Abstract
The unobliterated portion of embryological thyroglossal duct may present as cystic swelling later in life and may contain functional thyroid follicles. This cyst requires excision along with the entire thyroglossal duct remnant and adjacent portion of hyoid bone. At times, the excised specimen could demonstrate a focus of carcinomatous change inside the cyst wall. Very rarely, this thyroglossal duct cyst carcinoma could be associated with malignancy of native thyroid gland. This case report illustrates an interesting case of synchronous carcinoma of thyroglossal duct cyst and native thyroid gland. It also sheds light on the controversies related to the pathophysiology of such association and the dilemmas surrounding the management of thyroglossal duct cyst carcinoma, with or without concurrent carcinoma of thyroid gland.
Keywords: Ear, nose and throat/otolaryngology; Thyroid disease; Endocrine cancer; Head and neck surgery; General surgery
Background
Thyroglossal duct cyst (TDC) is one of the most common developmental anomalies of the neck. It represents an unobliterated portion of the embryological thyroglossal duct, and presents as painless cystic swelling in the anterior upper neck, mostly in adolescents and young adults.1 2 Nearly all cases of TDC can be effectively managed by the Sistrunk surgery, a procedure that includes excision of the entire tract of the thyroglossal duct remnant along with the adjacent central part of the hyoid bone.1–3 As per the literature, 60%–100% of the excised TDCs demonstrate functional thyroid follicles of their cyst walls.1 4 Further, similar to the thyroid follicles of a native thyroid gland, these aberrant thyroid follicles of TDC could also undergo a carcinomatous transformation, constituting a peculiar clinical entity called the thyroglossal duct cyst carcinoma (TDCC).5 Histologically, the majority of the TDCCs tend to be papillary cancers, but rarely could there be a focus of follicular carcinoma, squamous cell carcinoma or even mucoepidermoid carcinoma inside the TDC.6–8 There are also reports of TDCC being coexistent with the concurrent carcinoma of the native thyroid gland.9–12
The aetiopathogenesis and the management policies of TDCC have been a topic of debate for years. While some of the authors consider the TDCC as an independent and primary neoplasm of TDC, others attribute it as a metastatic lesion from primary papillary carcinoma of the native thyroid gland.11–15 Consequently, there are ongoing deliberations on whether or not to consider thyroidectomy along with the Sistrunk surgery in TDCC.16–18 This case report presents an interesting and rare case of TDCC that was associated with a concurrent papillary microcarcinoma of the thyroid gland. After careful review of the relevant literature from the recent years, this report also outlines the current management principles of TDCC.
Case presentation
A healthy woman in her early thirties presented to our tertiary care hospital with a slowly progressive and painless swelling in the upper part of the neck that she had noticed for the last year. She had not perceived any voice change, dysphagia or breathing difficulty. On examination, swelling of 3×3 cm was noted in the upper part of the neck, at the midline and just above the hyoid bone, without any overt skin changes. The swelling was firm and non-tender on palpation and moved with tongue protrusion, suggestive of attachment to thyroglossal tract. There were no palpable lymph nodes or nodularities in the thyroid gland. The examinations of the oral cavity, pharynx and larynx were also within normal limits.
Investigations
An ultrasonography of the neck was ordered to further characterise the neck swelling. Sonologically, the well-defined cystic lesion measured around 1.9×0.8 cm and had contained solid components with internal septations, debris and macrocalcification, suggestive of an infected TDC. Incidentally, a hypoechoic nodule of 5×6 mm was also noted in the left lobe of the thyroid without any internal or peripheral vascularity, reported as category II as per the American College of Radiologists—Thyroid Imaging, Reporting and Data System.19 The patient was euthyroid clinically as well as biochemically.
Differential diagnosis
The slowly progressive midline neck swelling just above the hyoid bone, which moves with the tongue protrusion and without any evidence of local inflammation or lymphadenopathy, suggested the diagnosis of TDC. The ultrasonography corroborated with our clinical diagnosis.
Treatment
With the informed written consent, the patient was taken up for Sistrunk surgery under general anaesthesia. The cyst was excised in toto, along with the entire tract of the thyroglossal duct remnant and a cuff of soft tissue around the foramen cecum. The histopathological examination of the excised specimen showed a focus of papillary carcinoma, classic variant (size of 15×12 mm), inside the unobliterated portion of the thyroglossal cyst, as shown in figure 1.
Figure 1.
