Abstract
Background
BOADICEA (Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm) for breast cancer and the epithelial tubo-ovarian cancer (EOC) models included in the CanRisk tool (www.canrisk.org) provide future cancer risks based on pathogenic variants in cancer-susceptibility genes, polygenic risk scores, breast density, questionnaire-based risk factors and family history. Here, we extend the models to include the effects of pathogenic variants in recently established breast cancer and EOC susceptibility genes, up-to-date age-specific pathology distributions and continuous risk factors.
Methods
BOADICEA was extended to further incorporate the associations of pathogenic variants in BARD1, RAD51C and RAD51D with breast cancer risk. The EOC model was extended to include the association of PALB2 pathogenic variants with EOC risk. Age-specific distributions of oestrogen-receptor-negative and triple-negative breast cancer status for pathogenic variant carriers in these genes and CHEK2 and ATM were also incorporated. A novel method to include continuous risk factors was developed, exemplified by including adult height as continuous.
Results
BARD1, RAD51C and RAD51D explain 0.31% of the breast cancer polygenic variance. When incorporated into the multifactorial model, 34%–44% of these carriers would be reclassified to the near-population and 15%–22% to the high-risk categories based on the UK National Institute for Health and Care Excellence guidelines. Under the EOC multifactorial model, 62%, 35% and 3% of PALB2 carriers have lifetime EOC risks of <5%, 5%–10% and >10%, respectively. Including height as continuous, increased the breast cancer relative risk variance from 0.002 to 0.010.
Conclusions
These extensions will allow for better personalised risks for BARD1, RAD51C, RAD51D and PALB2 pathogenic variant carriers and more informed choices on screening, prevention, risk factor modification or other risk-reducing options.
Keywords: genetic counseling
WHAT IS ALREADY KNOWN ON THIS TOPIC
Pathogenic variants in BARD1, RAD51C and RAD51D have recently been established as breast cancer susceptibility genes, and pathogenic variants in PALB2 have been shown to be associated with epithelial ovarian cancer risk. No cancer risk prediction model currently exists which incorporates these associations.
WHAT THIS STUDY ADDS
The BOADICEA (Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm) multifactorial breast and ovarian cancer risk prediction model has been extended to incorporate these associations and has been implemented in the CanRisk tool (www.canrisk.org) for use by healthcare professionals.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE AND/OR POLICY
The enhanced risk prediction models will enable healthcare professionals to provide personalised breast and epithelial ovarian cancer risks to BARD1, RAD51C, RAD51D and PALB2 pathogenic variant carriers and will allow for more informed choices on cancer risk management options.
Introduction
Breast cancer (BC) and epithelial tubo-ovarian cancer (EOC) are two of the most common cancers in women.1 2 Through mammography or other methods, screening for BC can reduce mortality, and organised screening is available in most developed countries.3 For EOC, no effective screening exists, but the disease can be prevented by salpingo-oophorectomy. However, these preventative options are associated with adverse effects. Therefore, identifying those at increased risk may help to target screening and preventative options to those most likely to benefit.4 Both BC and EOC risks are multifactorial diseases, with family history of cancer (FH), genetic factors and lifestyle, hormonal and reproductive risk factors (RFs) all contributing to risk.5–7
Previously we developed the BOADICEA (Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm) model for BC risk prediction and for the likelihood of carrying pathogenic variants (PVs) in BC susceptibility genes. BOADICEA v5 incorporates the effects of PVs in five BC susceptibility genes (BRCA1, BRCA2, PALB2, CHEK2 and ATM), the effects of known common genetic variants summarised as a polygenic risk score (PRS, accounting for ~20% of the polygenic variance), and a polygenic component that accounts for any residual familial aggregation.8 9 We also developed a similar EOC model (Ovarian Cancer Model v1) that considers the effects of PVs in BRCA1, BRCA2, RAD51D, RAD51C and BRIP1 on EOC together with a PRS (accounting for ~5% of the polygenic variance) and a residual polygenic component.10 11 BOADICEA includes mammographic density and both models incorporate the effects of known lifestyle, hormonal, reproductive and anthropometric RFs. In addition, the models incorporate breast tumour heterogeneity by considering the distributions of tumour oestrogen receptor (ER) and triple-negative (TN) (ER, progesterone receptor and human epidermal growth factor receptor 2 negative) status for BRCA1 and BRCA2 PV carriers and the general population.12 13 Both models are freely available to healthcare professionals via the CanRisk webtool (www.canrisk.org) and are widely used by healthcare professionals.14
Recently, large population-based and family-based targeted sequencing studies have established that PVs in RAD51C, RAD51D and BARD1 are associated with BC risk15 16 and that PVs in PALB2 are associated with EOC risk.17 18 In addition, analysis of the tumour characteristics in the BRIDGES study has provided age-specific estimates of the distributions of tumour characteristics for PV carriers in all established susceptibility genes.19
A further limitation of the previous models is that all epidemiological RFs are treated as categorical. However, some RFs (eg, height, body mass index (BMI) mammographic density) are intrinsically continuous, and discretisation results in a loss of information, reducing their predictive ability.
Here we extend both models to explicitly model the effects of PVs in the recently established BC and EOC susceptibility genes and incorporate up-to-date age-specific pathology distributions. We present a methodological framework for incorporating continuous RFs into the model, and we demonstrate this by including height as a continuous variable. Finally, we describe updates to the population reference cancer incidence rates used in the models by incorporating more up-to-date incidences, incidences for additional countries and refining the derivation of birth-cohort-specific incidences for inclusion in the models that address sparsity in the population incidence data.
Methods
Rare moderate-risk pathogenic variants
Both BOADICEA and the EOC models, model cancer incidence as an explicit function of PVs in known high- and moderate-penetrance susceptibility genes (major genes) together with a polygenic component.9–12 20–22 By using an explicit genetic model, they can account for both genetic testing and detailed FH. BOADICEA includes the genes BRCA1, BRCA2, PALB2, CHEK2 and ATM, with dominance in that order, along with a BC susceptibility polygenic component. The EOC model includes the genes BRCA1, BRCA2, RAD51D, RAD51C and BRIP1, with dominance in that order, along with an EOC susceptibility polygenic component. Details of the underlying model are included in the online supplemental material. The values of the parameters for the original models were determined by complex segregation analysis.9 10 However, this was not possible for the extended versions since no sufficiently large dataset containing all the model features was available. Instead, we adopted a synthetic approach,23 in which additional model parameters are taken from large-scale external studies.8 11 12 21
jmedgenet-2022-108471supp001.pdf (1.3MB, pdf)
Here, BOADICEA was extended to explicitly model the effects of PVs in BARD1, RAD51C and RAD51D (i.e. in total, eight BC susceptibility genes), while the EOC model was extended to include PALB2 (i.e. in total, six EOC susceptibility genes). In both models, the effects of PVs were included as major genes and are parameterised by their allele frequency in the general population and their age-specific relative risks (RRs). The BC RR for carriers of PV in BARD1 was taken from the BRIDGES study,15 while those for RAD51C and RAD51D were the meta-analysed values from Dorling et al 15 and Yang et al.24 The EOC RR for PALB2 PV carriers was taken from Yang et al.17 The BRIDGES study15 suggested that the RR estimates associated with PVs in ATM are lower than the previously assumed estimate of 2.8,21 and it was therefore updated to the Dorling et al 15 estimate. The previously assumed RR estimates for PVs in BRCA1, BRCA2, PALB2 and CHEK2 8 21 were based on large studies that enabled the estimation of age-specific risks or were estimated as part of the BOADICEA model fitting process, and were not updated, except for the BRCA2-associated EOC RRs for ages 59 and over (online supplemental material). The PV carrier frequencies for PALB2, CHEK2 (including all PVs), ATM, BARD1, RAD51D, RAD51C and BRIP1 and screening test sensitivities for all genes were derived from Dorling et al.15 We used the BRIDGES study to derive these frequency estimates as it is a very large population-based dataset that includes targeted sequencing data. Frequencies were based on the control frequencies in European populations, adjusted for the assumed sensitivity of the sequencing and the fact that large rearrangements were not detectable (online supplemental material). The default sensitivities were then calculated, assuming that clinical genetic testing will detect all known pathogenic mutations except for large rearrangements (except BRCA1 and BRCA2, where testing for large rearrangements is routinely done). All model parameters for PVs are given in table 1.
Table 1.
Parameters used to include the effects of rare high-risk and intermediate-risk pathogenic variants in the models
| Gene | Allele Freq | SS | RR of female breast cancer (95% CI) | RR of EOC (95% CI) | RR of male breast cancer (95% CI) | RR of Prostate cancer | RR of pancreatic cancer (95% CI) | |||||
| BRCA1 | BOADICEA | 0.89 | 1 | age<20 | 1 | age<30 | 8 | |||||
| 0.0006394 | exp (3.0146+0.02412× age) | 20≤age≤29 | exp (−3.55+0.1986× age) | 30≤age≤39 | 1.82 | age<65 | 3.10 | age<65 | ||||
| exp (6.0707−0.07775×age) | 30≤age≤39 | exp (7.1776−0.06959×age) | 40≤age≤49 | 0.84 | age≥65 | 1.54 | age≥65 | |||||
| EOC model | exp (4.2511−0.03226×age) | 40≤age≤49 | exp (4.5236−0.01651×age) | 50≤age≤79 | ||||||||
| 0.0007947 | exp (4.2086−0.03141×age) | 50≤age≤79 | ||||||||||
| BRCA2 | BOADICEA | 0.96 | 1 | age<20 | 1 | age<40 | 80 | 7.33 | age<65 | 5.54 | age<65 | |
| 0.00102 | exp (3.2153−0.008815×age) | 20≤age≤29 | exp (−9.708+0.2427× age) | 40≤age≤53 | 3.39 | age≥65 | 1.61 | age≥65 | ||||
| exp (4.28945−0.04462×age) | 30≤age≤39 | exp (6.50334−0.05751×age) | 54≤age≤57 | |||||||||
| EOC model | exp (3.96865−0.0366×age) | 40≤age≤49 | exp (11.3175−0.140513×age) | 58≤age≤69 | ||||||||
| 0.002576 | exp (1.8169+0.006435× age) | 50≤age≤59 | 4.4 | 70≤age≤79 | ||||||||
| exp (−0.2606+0.04106× age) | 60≤age≤69 | |||||||||||
| 13.0991 | 70≤age≤79 | |||||||||||
| PALB2 | 0.00064 | 0.92 | 1 | age<20 | 1 | age<30 | 1 | age<30 | 1 | 1 | age<30 | |
| 9.1 | 20≤age≤24 | 2.91 (1.40 to 6.04) | age≥30 | 7.34 (1.28 to 42.18) | age≥30 | 2.37 (1.24 to 4.50) | age≥30 | |||||
| 8.97 | 25≤age≤29 | |||||||||||
| 8.85 | 30≤age≤34 | |||||||||||
| 8.54 | 35≤age≤39 | |||||||||||
| 8.02 | 40≤age≤44 | |||||||||||
| 7.31 | 45≤age≤49 | |||||||||||
| 6.55 | 50≤age≤54 | |||||||||||
| 5.92 | 55≤age≤59 | |||||||||||
| 5.45 | 60≤age≤64 | |||||||||||
| 5.1 | 65≤age≤69 | |||||||||||
| 4.82 | 70≤age≤74 | |||||||||||
| 4.56 | 75≤age≤79 | |||||||||||
| CHEK2 | 0.00373 | 0.98 | 1 | age<20 | 1 | 1 | 1 | 1 | ||||
| exp (1.6053−0.01483×age) | age≥20 | |||||||||||
| ATM | 0.0018 | 0.94 | 2.10 (1.17 to 2.57) | 1 | 1 | 1 | 1 | |||||
| BARD1 | 0.00043 | 0.89 | 2.09 (1.35 to 3.23) | 1 | 1 | 1 | 1 | |||||
| RAD51C | 0.00035 | 0.78 | 1.97 (1.48 to 2.62) | 1 | age<30 | 1 | 1 | 1 | ||||
| exp (−1.7974+0.07631× age) | 30≤age<60 | |||||||||||
| exp (9.7592−0.1163×age) | age≥60 | |||||||||||
| RAD51D | 0.00035 | 0.86 | 1.82 (1.34 to 2.47) | 1 | age<30 | 1 | 1 | 1 | ||||
| exp (−2.88662+0.09656× age) | 30≤age<58 | |||||||||||
| exp (5.99144−0.05651×age) | age≥58 | |||||||||||
| BRIP1 | 0.00071 | 0.95 | 1 | 3.41 (2.12 to 5.54) | 1 | 1 | 1 | |||||
'Allele freq’ is the pathogenic variant allele frequency in the general population. RR is relative to the general population. The BOADICEA model includes the effects of BRCA1, BRCA2, PALB2, CHEK2, ATM, BARD1, RAD51C and RAD51D, while the EOC model includes the effects of BRCA1, BRCA2, RAD51D, RAD51C, BRIP1 and PALB2. The updated parameters are the allele frequencies for PALB2, CHEK2, ATM, RAD51C, RAD51D, BRAD1 and BRIP1,15 the SS for pathogenic variants for all genes,15 the RR for female breast cancer for ATM, BARD1, RAD51C and RAD51D,15 24 and the EOC, male breast cancer and the pancreatic cancer RRs for PALB2.17 All other parameters are as previously published.8–11 21
BOADICEA, Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm; EOC, epithelial tubo-ovarian cancer; RR, relative risk; SS, screening sensitivity.
