Abstract
As a promising source of biologically active substances, the Artemisia species from Kazakhstan have not been investigated efficiently. Considering the rich history, medicinal values, and availability of the Artemisia plants, systematic investigations of two Artemisia species growing in the East Kazakhstan region were conducted. In this study, one new germacrane-type sesquiterpene lactone (11), together with 10 known sesquiterpenes and its dimer, were characterized from A. nitrosa Weber. Additionally, one new chromene derivative (1’) with another 12 known compounds, including coumarins, sesquiterpene diketones, phenyl propanoids, polyacetylenics, dihydroxycinnamic acid derivatives, fatty acids, naphthalene derivatives, flavones, and caffeic acid derivatives were isolated from A. marschalliana Spreng. All compounds were isolated and identified for the first time from these two Artemisia species. The structures of new compounds (11, 1’) were established by using UV, TOFMS, LC–MS, 1D and 2D NMR spectroscopic analyses. The cytotoxicity of all isolated compounds was evaluated. As a result, all compounds did not show significant inhibition against HL-60 and A-549 cell lines. The sesquiterpenoids isolated from A. nitrosa were tested for their inhibitory activity against the LPS-induced NO release from the RAW624.7 cells, and neither of them exhibited significant activity.
Keywords: Artemisia nitrosa, Artemisia marschalliana, sesquiterpene lactone, coumarin, flavonoid, phenolic compound, cytotoxicity, HL-60, A-549
1. Introduction
The Artemisia species are perennial high-vascular plants and have been used for centuries in traditional medicine [1]. The medicinal benefits of the Artemisia genus include normalizing the work of the gastrointestinal tract, especially in gastritis with low acidity, increasing appetite [2,3,4], and treating bronchial asthma [5], rheumatism [6], dermatitis [7,8], malaria [9], etc. Moreover, a few scientific publications reported that some natural Artemisia drugs showed promising potential to cure diseases, such as AIDS, cancer, cardiovascular diseases, and renal disorders [10,11,12]. Extensive research has resulted in the isolation of a number of bioactive secondary metabolites, such as essential oils, flavonoids, terpenes, esters, and phenolic [13,14]. Many compounds from the genus showed antimalarial, antiviral, anticancer, antipyretic, antihemorrhagic, anticoagulant, antianginal, antioxidant, antiulcer, and antispasmodic properties [1,15,16,17].
Artemisia is one of the largest genera in the Asteraceae family, encompassing more than 400 species, and is widely distributed all over the world [18,19]. The most significant number of species are found in Russia and China and, in Kazakhstan, 81 species were documented, with 19 being endemic, and 34 growing in the territory of Central Kazakhstan [20,21]. As is well known, plants of the Artemisia species have a history of manufacturing potentially cytotoxic substances. For instance, the Central Asian oncology clinics use a sesquiterpene lactone named arglabin, derived from the A. glabella plant growing in Central Kazakhstan, to treat various cancers [22]. ]. The pharmacologically active flavone eupatrilin, which was isolated from A. asiatica, has cytotoxic and chemopreventive properties [23]. Our previous work on the endemic A. heptaptamica in the Almaty region of Kazakhstan revealed 13 sesquiterpene lactones, most of which showed potent inhibition against the activation of NF-kB induced by LPS [24].
Another recent study of our group has revealed that methanolic extracts of a total of nine Artemisia species from Central Asia showed a high potential for α-glucosidase, PTP1B, antioxidant, and BNA inhibition, which are associated with diabetes, obesity, and bacterial infections. Of these, both A. nitrosa and A. marschalliana exhibited a PTP1B inhibition around 75% at a concentration of 50 µg/mL. Similarly, both Artemisia species also showed the highest activities (>85%) against BNA even at lower concentration of 20 µg/mL [21].
Artemisia nitrosa Weber is native to saline desert-steppe landscapes of Kazakhstan, southern Siberia, and Mongolia, with secondary distribution in Transbaikalia [25]. However, A. nitrosa is a poorly studied plant. Secondary metabolites of A. nitrosa, such as sesquiterpene lactones and dimers, are being isolated and identified for the first time by our research team.
Artemisia marshalliana Spreng is found in steppe meadows, steppes, and pine forests throughout the Far East, Siberia, the Caucasus, and Kazakhstan [20]. It is an Iranian traditional medicinal plant whose extracts showed antibacterial and anticancer properties in human gastric carcinoma (AGS) and L929 cell lines, while the essential oil has antimalarial properties [26,27].
This study aimed to phytochemically investigate non-explored Artemisia species in Kazakhstan, and resulted in the characterization of germacrene-type sesquiterpene lactones from A. nitrosa and phenolic compounds from A. marschalliana, including a total of 2 new and 23 known compounds for the first time. Their structures have been established using extensive analyses of UV, MS, 1D, and 2D NMR spectroscopic data. All compounds were evaluated for cytotoxicity against human cancer cell lines HL-60 and A-549.
2. Materials and Methods
2.1. General Experimental Procedures
To distinguish a certain substance, the combination of NMR (1D and 2D) analytical techniques with other experimental methods, such as LC–MS, UV, IR, preparative HPLC, and semi-preparative HPLC were used. A Shimadzu UV-2550 UV–vis spectrophotometer is used for the measurement of UV spectra. The IR spectra are registered on a Thermo Nicolet FTIR IS 5 spectrophotometer. The HR-ESIMS spectra were measured on a Waters Synapt G2-Si Q-TOF instrument with a Waters BEH C18 column (1.7 μm, 2.1 mm× 50 mm, CH3CN:H2O with 0.1% formic acid, from 5% to 95%, 0–9 min, flow rate 0.4 mL/min, 45 °C). Analytical HPLC was performed on a Waters e2695 system equipped with a Waters 2998 photodiode array detector (PDA), a Waters 2424 evaporative light-scattering detector (ELSD), and a Waters 3100 MS detector, using a Waters Sunfire RP C18 column (5 μm, 4.6 mm × 150 mm, CH3CN:H2O with 0.1% formic acid, from 5% to 95%, 0–25 min, flow rate 1.0 mL/min, 30 °C). Preparative HPLC was run on a Waters system equipped with a Waters 2767 autosampler, a Waters 2545 pump, a Waters 2489 PDA and an Acuity ELSD using a Waters Sunfire RP C18 column (5 μm, 30 mm × 150 mm, flow rate 30 mL/min).
The NMR spectra were recorded on a Bruker Avance III (Bruker, Zurich, Switzerland) using a 500 M NMR spectrometer with TMS as the internal standard. The chemical shift (δ) values were given in ppm and coupling constants (J) in Hz. All solvents used for CC were of at least analytical grade (Shanghai Chemical Reagents Co., Ltd., Shanghai, China), and solvents used for HPLC were of HPLC grade (Merck KGaA, Darmstadt, Germany).
Column chromatography (CC) was performed on MCI gel CHP20P (75−150 μm, Mitsubishi Chemical Industries, Tokyo, Japan), Econosep C18 60A (50 μm, DIKMA, Beijing, China), Sephadex LH-20 (Pharmacia Biotech AB, Uppsala, Sweden), and silica gel (100−200 and 300−400 mesh, Qingdao Haiyang Chemical Co., Ltd., Qingdao, China). The TLC was carried out on precoated silica gel 60 F254 aluminum sheets (Merck, Darmstadt, Germany), and the TLC spots were viewed at 254 nm and visualized using 5% sulfuric acid in alcohol containing 10 mg/mL of vanillin.