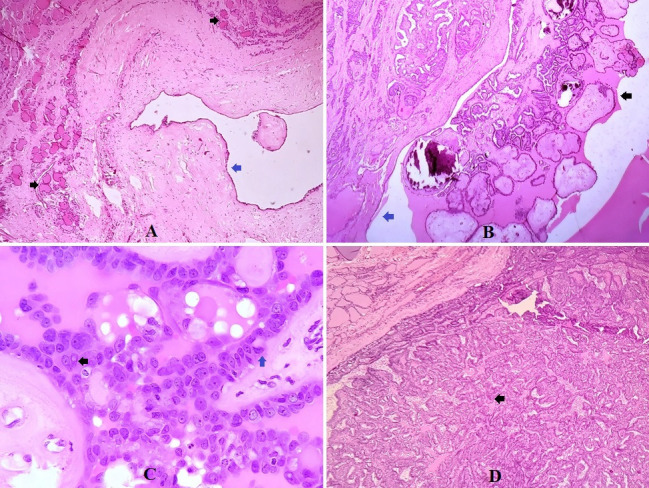
Photomicrographs (all H&E staining) of surgical specimen, showing normal thyroid follicles (black arrows) inside the excised thyroglossal cyst (blue arrow) (A) (magnification 10×); papillary carcinoma (black arrow) arising from the thyroglossal duct cyst wall (blue arrow) along with psammomatous calcification (B) (magnification 10×); nuclear features of papillary carcinoma -pseudonuclear inclusions (black arrow), intranuclear groove (blue arrow) with crowding and overlapping of nucleus (C) (magnification 40×); and papillary microcarcinoma (black arrow) in the thyroidectomy specimen (D) (magnification 10×).
Subsequently, the case was discussed in a multidisciplinary tumour board meeting, and the patient and relatives were counselled about the nature of the illness and further management options. As per the consensus between the involved parties, the patient then received total thyroidectomy and the level VI lymphadenectomy, along with the preservation of parathyroid glands. The surgery was undertaken within 3 weeks of the initial surgery, and the patient had uneventful postoperative recovery. As depicted in figure 1, the histopathological examination of the excised thyroid gland also revealed a focus of papillary microcarcinoma (7×5 mm) inside the left thyroid lobe nodule that had been witnessed on ultrasonogram previously. However, there was no evidence of any capsular breach, and none of the excised lymph nodes showed metastatic disease.
Outcome and follow-up
After reviewing the case in a multidisciplinary board about the adjuvant treatment, the patient was given 50 mCi radioiodine ablation therapy 4 weeks after the total thyroidectomy. The patient is kept on the replacement dose of levothyroxine sodium since and has been doing well. The follow-up radioiodine scan done after 5 months showed no abnormal radioiodine uptake, as shown in figure 2, and the serum thyroglobulin levels accorded with the complete remission. At the latest follow-up, 16 months after the thyroid surgery, the patient is disease free both clinically as well as biochemically.
Figure 2.
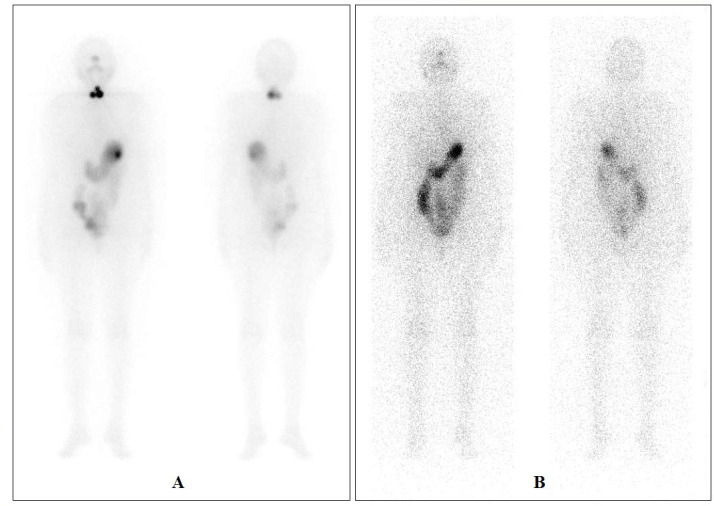
Immediate post-therapy scan (50 mCi iodine-131) showing multifocal residue at the thyroid bed (A); and follow-up iodine-131 whole body scan (2 mCi) done after 5 months of radioiodine ablation showed no significant uptake in the thyroid bed or elsewhere in the body (B).