As the polygenic component captures all residual familial aggregation not explained by the major genes, the previous models implicitly included the contributions of PVs in the new genes (ie, BARD1, RAD51C and RAD51D for BOADICEA and PALB2 for the EOC model). Therefore, to avoid double counting their contribution, it was necessary to remove their contribution from the polygenic component by adjusting the log-RR per SD of the polygenic component such that the total variance of the polygenic component and the new genes is the same as that of the polygenic component of the previous model21 (online supplemental material).
The association between PALB2 PVs and EOC was also included in the BOADICEA model, and the associations with male BC and pancreatic cancer have been included in both models.17
The impact of including PVs in the new BC susceptibility genes on risk prediction were assessed by considering the risk categories described in the National Institute for Health and Care Excellence familial BC guidelines25 for hypothetical women with different ages or family history. For lifetime risk (aged 20–80 years), three categories are defined: (1) near-population risk, for risks less than 17%, (2) moderate risk, for risks in the range of 17%–30% and (3) high risk, for risks of 30% or greater. Reclassification was considered based on questionnaire-based RFs (QRFs) (RFs other than mammographic density), mammographic density (MD, based on the BI-RADS system) and a polygenic risk score (PRS). The assumed distributions and RRs for QRFs and MD have been described in detail previously.8 11 For BC, the PRS was taken to be the Breast Cancer Association Consortium 313 variant PRS, which accounts for 20% of the overall polygenic variance.8 26 For EOC, we defined three risk categories based on lifetime risk27 28: (1) near-population risk, for risks of less than 5%, (2) moderate risk, for risks in the range of 5%–10% and (3) high risk, for risks of 10% or greater, and reclassification was considered based on RFs and PRS. For EOC, the PRS was taken as the Ovarian Cancer Association Consortium 36 variant PRS, which accounts for 5% of the overall polygenic variance.11 29
Updates to tumour pathology
Both models incorporate data on BC tumour pathology, specifically ER and TN. The distribution of pathology for affected carriers of PVs differs substantially from that in non-carriers for several genes, so that pathology data can affect the carrier probabilities and hence cancer risks.11 12 In BOADICEA and the EOC model, breast tumours are classified into five groups based on ER and TN status: ER unknown, ER-positive, ER-negative/TN unknown, ER-negative/not TN and TN. Previously, the models achieved this using age-dependent distributions in the general population and BRCA1 and BRCA2 PV carriers and an age-independent distribution for CHEK2 PV carriers.12 21 Due to the lack of data, the tumour ER distribution for carriers of PV in other genes was assumed to be the same as the general population. Here, the models have been updated to incorporate age-dependent ER and TN tumour distributions for carriers of PVs in the BC susceptibility genes PALB2, CHEK2, ATM, BARD1, RAD51C and RAD51D, using data from BRIDGES.19
Continuous risk factors
The previous versions of the models included reproductive, lifestyle, hormonal and anthropometric RFs.8 11 One limitation of these models was that the RFs needed to be coded as categorical variables. Some RFs are naturally continuous, requiring prior discretisation to a finite number of categories, resulting in some loss of information and reduction in risk discrimination. Here, the methodology was extended to allow the inclusion of continuous RFs.
The key challenge is to calculate the baseline incidences in equation s.1 (online supplemental file 1) from the population incidence and the RF distributions. The baseline incidences are calculated sequentially for each age (considered discrete) using the values at age , starting from age 0, requiring the evolution with age of the probability distribution of those who are disease free.30 For discrete factors/genes, this involves summing over all possible categories/genotypes, but for continuous factors/genes, it would involve integrating over all possible values. In principle, these integrals could be computed (either analytically or numerically). However, at each age, the number of terms in the integrand increases by a factor of 2, so by age 80, there are >1024 terms, with evaluation becomes impracticable. Alternatively, the RF could be discretised into a very large number of categories. This would give a very close approximation to the continuous distribution, but (particularly once multiple RFs are considered, as here) the large number of categories would also make the calculations impractical. Instead, we propose an alternate approach in which the continuous factors are discretised with categories adapted according to the observed RF. The approach is as follows:
1. First, discretise the range of possible RF values into a finite number ( ) of bins and calculate the probability mass and RR for each bin from the probability density and RR function for the continuous RF. This part is identical to the standard approach for discretising RFs, used in the existing models.8 For a RF, , with probability density and relative risk , the probability mass for bin with range is:
| (1) |
and the corresponding RR is
| (2) |
2. Create an additional bin based on the individual’s measured RF value that has an infinitesimal width. The RR for this bin is taken as the RR at the measured value, and it has zero mass. As this bin is infinitesimal, its overlap with the other bins is zero, so there is no double-counting.
This procedure creates a categorical RF with categories, where the individual is assigned to the category defined in step 2. This allows the exact value of the risk for the individual to be used, while the number of categories required to compute the baseline rates is fixed, limiting the computation time.
The accuracy of the approximation in the procedure relies on the assumption that the range of values within each bin have similar RRs, which should be reflected in the choice of discretisation scheme and the number of bins . These choices will depend on the shape of the distribution and the RR function.
The above procedure can be applied to any RF distribution or RR function. However, the process assumes that an individual’s position within the distribution is fixed with respect to age, although the value of the RF and RR may vary with age. Here, the method was applied to height.
Updates to population incidences
The baseline incidences in equation s.1 in online supplemental file 1 are birth year and country specific as a consequence of using birth year and country-specific population incidences in the constraining process. We refined the derivation of cohort-specific population incidences to account for variability in the incidences due to small numbers. In addition, we have updated existing incidences in the model to include more recent calendar periods and adapted the model to use cancer incidence from four new populations: the Netherlands, France, Slovenia and Estonia. Details are included in the online supplemental material.
Results
Rare moderate-risk pathogenic variants
Table 1 summarises the models’ genetic parameter estimates, including those for the new genes. The estimated cumulative age-specific BC risks for BARD1, RAD51C and RAD51D PV carriers in BOADICEA and EOC risks for PALB2 carriers, assuming the UK incidences applicable to those born in the 1980s, are shown in figure 1. The estimated average lifetime BC risks for PV carriers are 24%, 22% and 21% for BARD1, RAD51C and RAD51D PV carriers, respectively. The estimated lifetime EOC risk for PALB2 carriers is 5.0%. Based on the assumed allele frequencies, 0.22% of the population carry PV in the genes BARD1, RAD51C or RAD51D, and these explain on average 0.31% of the female BC polygenic variance (averaged over all ages and cohorts, weighted by the age-specific and cohort-specific BC incidences). Approximately 0.13% of the population carry PVs in PALB2, explaining 0.16% of the EOC polygenic variance and 2.5% of the male BC polygenic variance.
Figure 1.
Predicted risks by age for a female born in 1985 with an unknown family history based on pathogenic variant carrier status for the new genes in the model. Figure (A) shows the breast cancer risk for carriers of pathogenic variants in BARD1, RAD51C and RAD51D along with the population risk. Figure (B) shows the ovarian cancer risk for carriers of pathogenic variants in PALB2 along with the population risk. Predictions are based on UK cancer incidences.
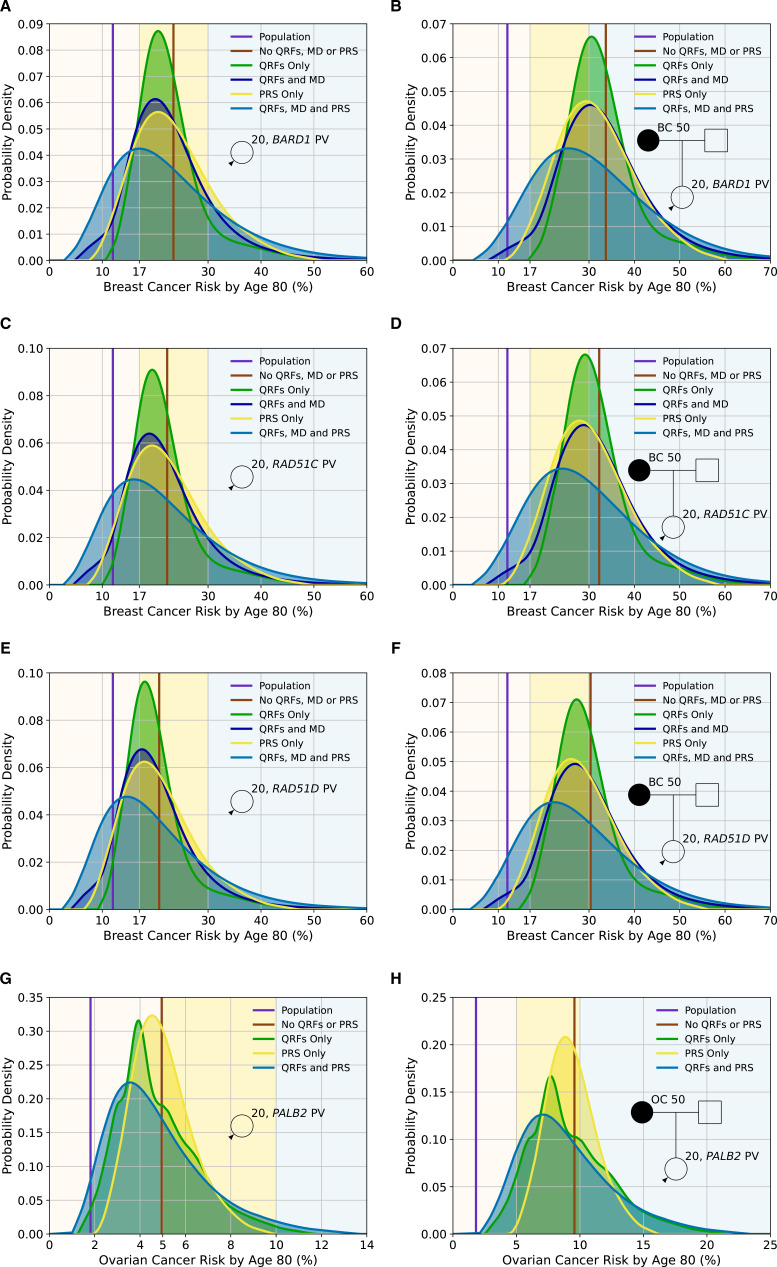
Figure 2A–F and online supplemental table S1 show the distributions of lifetime BC risks for carriers of PVs in BARD1, RAD51C and RAD51D for a female with unknown FH and a female whose mother is affected at age 50 based on PV carrier status alone and including QRF, MD and a PRS. Based solely on PV carrier status, all females with unknown FH would be classified as at moderate risk. When information on QRF, MD or PRS is known, there is significant reclassification to near-population and high-risk categories, which is greatest when all factors are used in combination. For example, based on lifetime BC risks and using the full multifactorial model incorporating QRF, MD and with unknown FH would be classified as at moderate risk. When information on QRF, MD or PRS is known, there is significant reclassification to near-population and high-risk categories, which is greatest when all factors are used in combination. For example, based on lifetime BC risks and using the full multifactorial model incorporating QRF, MD and PRS, 33.9% of BARD1 PV carriers with unknown FH would be reclassified from moderate risk to near-population risk, and 21.9% would be reclassified to high risk (online supplemental table S1). Similarly, BARD1 PV carriers with an affected first-degree relative would be considered high risk (risk of 33.7% by age 80) based on family history and PV status alone. Incorporating the other risk factors would reclassify 12% as near-population risk and 40.2% as moderate risk (online supplemental table S1).
