Abstract
Background:
Contact tracing (CT) is an effective tool for breaking the chains of transmission in infectious disease outbreaks. This study was conducted to observe the trend of isolation and quarantine, assess the source of infection and contacts, and assess the effectiveness of CT in the early detection of infection among health-care workers (HCWs).
Methods:
This study was conducted using secondary analysis of routine CT records of HCWs of a tertiary care hospital in Mumbai from April 9, 2020, to December 31, 2020. Details of all HCWs exposed or infected with COVID-19 were collected in a standard format developed for this purpose telephonically. The exposed HCWs were further divided into high-risk (HR)/low-risk (LR) contacts and quarantined.
Results:
A total of 744 HCWs were isolated during this period and 1486 contacts were quarantined against them. Majority of the HCWs affected from COVID-19 were resident doctors, interns, and nursing staff. More than 81% of the positive HCWs were symptomatic. The overall ratio between isolated HCWs and quarantined HCWs is 1:2. A total of 88 (6%) HCWs tested positive from quarantine. The test positivity rate among HR contacts was 9.01% and among LR contacts was 2.72%.
Conclusions:
Effective CT of positive HCWs greatly aids in the early identification of contacts and timely quarantine. Over a period of time, the number of HCWs getting isolated or quarantined is found to decrease. This is the true success of CT. This strategy can be implemented among other medical colleges and hospitals too.
Keywords: Contact tracing, COVID-19, health-care workers, risk stratification
INTRODUCTION
Ever since the beginning of the pandemic, COVID-19 has been surprised with its novelty and posed challenges in its prevention and control. Activities such as case identification, isolation, testing and care, contact tracing (CT), and quarantine play an important role. CT, when systematically applied, breaks the chains of transmission and serves as an essential public health tool for controlling infectious disease outbreaks.[1]
An adequate number of health-care workers (HCWs) are crucial to maintain patient care during the ongoing COVID-19 pandemic. Potential exposure to SARS-CoV-2 is inherent to their work, thus making them a highly vulnerable group.[2,3] Effective CT of potentially exposed HCWs is crucial for the prevention and control of infectious disease outbreaks in the health-care setting. This study was conducted in a tertiary care hospital in Mumbai, India, to observe the trend of isolation and quarantine, assess the source of infection and contacts, and assess the effectiveness of CT in the early detection of infection among HCWs.
METHODS
CT of HCWs who are exposed to COVID-19 was started from April 9, 2020, by the department of community medicine after the first case was detected in the institute. Lab results of all those who test positive are notified to the CT team via a line list by the Department of Microbiology. A telephonic call is made by the team to each person tested positive and identify who among them were HCWs of the institute. HCWs who were tested outside the institute self-reported to the team or were reported by the respective supervisors. A standard format for the same was developed in line with the format used by the Public Health Department. Details of the positive HCWs such as demographic details, movement history in the past 2 weeks, type of test, source of infection, clinical condition, outcome, and details of contacts (low and high) were collected telephonically. Criteria for identifying high-risk and low-risk contacts are given in Table 1. All records were maintained as printed hard copy and soft copy on Microsoft Excel 2016. Secondary analysis of these records was done from April 9, 2020, to December 31, 2020. Ethical approval was obtained from the institutional ethics committee (EC/OA-144/2020). A total of 744 HCWs were isolated during this period and 1486 contacts were quarantined against them. In this study, isolation is a term reserved only for those who are confirmed cases of Covid 19 and quarantine refers to separating and restricting the movement of those who are exposed to Covid 19. Analysis was done using SPSS version 26.0 (IBM Corp. Released 2019. IBM SPSS Statistics for Windows , version 26.0. Armonk, NY:IBM Corp).
Table 1.
