Abstract
Background
The number of patients suffering from depression is continuously increasing in China. Demographic characteristics, physical health levels, and individual lifestyles/healthy behaviors are associated with the severity of depression. However, the major risk factor for depression remains unclear.
Materials and methods
In this investigation, 16,512 patients were screened using the CHARLS (China Health and Retirement Longitudinal Study) database after being determined to be eligible based on the inclusion criteria. Depressive symptoms were evaluated through the CESD-10 (10-item Center for Epidemiological Studies Depression Scale). Consequently, various models were developed based on potential predictive factors, employing stepwise LR (Logistic Regression)/RF (Random Forests) models to examine the influence and weighting of candidate factors that affect depression.
Results
Gender, residential address location, changes in health status following last interview, physical disabilities, chronic pain, childhood health status, ADL (activity of daily living), and social activity were all revealed to be independent risk factors for depression (p < 0.05) in this study. Depression has a synergic effect (across chronic pain and age groups). In comparison to other factors, RF results showed that chronic pain had a stronger impact on depression.
Conclusion
This preliminary study reveals that chronic pain is a major risk factor for depression.
Keywords: epidemiology, cross-sectional study, depression, major risk factor, chronic pain
Introduction
Depression is estimated to affect 322 million individuals worldwide, or 4.4% of the global population (1). The incidence of depression cases in China reached 90 million in 2020, making it the second-leading cause of human mortality, after cancer, with incidence numbers for depression cases in China reaching 90 million (2).
Depression is a prevalent chronic condition in the majority of the world’s population; it can impair normal functioning, cause depressive thoughts, and have a negative impact on the quality of life. Furthermore, individuals with severe depressive disorder have a higher risk of developing cardiovascular diseases and obtaining inadequate treatments, as well as a higher risk of morbidity and mortality (3, 4). The major risk for depression is determined by both genes and environmental factors (5). Among them, estimations of depression’s heritability based on twin studies are only about 37% (6), which is significantly less than the impact of environmental factors. Epidemiological studies have demonstrated that physical health, the lifestyle of childhood, and various stress events in life increase the incidence of depression in the middle-aged and elderly population (7–9). Due to the lack of nationally representative epidemiological data (including demographic profiling, health status and functioning, lifestyle behaviors, etc.) on depressive disorders in China (10), the main risk factors for depression in the Chinese middle-aged and elderly population are still unclear, much less identifying modifiable risk factors for depression to strategically prevent and intervene depressive disorders.
Most Chinese depression studies in recent years have been based on the CHARLS (CHARLS, China Health and Retirement Longitudinal Study), a large-scale epidemiological survey of nationwide middle-aged and older individuals that have been included in the depression scale since 2015. These studies separately examined the association between specific risk factors (e.g., chronic diseases, obesity, and physical activity) and depressive disorders, but a comprehensive, systematic analysis of the main risk factors for depression among middle-aged and elderly people in China is still lacking (11–13). Thus, major risk factors for depression were thoroughly and systematically investigated using cross-sectional data from CHARLS to identify feasible and efficient methods for reducing the incidence of depressive disorders.
Subjects, materials, and methods
Patients
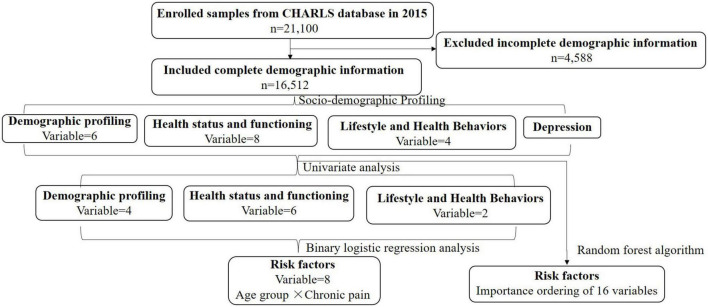
A total of 16,512 participants with complete demographic information were incorporated from 21,100 cases in the wave three surveys of CHARLS. Participants ranged in age from 20 to 102 years old. A flow chart of the consecutive analysis steps is depicted in Figure 1 (Supplementary materials and Supplementary methods. Subjects).
FIGURE 1.
The flowchart of the consecutive analysis steps.
Demographic profiling
Age, gender, residential address, location, birth address, and marital status were included among the demographic characteristics. Detailed classification criteria for these characteristics can be found in the demographic profiling section of Supplementary materials and Supplementary methods.
Health status and functioning
The direct inquiry was used to examine self-assessment of the state of health including the present state of health, changes in health status following last interview, physical disabilities, the loss of teeth, chronic pain, other medical diseases or conditions, and health status in childhood (Supplementary materials and Supplementary methods. Health status and functioning).
Activity of daily living evaluations
The actual physical function of the participants was assessed by ADL scales in this study (14). Participants were separated into three groups based on their overall ADL scores : NFI Group (NFI, No Functional Impairments), MFI Group (MFI, Mild Functional Impairments), and FI Group (FI, Functional Impairments) (15) (Supplementary materials and Supplementary methods. ADL evaluations).
Healthy/lifestyle behaviors
The direct inquiry was used to evaluate the healthy/lifestyle behaviors such as sporting activities, social activity, smoking, and frequency of drinking (Supplementary materials and Supplementary methods. Healthy/lifestyle behaviors).