Discussion
As per the recent systematic review that analysed all the published reports of TDCC, unlike the TDC that commonly manifests in children or adolescents, the TDCC tends to present much later in life, with the mean age of presentation at around 40 years.8 However, the age at presentation is not a reliable predictor of malignancy as several non-malignant TDCs could become clinically evident in later years of life, and a few TDC cases diagnosed among the young could harbour malignant neoplasm.20 21 Concerning the gender distribution, there is a slight female preponderance among the previously published cases of TDCC.8 The clinical manifestations of TDCC are mostly non-specific and are indistinguishable from that of a simple TDC. Some of the clinical signs that could reliably suggest an underlying malignant pathology in nodules of native thyroid gland could be of least diagnostic value in predicting TDCC. For instance, the presence of overlying skin fixity in a thyroid nodule is almost always suggestive of malignant neoplasm, but such finding in an otherwise inconspicuous TDC is mostly attributed to the past infection and scarring/fibrosis. Similarly, some of the other warning signs such as, dysphonia, stridor or dysphagia, that generally imply malignancy in thyroid nodule could be seen even in non-malignant TDC with unusual location and extension, rendering them non-reliable for predicting malignancy in TDC.22–25 Of all the signs and symptoms, the presence of a suspicious cervical lymph node is probably the most reliable clinical finding to suggest a possible malignant pathology inside the TDC, but the incidence of metastatic cervical lymphadenopathy in TDCC is only around 10%–15%.6 8 11
Almost three-fourths of the diagnosed cases of TDCC in the literature were identified only after the histopathological examination of the excised specimen, which preoperatively had been considered as a simple TDC.8 26 The index case presented here represents a typical case of TDCC with respect to demographic profile, clinical manifestations and diagnosis. As for the reviewed literature, only fourth of the published cases of TDCC had received pre-excision diagnosis, majority by a fine-needle aspiration cytology (FNAC) and a few cases by intraoperative frozen section.8 Although the simple and straightforward investigation of FNAC could provide the diagnosis of TDCC preoperatively in many cases (and thus aid in appropriate counselling of the patients and therapeutic planning), it may not be cost-effective as a routine test in all cases of TDC, considering its poor negative predictive value as well as the low incidence of malignancy in TDC.8 27 As per the recent systematic review on TDCC, the role of FNAC in diagnosing TDCC is debatable at best and mostly considered ineffective as a routine investigation.8 However, this should be very well considered in suspicious cases, particularly in those with cervical lymphadenopathy, in which case a FNAC from the suspicious lymph node should also be considered.6 21 28
As far as the therapeutic principle of the TDCC is concerned, Sistrunk procedure with or without thyroidectomy and with or without neck dissection forms the mainstay of treatment. And this has to be followed up by adjuvant radioiodine ablation as per the post-surgery risk stratification. Interestingly, we found no substantial evidence that could back a universal surgical recommendation, applicable for all cases of TDCC. In fact, the present consensus suggests an individualised surgical approach, depending on the clinical scenario at hand. As depicted in figure 3, on the basis of the available literature, we have formulated a management algorithm for TDCC with or without concurrent thyroid neoplasm. According to this approach, in a typical case of TDCC, in the absence of thyroid nodule and cervical lymph nodes, a good Sistrunk surgery itself is an adequate and oncologically sound surgical procedure for definitive treatment.8 9 16 18
Figure 3.
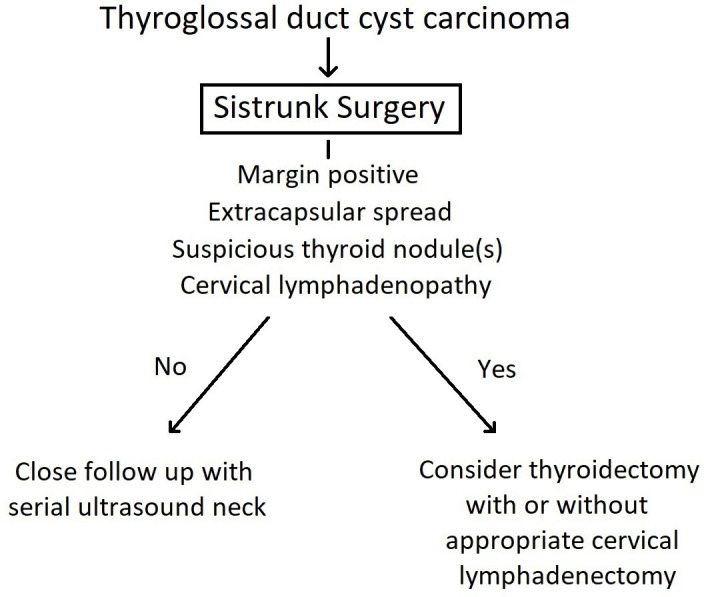
Flow chart depicting the therapeutic approach in thyroglossal duct cyst carcinoma.