2.2. Plant Materials
Here, A. nitrosa and A. marschalliana were gathered from East Kazakhstan at the end of July 2020 and identified by experts of the Republican State Enterprise on the subject of economic management at the “Institute of Botany and Phytointroduction” of the Committee of Forestry and Wildlife of the Ministry of Ecology, Geology, and Natural Resources of the Republic of Kazakhstan. A sample of A. nitrosa (No. ANI-07) and a sample of A. marschalliana (AMA-07) were deposited in the herbarium of the Research Center for Medicinal Plants, Faculty of Chemistry and Chemical Technology, Al-Farabi Kazakh National University, Almaty, Kazakhstan (Figures S31 and S32). The air-dried whole plants of A. nitrosa (14 kg) and A. marschalliana (13 Kg) were cut into small pieces and stored at room temperature.
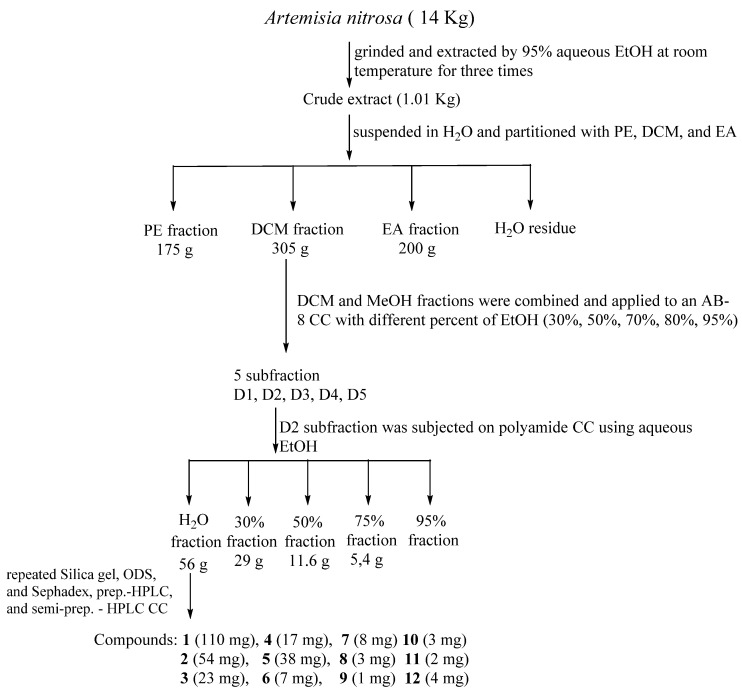
2.3. Extraction and Isolation of A. nitrosa
The air-dried whole plants of A. nitrosa (14 kg) were ground and extracted by 95% aqueous EtOH at room temperature three times (three days each). The EtOH extract was dried with evaporation under reduced pressure. The residue was suspended in H2O and partitioned with petroleum ether (PE), CHCl3, and EtOAc (EA), successively (Figure 1). The CHCl3 fraction (355 g) was subjected to an AB-8 column chromatography (CC), eluted with aqueous EtOH in a gradient manner (30, 50, 70, 80, and 95%), obtaining fractions 1–6. Fraction 2 of 50% of EtOH (110 g) was applied to a polyamide column using H2O, 30, 50, 70, 95% of EtOH/H2O (v/v) as an eluent. The water fraction (56 g) was further fractionated over a Sephadex LH-20 column eluted with CHCl3–MeOH (1:1) to give five fractions (A1–A5). Subfraction A4 was subjected to CC on a ODS medium pressure column eluted with MeOH (through a gradient from 35 to 100% aqueous MeOH) to obtain A4A–A4H + J subfractions. The subfraction A4E (3.9 g) was passed through the silica gel column using a solvent mixture of CHCl3:MeOH (from 100:1 to 1:1) to give subfractions A4E1–A4E10. Further purification of subtraction A4E was performed by repeated CC over silica gel, giving seven pure compounds, as follows: 1 (110 mg), 2 (54 mg), 3 (23 mg), 4 (17 mg), 5 (38 mg), 6 (7 mg), and 7 (8 mg). Subfraction A4F (602 mg) was purified first by CC over silica gel, and then preparative HPLC (with a gradient of CH3CN/H2O) to obtain compounds 8 (3 mg) and 11 (2 mg). In a similar way, subfraction A4C (667 mg) was treated and finally purified by semi-preparative HPLC using CH3CN/H2O (15 min, from 50% to 75%, flow rate 3.0 mL/min) to obtain compound 12 (4 mg). Subfraction A4D (3.2 g) was applied to a silica gel column eluted with different solvent systems (CHCl3:acetone, and CHCl3:MeOH in a ratio of 100:1 to 10:1) to obtain compounds 9 (1 mg) and 10 (3 mg) (Figure 1).
Figure 1.
Isolation scheme of A. nitrosa.
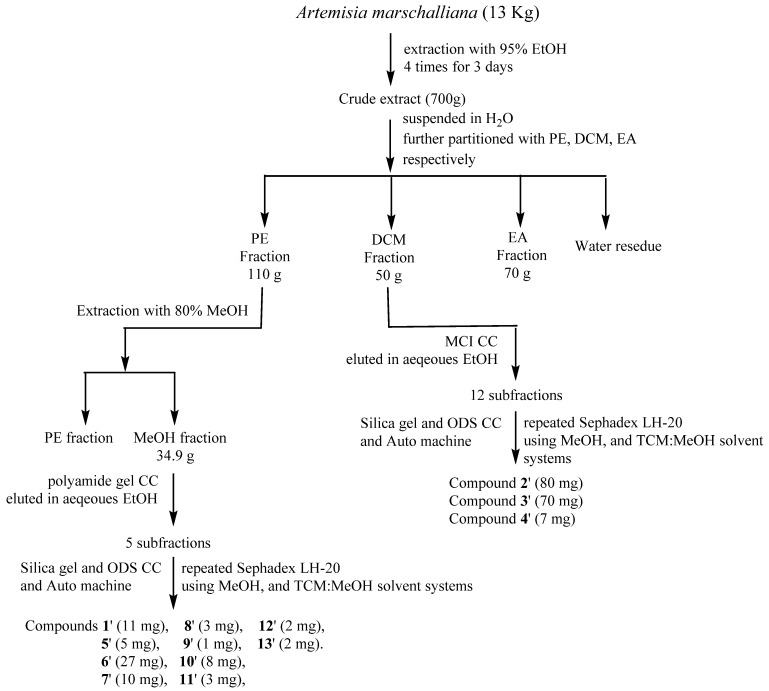
2.4. Extraction and Isolation of A. marschalliana
The air-dried whole plants of A. marschalliana (13 kg) were powdered and extracted by 95% aqueous EtOH at room temperature three times (3 day each). The EtOH extract was dried with evaporation under reduced pressure. The residue was suspended in water and partitioned with petroleum ether (PE), CHCl3, and EA, respectively (Figure 2). The obtained CHCl3 fraction (50 g) was applied to a silica gel column (200–300 mesh) eluted with aqueous EtOH (in a gradient manner from 20% to 95%) to obtain 12 subfractions. The subfractions 7 and 8 (3.579 g) were subjected to CC over Sephadex LH-20 using MeOH as mobile phase, giving five subfractions (7 and 8A to 7 and 8E). Fraction 4 (890 mg) was further applied to CC over silica gel (200–300 mesh) eluting with a gradient solvent system of PE/EtOAc to give compound 1’ (11 mg). Subfraction 5 (602 mg) was passed through a column of silica gel (200–300 mesh, PE/EtOAc) to give subfractions 5A–5H. Subsequently, subfraction 5F was purified by preparative HPLC using CH3CN/H2O to yield compound 2’ (80 mg). Fraction 10 (2.49 g) was subjected to CC over ODS using aqueous MeOH to yield 13 subfractions (Fr10A–Fr10M). Furthermore, subfraction 10J was subjected to CC over Sephadex LH-20 to obtain compound 3’ (70 mg). The obtained PE fraction (110 g) was further extracted with 80% aqueous MeOH (34.3 g), which was applied to a polyamide gel column eluted with aqueous EtOH in a gradient manner (20%, 40%, to 95%) to obtain five subfractions (A-E). Subfraction B (3.5 g) was further applied to silica gel CC eluting through a gradient with a solvent mixture of PE/EtOAc (10:1, 1:1, 0:1) to give 10 subfractions (B1–B10). Subfraction B8 (933 mg) was passed through a column of Sephadex LH-20 (eluted with MeOH), giving four subfractions (A to D). Subfraction B8D (460 mg) was applied to CC over ODS (aqueous MeOH, from 98:2 (v/v) to 25:75 (v/v)) to obtain subfractions B8D1–B8D5. Subsequently, fraction B8D2 was purified by silica gel CC using a gradient solvent system petroleum ether/EtOAc to obtain compound 4’ (7 mg), and then subfractions were subjected to preparative HPLC (CH3CN/H2O) to yield compounds 5’ (5 mg), 6’ (27 mg), 7’ (10 mg), and 8’ (3 mg). Subfraction C was treated first by CC over polyamide, and then applied to CC over Sephadex LH-20 eluting with MeOH, obtaining six subfractions (C1 to C6). Subfraction C6 was purified using silica gel CC (CHCl3/EtOAc), obtaining five fractions (C6A to C6E), and then fraction C6E was applied to an Auto-P machine to obtain compounds 9’ (1 mg), and compound 10’ (8 mg). Subfraction C6C was also applied on an Auto-P machine using CH3CN/H2O as an eluent to obtain compound 11’ (3 mg) and compound 12’ (2 mg). Fraction C5 was subjected on CC over ODS using CH3CN/H2O as an eluent to obtain compound 13’ (2 mg) (Figure 2).