Depressive symptom manifestations
The depressive symptom manifestations of the participants were assessed by the CESD-10 (CESD-10, 10-item Center for Epidemiological Studies Depression Scale) (16). Based on their CESD-10 scores, the participants were classified into three groups: D group (D, depression), DS group (DS, depressive symptoms), and NDS group (NDS, no depressive symptoms) (17) (Supplementary materials and Supplementary methods. Depressive symptom manifestations).
Statistical analyses
SPSS 26.0® (SPSS Inc.™, USA) was utilized to analyze data statistics, chi-square tests, and binary logistic regression. All p-values were two-sided, and p < 0.05 was considered statistically significant. The R package caret was used to implement the RF algorithm, which measures the risk factors that cause depression and ranks them by importance. Figure 1 depicts a flowchart of the consecutive analysis steps (Supplementary materials and Supplementary methods. Statistical analyses).
Results
Socio-demographic profiling
A total of 16,512 participants were included in the sample, including 8,024 men (48.59%) and 8,488 women (51.41%). According to new guidelines developed by the World Health Organization of the United Nations for the classification of age phases (18), participants in this study were divided into 908 (5.5%) young individuals (20–44 years old), 8,419 (50.99%) middle-aged individuals (45–59 years old), 6,219 (37.66%) younger-old individuals (60–74 years old), 949 (5.75%) older people (75–89 years old), and 17 (0.10%) longevity (above 90 years old). Approximately 98.48% of participants lived at home. The majority of participants (70.21%) resided in a village. Nearly 50% of participants’ birth address was identical to their permanent address. Approximately >80% were married, with a spouse present or cohabiting.
Over 50% of individuals had health conditions that may be considered fair. Following the previous interview, the health status of over 50% of participants remained the same. Only 1,778 (10.17%) people experienced physical impairments, while 663 (4.02%) had lost all of their teeth. In addition, 4,703 (28.48%) participants were frequently affected by chronic pain, 1,259 (7.62%) participants suffered from other medical diseases or conditions, 1,985 (12.02%) participants self-reported having an excellent health status during childhood, whereas the remaining participants, this was either outstanding (6,738; 40.81%), good (3,123; 18.91%), fair 3,656 (22.14%), or poor (1,010; 6.12%). The post-ADL examination revealed that 9,678 individuals (58.61%) had no functional impairments, 5,459 participants (33.06%) had mild functional impairments, and 1,375 individuals (8.33%) had functional impairments. Following post-classification based on a total depression score, 6,143 (37.20%) were assigned to the D group, 8,152 (49.37%) were assigned to the DS group, and 2,217 (13.43%) were assigned to the NDS group.
In terms of lifestyle, 8,194 participants (49.62%) engaged in at least 10 min of continuous physical activity, 7,123 individuals (43.14%) participated in social activities, and 6,586 individuals (39.89%) smoked, and 10,414 individuals (63.07%) did not use alcohol. Table 1 shows specific socio-demographic information for each record.
TABLE 1.
Sociodemographic characteristics description.
| Variables | Num (feq.%) |
| Demographic backgrounds | |
| Age (years old) | |
| 20–44 (young) | 908 (5.50) |
| 45–59 (middle-aged) | 8,419 (50.99) |
| 60–74 (young, older man) | 6,219 (37.66) |
| 75–89 (the aged) | 949 (5.75) |
| 90–110 (longevity) | 17 (0.10) |
| Gender | |
| Male | 8,024 (48.59) |
| Female | 8,488 (51.41) |
| Type of residential address | |
| Family housing | 16,261 (98.48) |
| Other | 251 (1.52) |
| Location of residential address | |
| Main city zone | 2,408 (14.58) |
| Combination-zone (urban-rural) | 830 (5.03) |
| Town/city-center | 925 (5.60) |
| ZhenXiang area | 756 (4.58) |
| Village | 11,593 (70.21) |
| Born address | |
| Permanent address | 7,709 (46.69) |
| Separate village/neighborhood within permanent address county/city/district | 5,743 (34.78) |
| Other county/city/district | 3,060 (18.53) |
| Marital status | |
| Married with spouse present/Cohabitated | 13,805 (83.61) |
| Married though temporarily apart due to employment | 992 (6.01) |
| Separated/divorced | 195 (1.18) |
| Widowed | 1,416 (8.58) |
| Never married | 104 (0.63) |
| Health status and functioning | |
| State of health | |
| Very good | 2,122 (12.85) |
| Good | 2,023 (12.25) |
| Fair | 8,453 (51.19) |
| Poor | 3,461 (20.96) |
| Very poor | 453 (2.74) |
| Changes in health status following last interview | |
| Better | 1,571 (9.51) |
| About the same | 8,188 (49.59) |
| Worse | 6,753 (40.90) |
| Physical disabilities | |
| No | 14,734 (89.23) |
| Yes | 1,778 (10.77) |
| The loss of teeth | |
| Yes | 663 (4.02) |
| No | 15,849 (95.98) |
| Chronic pain | |
| Yes | 4,703 (28.48) |
| No | 11,809 (71.52) |
| Other medical diseases or conditions | |
| Yes | 1,259 (7.62) |
| No | 15,253 (92.38) |
| Childhood health status | |
| Excellent | 1,985 (12.02) |
| Very good | 6,738 (40.81) |
| Good | 3,123 (18.91) |
| Fair | 3,656 (22.14) |
| Poor | 1,010 (6.12) |
| ADL | |
| No functional impairments (NFI group) | 9,678 (58.61) |
| Mild functional impairments (MFI group) | 5,459 (33.06) |
| Functional impairments (FI group) | 1,375 (8.33) |
| Lifestyle and health behaviors | |
| Sporting activities | |
| Yes | 8,194 (49.62) |
| No | 8,318 (50.38) |
| Social activity | |
| Yes | 7,123 (43.14) |
| No | 9,389 (56.86) |
| Smoking | |
| No | 9,926 (60.11) |
| Yes | 6,586 (39.89) |
| Frequency of drinking | |
| Drink more than once a month | 4,599 (27.85) |
| Drink but less than once a month | 1,499 (9.08) |
| Do not drink | 10,414 (63.07) |
| Depression | |
| No depressive symptoms (NDS group) | 2,217 (13.43) |
| Depressive symptoms (DS group) | 8,152 (49.37) |
| Depressive (D group) | 6,143 (37.20) |
Num, number; freq, frequency.