Figure 2.
Predicted lifetime cancer risks (from age 20–80 years) for a female born in 1985 with a pathogenic variant in BARD1 (breast cancer risk), RAD51C (breast cancer risk), RAD51D (breast cancer risk) and PALB2 (ovarian cancer risk) on the basis of the different predictors of risk (pathogenic variant (PV) status, questionnaire-based risk factors (QRFs), mammographic density (MD) and polygenic risk score (PRS)). All figures show the probability density against the absolute risk. Figures (A), (C), (E) and (G) show risks for a female with unknown family history, while Figures (B), (D), (F) and (H) show risks where the individual’s mother has had cancer at age 50. The backgrounds of the graphs are shaded to indicate the risk categories. For breast cancer, these are the categories defined by the National Institute for Health and Care Excellence familial breast cancer guidelines25: (1) near-population risk shaded in pink (<17%), (2) moderate risk shaded in yellow (≥17% and<30%) and (3) high risk shaded in blue (≥30%). For ovarian cancer, the categories are: (1) near-population risk shaded in pink (<5%), (2) moderate risk shaded in yellow (≥5% and <10%) and (3) high risk shaded in blue (≥10%). Predictions were based on UK cancer incidences. The line-labelled population denotes the average population risk in the absence of knowledge of family history, PV status, RFs or a PRS. All figures assume the population distributions of QRFs and MD.
Figure 2G, H and online supplemental table S2 show the distribution of lifetime EOC risks for carriers of PVs in PALB2 for a female with unknown FH and a female whose mother is affected at age 50, as a function of the RFs and PRS. For a PALB2 carrier with unknown FH, when the RFs and PRS are considered jointly, 62.4% are classified as near-population risk, 34.9% as moderate risk and 2.7% as high risk. The corresponding proportions with an affected mother are 11.2%, 55.8% and 33%, respectively. However, even among PALB2 carriers with an affected mother, 97.5% will have risks of less than 3% by age 50 (online supplemental table S2).
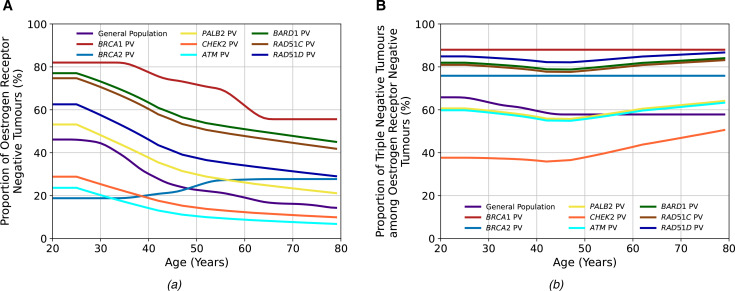
Tumour pathology
Figure 3 and online supplemental tables S3 and S4 show the age-specific distributions of ER-negative tumours and TN tumours among ER-negative tumours used in the models for PALB2, ATM, CHEK2, BARD1, RAD51C and RAD51D PV carriers based on the BRIDGES data.19 BARD1, RAD51C and RAD51D PV carriers predominantly develop ER-negative BCs, and the proportions decrease with increasing age. On the other hand, CHEK2 and ATM carriers primarily develop ER-positive BCs, and the proportion of ER-positive tumours increases with age. Among those with ER-negative tumours, most tumours are TN for PV carriers in all genes, except CHEK2 carriers, in whom the majority are ER-negative but not TN.
Figure 3.
The tumour pathology proportions in the general population and among carriers of pathogenic variants (PVs) in the breast cancer (BC) susceptibility genes included in the BOADICEA (Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm) model. Figure (A) shows the proportion of oestrogen-receptor-negative (ER−) tumours among all tumours, and figure (B) shows the proportion of triple-negative (TN) (ER−, progesterone receptor-negative and human epidermal growth factor receptor 2) tumours among ER− tumours. The general population, BRCA1 PV and BRCA2 PV values are the same as previously used in the model,12 while those for the other genes are updated using recent BRIDGES data.19
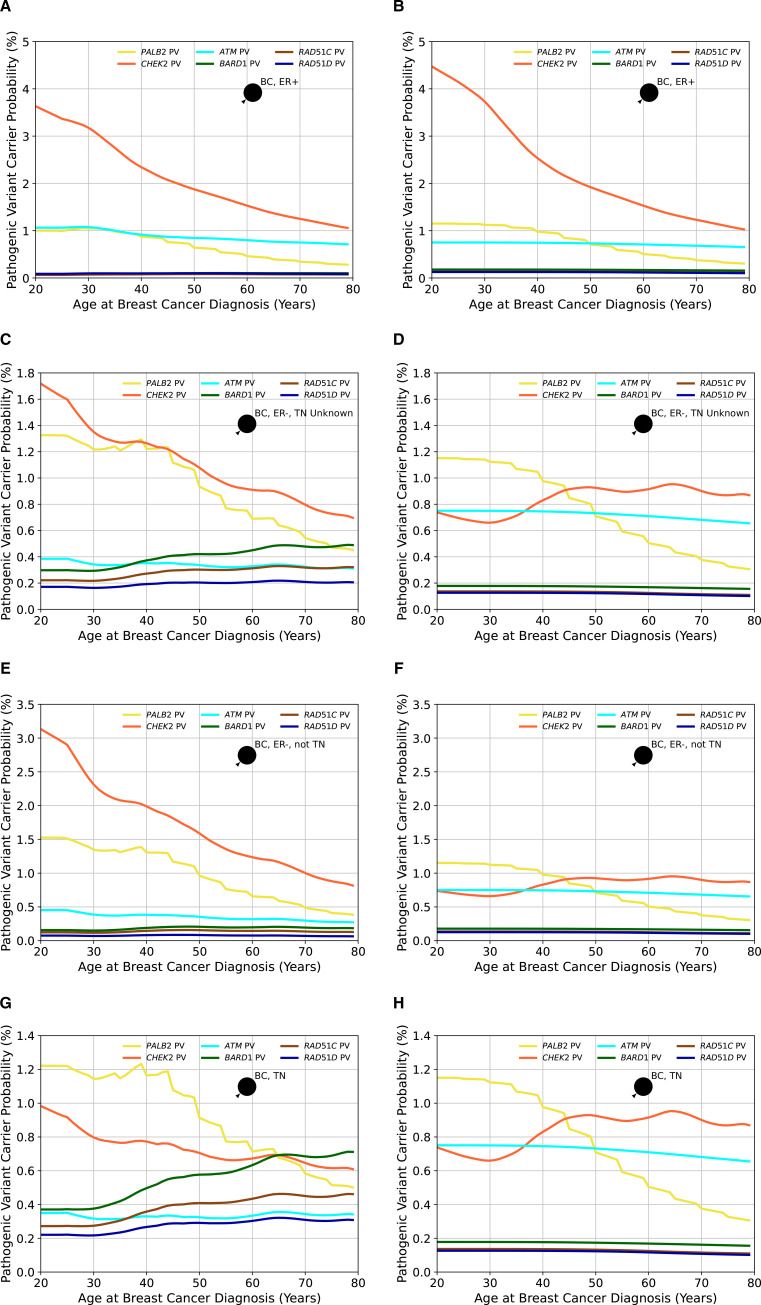
Using the updated age-specific and gene-specific ER-negative and TN tumour status distributions resulted in differences in the predicted overall and gene-specific carrier probabilities by different tumour pathology and age (figure 4). For ATM, the carrier probabilities for ER-negative tumours are reduced relative to previous estimates, reflecting the stronger association with ER-positive disease. Carrier probabilities for CHEK2 now show a decline with age for ER-negative tumours (previously, this was only predicted for ER-positive disease). The carrier probabilities for PALB2 remain similar to previous estimates. For the new genes BARD1, RAD51C and RAD51D, the carrier probabilities are, as expected, higher for ER-negative and TN diseases, but there is little variation by age.
Figure 4.
The probabilities of carrying a pathogenic variant estimated by BOADICEA (Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm) model in the genes PALB2, CHEK2, ATM, BARD1, RAD51C and RAD51D for an affected female born in 1985 as a function of her age at diagnosis based on different tumour pathology. Figures (A), (C), (E) and (G) show the probabilities based on the updated proportions (current model), while figures (B), (D), (F) and (H) are based on the previously assumed tumour pathology proportions (previous model version) and where proportions for BARD1, RAD51C and RAD51D, which were not in the previous model, are assumed to be the same as in the general population. In figures (A) and (B), the woman has had an oestrogen receptor-positive (ER+) tumour; in figures (C) and (D), the female has had an oestrogen receptor-negative (ER−) tumour, but the triple-negative (TN) status is unknown; in figures (E) and (F), the woman has had an ER− tumour that is not TN and in figures (G) and (H), the woman has had a TN tumour. Predictions are based on UK cancer incidences. BC, breast cancer.