The decision to proceed with total thyroidectomy in the case of TDCC is not straightforward and is marred with controversy.14–18 The need for prophylactic thyroidectomy in TDCC is fuelled by two arguments. One, the reported incidence of concurrent thyroid neoplasm in TDCC can be as high as 50%–65%29–31; and the other is to facilitate the post-surgery radioiodine ablation indicated in differentiated thyroid malignancies.8 However, as per the systematic review of all published cases of TDCC, the rate of concurrent thyroid malignancy in TDCC who had undergone thyroidectomy is actually less than the rate of incidental thyroid carcinoma being detected at autopsy.8 Moreover, as in the index case presented here, in most of the TDCC cases, the concurrent thyroid neoplasms in thyroidectomy specimen tend to be microcarcinoma (size less than 1 cm), suggesting a favourable prognosis even when not operated on.4 The extrapolation from the American Thyroid Association’s recommendations for early thyroid neoplasm also downplays the survival benefit offered by the routine thyroidectomy in all cases of TDCC, and suggests a conservative approach for those TDCCs which have no other risk factors.4 16 Considering the preceding discussion, it is safe to presume that the total thyroidectomy may not be necessary in all cases of TDCC and should be reserved for only those with a high-risk profile. Similarly, the requirement of neck dissection in a case of TDCC could be determined by the clinic-radiological presence or absence of the high-risk features such as suspicious thyroid nodule or cervical lymph node(s).8 This recommendation is also supported by the several other reports.1 5 10 14 18 However, we would like to reiterate that, in the absence of other risk factors, close follow-up without thyroidectomy is a valid option in TDCC cases, even when there is a small non-suspicious thyroid nodule. In the index case reported here, although the presence of a thyroid nodule in sonography prompted us to offer thyroidectomy to the patient, it was the consensus reached between the treating team and the patient which led to the completion of thyroidectomy.
Concerning postoperative radioiodine ablation, although there is no clear evidence of its benefit in all operated cases of TDCC, the current consensus suggests its use only in cases with additional risk factors such as extracapsular extension (soft tissue involvement), positive lymph nodes and concurrent thyroid malignancy.8 17 18 The patient described in this report received radioiodine ablation owing to the concurrent thyroid neoplasm but had no additional risk factors to consider adjuvant radiotherapy. Despite the dearth in the guidelines with respect to the utility of adjuvant radiotherapy in TDCC, it seems to offer some benefit only when a TDCC harbours squamous cell carcinoma, with or without lymph node metastasis.8 The adjuvant radiotherapy may also be indicated in recurrent cases that do not express radioiodine avidity.8 32 Lastly, with regard to the prognosis of TDCC, the survival outcomes are excellent after appropriate surgical management, with only a few reports of locoregional recurrences and distant metastasis in the literature.4 5 8 16
PATIENT’S PERSPECTIVE
I had a neck swelling which was initially told to be a benign thyroglossal disease. Although I was reluctant to undergo surgery, after multiple consultations at different places I decided to undergo surgery at this hospital. During the post-operative follow-up, I was told to have malignant disease, which increased my fear. However, the treating doctors counselled me and my family about the available treatment options and their results, which to certain extent relieved my anxiety. The surgery and further radio-ablation were uneventful and I am happy to be disease-free now. Compared to the other patients whom I was interacting with at the hospital, who had aggressive diseases, I am fortunate to have gotten rid of this disease in the smaller stage itself. I am grateful to the doctors and hospital that treated me. (only grammar has been edited by the authors).
Learning points
Thyroglossal duct cyst is not uncommon; however, several of these cases might have functional thyroid follicles, and rarely, can harbour differentiated thyroid carcinoma arising from such follicles.
Since the thyroglossal duct cyst carcinoma tends to be indolent and its clinical presentation tends to be identical to that of a simple thyroglossal duct cyst, the majority of these carcinoma cases get diagnosed only after final pathological examination of the excised cyst.
Very rarely, such thyroglossal duct cyst carcinoma could exhibit concurrent carcinoma of native thyroid gland too.
The treating surgeon should be able to tackle these situations by appropriate risk stratification and proceed accordingly.