Associated factors for depression
Except for age, the variables in this study were all categorical. After the post-normality test, the age did not follow a normal distribution. According to the findings of the ROC curve for follow-up analysis, the study divided age into two groups, with ≤59 and >59 as categorical variables. In contrast to the variance inflation factor, which was significantly less than 10, the examination of collinearity revealed that tolerance was significantly greater than 0.1. There was consequently no collinearity between the independent variables. Univariate analysis revealed a significant difference (p < 0.05) between the NDS group and the combined D and DS groups in age, gender, place of residence, place of birth, state of health, changes in health status since the last interview, physical disabilities, chronic pain, childhood health status, ADL, social activity, and smoking (Table 2).
TABLE 2.
Univariate analysis of independent variables on depressive status.
| Depression |
χ2 | P-value | ||
| Variables | NDS group (n/%) | DS+D group (n/%) | ||
| Demographic backgrounds | ||||
| Age group | ||||
| Less than 59 years old | 1,107 (49.93) | 8,220 (57.50) | 44.751 | 2.24E-11 |
| More than 59 years old | 1,110 (50.07) | 6,075 (42.50) | ||
| Gender | ||||
| Male | 1,292 (58.28) | 6,732 (47.09) | 96.098 | 1.09E-22 |
| Female | 925 (41.72) | 7,563 (52.91) | ||
| Type of residential address | ||||
| Family housing | 2,185 (49.28) | 14,076 (49.23) | 0.101 | 0.751 |
| Other | 32 (0.72) | 219 (0.77) | ||
| Location of residential address | ||||
| Main city zone | 310 (6.99) | 2,098 (7.34) | 11.846 | 1.85E-02 |
| Combination-zone (urban-rural) | 101 (2.28) | 729 (2.55) | ||
| Town/city-center | 104 (2.35) | 821 (2.87) | ||
| ZhenXiang area | 84 (1.89) | 672 (2.35) | ||
| Village | 1,618 (36.49) | 9,975 (34.89) | ||
| Born address | ||||
| Permanent address | 1,140 (51.42) | 6,569 (45.95) | 25.883 | 2.40E-06 |
| Separate village/neighborhood within permanent address county/city/district | 677 (30.54) | 5,066 (35.44) | ||
| Other county/city/district | 400 (18.04) | 2,660 (18.61) | ||
| Marital status | ||||
| Married with spouse present/cohabitated | 1,881 (84.84) | 11,924 (83.41) | 5.882 | 0.208 |
| Married though temporarily apart due to employment | 129 (5.82) | 863 (6.04) | ||
| Separated/divorced | 19 (0.85) | 176 (1.23) | ||
| Widowed | 171 (7.72) | 1,245 (8.71) | ||
| Never married | 17 (0.77) | 87 (0.61) | ||
| Health status and functioning | ||||
| State of health | ||||
| Very good | 317 (14.30) | 1,805 (12.63) | 90.711 | 9.30E-19 |
| Good | 307 (13.85) | 1,716 (12.01) | ||
| Fair | 1,244 (56.11) | 7,209 (50.43) | ||
| Poor | 314 (14.16) | 3,147 (22.01) | ||
| Very poor | 35 (1.58) | 418 (2.92) | ||
| Changes in health status following last interview | ||||
| Better | 235 (10.60) | 1,336 (9.35) | 68.198 | 1.55E-15 |
| About the same | 1,253 (56.52) | 6,935 (48.51) | ||
| Worse | 729 (32.88) | 6,024 (42.14) | ||
| Physical disabilities | ||||
| No | 2,041 (92.06) | 12,693 (88.79) | 21.334 | 3.86E-06 |
| Yes | 176 (7.94) | 1,602 (11.21) | ||
| Loss of teeth | ||||
| Yes | 92 (4.15) | 571 (3.99) | 0.12 | 0.729 |
| No | 2,125 (95.85) | 13,724 (96.01) | ||
| Chronic pain | ||||
| Yes | 311 (14.03) | 4,392 (30.72) | 262.657 | 4.52E-59 |
| No | 1,906 (85.97) | 9,903 (69.28) | ||
| Other medical diseases or conditions | ||||
| Yes | 148 (6.68) | 1,111 (7.77) | 3.275 | 0.07 |
| No | 2,069 (93.32) | 13,184 (92.23) | ||
| Childhood health status | ||||
| Excellent | 218 (9.83) | 1,767 (12.36) | 27.638 | 1.48E-05 |
| Very good | 876 (39.51) | 5,862 (41.01) | ||
| Good | 463 (20.88) | 2,660 (18.61) | ||
| Fair | 546 (24.63) | 3,110 (21.76) | ||
| Poor | 114 (5.15) | 896 (6.26) | ||
| ADL | ||||
| No functional impairments (NFI group) | 1,528 (68.92) | 8,150 (57.01) | 118.191 | 2.16E-26 |