Figure 2.
Isolation scheme of A. marshalliana.
2.5. Cytotoxicity Assay
The cytotoxic effects of A. nitrosa and A. marschalliana were determined using the colorimetric (CCK8) method [28] and the sulforhodamine B (SRB) protein staining method [29]. The CCK8 method was used to detect the growth inhibition of HL-60 cell lines. Cells with a logarithmic growth phase were seeded into a 96-well culture plate at a specific density (90 μL per well); after culturing overnight, different concentrations of drugs were added for 72 h. Three replicate wells were set up for each concentration, which corresponds to concentrations of vehicle control and cell-free zero adjustment wells. Then, 10 μL of CCK-8 was added to each well. After incubating for 2~3 h in the incubator, the SpectraMax 190 microplate reader was used to measure the optical density (OD value) at the 450 nm wavelength.
The compound’s inhibitory effect on the proliferation of A549 cells was detected by the sulforhodamine B (SRB) protein staining method. The specific steps are as fol-lows: A549 cells in the logarithmic growth phase are seeded into a 96-well culture plate at an appropriate density, 90 μL per well; after overnight culture, different con-centrations of compounds (DMSO concentration less than 0.5%) are added for 72 h, each set has three wells for each concentration, and a solvent control group (negative control) is set. After the effect is over, the culture medium is discarded, and 10% (w/v) trichloroacetic acid (100 μL/well) is added; the solution is fixed at 4 °C for 1 h, then washed with distilled water five times, before being dried at room temperature. Then, we added 100μL of SRB solution (4 mg/mL, dissolved in 1% glacial acetic acid), incu-bated it for 15 min at room temperature, rinsed with 1% glacial acetic acid five times to wash away unbound SRB, and added 10 mM Tris solution 100 μL to each well after drying at room temperature, before using a full-wavelength microplate reader Spec-traMax 190 at the 515 nm wavelength to determine the OD value.
The inhibitory rate of the compound on cell proliferation is calculated by the following formula: Inhibition Rate = [1 − (ODcpd − ODuntreated)/(ODLPS − ODuntreated)] ∗ 100%.
2.6. Cell Viability Evaluation
Here, RAW264.7 cells were seeded into 96-well plates at a concentration of 1 × 104 cells per well and allowed to adhere to the bottom of the plate overnight. Then, the cells were treated with different concentrations of compounds for 18 h. The cell viability was determined by MTT assay, as described previously [30]. Then, cell viability was determined by incubation with DMEM containing MTT (1 mg·mL−1) for 4 h, followed by dissolving the formazan crystals with 150 μL DMSO. The absorbance at 540 nm was measured by a SpectraMax M5 microplate reader (Molecular Devices, San Jose, CA, USA).
2.7. Measurement of Nitric Oxide (NO) Production
Here, RAW264.7 cells were seeded into 96-well plates (1 × 104 cells per well) and allowed to adhere for 24 h. The cells were then treated with different concentrations of compounds or vehicles (DMSO) followed by stimulation with 1 μg·mL−1 lipopolysaccharide (LPS, Sigma-Aldrich, St. Louis, MO, USA). The DMSO was used as the vehicle, with the final concentration of DMSO being maintained at 0.1% of all cultures. After 18 h of incubation, the supernatant was collected to determine the NO content using the Griess reagent (Sigma-Aldrich, St. Louis, MO, USA) as described previously [31]. The absorbance at 490 nm was measured by a SpectraMax M5 microplate reader (Molecular Devices, San Jose, CA, USA).
3. Results and Discussion
3.1. Structural Elucidation of Compounds from A. nitrosa
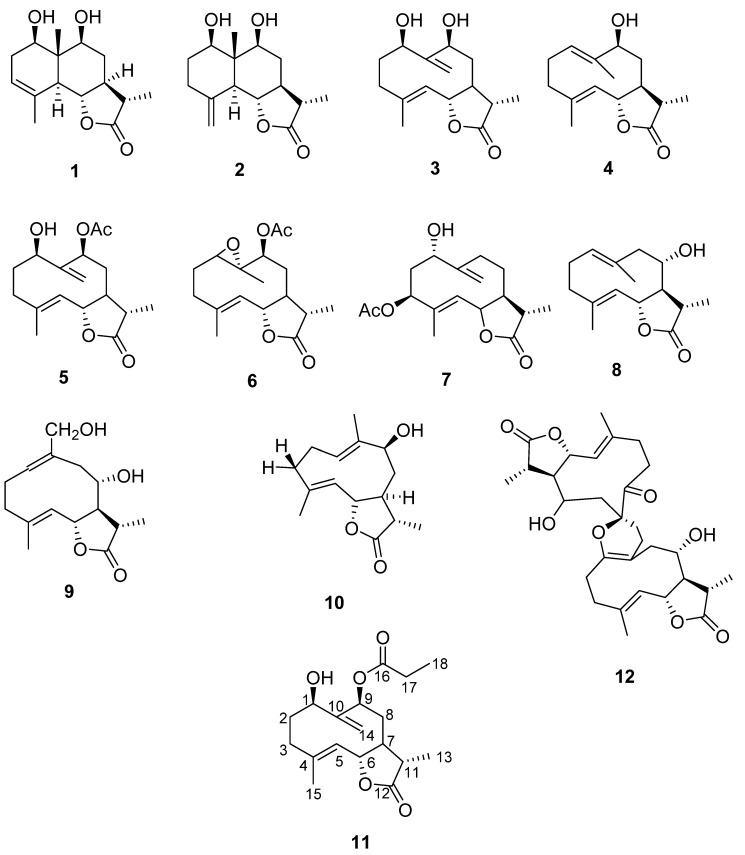
A new germacranolide type sesquiterpene lactone (11), together with 10 known sesquiterpene lactones (1–10) and 1 known dimeric sesquiterpene lactone (12) (Figure 3) were separated from A. nitrosa. After detailed spectroscopic analysis (1D, 2D NMR, LC–MS, TLC) and comparing with the literature data, the known compounds were identified as 1β,9β-Dthydroxyeudesm-3-en-5α,6β,11β-λ2,6-olide (1) [32,33], decahydro-5,6-dihydroxy-3,5α-dimethyl-9-methylenenaphtho[1,2-β]furan-2(3H)-one (2) [34], deacetylherbolide D (3) [32], deacetyl derivative of herbolide A (4) [32],1β-ydroperoxy-9β-acetoxygermacra-4,10(14)-dien-6β,11β-12,6-olide (5) [32], herbolide B (6) [32], 11β,13-dihydroridentin 3-acetate (7) [35], balchanolide (8) [36], 11,13-dihydro germacronolide (9) [37], deacetylherbolide A (10) [38], and artebarrolide (12) [36] (Figure 3, Figures S1–S14, Supplementary information).