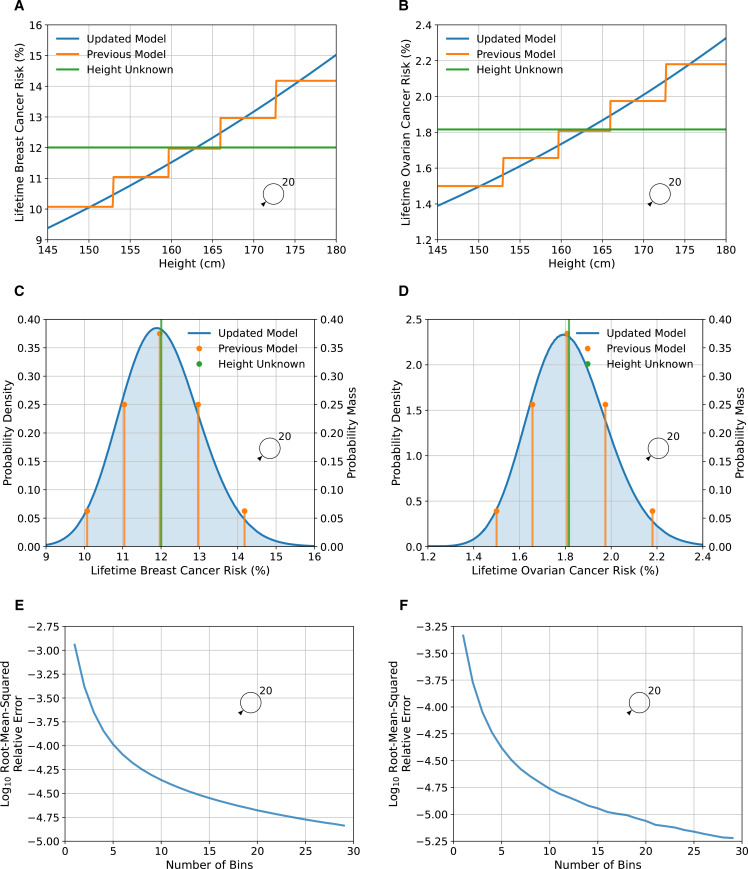
Continuous risk factors
As previously, adult female height was assumed to be normally distributed with mean 162.81 cm and SD 6.452 cm, and be associated with a log-RR per SD, for both BC and EOC, of 0.10130.8 11 We therefore discretised the normal distribution such that the probability masses of the bins were given by a binomial distribution , giving sufficient discretisation to adequately capture the tails of the distribution. We examined the relative discretisation error of the predicted lifetime risk as a function of the number of bins (figure 5E, F) and chose , as the lowest number of bins such that the root-mean-square relative error was less than . Compared with the discrete (five-level) RF, the variance of the RR of both BC and EOC increased from 0.002 to 0.010 when height was included as a continuous RF. The effects on predicted lifetime risks are shown in figure 5 A–D). Under the continuous implementation here, the lifetime BC risk varied from 9.7% for the first percentile to 14.6% for the 99th percentile, whereas under the previous discrete distribution, the risks range from 10.1% to 14.2%.
Figure 5.
Predicted lifetime breast and ovarian cancer risks as a function of height for a female born in 1985 with unknown family history, comparing the updated model, where height is treated as continuous, to the previous model, where height was treated as categorical. Figures (A), (C) and (E) show breast cancer, while figures (B), (D) and (F) show ovarian cancer risks. Figures (A) and (B) show the predicted risk as a function of height, while figures (C) and (D) show the probability density/mass of risk as a function of height. Predictions are based on UK cancer incidences. Figures (E) and (F) show the log (base 10) of the root-mean-squared relative discretisation error as a function of the number of bins. The error was taken to be the absolute difference between the value and the asymptotic extrapolation of the measurements as a function of the number of bins. The average is taken over 100 heights that are spaced 1% apart, from 0.5% to 99.5%.
Discussion
This work has extended the multifactorial BOADICEA BC and EOC risk prediction models (BOADICEA v6 and the Ovarian Cancer Model v2), employing a synthetic approach.23 The explicit effects of PVs in RAD51C, RAD51D, BARD1 and PALB2, which have now been established as BC and/or EOC susceptibility genes15–17 and are commonly included on cancer gene panels, are now included in the models. The models have also been extended to accommodate continuous RFs, and parameterisation of tumour pathology and cancer incidence have been updated with more recent data. These represent the most comprehensive models for BC and EOC and will allow more complete BC and EOC risk assessment of those undergoing gene-panel testing. In a separate study, the BOADICEA v6 breast cancer model presented here has been validated in an independent prospective study of 66 415 women attending mammographic screening in Sweden. The full model, including RFs, mammographic density, PRS and PVs in BRCA1, BRCA2, PALB2, CHEK2, ATM, BARD1, RAD51C and RAD51D was well calibrated overall (calibration slope 0.97 (95% CI: 0.95 to 0.99)) and in deciles of predicted 5-year risks and had a C-index of 0.71 (95% CI: 0.68 to 0.74) for discriminating between affected and unaffected women.31
By explicitly modelling the effects of PVs in the new cancer susceptibility genes, the models provide personalised cancer risks of PV carriers when combined with QRFs, MD and PRS. Although the numbers affected by these changes will be small at population level, for individuals with RAD51C, RAD51D and BARD1 PVs and their families, the updated risks will be clinically important. RAD51C, RAD51D and BARD1 (like ATM and CHEK2) would be classified as ‘moderate risk’ BC genes based on the average risks.15 However, according to the BOADICEA predictions, over half (56%–59%) of carriers of PVs in these genes in the population would be reclassified from being in the moderate BC risk category to either being near-population risk (34%–44%) or high risk (15%–22%), if data on the other RFs were incorporated (online supplemental table S1). Such changes may have important implications for discussions around earlier or more frequent screening or on risk-reduction options for these women. Similarly, based on the multifactorial EOC model ~38% of PALB2 PV carriers will have lifetime EOC risks of >5% (online supplemental table S2), which may influence recommendations on the timing of risk-reducing surgery.
As previously, the models assume that the effects of the PVs in the new genes interact multiplicatively with the PRS and the RFs. No studies have yet assessed the joint effects of PVs in these genes and the PRS or RFs. Previous results for CHEK2 and ATM suggest that the multiplicative model holds true for earlier versions of the PRS.32–34 Unlike CHEK2 and ATM, however, the new genes predispose more strongly to ER-negative disease, and the combined effect may depart from the multiplicative assumption. Demonstrating this explicitly for the new genes will be challenging given the rarity of the mutations. The multiplicative model has also been shown to be reasonable for the combined effects of PRS and RFs,35 but there is as yet no large-scale evaluation of the combined effects of PVs and RFs. However, recent prospective validation studies of the current and previous versions of the models suggest that, overall, the models fit well.11 31 Should deviations from the multiplicative model between these PVs and RFs emerge, the model can be updated to take them into account.
Both the BC and EOC models incorporate PVs’ effects using the estimated population allele frequencies and RRs. These are combined with reference population incidences to calculate absolute risks while constraining the overall incidences over the RFs included in the model. Our implementation used RR and allele frequency estimates from the largest available studies on those of European ancestry.15 These were assumed to be constant across all countries. Available data are currently too sparse to obtain country-specific estimates. Although there is no evidence that RRs vary among populations, the allele frequencies are likely to vary to some extent.15 This is most apparent for CHEK2, where the founder c.1100delC variant (p.Thr367Metfs*15) is common in northwest Europe with carrier frequencies between 0.3% and 1.2%36 and explains the majority of carriers but is rare or absent in other populations. If population-specific variant frequencies can be generated, the model can be easily updated to accommodate these. Nevertheless, by allowing population incidences to vary by country, the predicted absolute risks given by the models are country-specific.
The updated age-specific distributions of tumour ER and TN status for six of the BC susceptibility genes in the model (PALB2, CHEK2, ATM, BARD1, RAD51C and RAD51D) should allow better differentiation between PVs that may be present in a family and provide age-specific and gene-specific mutation carrier probabilities consistent with the prevalence of PVs observed in Mavaddat et al.19 We note, however, that estimates are more uncertain at very young and very old ages, where the data are sparse, and more extensive validation may be required in these age-groups. Since PV carrier probabilities are used internally in the models, these will also impact the predicted absolute risks for all unaffected individuals if information on tumour characteristics is available for affected relatives whether or not they carry a PV.
We have developed a novel methodological approach for including continuous RFs into the models. We demonstrated this by including height in both the BC and EOC models, allowing for more nuanced predictions and improving the risk discrimination. While the resulting discrimination based on height alone is modest, the framework will allow other more predictive RFs to be included in the model if accurate risk estimates become available. The most important example is MD: continuous measures of MD, available through tools such as STRATUS, CUMULUS and Volpara,37–39 have been shown to have stronger associations with BC risk than the categorical BI-RADS system. Other examples include BMI and ages at menarche and menopause. Further, the method could be applied to the joint distribution of several continuous risk factors, where the integrals in equations (1) and (2) become multidimensional integrals.
We have further refined the method for creating cohort incidences from calendar period incidences (online supplemental material). The approach provides incidences that are less sensitive to year-on-year fluctuations by averaging over all years in the birth cohort. This method is particularly useful for cancers with low incidences, such as EOC and male BC, where the population size is small, and there is no prior averaging over calendar years. The refinement will have little effect on incidences from larger countries.
Our models have certain limitations. No single dataset containing all the required information was available to construct the multifactorial models, so the models were extended via a synthetic approach. The new model parameters were taken from extensive, well-designed published studies together with existing parameters from model fitting.9 10 We and others have used this approach for developing previous versions of the models,8 11 12 21 40 41 which have been shown to provide clinically valid predictions.42 43 31 As is the case for the previous versions, the updates presented here are primarily based on studies of those of European ancestry in developed countries. There is little evidence that the RRs associated with PVs differ by ancestry. The PV frequencies are also broadly similar across populations, except for specific founder mutations and CHEK2 PVs, which have a much higher frequency in European than non-European populations. However, other parameters in the model, including RF and PRS distributions, will differ by population, and the model will need to be adapted for use in non-European ancestry populations and developing countries. The synthetic approach presented here allows the model to be easily customised to other populations as better estimates become available.44 45 Although we used the associations between PVs and tumour ER and TN status, the models do not currently consider the associations with intrinsic BC subtypes based on combinations of ER, progesterone receptor, HER2 and/or grade.19 The methodology described here could be used to further extend the models to consider these BC subtypes. Finally, the models make the simplifying assumption that PVs in the assumed BC and EOC susceptibility genes are associated with similar risks to those for truncating variants. These would include missense variants which have similar risks to truncating variants. However, there is evidence that missense variants in CHEK2 and ATM are associated with BC risk, which may be different from the risks for truncating variants.46 The models would not be applicable to carriers of such variants.
The new model features have been built on the established and well-validated BOADICEA and EOC models.8 11 42 The updated models will allow for more personalised risk assessment and can help guide decisions on screening, prevention, risk factor modification or other risk-reducing options. The models presented are now available for use by healthcare professionals through the user-friendly CanRisk webtool (www.canrisk.org, CanRisk V.2).
Footnotes
Contributors: Conceptualisation: ACA, PPDP, DFE; Methodology: AL, ACA, DFE, PPDP; Software: AL, AC, TC, LF, SA, FMW, MT, JR, JU-S, ACA; Investigation: AL, ACA, PPDP, DFE; Formal analysis: AL, NM, LF; Funding acquisition: ACA, MKS, PD, JS; Resources: PPDP, DFE, ACA, VZ, HJ, EM-F, ADP, MR, TMM; Supervision: ACA; Visualisation: AL; Writing–original draft: AL, DFE, ACA; Writing–review and editing: all authors.