| Mild functional impairments (MFI group) | 578 (26.07) | 4,881 (34.14) | ||
| Functional impairments (FI group) | 111 (5.01) | 1,264 (8.85) | ||
| Lifestyle and health behaviors | ||||
| Sporting activities | ||||
| Yes | 1,135 (51.20) | 7,059 (49.38) | 2.528 | 0.112 |
| No | 1,082 (48.80) | 7,236 (50.62) | ||
| Social activity | ||||
| Yes | 1,122 (50.61) | 6,001 (41.98) | 58.265 | 2.29E-14 |
| No | 1,095 (49.39) | 8,294 (58.02) | ||
| Smoking | ||||
| No | 1,208 (54.49) | 8,718 (60.99) | 33.803 | 6.10E-09 |
| Yes | 1,009 (45.51) | 5,577 (39.01) | ||
| Frequency of drinking | ||||
| Drink more than once a month | 651 (29.36) | 3,948 (27.62) | 3.238 | 0.198 |
| Drink but less than once a month | 190 (8.57) | 1,309 (9.16) | ||
| Do not drink | 1,376 (62.07) | 9,038 (63.22) | ||
Num, number; %, frequency.
Logistic regression analysis for depression
Further logistic regression analysis revealed eight independent risk factors for depression among all 12 variables, including gender, residential address location, changes in health status following the last interview, physical disabilities, chronic pain, childhood health status, ADL, and social activity (p < 0.05) (Table 3). Notably, individuals above the age of 59 who did not have chronic pain were protected from depression, and the results of these datasets also revealed a synergic effect between chronic pain and age group.
TABLE 3.
Binary logistic regression analysis of related factors of depressive symptoms.
| Variables | B | SE | Wald | P-value | OR | 95% CI | |
| Gender | Male | ||||||
| Female | 0.317 | 0.048 | 43.539 | 4.155E-11 | 1.373 | 1.250–1.509 | |
| Location of residential address | Main city zone | 13.763 | 0.008 | ||||
| Combination-zone (urban-rural) | 0.023 | 0.124 | 0.036 | 0.850 | 1.024 | 0.803–1.306 | |
| Town/city-center | 0.053 | 0.122 | 0.190 | 0.663 | 1.055 | 0.830–1.341 | |
| ZhenXiang area | 0.078 | 0.133 | 0.348 | 0.555 | 1.081 | 0.834–1.403 | |
| Village | –0.168 | 0.068 | 6.019 | 0.014 | 0.845 | 0.739–0.967 | |
| Changes in health status following last interview | Better | 9.837 | 0.007 | ||||
| About the same | 0.036 | 0.079 | 0.212 | 0.645 | 1.037 | 0.889–1.210 | |
| Worse | 0.189 | 0.083 | 5.174 | 0.023 | 1.208 | 1.027–1.422 | |
| Physical disabilities | No | ||||||
| Yes | 0.205 | 0.086 | 5.656 | 0.017 | 1.228 | 1.037–1.454 | |
| Chronic pain | Yes | ||||||
| No | –0.623 | 0.075 | 69.833 | 6.453E-17 | 0.536 | 0.464–0.621 | |
| Childhood health status | Excellent | 21.085 | 3.046E-04 | ||||
| Very good | –0.162 | 0.082 | 3.921 | 0.048 | 0.851 | 0.725–0.998 | |
| Good | –0.345 | 0.089 | 14.878 | 1.147E-04 | 0.709 | 0.595–0.844 | |
| Fair | –0.290 | 0.087 | 11.052 | 0.001 | 0.748 | 0.631–0.888 | |
| Poor | –0.088 | 0.125 | 0.492 | 0.483 | 0.916 | 0.717–1.171 | |
| ADL | NFI group | 28.206 | 7.502E-07 | ||||
| MFI group | 0.261 | 0.057 | 21.228 | 4.077E-06 | 1.298 | 1.162–1.451 | |
| FI group | 0.410 | 0.111 | 13.580 | 2.286E-04 | 1.507 | 1.212–1.875 | |
| Social activity | Yes | ||||||
| No | 0.373 | 0.047 | 61.846 | 3.715E-15 | 1.452 | 1.323–1.593 | |
| Age group × Chronic pain | –0.405 | 0.052 | 60.268 | 8.277E-15 | 0.667 | 0.602–0.739 | |
| Constant | 2.249 | 0.138 | 265.396 | 1.144E-59 | 9.474 |
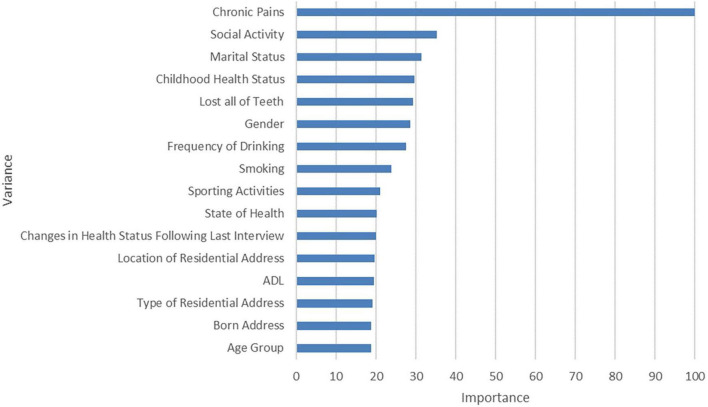
Feature importance analysis
Figure 2 displays the characteristics of the RF model for predicting the result of depression in the order of permutation importance. The y-axis displays the predictive variables, while the x-axis displays the feature important scores. The predictive variables were scored from high to low. Regarding interpersonal communications, the “chronic pain” variable scored the highest in this model, followed by “social activity” and “marital status.” Regarding this dataset results, RF outperforms LR with an AU-ROC score of 70.0%, whereas LR had an AU-ROC score of 65.5% (Supplementary Figure 1).