Figure 3.
Chemical structures of compounds 1–12 from A. nitrosa.
Compound 11, obtained as a colorless oil, had a molecular formula of C18H26O5 on the basis of UV, ESIMS, TOFMS, LC–MS, and NMR spectroscopic data. The TOFMS showed m/z 322.087 (Figure S13 Supplementary Material); UV (MeOH) λmax (log Ɛ) 256 (2.07) (Figure S12).The 1H NMR spectrum data displayed signals of three methyl groups (δH 1.58 (d, J = 1.3 Hz, 3H), 1.27 (d, J = 6.9 Hz, 3H), and 1.11 (t, J = 7.6 Hz, 3H)), one exocyclic methylene group (δH 4.76, 3.93 each d, J = 10.2 Hz), and a characteristic signal of a double bond (δH 5.13 (dd, J = 10.2, 1.6 Hz, 1H)) (Table 1). The 13C NMR and DEPT NMR spectra indicated 18 carbon resonances, including 3 methyls (δC 17.48, 12.55, 8.53), 5 methylenes (δC 37.54, 36.81, 30.76, 27.64, 114.37), 6 methines (δC 80.05, 78.81, 74.36, 51.05, 41.56, 121.28), and 4 quaternary carbons (δC 177.43, 175.06, 153.51, 145.18) (Table 1). The data suggested that compound 11 might be a germacrane-type of sesquiterpene lactone.
Table 1.
NMR Data for 11 (500 MHz for 1H and 125 MHz for 13C, in CDCl3, δ in ppm, J in Hz).
| Positions | 1H | 13C * |
|---|---|---|
| 1 | 3.93 dt (10.5, 1.4) | 74.8 |
| 2 | 2.18–2.04 m | 31.34 |
| 3 | 2.36–2.21 m | 37.94 |
| 4 | - | 153.51 |
| 5 | 5.13 dd (10.2, 1.6) | 121.28 |
| 6 | 4.34 t (9.8) | 80.05 |
| 7 | 2.36–2.21 m | 41.56 |
| 8 | 1.97–1.80 m | 36.81 |
| 9 | 4.76 dt (10.2, 1.5) | 78.81 |
| 10 | - | 145.18 |
| 11 | 1.97–1.80 m | 51.05 |
| 12 | - | 175.06 |
| 13 | 1.27 d (6.9) | 12.55 |
| 14 | 5.42 d (1.2); 5.34 br s | 114.37 |
| 15 | 1.58 d (1.3) | 17.48 |
| 16 | - | 177.43 |
| 17 | 2.36–2.21 m | 27.64 |
| 18 | 1.11 t (7.6) | 8.53 |
* The assignments were based on HSQC and HMBC data.
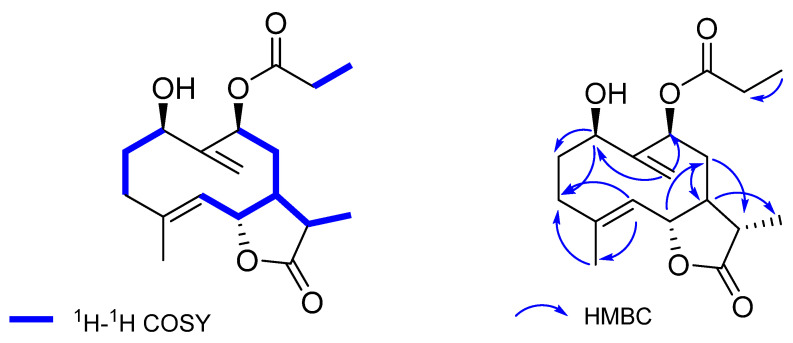
A comparison of NMR data of 11 and the known compound 1β-hydroperoxy-9β-acetoxygermacra-4,10(14)-dien-6β,11β-12,6-olide (5), reported from A. herba-alba [32,33] and also obtained in this study, revealed high similarities between these two compounds, except for an extra methyl group (δH 1.11, m; δC 8.53) (Table 1) present in compound 11. Detailed analysis of the 2D NMR data of 11 further established the structure. The 1H-1H COSY correlations of H-1/H-2/H-3, H-5/H-6/H-7/H-8/H-9, H-7/H-11/H-13, and H-17/H-18 revealed the existence of four segments as shown (Figure 4). The key HMBC correlations from H-1 to C-2 and C-3, H-5 to C-3 and C-15, H-6 to C-8, H-7 to C-13, H-8 to C-7 and C-11, H-14 to C-1, C-9, and H-18 to C-17 further constructed the planar structure of 11, with a propionyloxy group attached to C-9 (Figure 4). The relative configuration of 11 was inferred as the same with that of the known compound 5 by the similar chemical shifts and the similar coupling constants of H-1, H-6, H-9, and H-13 between these two compounds. Therefore, the structure of 11 was fully established, and named 1β-hydroperoxy-9β-propionoxygermacra-4, 10(14)-dien-6β,11β-12,6-olide (11).
Figure 4.
1H-1H COSY and key HMBC correlations (H→C) of compound 11.
Compounds 1–10 and 12 have already been isolated and described from other Artemisia species, such as A. herba-alba, A. barrelieri, and A. gypsacea. Artebarrolide (12), which is the first dimeric germacranolide described from A. barrelieri [36], was discovered for the second time in this investigation.