Baseline characteristics of isolated and quarantined health-care workers
| Baseline characteristics | Isolated HCWs (n=744), n (%) | Quarantined HCWs (n=1486), n (%) |
|---|---|---|
| HCW cadre | ||
| Senior doctors | 79 (10.6) | 184 (12.4) |
| Postgraduate doctors and interns | 221 (29.7) | 459 (30.9) |
| Nursing staff | 181 (24.3) | 434 (29.2) |
| Technicians - lab, X-ray, ECG | 49 (6.6) | 81 (5.5) |
| Class IV staff | 128 (17.2) | 215 (14.5) |
| Office staff | 69 (9.3) | 96 (6.4) |
| Security personnel | 17 (2.3) | 17 (1.1) |
| Age group (years) | ||
| ≤40 | 518 (69.6) | 1103 (74.2) |
| 41-50 | 110 (14.78) | 290 (19.5) |
| ≥50 | 116 (15.6) | 93 (6.3) |
| Mean age | 34.6±10.9 | 31.8±11.3 |
| Sex | ||
| Male | 394 (52.95) | 646 (43.5) |
| Female | 350 (47.04) | 840 (56.5) |
| Residence | ||
| In-campus hostels/quarters | 274 (36.82) | 625 (42.05) |
| Off campus - within/outside limits of the city | 470 (63.17 | 861 (57.94) |
HCWs: Health-care workers, ECG: Electrocardiogram
RESULTS
A total of 744 HCWs were isolated during this period and 1486 contacts were quarantined against them. The first COVID-19-positive HCW (sweeper) was notified on April 9, 2020. A maximum number of cases were reported in the months of May (179) and June (178). The number started decreasing from the month of July [Figure 1]. The highest count of positive cases was reported on April 29, where 22 cases were reported on a single day, 20 days after the first case [Figure 2]. The highest number of contacts that had to be quarantined against one case was 63, which was in the month of April 2020. The ratio between isolated HCWs and quarantined HCWs was 1:15 in the month of April which decreased significantly from the month of May. The overall ratio between isolated HCWs and quarantined HCWs is 1:2. On risk stratification, 899 (60.49%) were identified as high-risk (HR) contacts and 257 (17.29%) as low-risk (LR) contacts. Risk was not specified in 330 (22.20%) HCWs during the month of April. A total of 88 (6%) HCWs tested positive from quarantine, of which 81 (92%) were identified as HR contacts. The test positivity rate (total number of HR or LR contacts who tested positive from quarantine / total HR or LR contacts who are quarantined) among HR contacts was 9.01% and among LR contacts was 2.72%. The baseline characteristics of isolated and quarantined HCWs are given in Table 1.
Figure 1.
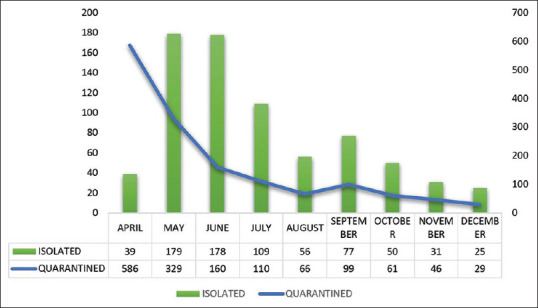
Month-wise distribution of isolated and quarantined health-care workers
Figure 2.
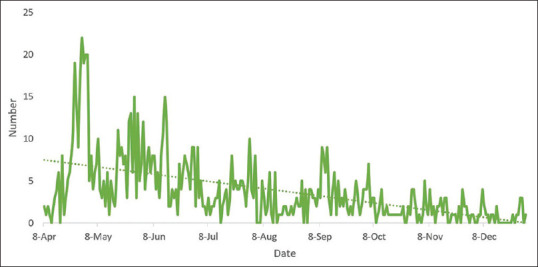
Daily trend of new positive cases from April 2020 to December 2020
The most common probable source of infection among HCWs was definitive history of contact with a positive person (51.88%), followed by workplace exposure (38.3%). About 46% of the HCWs gave a history of definitive contact with another positive HCW. No source of infection could be identified in 32% of the HCWs. The most common specific symptoms were fever (54.7%), cough (30.3%), sore throat (10%), and rhinitis (6.1%). Nonspecific symptoms cluster-like headache/myalgia/joint pains were seen in 40% of the HCWs. Around 32% of them reported multiple symptoms. Diarrhea was seen in 1.5% of the HCWs. A significant association was seen between symptom status and hydroxychloroquine (HCQ) chemoprophylaxis (P = 0.014). Those who took HCQ partially or did not take were more likely to be symptomatic than those who completed the full course. Most of the HCWs (86.7%) gave no history of comorbidity, and among the rest, hypertension (10%) was most common, followed by diabetes (8.2%), bronchial asthma, and allergy (7.5%). Duration of hospital stay was longer among HCWs who had one or the other comorbidity (P = 0.01). Other factors such as age, sex, clinical presentation, and HCQ prophylaxis were not significantly associated with the duration of hospital stay (all P > 0.05). Other clinical details are given in Table 2.