Footnotes
Contributors: KD was involved in all stages of patient care and in manuscript writing, analysis and submission. SSM was involved in all stages of patient care and in manuscript analysis and submission. RN was involved in patient care, manuscript writing and submission. DHC was involved in patient care and in manuscript analysis and submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Zhu Y-Y, Wang C-G, Li W-Y, et al. Papillary thyroglossal duct carcinoma: report of nine cases and review of literature. Int J Clin Exp Pathol 2017;10:10102–11. [PMC free article] [PubMed] [Google Scholar]
- 2.Isaacson G. Sistrunk centennial: evolution of a classic operation. Laryngoscope 2020;130:E45–7. 10.1002/lary.27914 [DOI] [PubMed] [Google Scholar]
- 3.Rohof D, Honings J, Theunisse HJ, et al. Recurrences after thyroglossal duct cyst surgery: results in 207 consecutive cases and review of the literature. Head Neck 2015;37:1699–704. 10.1002/hed.23817 [DOI] [PubMed] [Google Scholar]
- 4.Thompson LDR, Herrera HB, Lau SK. Thyroglossal duct cyst carcinomas: a clinicopathologic series of 22 cases with staging recommendations. Head Neck Pathol 2017;11:175–85. 10.1007/s12105-016-0757-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choi YM, Kim TY, Song DE, et al. Papillary thyroid carcinoma arising from a thyroglossal duct cyst: a single institution experience. Endocr J 2013;60:665–70. 10.1507/endocrj.EJ12-0366 [DOI] [PubMed] [Google Scholar]
- 6.Puccini M, Roffi N, Pucci V. Synchronous squamous cell carcinoma and papillary thyroid carcinoma arising from the thyroglossal duct remnant: case report and a review of the literature. SAGE Open Med Case Rep 2020;8:2050313X:20917846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang Q, Shen Y, Wang AY, et al. Squamous cell carcinoma arising from a thyroglossal duct cyst: a case report and review of the literature. SAGE Open Med Case Rep 2018;6:2050313X1876705. 10.1177/2050313X18767050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rayess HM, Monk I, Svider PF, et al. Thyroglossal duct cyst carcinoma: a systematic review of clinical features and outcomes. Otolaryngol Head Neck Surg 2017;156:794–802. 10.1177/0194599817696504 [DOI] [PubMed] [Google Scholar]
- 9.Cherian MP, Nair B, Thomas S, et al. Synchronous papillary carcinoma in thyroglossal duct cyst and thyroid gland: case report and review of literature. Head Neck 2009;31:1387–91. 10.1002/hed.21029 [DOI] [PubMed] [Google Scholar]
- 10.Penna GCE, Mendes HG, Kraft AO, et al. Simultaneous papillary carcinoma in thyroglossal duct cyst and thyroid. Case Rep Endocrinol 2017;2017:8541078–5. 10.1155/2017/8541078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang S-I, Park K-K, Kim J-H. Papillary carcinoma arising from thyroglossal duct cyst with thyroid and lateral neck metastasis. Int J Surg Case Rep 2013;4:704–7. 10.1016/j.ijscr.2013.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ozturk K, Li F, Özütemiz C, et al. Not a pearl necklace: synchronous papillary carcinoma of thyroglossal duct cyst and thyroid gland. Clin Imaging 2021;73:111–4. 10.1016/j.clinimag.2020.12.005 [DOI] [PubMed] [Google Scholar]
- 13.Roehlen N, Takacs S, Ebeling O, et al. Ectopic papillary thyroid carcinoma within a thyroglossal duct cyst: a case report. Medicine 2017;96:e8921. 10.1097/MD.0000000000008921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rossi ED, Martini M, Straccia P, et al. Thyroglossal duct cyst cancer most likely arises from a thyroid gland remnant. Virchows Arch 2014;465:67–72. 10.1007/s00428-014-1583-9 [DOI] [PubMed] [Google Scholar]
- 15.Kermani W, Belcadhi M, Abdelkéfi M, et al. Papillary carcinoma arising in a thyroglossal duct cyst: case report and discussion of management modalities. Eur Arch Otorhinolaryngol 2008;265:233–6. 10.1007/s00405-007-0405-y [DOI] [PubMed] [Google Scholar]