3.2. Structural Elucidation of Compounds from A. marschalliana
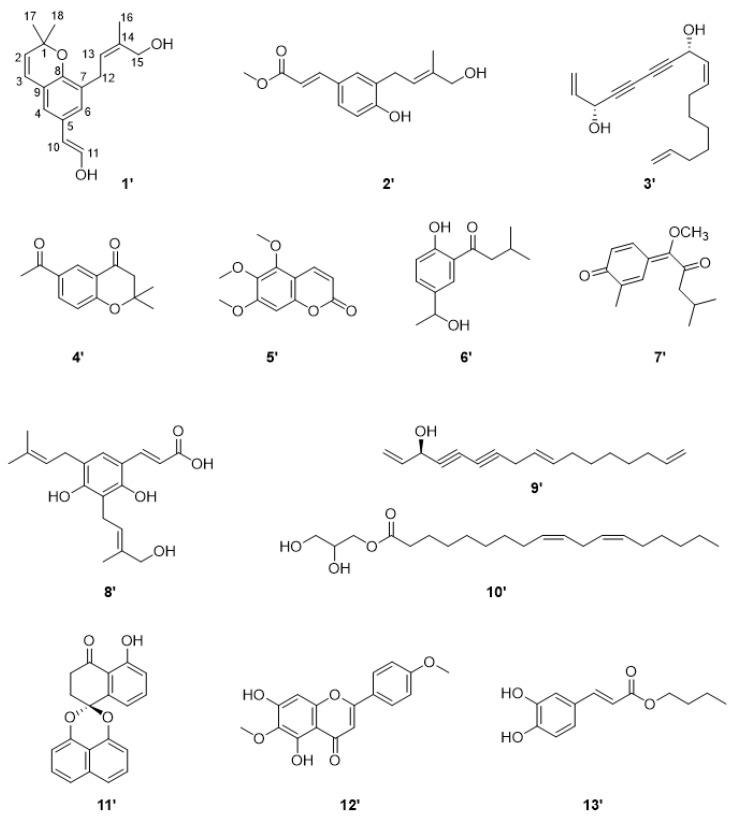
A total of 13 compounds were isolated and identified from the whole plant of A. marschalliana that grows in Kazakhstan, including coumarins, sesquiterpene diketone, phenylpropanoid, benzopuran derivative, polyacetylenic compounds, fatty acids, naphthalene derivative, flavone, and caffeic acid derivative (Figure 5). By extensive spectroscopic analysis of MS, 1H, and 13C NMR data, and comparison with previously reported data, the structures of known compounds were identified as 1 new 2,2-dimethyl-8-(19-hydroxy)prenyl-6-(12-hydroxy) vinylchromene (1’) [39], together with 12 known compounds, namely a methyl 3-(4′-hydroxyprenyl)-7Z-coumarate (2’) [40], arteordoyn A (3’) [41,42], 6-acetyl-2,2-dimethylchroman-4-one (4’) [43], 5,6,7-trimethoxycoumarin (5’) [41], 2-isovaleroyl-4[1-hydroxyethyl]-phenol (6’) [44], guayulone (7’) [45], diprenylated-dihydroxycinnamic acid (8’) [46], dehydrofalcarinol (9’) [44], 9,12-Octadecadienoic acid (9Z,12Z)-,(2R)-2,3-dihydroxypropyl ester (10’) [47], palmarumycin CP 2 (11’) [48], 5,7-dihydroxy-6,4’-dimethoxyflavone (12’) [49], and propyl caffeate (13’) [50] (Figure 5, Figures S15–S29, Supplementary information).
Figure 5.
Chemical structures of compounds 1’–13’ of A. marschalliana.
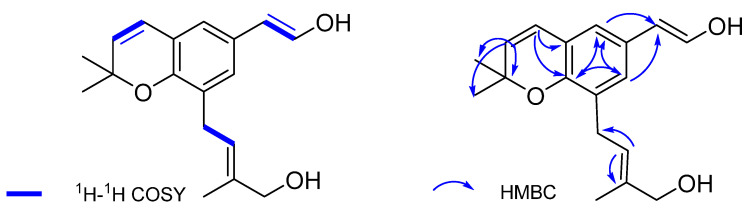
Compound 1’, obtained as a colorless oil, had the molecular formula of C18H22O3 on the basis analysis of ESIMS and 13C NMR data. The UV spectrum showed maximal absorptions at 239, 274, and 318 nm (Figure S16), indicative of the presence of a conjugated aromatic ring. The 1H NMR spectrum showed signals of three methyls (δH 1.72 (s, 3H), 1.36 (s, 6H)), two characteristic signals of a double bond (δH 5.48 (s, 1H); 6.22 (t, J = 13.6 Hz, 2H), and a benzol ring. The 13C and DEPT NMR spectra (Table 2) displayed 18 carbon resonances ascribed to 3 methyls (δC 27.80, 27.80, 13.37), 2 methylenes (δC 27.29, 68.33), 7 methines (δC 146.10, 130.60, 129.44, 128.41, 124.09, 123.08, 121.53, 113.92), and 6 quaternary carbons (δC 171.21, 152.67, 135.27, 120.60, 125.98, 76.66) (Table 2). The HMBC spectrum revealed H-2 (5.57 (d, J = 9.8 Hz, 1H)) correlated to C-1, C-17, C-18; H-3 (6.22 (t, J = 13.6 Hz, 2H)) to C-8, C-9; correlation in benzoyl ring; moreover H-4 (7.10 (s, 1H)) to C-10; H-6 (6.96 (s, 1H)) to C-10; H-13 (5.48 (s, 1H)) to C-12 and C-14 (Figure 6).
Table 2.
NMR Data for 1’ (500 MHz for 1H and 125 MHz for 13C, in CDCl3, δ in ppm, J in Hz).
| Positions | 1H | 13C * |
|---|---|---|
| 1 | - | 76.63 |
| 2 | 5.57 (d, J = 9.8 Hz, 1H) | 130.60 |
| 3 | 6.22 (t, J = 13.6 Hz, 2H) | 121.53 |
| 4 | 7.10 (s, 1H) | 129.44 |
| 5 | - | 128.41 |
| 6 | 6.96 (s, 1H) | 123.08 |
| 7 | - | 135.27 |
| 8 | - | 152.67 |
| 9 | - | 120.60 |
| 10 | 6.22 (t, J = 13.6 Hz, 2H) | 113.92 |
| 11 | 7.58 (d, J = 15.6 Hz, 1H) | 146.23 |
| 12 | 3.25 (d, J = 7.2 Hz, 2H) | 27.29 |
| 13 | 5.48 (s, 1H) | 124.09 |
| 14 | - | 125.98 |
| 15 | 3.98 (s, 2H) | 68.33 |
| 16 | 1.72 (s, 3H) | 13.37 |
| 17 | 1.36 (s, 6H) | 27.80 |
| 18 | 1.36 (s, 6H) | 27.80 |
* The assignments were based on HSQC and HMBC data.
Figure 6.
1H-1H COSY and key HMBC correlations (H→C) of compound 1’.
The 1H-1H COSY correlations revealed the relations between H-2 to H-3, H-10 to H-11 and H-12 to H-13 (Figure 6). A comparison of compound 1’ with the known compound 2, 2-dimethyl-8-prenyl-6-vinylchromene showed the presence of two hydroxyl groups located at C-12 and C-19 (δH 6.22, t; δC 114; δH 3.98, s; δC 68.22) [39]. Accordingly, the full structure of 1’ was proposed and named 2,2-dimethyl-8-(19-hydroxy)prenyl-6-(12-hydroxy) vinylchromene.
Earlier phytochemical studies on A. marschalliana harvested in the Iranian prov-ince of East Azerbaijan led to the isolation and identification of a high concentration of oxygenated sesquiterpenes [26,27], which is surprising due to fewer plants growing in Kazakhstan containing sesquiterpenoid compounds.