FIGURE 2.
Permutation importance of features in random forest model.
Discussion
Depression is a highly prevalent condition that severely limits psychosocial function and, as a result, reduces life quality (19), contributing to the majority of global health burdens (20). Depression is expected to be the greatest worldwide health burden by 2,030, according to the WHO (19). Working-age adults in China have a high risk of developing depression, which has different degrees of negative effects on their health and longevity. In addition, the onset and severity of depression symptoms tend to increase with age, which is extremely undesirable for the current trend of the Chinese population aging (13). Therefore, it is urgent to explore the main risk factors affecting the occurrence of depression in China, especially in middle-aged and elderly people.
Depression and basic characteristics of the individual
Depression is a condition that can be influenced by individual differences (21). According to studies, the prevalence of depression is twice as high in women as in men (22). The results of this study also indicated that women are at risk factors for developing depression (p < 0.01, OR = 1.373) (Table 3). This could be related to the fact that males and females have distinct biological patterns. The findings revealed that women have higher levels of inflammatory, neurotrophic, and serotonergic markers than men, which may be the biological basis for sex differences in depression (22). Due to the influence of gender and age, marital status has also emerged as one of the risk factors for depression (23). This could also explain why the marital status was not found to be an independent risk factor for depression in the findings of this study. Moreover, the residence is a significant influence on depression. Compared to living in a village and having a permanent address, city life is associated with negative mental health outcomes due to work stress, loss of communication with friends and family in the neighborhood, overcrowding, heavy traffic, and lack of green spaces (24).
Depression and health status and functioning
From a cultural perspective, physical health was given preferential treatment over mental health throughout China (25). Changes in health status following last interview, physical disabilities, health status in childhood, chronic pain, and ADL as defined by physical health were also found to be independent risk factors for depression in this study (p < 0.05) (Table 3). Among them, chronic pain is more significantly related to depression than other variables. Studies conducted in clinical settings demonstrated that chronic pain is a stressful event or condition that frequently promotes depressive disorders, with strong depressive symptoms present in roughly 85% of chronic pain cases. Depression symptom presentation is more prevalent among older patients with chronic pain than among older patients without chronic pain (26). In addition, the prognosis for patients with depression caused by chronic pain was worse than for those with chronic pain alone. Exploring its biological molecular mechanism, it was found that inflammatory signals and monoamine neurotransmitters such as 5-HT (5-HT, serotonin), DA (DA, dopamine), NE (NE, norepinephrine), and glutamate were the key molecules for chronic pain to induce depression (27).
A substantial positive correlation between physical health multimorbidity and depression was discovered in 42 countries, with notably high odds ratios in China, Laos, Ethiopia, the Philippines, and Malaysia, according to a comprehensive international investigation (28). Another CHARLS-based study indicated that individuals with chronic diseases or multimorbidity are more likely to be depressed in the elderly Chinese population, indicating the importance of assessing depressive symptoms in patients who exhibit poor physical performance (11). Other investigations have found a correlation between childhood obesity and an increased incidence of depression in old age (29). In addition to the psychological impact of life’s inconveniences, adults with physical disabilities have fewer opportunities for positive communication with the outside world, which contributes to their greater risk of depression (30). Similarly, CHARLS-based studies demonstrated that social support moderates the influence of disability on depression symptoms (31).
Depression and healthy/lifestyle behaviors
There is currently a large and validated research base showing lifestyle behaviors as an important cause of depression. These behaviors may be particularly essential in the development and progression of depression (32). For example, good social relationships can play a protective role against the onset of depressive symptoms, particularly in late-life depression (33), which is consistent with the findings of this study in both LR and RF. Physical activity has also been shown to considerably lower the risk of depression and to have antidepressant effects. Physical activity has been shown to influence the onset and progression of depression by altering neuroplasticity, inflammation, oxidative stress, the endocrine system, self-esteem, social support, and self-efficacy (34). Regarding smoking and alcohol use in this study, numerous studies have found a positive relationship between smoking/excessive alcohol consumption and the onset and development of depression (35, 36). Therefore, healthy activities are not only advantageous for maintaining physical health, but they can also have a direct impact on mental health. Through early lifestyle interventions, depression can be prevented or delayed in its onset and progression.
