present study, PEARL focused on post-discharge readmission factors that could be addressed with a video visit. At our institution, patients receive discharge education (i.e., changes to medications, upcoming appointments) prior to discharge, and therefore, PEARL video visits were conducted to provide an additional opportunity to reinforce discharge recommendations and address barriers after patients returned home. The association between PEARL video visits and hospital readmission rates will be evaluated in future work.
Prior to the COVID-19 pandemic, studies evaluated the effect of post-discharge virtual interventions on 30-day hospital readmission rates. In a Canadian study, randomization to a virtual ward (i.e., care coordination and direct care through telephone, home/clinic visits), compared with usual care, showed no effect on readmission or death at 30 days after discharge.10 In a study in North Carolina, randomization of patients with >20% risk of readmission to an intensive transition services program (i.e., spanned inpatient, outpatient, and home settings) showed no effect on 30-day readmission rates but had fewer admissions to the intensive care unit.11 However, in that study, the 75% crossover from intervention to usual care likely contributed to the null effect of the intervention.11 Despite these and other studies on the mixed benefit of post-discharge interventions, we developed PEARL to address the limited availability and accessibility to outpatient care early in the COVID-19 pandemic (i.e., after March 2020). Early in the pandemic, there was a ~70% decline in outpatient visits compared to the same week in prior years.6 From March–June 2020, an estimated 30% of clinic visits used telemedicine, which represented a 23-fold increase compared with use in the pre-pandemic period from January–March 2020.12 Furthermore, many clinics were closed and/or had limited capability to transition to virtual care and many patients deferred care due to concern about contracting COVID-19.13 In this context, PEARL leveraged HM-APPs to reinforce discharge recommendations and address the limited availability of outpatient care. This initiative represented a novel expansion of the role of HM-APPs, who were traditionally not involved in post-discharge care. PEARL required an increase in staffing resources (e.g., APP, DOS) and technology (e.g., dedicated workroom, computers with video capability), which was foundational for our efforts to provide tele-based care, bring care to the privacy of patients’ homes, support rural populations with limited access to outpatient care, and potentially improve patient outcomes.
In the present study, several patients did not enroll or attend the video visit due to lack of technology, which underscores concern that the shift toward telemedicine/video visits may exacerbate health disparities based on access to technology.14-16 In a study at a US academic health system, patients with lower telemedicine use were of Asian race, older, and non-English speaking, whereas patients with lower video use were Black, Latinx, older, and poorer.17 In a cross-sectional study across 1652 outpatient practices in an integrated health system, the use of video visits was lower in patients who were older, Black, Hispanic, Spanish-speaking, and with low broadband access.18 In the present study, we did not evaluate patient outcomes (i.e., emergency department visits or 30-day readmission rates) stratified by access/availability of technology but will examine these in future studies. In addition to disparity based on technology, there may be concern that patients with homelessness or in shelters will not access telemedicine care or video visits. However, this concern is tempered by recent reports that people experiencing homelessness have access to phones and the internet,19 and benefit from telemedicine visits,20 including when provided a telehealth tablet21.
In the present study, the majority of patients expressed interest in future video visits but were equivocal in their preference for video visits over clinic visits. In an international study of 6,326 community residents, there was high interest in the use of telemedicine consultation (56%), video consultation (37%), and patient-initiated digital services (56%).22 In a study on telehealth orthopedic services, 64% of respondents preferred video visits over clinic visits but 81% were concerned over the lack of physical contact during the examination. Despite patient and provider participation in telemedicine, it is unclear if the use and reliance on telemedicine will be sustained in the post-pandemic era.22,23 Healthcare facilities will have to monitor both patient and provider preferences for telemedicine visits after the COVID-19 pandemic and possibly tailor visits to select patient populations.
The present study has limitations. It was based on two hospitals within a single institution and may not reflect patient or provider experiences at other institutions. Most patients were of White race and the experience in other race/ethnic groups will require evaluation. However, the study also has strengths. PEARL was developed early in the COVID-19 pandemic to mitigate the effect of pandemic-related reduction in outpatient staff and services. PEARL expanded on the traditional role of HM-APPs and evaluated their role in virtual post-discharge care. PEARL represents a virtual platform that can continue after the COVID-19 pandemic and allow HM-APPs to improve post-discharge care. The present study formed the basis for our ongoing pragmatic randomized controlled trial (NCT04547803) to assess the effect of virtual visits on adherence to discharge recommendations.
In summary, PEARL was developed during the COVID-19 pandemic to optimize discharge care in the setting of reduced availability and accessibility of outpatient care. PEARL expanded beyond the traditional role of HM-APPs through a novel virtual post-discharge initiative. The results from our ongoing clinical trial, expected in late 2022–early 2023, will report the effect of post-discharge video visits on adherence to discharge recommendations and patient outcomes.
Conclusion
We developed PEARL for hospital medicine patients to reinforce discharge recommendations, improve post-discharge care, and overcome COVID-19 related reduction in availability and accessibility of outpatient care. Through scripted video visit encounters, HM-APPs reviewed discharge recommendations related to new medications, chronic medications, home equipment, and self-care. To our knowledge, the present study is the first to report the role of HM-APPs in post-discharge telemedicine care and formed the basis for our ongoing clinical trial on the effect of a virtual intervention to improve patient adherence to discharge recommendations.