Table 2.
Clinico-epidemiological profile of isolated health-care workers
| Clinico-epidemiological profile of isolated HCWs (n=744) | n (%) |
|---|---|
| Source of infection | |
| Definitive contact with positive person (HCW/family/friend) | 386 (51.88) |
| Workplace: Breach in PPE in COVID ward | 258 (34.7) |
| Workplace: Non-COVID wards | 27 (3.6) |
| Travel from home to hospital (public transport) | 18 (2.4) |
| Social gatherings | 3 (0.4) |
| Unknown | 238 (32.0) |
| Clinical presentation | |
| Symptomatic | 606 (81.45) |
| Asymptomatic | 138 (18.54) |
| Severity of the infection | |
| Mild | 422 (56.72) |
| Moderate | 265 (35.61) |
| Severe | 57 (2 deaths) (7.66) |
| HCQ chemoprophylaxis | |
| Completely taken (7 weeks) | 238 (32.0) |
| Not taken/partially taken | 506 (68.0) |
| Comorbidities | |
| Yes | 99 (13.3) |
| No | 645 (86.7) |
| Isolation | |
| Home | 106 (14.25) |
| Institutional | 638 (85.75) |
| Interval between test results and admission/isolation (h) | |
| Within 24 | 631 (84.8) |
| More than 24 | 113 (15.2) |
| Discharge from isolation (days) | |
| ≤10 | 392 (52.7) |
| >10 | 352 (47.3) |
| Throat swab at discharge | |
| Negative | 632 (84.95) |
| Not done | 112 (15.05) |
HCWs: Health-care workers, HCQ: Hydroxychloroquine
DISCUSSION
Studies have shown that frontline HCWs have at least a threefold increased risk of COVID-19 infection compared to the general community.[2,3] They can be at greater risk to their co-workers, family, and patients being treated by them. Hence, institutional CT serves as an important pillar of control of transmission. CT includes identification of positive cases, contact identification, categorization into HR and LR status, and quarantine of these contacts as per guidelines by the Ministry of Health and Family Welfare.[4]
CT activity began on April 9, 2020. The trend in isolation shows that the highest number of cases was detected in the month of May and June 2020, after which the positive cases started decreasing from the month of July onward. However, the quarantine trend shows a decrease after the month of April 2020. On risk stratification, 60.49% were HR contacts and 17.29% were LR contacts. The highest number of contacts that had to be quarantined against one HCW was 63 in the month of April. However, such incidences were never reported again. All of them reported to work after 14 days of quarantine period and one negative swab at the end of quarantine. The overall ratio between isolated and quarantined HCWs was 1:2. An adequate number of HCWs are crucial to maintain patient care during the ongoing COVID-19 pandemic. Therefore, it is important to take into consideration the manpower, patient safety, and medicolegal issues, along with “breaking the chain of transmission.” Institutional CT can be tricky as blindly quarantining contacts of a case will increase the workload of the remaining staff, but, at the same time, care should be taken that no probable contact is left from being quarantined. As a part of institutional policy, and to maintain adequate manpower, quarantine was reduced to 7 days with mandatory testing before resuming work. They were further required to self-monitor for 7 days while continuing duties and following COVID-appropriate behavior (CAB). However, none of the contacts tested positive or developed any symptoms during the period of self-monitoring. About 88 HCWs tested positive from quarantine, of which majority were HR contacts. The HR exposures identified were sharing the same room and having food together where there is a chance of direct conversations without face masks. The test positivity rate among HR and LR contacts was 9.01% and 2.72%, respectively. This is the true success of CT. Few other institutes have also reported successful implementation of CT. Prasad Sahoo et al. reported that out of 3411 HCWs were exposed, 26.1% were HR contacts and 73.9% were LR. Their test positivity rate for HR and LR contact was 3.82% and 1.90%, respectively. There was a gradual decline in the number of HR contacts over time.[5] Kaur et al. reported a test positivity rate of 7.1% among HR contacts and an overall positivity rate of 3.1%.[6]
The CT team actively raised awareness regarding CAB at workplace and reinforced it from time to time. The evolving pandemic and training sessions conducted by the hospital also raised awareness among HCWs. These factors may be the reason for decreased contacts after the initial month. Similar findings are reported by Prasad Sahoo et al. too.[5]