Funding: This work has been supported by grants from Cancer Research UK (C12292/A20861 and PPRPGM-Nov20\100002); the European Union’s Horizon 2020 research and innovation programme under grant agreement numbers 633784 (B-CAST) and 634935 (BRIDGES); the PERSPECTIVE I&I project, which the Government of Canada funds through Genome Canada (#13529) and the Canadian Institutes of Health Research (#155865), the Ministère de l’Économie et de l’Innovation du Québec through Genome Québec, the Quebec Breast Cancer Foundation, the CHU de Quebec Foundation and the Ontario Research Fund. MT is supported by the NIHR Cambridge Biomedical Research Centre (BRC-1215-20014).
Competing interests: The authors ACA, DFE, AL, AC and TC are named inventors of BOADICEA v5 commercialised by Cambridge Enterprise. AL is now employed by Illumina.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study. The models are implemented in the CanRisk tool, which is freely available at www.canrisk.org.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Not applicable.
References
- 1. Cancer Research UK . Ovarian Cancer Statistics [Ovarian cancer statistics for the UK]. Available: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/ovarian-cancer [Accessed 21 June 2021].
- 2. Cancer Research UK . Breast cancer statistics [Breast cancer statistics for the UK]. Available: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer [Accessed 21 June 2021].
- 3. The UK Government . Breast screening: programme overview. Available: https://www.gov.uk/guidance/breast-screening-programme-overview [Accessed 15 July 2021].
- 4. Pashayan N, Antoniou AC, Ivanus U, Esserman LJ, Easton DF, French D, Sroczynski G, Hall P, Cuzick J, Evans DG, Simard J, Garcia-Closas M, Schmutzler R, Wegwarth O, Pharoah P, Moorthie S, De Montgolfier S, Baron C, Herceg Z, Turnbull C, Balleyguier C, Rossi PG, Wesseling J, Ritchie D, Tischkowitz M, Broeders M, Reisel D, Metspalu A, Callender T, de Koning H, Devilee P, Delaloge S, Schmidt MK, Widschwendter M. Personalized early detection and prevention of breast cancer: ENVISION consensus statement. Nat Rev Clin Oncol 2020;17:687–705. 10.1038/s41571-020-0388-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Maas P, Barrdahl M, Joshi AD, Auer PL, Gaudet MM, Milne RL, Schumacher FR, Anderson WF, Check D, Chattopadhyay S, Baglietto L, Berg CD, Chanock SJ, Cox DG, Figueroa JD, Gail MH, Graubard BI, Haiman CA, Hankinson SE, Hoover RN, Isaacs C, Kolonel LN, Le Marchand L, Lee I-M, Lindström S, Overvad K, Romieu I, Sanchez M-J, Southey MC, Stram DO, Tumino R, VanderWeele TJ, Willett WC, Zhang S, Buring JE, Canzian F, Gapstur SM, Henderson BE, Hunter DJ, Giles GG, Prentice RL, Ziegler RG, Kraft P, Garcia-Closas M, Chatterjee N. Breast cancer risk from modifiable and Nonmodifiable risk factors among white women in the United States. JAMA Oncol 2016;2:1295–302. 10.1001/jamaoncol.2016.1025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pearce CL, Rossing MA, Lee AW, Ness RB, Webb PM, Chenevix-Trench G, Jordan SM, Stram DA, Chang-Claude J, Hein R, Nickels S, Lurie G, Thompson PJ, Carney ME, Goodman MT, Moysich K, Hogdall E, Jensen A, Goode EL, Fridley BL, Cunningham JM, Vierkant RA, Weber RP, Ziogas A, Anton-Culver H, Gayther SA, Gentry-Maharaj A, Menon U, Ramus SJ, Brinton L, Wentzensen N, Lissowska J, Garcia-Closas M, Massuger LFAG, Kiemeney LALM, Van Altena AM, Aben KKH, Berchuck A, Doherty JA, Iversen E, McGuire V, Moorman PG, Pharoah P, Pike MC, Risch H, Sieh W, Stram DO, Terry KL, Whittemore A, Wu AH, Schildkraut JM, Kjaer SK. Combined and interactive effects of environmental and GWAS-identified risk factors in ovarian cancer. Cancer Epidemiol Biomarkers Prev 2013;22:880–90. 10.1158/1055-9965.EPI-12-1030-T [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pearce CL, Stram DO, Ness RB, Stram DA, Roman LD, Templeman C, Lee AW, Menon U, Fasching PA, McAlpine JN, Doherty JA, Modugno F, Schildkraut JM, Rossing MA, Huntsman DG, Wu AH, Berchuck A, Pike MC, Pharoah PDP. Population distribution of lifetime risk of ovarian cancer in the United States. Cancer Epidemiol Biomarkers Prev 2015;24:671–6. 10.1158/1055-9965.EPI-14-1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee A, Mavaddat N, Wilcox AN, Cunningham AP, Carver T, Hartley S, Babb de Villiers C, Izquierdo A, Simard J, Schmidt MK, Walter FM, Chatterjee N, Garcia-Closas M, Tischkowitz M, Pharoah P, Easton DF, Antoniou AC. Boadicea: a comprehensive breast cancer risk prediction model incorporating genetic and nongenetic risk factors. Genet Med 2019;21:1708–18. 10.1038/s41436-018-0406-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Antoniou AC, Cunningham AP, Peto J, Evans DG, Lalloo F, Narod SA, Risch HA, Eyfjord JE, Hopper JL, Southey MC, Olsson H, Johannsson O, Borg A, Pasini B, Passini B, Radice P, Manoukian S, Eccles DM, Tang N, Olah E, Anton-Culver H, Warner E, Lubinski J, Gronwald J, Gorski B, Tryggvadottir L, Syrjakoski K, Kallioniemi O-P, Eerola H, Nevanlinna H, Pharoah PDP, Easton DF. The BOADICEA model of genetic susceptibility to breast and ovarian cancers: updates and extensions. Br J Cancer 2008;98:1457–66. 10.1038/sj.bjc.6604305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jervis S, Song H, Lee A, Dicks E, Harrington P, Baynes C, Manchanda R, Easton DF, Jacobs I, Pharoah PPD, Antoniou AC. A risk prediction algorithm for ovarian cancer incorporating BRCA1, BRCA2, common alleles and other familial effects. J Med Genet 2015;52:465–75. 10.1136/jmedgenet-2015-103077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lee A, Yang X, Tyrer J, Gentry-Maharaj A, Ryan A, Mavaddat N, Cunningham AP, Carver T, Archer S, Leslie G, Kalsi J, Gaba F, Manchanda R, Gayther S, Ramus SJ, Walter FM, Tischkowitz M, Jacobs I, Menon U, Easton DF, Pharoah P, Antoniou AC. Comprehensive epithelial tubo-ovarian cancer risk prediction model incorporating genetic and epidemiological risk factors. J Med Genet 2022;59:632–43. 10.1136/jmedgenet-2021-107904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lee AJ, Cunningham AP, Kuchenbaecker KB, Mavaddat N, Easton DF, Antoniou AC, Consortium of Investigators of Modifiers of BRCA1/2, Breast Cancer Association Consortium . Boadicea breast cancer risk prediction model: updates to cancer incidences, tumour pathology and web interface. Br J Cancer 2014;110:535–45. 10.1038/bjc.2013.730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fischer C, Kuchenbäcker K, Engel C, Zachariae S, Rhiem K, Meindl A, Rahner N, Dikow N, Plendl H, Debatin I, Grimm T, Gadzicki D, Flöttmann R, Horvath J, Schröck E, Stock F, Schäfer D, Schwaab I, Kartsonaki C, Mavaddat N, Schlegelberger B, Antoniou AC, Schmutzler R, German Consortium for Hereditary Breast and Ovarian Cancer . Evaluating the performance of the breast cancer genetic risk models BOADICEA, ibis, BRCAPRO and Claus for predicting BRCA1/2 mutation carrier probabilities: a study based on 7352 families from the German hereditary breast and ovarian cancer Consortium. J Med Genet 2013;50:360–7. 10.1136/jmedgenet-2012-101415 [DOI] [PubMed] [Google Scholar]
- 14. Carver T, Hartley S, Lee A, Cunningham AP, Archer S, Babb de Villiers C, Roberts J, Ruston R, Walter FM, Tischkowitz M, Easton DF, Antoniou AC. CanRisk Tool—A web interface for the prediction of breast and ovarian cancer risk and the likelihood of carrying genetic pathogenic variants. Cancer Epidemiol Biomarkers Prev 2021;30:469–73. 10.1158/1055-9965.EPI-20-1319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Breast Cancer Association Consortium, Dorling L, Carvalho S, Allen J, González-Neira A, Luccarini C, Wahlström C, Pooley KA, Parsons MT, Fortuno C, Wang Q, Bolla MK, Dennis J, Keeman R, Alonso MR, Álvarez N, Herraez B, Fernandez V, Núñez-Torres R, Osorio A, Valcich J, Li M, Törngren T, Harrington PA, Baynes C, Conroy DM, Decker B, Fachal L, Mavaddat N, Ahearn T, Aittomäki K, Antonenkova NN, Arnold N, Arveux P, Ausems MGEM, Auvinen P, Becher H, Beckmann MW, Behrens S, Bermisheva M, Białkowska K, Blomqvist C, Bogdanova NV, Bogdanova-Markov N, Bojesen SE, Bonanni B, Børresen-Dale A-L, Brauch H, Bremer M, Briceno I, Brüning T, Burwinkel B, Cameron DA, Camp NJ, Campbell A, Carracedo A, Castelao JE, Cessna MH, Chanock SJ, Christiansen H, Collée JM, Cordina-Duverger E, Cornelissen S, Czene K, Dörk T, Ekici AB, Engel C, Eriksson M, Fasching PA, Figueroa J, Flyger H, Försti A, Gabrielson M, Gago-Dominguez M, Georgoulias V, Gil F, Giles GG, Glendon G, Garcia EBG, Alnæs GIG, Guénel P, Hadjisavvas A, Haeberle L, Hahnen E, Hall P, Hamann U, Harkness EF, Hartikainen JM, Hartman M, He W, Heemskerk-Gerritsen BAM, Hillemanns P, Hogervorst FBL, Hollestelle A, Ho WK, Hooning MJ, Howell A, Humphreys K, Idris F, Jakubowska A, Jung A, Kapoor PM, Kerin MJ, Khusnutdinova E, Kim S-W, Ko Y-D, Kosma V-M, Kristensen VN, Kyriacou K, Lakeman IMM, Lee JW, Lee MH, Li J, Lindblom A, Lo W-Y, Loizidou MA, Lophatananon A, Lubiński J, MacInnis RJ, Madsen MJ, Mannermaa A, Manoochehri M, Manoukian S, Margolin S, Martinez ME, Maurer T, Mavroudis D, McLean C, Meindl A, Mensenkamp AR, Michailidou K, Miller N, Mohd Taib NA, Muir K, Mulligan AM, Nevanlinna H, Newman WG, Nordestgaard BG, Ng P-S, Oosterwijk JC, Park SK, Park-Simon T-W, Perez JIA, Peterlongo P, Porteous DJ, Prajzendanc K, Prokofyeva D, Radice P, Rashid MU, Rhenius V, Rookus MA, Rüdiger T, Saloustros E, Sawyer EJ, Schmutzler RK, Schneeweiss A, Schürmann P, Shah M, Sohn C, Southey MC, Surowy H, Suvanto M, Thanasitthichai S, Tomlinson I, Torres D, Truong T, Tzardi M, Valova Y, van Asperen CJ, Van Dam RM, van den Ouweland AMW, van der Kolk LE, van Veen EM, Wendt C, Williams JA, Yang XR, Yoon S-Y, Zamora MP, Evans DG, de la Hoya M, Simard J, Antoniou AC, Borg Åke, Andrulis IL, Chang-Claude J, García-Closas M, Chenevix-Trench G, Milne RL, Pharoah PDP, Schmidt MK, Spurdle AB, Vreeswijk MPG, Benitez J, Dunning AM, Kvist A, Teo SH, Devilee P, Easton DF. Breast Cancer Risk Genes - Association Analysis in More than 113,000 Women. N Engl J Med 2021;384:428–39. 