- 16.Plaza CPR, López MED, Carrasco CE-G, et al. Management of well-differentiated thyroglossal remnant thyroid carcinoma: time to close the debate? report of five new cases and proposal of a definitive algorithm for treatment. Ann Surg Oncol 2006;13:745–52. 10.1245/ASO.2006.05.022 [DOI] [PubMed] [Google Scholar]
- 17.Lancini D, Lombardi D, Piazza C. Evidence and controversies in management of thyroglossal duct cyst carcinoma. Curr Opin Otolaryngol Head Neck Surg 2021;29:113–9. 10.1097/MOO.0000000000000699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wood CB, Bigcas J-L, Alava I, et al. Papillary-Type carcinoma of the thyroglossal duct cyst: the case for conservative management. Ann Otol Rhinol Laryngol 2018;127:710–6. 10.1177/0003489418791892 [DOI] [PubMed] [Google Scholar]
- 19.Tessler FN, Middleton WD, Grant EG, et al. ACR thyroid imaging, reporting and data system (TI-RADS): white paper of the ACR TI-RADS Committee. J Am Coll Radiol 2017;14:587–95. 10.1016/j.jacr.2017.01.046 [DOI] [PubMed] [Google Scholar]
- 20.Mohan PS, Chokshi RA, Moser RL, et al. Thyroglossal duct cysts: a consideration in adults. Am Surg 2005;71:508–11. 10.1177/000313480507100612 [DOI] [PubMed] [Google Scholar]
- 21.Vassilatou E, Proikas K, Margari N, et al. An adolescent with a rare midline neck tumor: thyroid carcinoma in a thyroglossal duct cyst. J Pediatr Hematol Oncol 2014;36:407–9. 10.1097/MPH.0000000000000113 [DOI] [PubMed] [Google Scholar]
- 22.Tynan T, Potter N. Intra-hyoid thyroglossal duct cyst: embryology in practice. ANZ J Surg 2020;90:1506–7. 10.1111/ans.15594 [DOI] [PubMed] [Google Scholar]
- 23.Bosco S, Cohn JE, Evarts M, et al. Thyroglossal duct cyst occupying posterior hyoid space with endolaryngeal extension presenting after neck trauma. Ann Otol Rhinol Laryngol 2020;129:628–32. 10.1177/0003489419901140 [DOI] [PubMed] [Google Scholar]
- 24.Kunitomo N, Fujii H, Fujita A, et al. Thyroglossal duct carcinoma originating in the hyoid bone. Case Rep Radiol 2019;2019:1–4. 10.1155/2019/3067346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang P-K, Hsieh L-C, Leu Y-S. Thyroglossal duct cyst papillary carcinoma with airway compromise. Ear Nose Throat J 2021;1455613211022077:014556132110220. 10.1177/01455613211022077 [DOI] [PubMed] [Google Scholar]
- 26.Alatsakis M, Drogouti M, Tsompanidou C, et al. Invasive thyroglossal duct cyst papillary carcinoma: a case report and review of the literature. Am J Case Rep 2018;19:757–62. 10.12659/AJCR.907313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bardales RH, Suhrland MJ, Korourian S, et al. Cytologic findings in thyroglossal duct carcinoma. Am J Clin Pathol 1996;106:615–9. 10.1093/ajcp/106.5.615 [DOI] [PubMed] [Google Scholar]
- 28.Das DK, George SA, Mohammad T, et al. Papillary carcinoma in thyroglossal duct cyst: diagnosis by fine-needle aspiration cytology and immunocytochemistry. Diagn Cytopathol 2018;46:797–800. 10.1002/dc.23968 [DOI] [PubMed] [Google Scholar]
- 29.Bakkar S, Biricotti M, Stefanini G, et al. The extent of surgery in thyroglossal cyst carcinoma. Langenbecks Arch Surg 2017;402:799–804. 10.1007/s00423-016-1460-x [DOI] [PubMed] [Google Scholar]
- 30.Miccoli P, Minuto MN, Galleri D, et al. Extent of surgery in thyroglossal duct carcinoma: reflections on a series of eighteen cases. Thyroid 2004;14:121–3. 10.1089/105072504322880355 [DOI] [PubMed] [Google Scholar]
- 31.Hartl DM, Al Ghuzlan A, Chami L, et al. High rate of multifocality and occult lymph node metastases in papillary thyroid carcinoma arising in thyroglossal duct cysts. Ann Surg Oncol 2009;16:2595–601. 10.1245/s10434-009-0571-9 [DOI] [PubMed] [Google Scholar]
- 32.Hanna E. Squamous cell carcinoma in a thyroglossal duct cyst (TGDC): clinical presentation, diagnosis, and management. Am J Otolaryngol 1996;17:353–7. 10.1016/S0196-0709(96)90025-3 [DOI] [PubMed] [Google Scholar]