Majority of the HCWs affected from COVID-19 were resident doctors, interns, and nursing staff. About 70% of the HCWs who were isolated/quarantined belonged to below 40 years of age. This could be because young faculty/residents and interns were doing duties in the COVID wards and senior faculties were performing routine non-COVID work. The nursing staff was also involved in direct patient care in COVID wards. A similar pattern is observed in the quarantine trend also. Apart from the nature of work, sharing the same residential quarters is another reason for increased quarantine among resident doctors, interns, and in-house nursing staff. About 37% of the isolated HCWs and 42% of the quarantined HCWs were residing on the campus. These figures helped in identifying the in-campus hotspots and facilitated timely tracing of contacts and for performing sanitization activities of the premises. Arrangements were made for institutional isolation as well as for quarantine for these HCWs. Even though majority of the infections of COVID-19 in the HCWs were mild in nature, a higher number of hospital admissions is due to the nonsuitability of living conditions for home isolation. A separate isolation ward was created for HCWs with mild disease and no facility for home isolation. Institutional quarantine was facilitated in collaboration with the Public Health Department. In the study by Kaur et al., the largest proportion of HCWs affected was hospital attendants and sanitation workers (35.3%), followed by nurses (17.2%), security personnel (13.3%), and doctors (12.2%). Informal workplace interactions such as having tea and lunch together and not maintaining enough physical distance were the most common reason for positivity.[6] Even Mahajan et al. reported the highest prevalence among security personnel (24.5%), followed by nursing staff (14%) and doctors (12.6%).
An attempt was made through the history obtained from positive HCWs to understand the likely source of infection. The most common probable source of infection among HCWs was definitive history of contact with a positive person (51.88%), followed by a breach in personal protective equipment in COVID wards (34.7%), exposure to unknown COVID-positive patients in non-COVID wards (3.6%), travel (2.4%), and social gatherings (0.4%). About 46% of the HCWs gave a history of definitive contact with another positive HCW. HCW-to-HCW transmission is a critical factor in the spread of SARS-CoV-2 which is often underestimated.[7]
The data of CT also gave insights into clinical profile of the COVID-19 infection among HCWs. More than 81% of the HCWs were symptomatic. Around 32% of them reported multiple symptoms. The most common symptoms were fever, cough, sore throat, and rhinitis. Nonspecific symptoms such as headache, myalgia, and diarrhea were also reported. Those who took HCQ partially or did not take were more likely to be symptomatic than those who completed the full course. Full course of HCQ prophylaxis has shown some benefit in reducing symptoms.[8] Majority of the HCWs gave no history of comorbidity. Comorbidities reported were hypertension (10%), diabetes (8.2%), bronchial asthma, and allergy (7.5%). Duration of hospital stay was found to be longer among HCWs who had one or the other comorbidity (P = 0.01). Other factors such as age, sex, clinical presentation, and HCQ prophylaxis were not significantly associated with duration of hospital stay (all P > 0.05). Mahajan et al. reported a similar clinical profile of HCWs infected with COVID-19 in another tertiary care hospital in Mumbai.[9]
The conduct of CT came with its share of challenges too. Decision making for the exact duration of quarantine while maintain an adequate workforce, enforcement of CAB, reliability of history either to get quarantined unnecessarily or to avoid getting quarantined, even though necessary, are some of them. Certain unanswered question remains regarding quarantine amongst recently recovered / antibody-positive individuals getting exposed to Covid-19 person or quarantine among low risk exposed vaccinated individuals. Certain unanswered question remains regarding quarantine among recently recovered/antibody-positive individuals getting exposed to COVID-19 person or quarantine among LR exposed vaccinated individuals.