10.1056/NEJMoa1913948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hu C, Hart SN, Gnanaolivu R, Huang H, Lee KY, Na J, Gao C, Lilyquist J, Yadav S, Boddicker NJ, Samara R, Klebba J, Ambrosone CB, Anton-Culver H, Auer P, Bandera EV, Bernstein L, Bertrand KA, Burnside ES, Carter BD, Eliassen H, Gapstur SM, Gaudet M, Haiman C, Hodge JM, Hunter DJ, Jacobs EJ, John EM, Kooperberg C, Kurian AW, Le Marchand L, Lindstroem S, Lindstrom T, Ma H, Neuhausen S, Newcomb PA, O’Brien KM, Olson JE, Ong IM, Pal T, Palmer JR, Patel AV, Reid S, Rosenberg L, Sandler DP, Scott C, Tamimi R, Taylor JA, Trentham-Dietz A, Vachon CM, Weinberg C, Yao S, Ziogas A, Weitzel JN, Goldgar DE, Domchek SM, Nathanson KL, Kraft P, Polley EC, Couch FJ. A population-based study of genes previously implicated in breast cancer. N Engl J Med Overseas Ed 2021;384:440–51. 10.1056/NEJMoa2005936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yang X, Leslie G, Doroszuk A, Schneider S, Allen J, Decker B, Dunning AM, Redman J, Scarth J, Plaskocinska I, Luccarini C, Shah M, Pooley K, Dorling L, Lee A, Adank MA, Adlard J, Aittomäki K, Andrulis IL, Ang P, Barwell J, Bernstein JL, Bobolis K, Borg Åke, Blomqvist C, Claes KBM, Concannon P, Cuggia A, Culver JO, Damiola F, de Pauw A, Diez O, Dolinsky JS, Domchek SM, Engel C, Evans DG, Fostira F, Garber J, Golmard L, Goode EL, Gruber SB, Hahnen E, Hake C, Heikkinen T, Hurley JE, Janavicius R, Kleibl Z, Kleiblova P, Konstantopoulou I, Kvist A, Laduca H, Lee ASG, Lesueur F, Maher ER, Mannermaa A, Manoukian S, McFarland R, McKinnon W, Meindl A, Metcalfe K, Mohd Taib NA, Moilanen J, Nathanson KL, Neuhausen S, Ng PS, Nguyen-Dumont T, Nielsen SM, Obermair F, Offit K, Olopade OI, Ottini L, Penkert J, Pylkäs K, Radice P, Ramus SJ, Rudaitis V, Side L, Silva-Smith R, Silvestri V, Skytte A-B, Slavin T, Soukupova J, Tondini C, Trainer AH, Unzeitig G, Usha L, van Overeem Hansen T, Whitworth J, Wood M, Yip CH, Yoon S-Y, Yussuf A, Zogopoulos G, Goldgar D, Hopper JL, Chenevix-Trench G, Pharoah P, George SHL, Balmaña J, Houdayer C, James P, El-Haffaf Z, Ehrencrona H, Janatova M, Peterlongo P, Nevanlinna H, Schmutzler R, Teo S-H, Robson M, Pal T, Couch F, Weitzel JN, Elliott A, Southey M, Winqvist R, Easton DF, Foulkes WD, Antoniou AC, Tischkowitz M. Cancer Risks Associated With Germline PALB2 Pathogenic Variants: An International Study of 524 Families. JCO 2020;38:674–85. 10.1200/JCO.19.01907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Song H, Dicks EM, Tyrer J, Intermaggio M, Chenevix-Trench G, Bowtell DD, Traficante N, Group A, Brenton J, Goranova T, Hosking K, Piskorz A, van Oudenhove E, Doherty J, Harris HR, Rossing MA, Duerst M, Dork T, Bogdanova NV, Modugno F, Moysich K, Odunsi K, Ness R, Karlan BY, Lester J, Jensen A, Krüger Kjaer S, Høgdall E, Campbell IG, Lázaro C, Pujara MA, Cunningham J, Vierkant R, Winham SJ, Hildebrandt M, Huff C, Li D, Wu X, Yu Y, Permuth JB, Levine DA, Schildkraut JM, Riggan MJ, Berchuck A, Webb PM, Group OS, Cybulski C, Gronwald J, Jakubowska A, Lubinski J, Alsop J, Harrington P, Chan I, Menon U, Pearce CL, Wu AH, de Fazio A, Kennedy CJ, Goode E, Ramus S, Gayther S, Pharoah P. Population-based targeted sequencing of 54 candidate genes identifies PALB2 as a susceptibility gene for high-grade serous ovarian cancer. J Med Genet 2021;58:305–13. 10.1136/jmedgenet-2019-106739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mavaddat N, Dorling L, Carvalho S, Allen J, González-Neira A, Keeman R, Bolla MK, Dennis J, Wang Q, Ahearn TU, Andrulis IL, Beckmann MW, Behrens S, Benitez J, Bermisheva M, Blomqvist C, Bogdanova NV, Bojesen SE, Briceno I, Brüning T, Camp NJ, Campbell A, Castelao JE, Chang-Claude J, Chanock SJ, Chenevix-Trench G, Christiansen H, Czene K, Dörk T, Eriksson M, Evans DG, Fasching PA, Figueroa JD, Flyger H, Gabrielson M, Gago-Dominguez M, Geisler J, Giles GG, Guénel P, Hadjisavvas A, Hahnen E, Hall P, Hamann U, Hartikainen JM, Hartman M, Hoppe R, Howell A, Jakubowska A, Jung A, Khusnutdinova EK, Kristensen VN, Li J, Lim SH, Lindblom A, Loizidou MA, Lophatananon A, Lubinski J, Madsen MJ, Mannermaa A, Manoochehri M, Margolin S, Mavroudis D, Milne RL, Mohd Taib NA, Morra A, Muir K, Obi N, Osorio A, Park-Simon T-W, Peterlongo P, Radice P, Saloustros E, Sawyer EJ, Schmutzler RK, Shah M, Sim X, Southey MC, Thorne H, Tomlinson I, Torres D, Truong T, Yip CH, Spurdle AB, Vreeswijk MPG, Dunning AM, García-Closas M, Pharoah PDP, Kvist A, Muranen TA, Nevanlinna H, Teo SH, Devilee P, Schmidt MK, Easton DF, Breast Cancer Association Consortium . Pathology of tumors associated with pathogenic germline variants in 9 breast cancer susceptibility genes. JAMA Oncol 2022;8:e216744. 10.1001/jamaoncol.2021.6744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mavaddat N, Rebbeck TR, Lakhani SR, Easton DF, Antoniou AC. Incorporating tumour pathology information into breast cancer risk prediction algorithms. Breast Cancer Res 2010;12:R28. 10.1186/bcr2576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lee AJ, Cunningham AP, Tischkowitz M, Simard J, Pharoah PD, Easton DF, Antoniou AC. Incorporating truncating variants in PALB2, CHEK2, and ATM into the BOADICEA breast cancer risk model. Genet Med 2016;18:1190–8. 10.1038/gim.2016.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Antoniou AC, Pharoah PPD, Smith P, Easton DF. The BOADICEA model of genetic susceptibility to breast and ovarian cancer. Br J Cancer 2004;91:1580–90. 10.1038/sj.bjc.6602175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Garcia-Closas M, Gunsoy NB, Chatterjee N . Combined associations of genetic and environmental risk factors: implications for prevention of breast cancer 2014;106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yang X, Song H, Leslie G, Engel C, Hahnen E, Auber B, Horváth J, Kast K, Niederacher D, Turnbull C, Houlston R, Hanson H, Loveday C, Dolinsky JS, LaDuca H, Ramus SJ, Menon U, Rosenthal AN, Jacobs I, Gayther SA, Dicks E, Nevanlinna H, Aittomäki K, Pelttari LM, Ehrencrona H, Borg Åke, Kvist A, Rivera B, Hansen TVO, Djursby M, Lee A, Dennis J, Bowtell DD, Traficante N, Diez O, Balmaña J, Gruber SB, Chenevix-Trench G, Investigators kConFab, Jensen A, Kjær SK, Høgdall E, Castéra L, Garber J, Janavicius R, Osorio A, Golmard L, Vega A, Couch FJ, Robson M, Gronwald J, Domchek SM, Culver JO, de la Hoya M, Easton DF, Foulkes WD, Tischkowitz M, Meindl A, Schmutzler RK, Pharoah PDP, Antoniou AC. Ovarian and breast cancer risks associated with pathogenic variants in RAD51C and RAD51D. J Natl Cancer Inst 2020;112:1242–50. 10.1093/jnci/djaa030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. National Institute for Health and Care Excellence . Familial breast cancer: classification and care of people at risk of familial breast cancer and management of breast cancer and related risks in people with a family history of breast cancer (CG164), 2013. Available: http://www.nice.org.uk/CG164 [PubMed]