Strengths and limitation
The primary risk factors for depression in middle-aged and elderly people in China were thoroughly and systematically examined in this study. As a result, according to recent research findings, the chance of developing depression will be significantly reduced if physical health (particularly for the treatment of chronic pain) and lifestyle improvements are identified and implemented promptly and effectively. In the meantime, both LR and RF were used to account for possible overall weighting of the main risk factors (25). The findings of the two models also showed excellent consistency. This study may investigate potential relationships between chronic pain and depression.
In fact, in addition to the influencing factors of depression covered in this study, other factors such as type of tea consumption (37), sleep quality (38), and spirituality/religion (39) are also included. Recent research has demonstrated that religion can be beneficial for modifying lifestyle and enhancing psychological health (40). Harvard University,1 Duke University,2 and Adventist Religion and Health Study3 have carried out research work related to religion. However, due to the lack of relevant data in the CHARLS, this study was not included in the analysis, and it is anticipated that this part will be conducted in the future.
Additionally, depression may be described in a variety of ways utilizing various assessment methods. The ability to compare prevalence estimates from multiple studies employing different depression definitions is limited. Moreover, self-reported health conditions and lifestyle choices may have contributed to memory bias in this study. Even though the AU-ROC scores for the sensitivity analysis were all lower, it demonstrated that chronic pain had a substantial impact on depression using the LR/RF model, which could be related to recall bias.
Conclusion
In conclusion, this study focused on how physical health and lifestyle affect psychological depression in the Chinese community before identifying that chronic pain had a substantial influence on depression. The comparison analysis of the LR and RF results further supported the consistency of the relationship between chronic pain and depression. Future studies will concentrate on looking for such follow-up data, with an emphasis on the association between depression and chronic pain.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: The datasets generated for this study can be found in the China Health and Retirement Longitudinal Study (CHARLS) online datasets (https://charls.charlsdata.com/pages/Data/2015-charls-wave4/zh-cn.html).
Ethics statement
Our protocols followed the Declaration of Helsinki and received approval from the Ethical Board at Beijing Hospital, Ministry of Health (2019BJYYEC-118-02). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
XN and HS contributed to the conception and design of the study and drafted the manuscript. YL, RL, CC, DZ, and QC interpreted the data. ZY, LS, QZ, XZ, DG, SF, and SZ analyzed the data and helped revise the manuscript. CH, GP, and HY helped revise the manuscript. All authors read and approved the final manuscript.
Acknowledgments
We thank the CHARLS team for their hard work and unselfish sharing of survey data. The protocols followed the Declaration of Helsinki and received approval from the Ethical Review Committee (IRB) of Peking University (IRB 00001052-11014).
Abbreviations
- CHARLS
the China Health and Retirement Longitudinal Study
- CESD-10
the 10-item Center for Epidemiological Studies Depression Scale
- LR
logistic regression
- RF
Random Forests
- ADL
activity of daily living
- D
depression group
- DS
depressive symptoms
- NDS
the no depressive symptoms
- AUC
the area under the curve
- NFI group
No Functional Impairments
- MFI
Mild Functional Impairments
- FI
Functional Impairments
- 5-HT
serotonin
- DA
dopamine
- NE
norepinephrine.
Footnotes
Funding
This work was supported by the National Key Research and Development Program of China (2018YFC2000400), Natural Science Foundation of China (82260289, 81870552, 81400790, 81600622, 71490732, 81849132, 81460203, 31760299, 81571385, 91849132, 91849118, and 81872096), Guangxi Natural Science Foundation (2014GXNSFDA118028, 2018GXNSFAA138156, and guike0991198), Self-funded Scientific Research Project of the health and family planning commission of Guangxi Zhuang Autonomous Region (Z20170162), Beijing Hospital Doctoral Scientific Research Foundation (BJ-2018-024), Beijing Hospital Nova Project (BJ-2018-139), and Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (2018RC330003).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.986389/full#supplementary-material
References
- 1.Guo Y, Sun J, Hu S, Nicholas S, Wang J. Hospitalization costs and financial burden on families with children with depression: a cross-section study in shandong province, China. Int J Environ Res Public Health. (2019) 16:3526. 10.3390/ijerph16193526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sun X, Zhou M, Huang L, Nuse B. Depressive costs: medical expenditures on depression and depressive symptoms among rural elderly in China. Public Health. (2020) 181:141–50. 10.1016/j.puhe.2019.12.011 [DOI] [PubMed] [Google Scholar]