3.3. Cytotoxicity Activity
The separated compounds of A. nitrosa and A. marschalliana were examined for their cytotoxicity against human myeloid leukemia HL-60 cells and A-549 human lung cancer cell lines by the CCK8 and the sulforhodamine B (SRB) protein staining methods, respectively. The results (Table 3 and Table 4) showed that monomeric sesquiterpene lactones from A. nitrosa showed weak cytotoxic activities against both A-549 and HL-60 cell lines, while the compounds from A. marschalliana did not show any effect on the growth of A-549 and HL-60 cell lines (Table 3 and Table 4).
Table 3.
Cytotoxic activities of isolated compounds from A. nitrosa and A. marschalliana against the A-549 cell line.
| Compounds of A. nitrosa |
Inhibition against A-549 (%) | Compounds A. marschallina |
Inhibition against A-549 (%) | ||
|---|---|---|---|---|---|
| 25 μM | 1 μM | 20 Μm | 2 μM | ||
| 2 | 23.7 | 24.8 | 2’ | <1 | <1 |
| 4 | 28.8 | 30.0 | 3’ | <1 | <1 |
| 5 | 8.7 | 21.5 | 4’ | 10.42 | <1 |
| 6 | <1 | <1 | 5’ | 3.07 | <1 |
| 9 | 22.7 | 24.4 | 8’ | <1 | <1 |
| 11 | 4.5 | 4.7 | 10’ | ND a | ND a |
| - | - | - | 12’ | <1 | <1 |
| ADT b | 84.4 | ADT b | 86.1 | ||
a ND indicates not determined. b ADT indicates positive control.
Table 4.
Cytotoxic activities of isolated compounds from A. nitrosa and A. marschalliana against the HL-60 cell line.
| Compounds of A. nitrosa |
Inhibition against HL-60 (%) | Compounds A. marschallina |
Inhibition against HL-60 (%) | ||
|---|---|---|---|---|---|
| 25 μM | 1 μM | 20 Μm | 2 μM | ||
| 5 | 8.7 | 21.5 | 4’ | 13.04 | <1 |
| 6 | 18.2 | <1 | 5’ | <1 | <1 |
| 7 | 8.7 | 21.5 | 6’ | 2.12 | <1 |
| 11 | <1 | 1.9 | 10’ | <1 | <1 |
| - | - | - | 12’ | 6.16 | <1 |
| ADT b | 82.5 | ADT b | 84.0 | ||
a ND indicates not determined. b ADT indicates positive control.
3.4. Anti-Inflammatory Activity
The sesquiterpenoids isolated from A. nitrosa were tested for their inhibitory effects against NO production on LPS-stimulated RAW264.7 macrophages. Firstly, the cytotoxicity of compounds 1–11 was evaluated using the MTT assay to determine the toxicity. Most compounds did not show obvious cytotoxicity towards RAW264.7 cells up to 10 μM (Figure S30). Among the isolates, compounds 2, 9, and 11 showed weak NO inhibitory effects at a concentration of 2.5 μM (Figure S30). Dexamethasone (Dex) was used as the positive control.
4. Conclusions
In this work, a phytochemical study of the whole plants of A. nitrosa and A. marschalliana growing in Kazakhstan was carried out for the first time. Twelve compounds were purified from A. nitrosa, including eight germacranolides, two eudesmanolides, one guaianolide, and one sesquiterpene dimer. Among them, compound 11 is a new germacrene-type sesquiterpene lactone. Moreover, a total of 13 compounds were isolated and identified from A. marschalliana, including 1 new chromene derivative (1’), and other known coumarins, sesquiterpene diketone, phenyl propanoid, polyacetylene compounds, fatty acids, naphthalene derivative, flavone, and caffeic acid derivative, respectively. The results revealed the chemical constituents of these two Artemisia plants of Kazakhstan for the first time. Their chemical constituents differed a lot from each other. The characteristic sesquiterpenoids were disclosed from A. nitrosa, while A. marschalliana was rich in other types of structures rather than sesquiterpenoids. It should be pointed out that the previous investigation of A. marschalliana led to the isolation of rich content of oxygenated sesquiterpenes, which suggested a more in-depth investigation for this species. All the known sesquiterpenes (1–10, 12) have been already reported from the Artemisia species, such as A. herba-alba, A. barrelieri, and A. gypsacea. Artebarrolide (12) is the first dimeric germacranolide reported from A. barrelieri, and it was found for the second time in this study. The biological assay of these compounds is rare in previous investigations.
In this study, the cytotoxicity assay of all isolated compounds and the anti-inflammatory assay of the sesquiterpenoids were performed. The results of the cytotoxicity assay showed that none of these compounds showed significant inhibition against A-549 and HL-60 cell lines. The sesquiterpenoids isolated from A. nitrosa did not show significant inhibition on the LPS-induced NO release from RAW-264.7 cells at the concentrations of 10 and 2.5 μM, which closely correlates to the anti-inflammatory activity. Compared with the compounds isolated from A. heptapotamica in the previous study [24], we found that the sesquiterpenoids obtained from A. nitrosa lack the α,β-unsaturated ketone moiety in their structures, which might be pivotal to the anti-inflammatory activity. It is obvious that more in-depth investigations are needed to discover bioactive compounds from the Artemisia species in Kazakhstan.
Acknowledgments
The authors appreciate the support provided by the Ministry of Education and Science of the Republic of Kazakhstan (AP08856717).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/molecules27228074/s1, Supplementary data for Artemisia nitrosa: Figure S1. 1H NMR, 13C NMR, DEPT spectrum of 1 in CDCl3; Figure S2. 1H NMR, 13C NMR, DEPT spectrum of 2 in CD3OD; Figure S3. 1H NMR, 13C NMR, DEPT spectrum of 3 in CDCl3; Figure S4. 1H NMR, 13C NMR, DEPT spectrum of 4 in CDCl3; Figure S5. 1H NMR, 13C NMR, DEPT spectrum of 5 in CDCl3; Figure S6. 1H NMR, 13C NMR, DEPT spectrum of 6 in CDCl3; Figure S7. 1H NMR, 13C NMR, DEPT spectrum of 7 in CDCl3; Figure S8. 1H NMR, 13C NMR, DEPT spectrum of 8 in CDCl3; Figure S9. 1H NMR, 13C NMR, DEPT spectrum of 9 in CD3OD; Figure S10. 1H NMR, 13C NMR, DEPT spectrum of 10 in CDCl3; Figure S11. 1H NMR, 13C NMR, DEPT, HSQC, HMBC and 1H-1H COSY spectra of 11 in CDCl3; Figure S12. UV spectrum of 11 in MeOH. Figure S13. TOFMS spectral analysis of 11. Figure S14. 1H NMR spectrum of 12 in CDCl3. Supplementary data for Artemisia marschalliana: Figure S15. 1H NMR, 13C NMR, DEPT, HSQC, HMBC and 1H-1H COSY spectra of 1’ in CDCl3; Figure S16. UV spectrum of 1’ in MeOH; Figure S17. ESI Mass spectrum of 1’. Figure S18. 1H NMR, 13C NMR, DEPT spectrum of 2’ in Acetone d-6; Figure S19. 1H NMR, 13C NMR, DEPT spectrum of 3’ in CDCl3; Figure S20. 1H NMR, 13C NMR, DEPT spectrum of 4’ in CDCl3; Figure S21. 1H NMR, 13C NMR, DEPT spectrum of 5’ in CDCl3; Figure S22. 1H NMR, 13C NMR, DEPT spectrum of 6’ in CDCl3; Figure S23. 1H NMR, 13C NMR, DEPT spectrum of 7’ in CDCl3; Figure S24. 1H NMR, 13C NMR, DEPT spectrum of 8’ in CDCl3; Figure S25. 1H NMR, 13C NMR, DEPT spectrum of 9’ in CDCl3; Figure S26. 1H NMR, 13C NMR, DEPT spectrum of 10’ in CDCl3; Figure S27. 1H NMR, 13C NMR, DEPT spectrum of 11’ in CDCl3; Figure S28. 1H NMR, 13C NMR, DEPT spectrum of 12’ in CDCl3; Figure S29. 1H NMR, 13C NMR, DEPT spectrum of 13’ in CDCl3. Figure S30. Inhibitory Effects of A. nitrosa compounds on LPS-Enhanced Inflammatory Mediators. Figure S31. Pictures of the whole plant of Artemisia nitrosa. Figure S32. Pictures of the whole plant of Artemisia marschalliana.