- 26. Mavaddat N, Michailidou K, Dennis J, Lush M, Fachal L, Lee A, Tyrer JP, Chen T-H, Wang Q, Bolla MK, Yang X, Adank MA, Ahearn T, Aittomäki K, Allen J, Andrulis IL, Anton-Culver H, Antonenkova NN, Arndt V, Aronson KJ, Auer PL, Auvinen P, Barrdahl M, Beane Freeman LE, Beckmann MW, Behrens S, Benitez J, Bermisheva M, Bernstein L, Blomqvist C, Bogdanova NV, Bojesen SE, Bonanni B, Børresen-Dale A-L, Brauch H, Bremer M, Brenner H, Brentnall A, Brock IW, Brooks-Wilson A, Brucker SY, Brüning T, Burwinkel B, Campa D, Carter BD, Castelao JE, Chanock SJ, Chlebowski R, Christiansen H, Clarke CL, Collée JM, Cordina-Duverger E, Cornelissen S, Couch FJ, Cox A, Cross SS, Czene K, Daly MB, Devilee P, Dörk T, dos-Santos-Silva I, Dumont M, Durcan L, Dwek M, Eccles DM, Ekici AB, Eliassen AH, Ellberg C, Engel C, Eriksson M, Evans DG, Fasching PA, Figueroa J, Fletcher O, Flyger H, Försti A, Fritschi L, Gabrielson M, Gago-Dominguez M, Gapstur SM, García-Sáenz JA, Gaudet MM, Georgoulias V, Giles GG, Gilyazova IR, Glendon G, Goldberg MS, Goldgar DE, González-Neira A, Grenaker Alnæs GI, Grip M, Gronwald J, Grundy A, Guénel P, Haeberle L, Hahnen E, Haiman CA, Håkansson N, Hamann U, Hankinson SE, Harkness EF, Hart SN, He W, Hein A, Heyworth J, Hillemanns P, Hollestelle A, Hooning MJ, Hoover RN, Hopper JL, Howell A, Huang G, Humphreys K, Hunter DJ, Jakimovska M, Jakubowska A, Janni W, John EM, Johnson N, Jones ME, Jukkola-Vuorinen A, Jung A, Kaaks R, Kaczmarek K, Kataja V, Keeman R, Kerin MJ, Khusnutdinova E, Kiiski JI, Knight JA, Ko Y-D, Kosma V-M, Koutros S, Kristensen VN, Krüger U, Kühl T, Lambrechts D, Le Marchand L, Lee E, Lejbkowicz F, Lilyquist J, Lindblom A, Lindström S, Lissowska J, Lo W-Y, Loibl S, Long J, Lubiński J, Lux MP, MacInnis RJ, Maishman T, Makalic E, Maleva Kostovska I, Mannermaa A, Manoukian S, Margolin S, Martens JWM, Martinez ME, Mavroudis D, McLean C, Meindl A, Menon U, Middha P, Miller N, Moreno F, Mulligan AM, Mulot C, Muñoz-Garzon VM, Neuhausen SL, Nevanlinna H, Neven P, Newman WG, Nielsen SF, Nordestgaard BG, Norman A, Offit K, Olson JE, Olsson H, Orr N, Pankratz VS, Park-Simon T-W, Perez JIA, Pérez-Barrios C, Peterlongo P, Peto J, Pinchev M, Plaseska-Karanfilska D, Polley EC, Prentice R, Presneau N, Prokofyeva D, Purrington K, Pylkäs K, Rack B, Radice P, Rau-Murthy R, Rennert G, Rennert HS, Rhenius V, Robson M, Romero A, Ruddy KJ, Ruebner M, Saloustros E, Sandler DP, Sawyer EJ, Schmidt DF, Schmutzler RK, Schneeweiss A, Schoemaker MJ, Schumacher F, Schürmann P, Schwentner L, Scott C, Scott RJ, Seynaeve C, Shah M, Sherman ME, Shrubsole MJ, Shu X-O, Slager S, Smeets A, Sohn C, Soucy P, Southey MC, Spinelli JJ, Stegmaier C, Stone J, Swerdlow AJ, Tamimi RM, Tapper WJ, Taylor JA, Terry MB, Thöne K, Tollenaar RAEM, Tomlinson I, Truong T, Tzardi M, Ulmer H-U, Untch M, Vachon CM, van Veen EM, Vijai J, Weinberg CR, Wendt C, Whittemore AS, Wildiers H, Willett W, Winqvist R, Wolk A, Yang XR, Yannoukakos D, Zhang Y, Zheng W, Ziogas A, Dunning AM, Thompson DJ, Chenevix-Trench G, Chang-Claude J, Schmidt MK, Hall P, Milne RL, Pharoah PDP, Antoniou AC, Chatterjee N, Kraft P, García-Closas M, Simard J, Easton DF. Polygenic risk scores for prediction of breast cancer and breast cancer subtypes. Am J Hum Genet 2019;104:21–34 10.1016/j.ajhg.2018.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Manchanda R, Legood R, Antoniou AC, Gordeev VS, Menon U. Specifying the ovarian cancer risk threshold of 'premenopausal risk-reducing salpingo-oophorectomy' for ovarian cancer prevention: a cost-effectiveness analysis. J Med Genet 2016;53:591–9. 10.1136/jmedgenet-2016-103800 [DOI] [PubMed] [Google Scholar]
- 28. Manchanda R, Legood R, Pearce L, Menon U. Defining the risk threshold for risk reducing salpingo-oophorectomy for ovarian cancer prevention in low risk postmenopausal women. Gynecol Oncol 2015;139:487–94. 10.1016/j.ygyno.2015.10.001 [DOI] [PubMed] [Google Scholar]
- 29. Dareng EO, Tyrer JP, Barnes DR, Jones MR, Yang X, Aben KKH, Adank MA, Agata S, Andrulis IL, Anton-Culver H, Antonenkova NN, Aravantinos G, Arun BK, Augustinsson A, Balmaña J, Bandera EV, Barkardottir RB, Barrowdale D, Beckmann MW, Beeghly-Fadiel A, Benitez J, Bermisheva M, Bernardini MQ, Bjorge L, Black A, Bogdanova NV, Bonanni B, Borg A, Brenton JD, Budzilowska A, Butzow R, Buys SS, Cai H, Caligo MA, Campbell I, Cannioto R, Cassingham H, Chang-Claude J, Chanock SJ, Chen K, Chiew Y-E, Chung WK, Claes KBM, Colonna S, Cook LS, Couch FJ, Daly MB, Dao F, Davies E, de la Hoya M, de Putter R, Dennis J, DePersia A, Devilee P, Diez O, Ding YC, Doherty JA, Domchek SM, Dörk T, du Bois A, Dürst M, Eccles DM, Eliassen HA, Engel C, Evans GD, Fasching PA, Flanagan JM, Fortner RT, Machackova E, Friedman E, Ganz PA, Garber J, Gensini F, Giles GG, Glendon G, Godwin AK, Goodman MT, Greene MH, Gronwald J, Hahnen E, Haiman CA, Håkansson N, Hamann U, Hansen TVO, Harris HR, Hartman M, Heitz F, Hildebrandt MAT, Høgdall E, Høgdall CK, Hopper JL, Huang R-Y, Huff C, Hulick PJ, Huntsman DG, Imyanitov EN, Isaacs C, Jakubowska A, James PA, Janavicius R, Jensen A, Johannsson OT, John EM, Jones ME, Kang D, Karlan BY, Karnezis A, Kelemen LE, Khusnutdinova E, Kiemeney LA, Kim B-G, Kjaer SK, Komenaka I, Kupryjanczyk J, Kurian AW, Kwong A, Lambrechts D, Larson MC, Lazaro C, Le ND, Leslie G, Lester J, Lesueur F, Levine DA, Li L, Li J, Loud JT, Lu KH, Lubiński J, Mai PL, Manoukian S, Marks JR, Matsuno RK, Matsuo K, May T, McGuffog L, McLaughlin JR, McNeish IA, Mebirouk N, Menon U, Miller A, Milne RL, Minlikeeva A, Modugno F, Montagna M, Moysich KB, Munro E, Nathanson KL, Neuhausen SL, Nevanlinna H, Yie JNY, Nielsen HR, Nielsen FC, Nikitina-Zake L, Odunsi K, Offit K, Olah E, Olbrecht S, Olopade OI, Olson SH, Olsson H, Osorio A, Papi L, Park SK, Parsons MT, Pathak H, Pedersen IS, Peixoto A, Pejovic T, Perez-Segura P, Permuth JB, Peshkin B, Peterlongo P, Piskorz A, Prokofyeva D, Radice P, Rantala J, Riggan MJ, Risch HA, Rodriguez-Antona C, Ross E, Rossing MA, Runnebaum I, Sandler DP, Santamariña M, Soucy P, Schmutzler RK, Setiawan VW, Shan K, Sieh W, Simard J, Singer CF, Sokolenko AP, Song H, Southey MC, Steed H, Stoppa-Lyonnet D, Sutphen R, Swerdlow AJ, Tan YY, Teixeira MR, Teo SH, Terry KL, Terry MB, Thomassen M, Thompson PJ, Thomsen LCV, Thull DL, Tischkowitz M, Titus L, Toland AE, Torres D, Trabert B, Travis R, Tung N, Tworoger SS, Valen E, van Altena AM, van der Hout AH, Van Nieuwenhuysen E, van Rensburg EJ, Vega A, Edwards DV, Vierkant RA, Wang F, Wappenschmidt B, Webb PM, Weinberg CR, Weitzel JN, Wentzensen N, White E, Whittemore AS, Winham SJ, Wolk A, Woo Y-L, Wu AH, Yan L, Yannoukakos D, Zavaglia KM, Zheng W, Ziogas A, Zorn KK, Kleibl Z, Easton D, Lawrenson K, DeFazio A, Sellers TA, Ramus SJ, Pearce CL, Monteiro AN, Cunningham J, Goode EL, Schildkraut JM, Berchuck A, Chenevix-Trench G, Gayther SA, Antoniou AC, Pharoah PDP, GEMO Study Collaborators, GC-HBOC Study Collaborators, EMBRACE Collaborators, OPAL Study Group, AOCS Group, KConFab Investigators, HEBON Investigators, OCAC Consortium, CIMBA Consortium . Polygenic risk modeling for prediction of epithelial ovarian cancer risk. Eur J Hum Genet 2022;30:349–62. 10.1038/s41431-021-00987-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Antoniou AC, Pharoah PD, McMullan G, Day NE, Ponder BA, Easton D. Evidence for further breast cancer susceptibility genes in addition to BRCA1 and BRCA2 in a population-based study. Genet Epidemiol 2001;21:1–18. 10.1002/gepi.1014 [DOI] [PubMed] [Google Scholar]
- 31. Yang X, Eriksson M, Czene K, Lee A, Leslie G, Lush M, Wang Q, Dennis J, Dorling L, Carvalho S, Mavaddat N, Simard J, Schmidt MK, Easton DF, Hall P, Antoniou AC. Prospective validation of the BOADICEA multifactorial breast cancer risk prediction model in a large prospective cohort study. J Med Gen 2022. 10.1136/jmg-2022-108806. [Epub ahead of print: 26 Sept 2022]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Muranen TA, Greco D, Blomqvist C, Aittomäki K, Khan S, Hogervorst F, Verhoef S, Pharoah PDP, Dunning AM, Shah M, Luben R, Bojesen SE, Nordestgaard BG, Schoemaker M, Swerdlow A, García-Closas M, Figueroa J, Dörk T, Bogdanova NV, Hall P, Li J, Khusnutdinova E, Bermisheva M, Kristensen V, Borresen-Dale A-L, Peto J, dos Santos Silva I, Couch FJ, Olson JE, Hillemans P, Park-Simon T-W, Brauch H, Hamann U, Burwinkel B, Marme F, Meindl A, Schmutzler RK, Cox A, Cross SS, Sawyer EJ, Tomlinson I, Lambrechts D, Moisse M, Lindblom A, Margolin S, Hollestelle A, Martens JWM, Fasching PA, Beckmann MW, Andrulis IL, Knight JA, Anton-Culver H, Ziogas A, Giles GG, Milne RL, Brenner H, Arndt V, Mannermaa A, Kosma V-M, Chang-Claude J, Rudolph A, Devilee P, Seynaeve C, Hopper JL, Southey MC, John EM, Whittemore AS, Bolla MK, Wang Q, Michailidou K, Dennis J, Easton DF, Schmidt MK, Nevanlinna H. Genetic modifiers of CHEK2*1100delC-associated breast cancer risk. Genetics in Medicine 2017;19:599–603. 10.1038/gim.2016.147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gao C, Polley EC, Hart SN, Huang H, Hu C, Gnanaolivu R, Lilyquist J, Boddicker NJ, Na J, Ambrosone CB, Auer PL, Bernstein L, Burnside ES, Eliassen AH, Gaudet MM, Haiman C, Hunter DJ, Jacobs EJ, John EM, Lindström S, Ma H, Neuhausen SL, Newcomb PA, O'Brien KM, Olson JE, Ong IM, Patel AV, Palmer JR, Sandler DP, Tamimi R, Taylor JA, Teras LR, Trentham-Dietz A, Vachon CM, Weinberg CR, Yao S, Weitzel JN, Goldgar DE, Domchek SM, Nathanson KL, Couch FJ, Kraft P. Risk of breast cancer among carriers of pathogenic variants in breast cancer predisposition genes varies by polygenic risk score. J Clin Oncol 2021;39:JCO2001992. 