- 3.Wilkinson P, Ruane C, Tempest K. Depression in older adults. BMJ. (2018) 363:k4922. 10.1136/bmj.k4922 [DOI] [PubMed] [Google Scholar]
- 4.Liu Q, He H, Yang J, Feng X, Zhao F, Lyu J. Changes in the global burden of depression from 1990 to 2017: findings from the global burden of disease study. J Psychiatric Res. (2020) 126:134–40. 10.1016/j.jpsychires.2019.08.002 [DOI] [PubMed] [Google Scholar]
- 5.Penner-Goeke S, Binder EB. Epigenetics and depression. Dialogues Clin Neurosci. (2019) 21:397–405. 10.31887/DCNS.2019.21.4/ebinder [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dall’Aglio L, Lewis CM, Pain O. Delineating the genetic component of gene expression in major depression. Biol psychiatry. (2021) 89:627–36. 10.1016/j.biopsych.2020.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Almeida OP. Prevention of depression in older age. Maturitas. (2014) 79:136–41. 10.1016/j.maturitas.2014.03.005 [DOI] [PubMed] [Google Scholar]
- 8.Manger S. Lifestyle interventions for mental health. Australian J General Pract. (2019) 48:670–3. 10.31128/AJGP-06-19-4964 [DOI] [PubMed] [Google Scholar]
- 9.Zdanowicz N, Reynaert C, Jacques D, Lepiece B, Godenir F, Pivont V, et al. Depression and physical health, the therapeutic alliance, and anti-depressants. Psychiatria Danubina. (2018) 30:401–4. [PubMed] [Google Scholar]
- 10.Lu J, Xu X, Huang Y, Li T, Ma C, Xu G, et al. Prevalence of depressive disorders and treatment in China: a cross-sectional epidemiological study. Lancet Psychiatry. (2021) 8:981–90. 10.1016/S2215-036600251-0 [DOI] [PubMed] [Google Scholar]
- 11.Jiang CH, Zhu F, Qin TT. Relationships between chronic diseases and depression among middle-aged and elderly people in China: a prospective study from CHARLS. Curr Med Sci. (2020) 40:858–70. 10.1007/s11596-020-2270-5 [DOI] [PubMed] [Google Scholar]
- 12.Luo H, Li J, Zhang Q, Cao P, Ren X, Fang A, et al. Obesity and the onset of depressive symptoms among middle-aged and older adults in China: evidence from the CHARLS. BMC Public Health. (2018) 18:909. 10.1186/s12889-018-5834-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang R, Bishwajit G, Zhou Y, Wu X, Feng D, Tang S, et al. Intensity, frequency, duration, and volume of physical activity and its association with risk of depression in middle- and older-aged Chinese: evidence from the China health and retirement longitudinal study, 2015. PLoS One. (2019) 14:e0221430. 10.1371/journal.pone.0221430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feng Z, Li Q, Zhou L, Chen Z, Yin W. The relationship between depressive symptoms and activity of daily living disability among the elderly: results from the China health and retirement longitudinal study (CHARLS). Public Health. (2021) 198:75–81. 10.1016/j.puhe.2021.06.023 [DOI] [PubMed] [Google Scholar]
- 15.Li ZZ, Tang Z, Wang R. [Status of elderly disability in 7 cities of China]. Zhonghua Liu Xing Bing Xue Za Zhi. (2016) 37:1561–4. 10.3760/cma.j.issn.0254-6450.2016.12.001 [DOI] [PubMed] [Google Scholar]
- 16.Chen H, Mui AC. Factorial validity of the center for epidemiologic studies depression scale short form in an older population in China. Int Psychoger. (2014) 26:49–57. 10.1017/S1041610213001701 [DOI] [PubMed] [Google Scholar]
- 17.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (center for epidemiologic studies depression scale). Am J Prevent Med. (1994) 10:77–84. [PubMed] [Google Scholar]
- 18.Medina-Solís CE, Pérez-Núñez R, Maupomé G, Avila-Burgos L, Pontigo-Loyola AP, Patiño-Marín N, et al. National survey on edentulism and its geographic distribution, among mexicans 18 years of age and older (with emphasis in WHO age groups). J Oral Rehabilit. (2008) 35:237–44. 10.1111/j.1365-2842.2007.01767.x [DOI] [PubMed] [Google Scholar]
- 19.Malhi GS, Mann JJ. Depression. Lancet. (2018) 392:2299–312. 10.1016/S0140-673631948-2 [DOI] [PubMed] [Google Scholar]
- 20.Meng R, Yu C, Liu N, He M, Lv J, Guo Y, et al. Association of depression with all-cause and cardiovascular disease mortality among adults in China. JAMA Network Open. (2020) 3:e1921043. 10.1001/jamanetworkopen.2019.21043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guyon-Harris KL, Taraban L, Bogen DL, Wilson MN, Shaw DS. Individual differences in symptoms of maternal depression and associations with parenting behavior. J Family Psychol JFP J Div Family Psychol Am Psychol Assoc. (2022) 36:681–91. 10.1037/fam0000988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Labaka A, Goñi-Balentziaga O, Lebeña A, Pérez-Tejada J. Biological sex differences in depression: a systematic review. Biol Res Nurs. (2018) 20:383–92. 10.1177/1099800418776082 [DOI] [PubMed] [Google Scholar]
- 23.Bulloch A, Williams J, Lavorato DH, Patten SB. The depression and marital status relationship is modified by both age and gender. J Affect Dis. (2017) 223:65–8. 10.1016/j.jad.2017.06.007 [DOI] [PubMed] [Google Scholar]