Author Contributions
Conceptualization of the manuscript, Y.Y. and J.J.; literature search, isolation and identification A.K., M.A. and C.-Q.K.; determination and drawing of structures, figures, A.N., A.K., U.A. and K.B.; biologically activity assay S.Y.; collection and identification of the plant species J.J. and K.B.; prepared, edited, and reviewed the manuscript, J.J., C.-P.T. and Y.Y. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Sample Availability
Samples of all the isolated compounds are available from the authors.
Funding Statement
This work was supported by the Ministry of Education and Science of the Republic of Kazakhstan (AP08856717).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abad M.J., Bedoya L.M., Bermejo P. In: Essential Oils from the Asteraceae Family Active against Multidrug-Resistant Bacteria. Fighting Multidrug Resistance with Herbal Extracts, Essential Oils and Their Components. Mahendra K.R., Volodymyrivna K.K., editors. Elsevier; Amsterdam, The Netherlands: 2013. pp. 205–221. [DOI] [Google Scholar]
- 2.Zibaee A., Bandani A.R. Effects of Artemisia annua L. (Asteracea) on the digestive enzymatic profiles and the cellular immune reactions of the Sunn pest, Eurygaster integriceps (Heteroptera: Scutellaridae), against Beauveria bassiana. Bull. Entomol. Res. 2010;100:185–196. doi: 10.1017/S0007485309990149. [DOI] [PubMed] [Google Scholar]
- 3.Ivanov M., Uroš G., Dejan S., Kostić M., Mišić D., Soković M. New Evidence for Artemisia absinthium L. Application in Gastrointestinal Ailments: Ethnopharmacology, Antimicrobial Capacity, Cytotoxicity, and Phenolic Profile. Evid.-Based Complement. Altern. Med. 2021;2021:14. doi: 10.1155/2021/9961089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang C., Wang B., Aili M. Effect of Artemisia rupestris L. Extract on Gastrointestinal Hormones and Brain-Gut Peptides in Functional Dyspepsia Rats. Evid.-Based Complement. Altern. Med. 2020;2020:2528617. doi: 10.1155/2020/2528617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zant D., Gubler D.A. The presence of eucalyptol in Artemisia australis validates its use in traditional Hawaiian medicine. Asian Pac. J. Trop. Biomed. 2014;4:520–522. doi: 10.12980/APJTB.4.2014C1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang M., Guo M.Y., Luo Y. Effect of Artemisia annua extract on treating active rheumatoid arthritis: A randomized controlled trial. Chin. J. Integr. Med. 2017;23:496–503. doi: 10.1007/s11655-016-2650-7. [DOI] [PubMed] [Google Scholar]
- 7.Ha H., Lee H., Seo C.S. Artemisia capillaris inhibits atopic dermatitis-like skin lesions in Dermatophagoides farinae-sensitized Nc/Nga mice. BMC Complement. Altern. Med. 2014;14:100. doi: 10.1186/1472-6882-14-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Han H.M., Kim S.J., Kim J.S. Ameliorative effects of Artemisia argyi Folium extract on 2,4-dinitrochlorobenzene-induced atopic dermatitis-like lesions in BALB/c mice. Mol. Med. Rep. 2016;14:3206–3214. doi: 10.3892/mmr.2016.5657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elfawal M.A., Towler M.J., Reich N.G., Golenbock D., Weathers P.J., Rich S.M. Dried whole plant Artemisia annua as an antimalarial therapy. PLoS ONE. 2012;7:e52746. doi: 10.1371/journal.pone.0052746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sajid M., Khan M.R., Shah N.A. Proficiencies of Artemisia scoparia against CCl4 induced DNA damages and renal toxicity in rat. BMC Complement. Altern Med. 2019;16:149. doi: 10.1186/s12906-016-1137-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xia M., Liu D., Liu Y., Liu H. The Therapeutic Effect of Artemisinin and Its Derivatives in Kidney Disease. Front. Pharmacol. 2020;11:380. doi: 10.3389/fphar.2020.00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krishna S., Ganapathi S., Ster I.C. A Randomised, Double Blind, Placebo-Controlled Pilot Study of Oral Artesunate Therapy for Colorectal Cancer. eBioMedicine. 2014;2:82–90. doi: 10.1016/j.ebiom.2014.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abad M.J., Bedoya L.M., Apaza L., Bermejo P. The Artemisia L. Genus: A Review of Bioactive Essential Oils. Molecules. 2012;17:2542–2566. doi: 10.3390/molecules17032542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koul B., Taak P. The Artemisia Genus: A Review on Traditional Uses, Phytochemical Constituents, Pharmacological Properties and Germplasm Conservation. J. Glycom. Lipidom. 2017;7:142–149. doi: 10.4172/2153-0637.1000142. [DOI] [Google Scholar]
- 15.Vallès J., Garcia S., Hidalgo O., Martín J., Pellicer J., Sanz M., Garnatje T. Biology, Genome Evolution, Biotechnological Issues and Research Including Applied Perspectives in Artemisia (Asteraceae) Adv. Bot. Researc. 2011;60:349–419. doi: 10.1016/b978-0-12-385851-1.00015-9. [DOI] [Google Scholar]
- 16.Ferreira M.P., Gendron F., Kindscher K. Bioactive prairie plants and aging adults: Role in health and disease. In: Watson R.R., Preedy V.R., editors. Bioactive Prairie Plants and Aging Adults. Bioactive Food as Dietary Interventions for the Aging Population. Elsevier Inc.; Amsterdam, The Netherlands: 2013. pp. 263–275. [DOI] [Google Scholar]
- 17.Anwar F., Ahmad N., Alkharfy K.M., Gilani A.H. Essential Oils in Food Preservation, Flavor and Safety. Academic Press; Cambridge, MA, USA: 2016. Mugwort (Artemisia vulgaris) Oils; pp. 573–579. [DOI] [Google Scholar]
- 18.Willcox M. Artemisia Species: From Traditional Medicines to Modern Antimalarials—And Back Again. J. Altern. Complement. Med. 2009;15:101–109. doi: 10.1089/acm.2008.0327. [DOI] [PubMed] [Google Scholar]