10.1200/JCO.20.01992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gallagher S, Hughes E, Wagner S, Tshiaba P, Rosenthal E, Roa BB, Kurian AW, Domchek SM, Garber J, Lancaster J, Weitzel JN, Gutin A, Lanchbury JS, Robson M. Association of a polygenic risk score with breast cancer among women carriers of high- and moderate-risk breast cancer genes. JAMA Netw Open 2020;3:e208501. 10.1001/jamanetworkopen.2020.8501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kapoor PM, Mavaddat N, Choudhury PP, Wilcox AN, Lindström S, Behrens S, Michailidou K, Dennis J, Bolla MK, Wang Q, Jung A, Abu-Ful Z, Ahearn T, Andrulis IL, Anton-Culver H, Arndt V, Aronson KJ, Auer PL, Freeman LEB, Becher H, Beckmann MW, Beeghly-Fadiel A, Benitez J, Bernstein L, Bojesen SE, Brauch H, Brenner H, Brüning T, Cai Q, Campa D, Canzian F, Carracedo A, Carter BD, Castelao JE, Chanock SJ, Chatterjee N, Chenevix-Trench G, Clarke CL, Couch FJ, Cox A, Cross SS, Czene K, Dai JY, Earp HS, Ekici AB, Eliassen AH, Eriksson M, Evans DG, Fasching PA, Figueroa J, Fritschi L, Gabrielson M, Gago-Dominguez M, Gao C, Gapstur SM, Gaudet MM, Giles GG, González-Neira A, Guénel P, Haeberle L, Haiman CA, Håkansson N, Hall P, Hamann U, Hatse S, Heyworth J, Holleczek B, Hoover RN, Hopper JL, Howell A, Hunter DJ, John EM, Jones ME, Kaaks R, Keeman R, Kitahara CM, Ko Y-D, Koutros S, Kurian AW, Lambrechts D, Le Marchand L, Lee E, Lejbkowicz F, Linet M, Lissowska J, Llaneza A, MacInnis RJ, Martinez ME, Maurer T, McLean C, Neuhausen SL, Newman WG, Norman A, O'Brien KM, Olshan AF, Olson JE, Olsson H, Orr N, Perou CM, Pita G, Polley EC, Prentice RL, Rennert G, Rennert HS, Ruddy KJ, Sandler DP, Saunders C, Schoemaker MJ, Schöttker B, Schumacher F, Scott C, Scott RJ, Shu X-O, Smeets A, Southey MC, Spinelli JJ, Stone J, Swerdlow AJ, Tamimi RM, Taylor JA, Troester MA, Vachon CM, van Veen EM, Wang X, Weinberg CR, Weltens C, Willett W, Winham SJ, Wolk A, Yang XR, Zheng W, Ziogas A, Dunning AM, Pharoah PDP, Schmidt MK, Kraft P, Easton DF, Milne RL, García-Closas M, Chang-Claude J, ABCTB Investigators, kConFab/AOCS Investigators . Combined associations of a polygenic risk score and classical risk factors with breast cancer risk. J Natl Cancer Inst 2021;113:329–37. 10.1093/jnci/djaa056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Schmidt MK, Hogervorst F, van Hien R, Cornelissen S, Broeks A, Adank MA, Meijers H, Waisfisz Q, Hollestelle A, Schutte M, van den Ouweland A, Hooning M, Andrulis IL, Anton-Culver H, Antonenkova NN, Antoniou AC, Arndt V, Bermisheva M, Bogdanova NV, Bolla MK, Brauch H, Brenner H, Brüning T, Burwinkel B, Chang-Claude J, Chenevix-Trench G, Couch FJ, Cox A, Cross SS, Czene K, Dunning AM, Fasching PA, Figueroa J, Fletcher O, Flyger H, Galle E, García-Closas M, Giles GG, Haeberle L, Hall P, Hillemanns P, Hopper JL, Jakubowska A, John EM, Jones M, Khusnutdinova E, Knight JA, Kosma V-M, Kristensen V, Lee A, Lindblom A, Lubinski J, Mannermaa A, Margolin S, Meindl A, Milne RL, Muranen TA, Newcomb PA, Offit K, Park-Simon T-W, Peto J, Pharoah PDP, Robson M, Rudolph A, Sawyer EJ, Schmutzler RK, Seynaeve C, Soens J, Southey MC, Spurdle AB, Surowy H, Swerdlow A, Tollenaar RAEM, Tomlinson I, Trentham-Dietz A, Vachon C, Wang Q, Whittemore AS, Ziogas A, van der Kolk L, Nevanlinna H, Dörk T, Bojesen S, Easton DF. Age- and tumor subtype-specific breast cancer risk estimates for CHEK2*1100delC carriers. J Clin Oncol 2016;34:2750–60. 10.1200/JCO.2016.66.5844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Eriksson M, Li J, Leifland K, Czene K, Hall P. A comprehensive tool for measuring mammographic density changes over time. Breast Cancer Res Treat 2018;169:371–9. 10.1007/s10549-018-4690-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Byng JW, Boyd NF, Fishell E, Jong RA, Yaffe MJ. The quantitative analysis of mammographic densities. Phys Med Biol 1994;39:1629–38. 10.1088/0031-9155/39/10/008 [DOI] [PubMed] [Google Scholar]
- 39. Astley SM, Harkness EF, Sergeant JC, Warwick J, Stavrinos P, Warren R, Wilson M, Beetles U, Gadde S, Lim Y, Jain A, Bundred S, Barr N, Reece V, Brentnall AR, Cuzick J, Howell T, Evans DG. A comparison of five methods of measuring mammographic density: a case-control study. Breast Cancer Res 2018;20:10. 10.1186/s13058-018-0932-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chatterjee N, Shi J, García-Closas M. Developing and evaluating polygenic risk prediction models for stratified disease prevention. Nat Rev Genet 2016;17:392–406. 10.1038/nrg.2016.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pal Choudhury P, Maas P, Wilcox A, Wheeler W, Brook M, Check D, Garcia-Closas M, Chatterjee N. iCARE: an R package to build, validate and apply absolute risk models. PLoS One 2020;15:e0228198. 10.1371/journal.pone.0228198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Pal Choudhury P, Brook MN, Hurson AN, Lee A, Mulder CV, Coulson P, Schoemaker MJ, Jones ME, Swerdlow AJ, Chatterjee N, Antoniou AC, Garcia-Closas M. Comparative validation of the BOADICEA and Tyrer-Cuzick breast cancer risk models incorporating classical risk factors and polygenic risk in a population-based prospective cohort of women of European ancestry. Breast Cancer Res 2021;23:22. 10.1186/s13058-021-01399-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pal Choudhury P, Wilcox AN, Brook MN, Zhang Y, Ahearn T, Orr N, Coulson P, Schoemaker MJ, Jones ME, Gail MH, Swerdlow AJ, Chatterjee N, Garcia-Closas M. Comparative validation of breast cancer risk prediction models and projections for future risk stratification. J Natl Cancer Inst 2020;112:278–85. 10.1093/jnci/djz113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ho W-K, Tan M-M, Mavaddat N, Tai M-C, Mariapun S, Li J, Ho P-J, Dennis J, Tyrer JP, Bolla MK, Michailidou K, Wang Q, Kang D, Choi J-Y, Jamaris S, Shu X-O, Yoon S-Y, Park SK, Kim S-W, Shen C-Y, Yu J-C, Tan EY, Chan PMY, Muir K, Lophatananon A, Wu AH, Stram DO, Matsuo K, Ito H, Chan CW, Ngeow J, Yong WS, Lim SH, Lim GH, Kwong A, Chan TL, Tan SM, Seah J, John EM, Kurian AW, Koh W-P, Khor CC, Iwasaki M, Yamaji T, Tan KMV, Tan KTB, Spinelli JJ, Aronson KJ, Hasan SN, Rahmat K, Vijayananthan A, Sim X, Pharoah PDP, Zheng W, Dunning AM, Simard J, van Dam RM, Yip C-H, Taib NAM, Hartman M, Easton DF, Teo S-H, Antoniou AC. European polygenic risk score for prediction of breast cancer shows similar performance in Asian women. Nat Commun 2020;11:3833. 10.1038/s41467-020-17680-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Shieh Y, Fejerman L, Lott PC, Marker K, Sawyer SD, Hu D, Huntsman S, Torres J, Echeverry M, Bohórquez ME, Martínez-Chéquer JC, Polanco-Echeverry G, Estrada-Flórez AP, Haiman CA, John EM, Kushi LH, Torres-Mejía G, Vidaurre T, Weitzel JN, Zambrano SC, Carvajal-Carmona LG, Ziv E, Neuhausen SL. A polygenic risk score for breast cancer in US Latinas and Latin American women. J Natl Cancer Inst 2020;112:590–8. 10.1093/jnci/djz174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dorling L, Carvalho S, Allen J, Parsons MT, Fortuno C, González-Neira A, Heijl SM, Adank MA, Ahearn TU, Andrulis IL, Auvinen P, Becher H, Beckmann MW, Behrens S, Bermisheva M, Bogdanova NV, Bojesen SE, Bolla MK, Bremer M, Briceno I, Camp NJ, Campbell A, Castelao JE, Chang-Claude J, Chanock SJ, Chenevix-Trench G, Collée JM, Czene K, Dennis J, Dörk T, Eriksson M, Evans DG, Fasching PA, Figueroa J, Flyger H, Gabrielson M, Gago-Dominguez M, García-Closas M, Giles GG, Glendon G, Guénel P, Gündert M, Hadjisavvas A, Hahnen E, Hall P, Hamann U, Harkness EF, Hartman M, Hogervorst FBL, Hollestelle A, Hoppe R, Howell A, Jakubowska A, Jung A, Khusnutdinova E, Kim S-W, Ko Y-D, Kristensen VN, Lakeman IMM, Li J, Lindblom A, Loizidou MA, Lophatananon A, Lubiński J, Luccarini C, Madsen MJ, Mannermaa A, Manoochehri M, Margolin S, Mavroudis D, Milne RL, Mohd Taib NA, Muir K, Nevanlinna H, Newman WG, Oosterwijk JC, Park SK, Peterlongo P, Radice P, Saloustros E, Sawyer EJ, Schmutzler RK, Shah M, Sim X, Southey MC, Surowy H, Suvanto M, Tomlinson I, Torres D, Truong T, van Asperen CJ, Waltes R, Wang Q, Yang XR, Pharoah PDP, Schmidt MK, Benitez J, Vroling B, Dunning AM, Teo SH, Kvist A, de la Hoya M, Devilee P, Spurdle AB, Vreeswijk MPG, Easton DF, NBCS Collaborators, kConFab Investigators, SGBCC Investigators . Breast cancer risks associated with missense variants in breast cancer susceptibility genes. Genome Med 2022;14:51. 10.1186/s13073-022-01052-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jmedgenet-2022-108471supp001.pdf (1.3MB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study. The models are implemented in the CanRisk tool, which is freely available at www.canrisk.org.