Supplementary Material
Acknowledgments
We are grateful for input from PEARL group members: Gina Kesselring, Mary Jordan, Kristine Andrist, Megan Lunde, Katie Rieck, Holly Schenzel, Tamara Buechler, Lee M. Deetz, and Meltiady Issa (all, Division of Hospital Internal Medicine, Mayo Clinic, Rochester). We are grateful for support from Donna Lawson, Elizabeth L. Canan, Kevin J. Whitford (all, Division of Hospital Internal Medicine, Mayo Clinic, Rochester), Bradley J. Niebuhr, Lori J. Routh (Mayo Clinic Health System-Austin), and Laura E. Walker (Department of Emergency Medicine, Mayo Clinic, Rochester). We are grateful to Advanced Practice Providers for ongoing assistance with video visits and telephone follow-up: Christopher Edquist, Amanda Effertz, Andrew Elli, Tiffany Galush, Jyoti Gautam, Karissa Geisthardt, Laura Boldenow, Sally Heusinkvelt, Emily Isaacson, Jenna Jacobson, Evan Jones, Gina Kesselring, Jason Kraus, Sara Lewis, Tova Lyng, Fardowsa Mohamed, Katherine Pearson, Taryn Ragaisis, Melissa Sorenson, Leah Tucker, Tanner VanLith, Brittany Vlaminck, Papya Wriston (all, Division of Hospital Internal Medicine, Mayo Clinic, Rochester), and Sarah Gerard and Francis Owusu (both, Mayo Clinic Health System-Austin).
Funding
PEARL staff were employees of the study institution and were not additionally remunerated for the study. SBD is supported by a career development award from the National Institutes of Health/National Institute on Minority Health and Health Disparities (K23 MD016230) and by the Robert and Elizabeth Strickland Career Development Award, Mayo Clinic. This publication was made possible by the Mayo Clinic CTSA through grant number UL1TR002377 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health.
The funders had no role in study design, data analysis and interpretation; in writing of the manuscript; and in the decision to submit the manuscript for publication. The findings do not necessarily represent the views of the funders.
Footnotes
Presentations
An abstract on this topic was presented at the virtual 26th Mayo-KI Annual Scientific Research Meeting, September 9-10, 2020.
Conflict of Interest
The authors reported no conflict of interest.
References
- 1.Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med 2014;174:1095–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Auerbach AD, Kripalani S, Vasilevskis EE, et al. Preventability and Causes of Readmissions in a National Cohort of General Medicine Patients. JAMA Intern Med 2016;176:484–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Commonwealth Fund. The Impact of COVID-19 on Outpatient Visits in 2020: Visits Remained Stable, Despite a Late Surge in Cases 2021. [Google Scholar]
- 4.Rubin R COVID-19's Crushing Effects on Medical Practices, Some of Which Might Not Survive. JAMA 2020;324:321–3. [DOI] [PubMed] [Google Scholar]
- 5.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Trends in Outpatient Care Delivery and Telemedicine During the COVID-19 Pandemic in the US. JAMA Intern Med 2021;181:388–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chatterji P, Li Y. Effects of the COVID-19 Pandemic on Outpatient Providers in the United States. Med Care 2021;59:58–61. [DOI] [PubMed] [Google Scholar]
- 7.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. Journal of biomedical informatics 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Becker C, Zumbrunn S, Beck K, et al. Interventions to Improve Communication at Hospital Discharge and Rates of Readmission: A Systematic Review and Meta-analysis. JAMA Netw Open 2021;4:e2119346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dhalla IA, O'Brien T, Morra D, et al. Effect of a postdischarge virtual ward on readmission or death for high-risk patients: a randomized clinical trial. JAMA 2014;312:1305–12. [DOI] [PubMed] [Google Scholar]
- 11.McWilliams A, Roberge J, Anderson WE, et al. Aiming to Improve Readmissions Through InteGrated Hospital Transitions (AIRTIGHT): a Pragmatic Randomized Controlled Trial. J Gen Intern Med 2019;34:58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation In Telemedicine Use And Outpatient Care During The COVID-19 Pandemic In The United States. Health Aff (Millwood) 2021;40:349–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Czeisler M, Marynak K, Clarke KEN, et al. Delay or Avoidance of Medical Care Because of COVID-19-Related Concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep 2020;69:1250–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thomas-Jacques T, Jamieson T, Shaw J. Telephone, video, equity and access in virtual care. NPJ Digit Med 2021;4:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang J, Graetz I, Millman A, et al. Primary care telemedicine during the COVID-19 pandemic: patient's choice of video versus telephone visit. JAMIA Open 2022;5:ooac002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sinsky CA, Jerzak JT, Hopkins KD. Telemedicine and Team-Based Care: The Perils and the Promise. Mayo Clin Proc 2021;96:429–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eberly LA, Kallan MJ, Julien HM, et al. Patient Characteristics Associated With Telemedicine Access for Primary and Specialty Ambulatory Care During the COVID-19 Pandemic. JAMA Netw Open 2020;3:e2031640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rodriguez JA, Betancourt JR, Sequist TD, Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care 2021;27:21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lal S, Halicki-Asakawa A, Fauvelle A. A Scoping Review on Access and Use of Technology in Youth Experiencing Homelessness: Implications for Healthcare. Front Digit Health 2021;3:782145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adams CS, Player MS, Berini CR, et al. A Telehealth Initiative to Overcome Health Care Barriers for People Experiencing Homelessness. Telemed J E Health 2021;27:851–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garvin LA, Hu J, Slightam C, McInnes DK, Zulman DM. Use of Video Telehealth Tablets to Increase Access for Veterans Experiencing Homelessness. J Gen Intern Med 2021;36:2274–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neves AL, van Dael J, O'Brien N, et al. Use and impact of virtual primary care on quality and safety: The public's perspectives during the COVID-19 pandemic. J Telemed Telecare 2021:1357633x211066235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Puzzitiello RN, Moverman MA, Pagani NR, et al. Public perceptions and disparities in access to telehealth orthopaedic services in the COVID-19 era. J Natl Med Assoc 2021;113:405–13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.