CONCLUSION
Effective CT of positive HCWs greatly aids in the early identification of contacts and timely quarantine which is necessary for breaking the chain of transmission. The test positivity rate among HR and LR contacts was 9.01% and 2.72% respectively. Over a period of time number of HCWs getting isolated or quarantined is found to decrease. This strategy can be implemented among other medical colleges and hospitals too.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Dr. Hemant Deshmukh, Dean, Seth G S Medical College and KEM Hospital, Parel, Mumbai
Public Health Department, Municipal Corporation of Greater Mumbai.
REFERENCES
- 1.Interim Guidance on Developing a COVID-19 Case Investigation &Contact Tracing Plan:Overview |CDC. CDC; 2021. [Last accessed on 2021 Jun 03]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/overview.html .
- 2.Zheng C, Hafezi-Bakhtiari N, Cooper V, Davidson H, Habibi M, Riley P, et al. Characteristics and transmission dynamics of COVID-19 in healthcare workers at a London teaching hospital. J Hosp Infect. 2020;106:325–9. doi: 10.1016/j.jhin.2020.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, et al. Risk of COVID-19 among front-line health-care workers and the general community:A prospective cohort study. Lancet Public Health. 2020;5:e475–83. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guidelines on Preventive Measures to Contain Spread of COVID-19 in Workplace Settings |Government of India, Ministry of Health &Family Welfare, Directorate General of Health Services. New Delhi; 2020. [Last accessed on 2021 Jun 04]. Available form: https://www.mohfw.gov.in/pdf/Guidelinesonpreventivemeasurestocontainspread ofCOVID19inworkplacesettings.pdf .
- 5.Prasad Sahoo D, Kumar Singh, Prasad Sahu D, Pradhan S, Kumar Patro B, Batmanabane G, et al. Hospital-Based Contact Tracing of Patients With COVID-19 and Health Care Workers During the COVID-19 Pandemic in Eastern India:Cross-sectional Study. JMIR Form Res. 2021;5:e28519. doi: 10.2196/28519. doi:10.2196/28519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaur R, Kant S, Bairwa M, Kumar A, Dhakad S, Dwarakanathan V, et al. Risk stratification as a tool to rationalize quarantine of health care workers exposed to COVID-19 cases:Evidence from a tertiary health care center in India. Asia Pac J Public Heal. 2021;33:134–7. doi: 10.1177/1010539520977310. [DOI] [PubMed] [Google Scholar]
- 7.Schneider S, Piening B, Nouri-Pasovsky PA, Krüger AC, Gastmeier P, Aghdassi SJ. SARS-coronavirus-2 cases in healthcare workers may not regularly originate from patient care:Lessons from a university hospital on the underestimated risk of healthcare worker to healthcare worker transmission. Antimicrob Resist Infect Control. 2020;9:1–7. doi: 10.1186/s13756-020-00848-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhattacharya R, Chowdhury S, Nandi A, Mukherjee R, Kulshrestha M, Ghosh R, et al. Pre-exposure hydroxychloroquine prophylaxis for COVID-19 in healthcare workers:a retrospective cohort. Int J Res Med Sci. 2021;9:89–96. [Google Scholar]
- 9.Mahajan N, Mathe A, Patokar G, Bahirat S, Lokhande P, Rakh V, et al. Prevalence and Clinical Presentation of COVID-19 among Healthcare Workers at a Dedicated Hospital in India. [Last accessed on 2021 Jun 04];J Assoc Physicians India [Internet] 2020 68:1621. Available from: https://pubmed.ncbi.nlm.nih.gov/33247637/ [PubMed] [Google Scholar]