- 24.Ram B, Limb ES, Shankar A, Nightingale CM, Rudnicka AR, Cummins S, et al. Evaluating the effect of change in the built environment on mental health and subjective well-being: a natural experiment. J Epidemiol Community Health. (2020) 74:631–8. 10.1136/jech-2019-213591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tang X, Qi S, Zhang H, Wang Z. Prevalence of depressive symptoms and related factors among China’s older adults in 2016. J Affect Dis. (2021) 292:95–101. 10.1016/j.jad.2021.04.041 [DOI] [PubMed] [Google Scholar]
- 26.Nguyen AT, Nguyen T, Nguyen T, Nguyen H, Nguyen TX, Nguyen TN, et al. Chronic pain and associated factors related to depression among older patients in hanoi, vietnam. Int J Environ Res Public Health. (2021) 18:9192. 10.3390/ijerph18179192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sheng J, Liu S, Wang Y, Cui R, Zhang X. The link between depression and chronic pain: neural mechanisms in the brain. Neural Plasticity. (2017) 2017:9724371. 10.1155/2017/9724371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stubbs B, Vancampfort D, Veronese N, Kahl KG, Mitchell AJ, Lin PY, et al. Depression and physical health multimorbidity: primary data and country-wide meta-analysis of population data from 190 593 people across 43 low- and middle-income countries. Psychol Med. (2017) 47:2107–17. 10.1017/S0033291717000551 [DOI] [PubMed] [Google Scholar]
- 29.Gibson-Smith D, Halldorsson TI, Bot M, Brouwer IA, Visser M, Thorsdottir I, et al. Childhood overweight and obesity and the risk of depression across the lifespan. BMC Pediatrics. (2020) 20:25. 10.1186/s12887-020-1930-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tough H, Siegrist J, Fekete C. Social relationships, mental health and wellbeing in physical disability: a systematic review. BMC Public Health. (2017) 17:414. 10.1186/s12889-017-4308-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Su D, Chen Z, Chang J, Gong G, Guo D, Tan M, et al. Effect of social participation on the physical functioning and depression of empty-nest elderly in china: evidence from the china health and retirement longitudinal survey (CHARLS). Int J Environ Res Public Health. (2020) 17:9438. 10.3390/ijerph17249438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Berk M, Sarris J, Coulson CE, Jacka FN. Lifestyle management of unipolar depression. Acta Psychiatrica Scand Supple. (2013) 443:38–54. 10.1111/acps.12124 [DOI] [PubMed] [Google Scholar]
- 33.Hodgetts S, Gallagher P, Stow D, Ferrier IN, O’Brien JT. The impact and measurement of social dysfunction in late-life depression: an evaluation of current methods with a focus on wearable technology. Int J Geriatric Psychiatry. (2017) 32:247–55. 10.1002/gps.4632 [DOI] [PubMed] [Google Scholar]
- 34.Kandola A, Ashdown-Franks G, Hendrikse J, Sabiston CM, Stubbs B. Physical activity and depression: towards understanding the antidepressant mechanisms of physical activity. Neurosci Biobehav Rev. (2019) 107:525–39. 10.1016/j.neubiorev.2019.09.040 [DOI] [PubMed] [Google Scholar]
- 35.Fluharty M, Taylor AE, Grabski M, Munafò MR. The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tobacco Res Offi J Soc Res Nicotine Tobacco. (2017) 19:3–13. 10.1093/ntr/ntw140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boden JM, Fergusson DM. Alcohol and depression. Addiction. (2011) 106:906–14. 10.1111/j.1360-0443.2010.03351.x [DOI] [PubMed] [Google Scholar]
- 37.Yao Y, Chen H, Chen L, Ju SY, Yang H, Zeng Y, et al. Type of tea consumption and depressive symptoms in Chinese older adults. BMC Geriat. (2021) 21:331. 10.1186/s12877-021-02203-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guo H, Zhang Y, Wang Z, Shen H. Sleep quality partially mediate the relationship between depressive symptoms and cognitive function in older Chinese: a longitudinal study across 10 years. Psychol Res Behav Manage. (2022) 15:785–99. 10.2147/PRBM.S353987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Koenig HG, Pearce MJ, Nelson B, Erkanli A. Effects on daily spiritual experiences of religious versus conventional cognitive behavioral therapy for depression. J Religion Health. (2016) 55:1763–77. 10.1007/s10943-016-0270-3 [DOI] [PubMed] [Google Scholar]
- 40.Abdala GA, Meira M, Rodrigo GT, Fróes M, Ferreira MS, Abdala SA, et al. Religion, age, education, lifestyle, and health: structural equation modeling. J Religion Health. (2021) 60:517–28. 10.1007/s10943-020-01034-3 [DOI] [PubMed] [Google Scholar]
- 41.Chan S, Jia S, Chiu H, Chien WT, Thompson R, Hu Y, et al. Subjective health-related quality of life of Chinese older persons with depression in Shanghai and Hong Kong: relationship to clinical factors, level of functioning and social support. Int J Geriatric Psychiatry. (2009) 24:355–62. 10.1002/gps.2129 [DOI] [PubMed] [Google Scholar]
- 42.Dennis M, Baillon S, Brugha T, Lindesay J, Stewart R, Meltzer H. The influence of limitation in the activity of daily living and physical health on suicidal ideation: results from a population survey of great britain. Soc Psychiatry Psychiatric Epidemiol. (2009) 44:608–13. 10.1007/s00127-008-0474-2 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: The datasets generated for this study can be found in the China Health and Retirement Longitudinal Study (CHARLS) online datasets (https://charls.charlsdata.com/pages/Data/2015-charls-wave4/zh-cn.html).