- 19.Sainz P., Cruz-Estrada Á., Díaz C.E. The genus Artemisia: Distribution and phytochemistry in the Iberian Peninsula and the Canary and Balearic Islands. Phytochem. Rev. 2017;16:1023–1043. doi: 10.1007/s11101-017-9516-2. [DOI] [Google Scholar]
- 20.Plavlov H.V. Flora Kazakhstan. 9th ed. Compositae; Academy of Sciences of the Kazakh SSR; In-t Botany; Almaty, Kazakhstan: 1966. p. 651. [Google Scholar]
- 21.Nurlybekova A., Kudaibergen A., Kazymbetova A., Amangeldi M., Baiseitova A., Ospanov M., Aisa H.A., Ye Y., Ibrahim M.A., Jenis J. Traditional Use, Phytochemical Profiles and Pharmacological Properties of Artemisia Genus from Central Asia. Molecules. 2022;27:5128. doi: 10.3390/molecules27165128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lone S.H., Bhat K.A., Khuroo M.A. Arglabin: From isolation to antitumor evaluation. Chem.-Bio. Interact. 2015;240:180–198. doi: 10.1016/j.cbi.2015.08.015. [DOI] [PubMed] [Google Scholar]
- 23.Seo H.J., Surh Y.J. Eupatilin, a pharmacologically active flavone derived from Artemisia plants, induces apoptosis in human promyelocytic leukemia cells. Mut. Res./Gen. Toxicol. Environmen. Mutagen. 2001;496:191–198. doi: 10.1016/S1383-5718(01)00234-0. [DOI] [PubMed] [Google Scholar]
- 24.Abilova Z., Yuan J., Janar J., Tang C.P., Ye Y. Monomeric and dimeric sesquiterpene lactones from Artemisia heptapotamica. Chin. J. Nat. Med. 2019;17:785–791. doi: 10.1016/S1875-5364(19)30095-0. [DOI] [PubMed] [Google Scholar]
- 25.Namzalov B.B., Namzalov M.B., Zhigzhizhapova S.V. About the new discovery wormwood Artemisia nitrosa web ex STECHM.—Rare species in the flora of Zabaikalya. Vestn. Buryat State Univ. Biol. Geogr. 2018;108:87–92. doi: 10.18101/2587-7143-2018-1-87-92. [DOI] [Google Scholar]
- 26.Asgharian P., Zadehkamand M., Delazar A., Safarzadeh E., Asnaashari S. Chemical composition and some biological activities of Artemisia marschalliana essential oi. Res. J. Pharmacog. 2019;6:71–77. doi: 10.22127/rjp.2019.93527. [DOI] [Google Scholar]
- 27.Salehi S., Mirzaie A., Sadat-Shandiz S.A., Noorbazargan H., Rahimi A., Yarmohammadi S., Ashrafi F. Chemical composition, antioxidant, antibacterial and cytotoxic effects of Artemisia marschalliana Sprengel extract. Nat. Prod. Res. 2013;31:469–472. doi: 10.1080/14786419.2016.1174234. [DOI] [PubMed] [Google Scholar]
- 28.Yang X., Zhong Y., Wang D., Lu Z. A simple colorimetric method for viable bacteria detection based on cell counting kit-8. Anal. Methods. 2021;13:5211–5215. doi: 10.1039/D1AY01624E. [DOI] [PubMed] [Google Scholar]
- 29.Vichai V., Kirtikara K. Sulforhodamine B colorimetric assay for cytotoxicity screening. Nat. Protoc. 2006;1:1112–1116. doi: 10.1038/nprot.2006.179. [DOI] [PubMed] [Google Scholar]
- 30.Feng Z.-L., Zhang L.-L., Zheng Y.-D., Liu Q.-Y., Liu J.-X., Feng L., Huang L., Zhang Q.-W., Lu J.-J., Lin L.-G. Norditerpenoids and Dinorditerpenoids from the Seeds of Podocarpus nagi as Cytotoxic Agents and Autophagy Inducers. J. Nat. Prod. 2017;80:2110–2117. doi: 10.1021/acs.jnatprod.7b00347. [DOI] [PubMed] [Google Scholar]
- 31.Feng Z., Chen J., Feng L., Chen C., Ye Y., Lin L. Polyisoprenylated benzophenone derivatives from Garcinia cambogia and their anti-inflammatory activities. Food Funct. 2021;12:6432–6441. doi: 10.1039/D1FO00972A. [DOI] [PubMed] [Google Scholar]
- 32.Marco J.A., Sanz-Cervera J.F., Ocete G., Carda M., Rodríguez S., Vallès-Xirau J. New Germacranolides and Eudesmanolides from North African Artemisia herba-alba. J. Nat. Prod. 1994;57:939–946. doi: 10.1021/np50109a010. [DOI] [Google Scholar]
- 33.Segal R., Feuerstein I., Duddeck H., Kaiser M., Danin A. The sesquiterpene lactones from two populations of Artemisia herba alba. Phytochemistry. 1983;22:129–131. doi: 10.1016/S0031-9422(00)80072-2. [DOI] [Google Scholar]
- 34.Mohamed A.H., Esmail A.M., El-Saade A.M. Terpenes from Artemisia herba-alba. Z. Nat. 2013;68:343–346. doi: 10.1515/znc-2013-9-1001. [DOI] [PubMed] [Google Scholar]
- 35.Marco J.A., Sanz-cervera J.F., Manglano E., Sancenon F., Rustaiyan A., Kardar M. Sesquiterpene lactones from iranian Artemisia species. Phytochemistry. 1993;34:1561–1564. doi: 10.1016/S0031-9422(00)90845-8. [DOI] [Google Scholar]
- 36.Marco J.A., Sanz J.F., Yuste A., Carda M., Jakupovic J. Sesquiterpene lactones from Artemisia barrelieri. Phytochemistry. 1991;30:3661–3668. doi: 10.1016/0031-9422(91)80088-I. [DOI] [Google Scholar]
- 37.Rustaiyan A., Zare K., Ganj M.T., Sadri H.A. A melampolide and two dihydro artemorin derivatives from Artemisia gypsacea. Phytochemistry. 1989;28:1535–1536. doi: 10.1016/S0031-9422(00)97784-7. [DOI] [Google Scholar]
- 38.Zhang H., Liao Z.H., Yue J.M. Five New Sesquiterpenoids from Parasenecio petasitoides. Helv. Chem. Acta. 2004;87:976–982. doi: 10.1002/hlca.200490090. [DOI] [Google Scholar]
- 39.Kusumoto T., Miyamoto T., Higuchi R., Doi S., Sugimoto H., Yamada H. Isolation and Structures of Two New Compounds from the Essential Oil of Brazilian Propolis. Chem. Pharmaceut. Bull. 2001;49:1207–1209. doi: 10.1248/cpb.49.1207. [DOI] [PubMed] [Google Scholar]
- 40.Jakupovic J., Bohlmann F., Tan R.X., Jia Z.J., Huneck S. Prenylated coumarates from Artemisia xanthochroa. Phytochemistry. 1990;29:3683–3685. doi: 10.1016/0031-9422(90)85307-2. [DOI] [Google Scholar]
- 41.Jin L., Zhou W., Li R., Jin M., Jin C., Sun J., Li G. A new polyacetylene and other constituents with anti-inflammatory activity from Artemisia halodendron. Nat. Prod. Res. 2019;35:1010–1013. doi: 10.1080/14786419.2019.1610962. [DOI] [PubMed] [Google Scholar]
- 42.Wang Q., Hao J., Gong J., Bao W. Isolation and structure elucidation of two new compounds from Artemisia Ordosica Krasch. Nat. Prod. Res. 2019;34:1862–1867. doi: 10.1080/14786419.2018.1564298. [DOI] [PubMed] [Google Scholar]
- 43.Rocha D.D., Dantas I.N., Albuquerque M.R. Studies on the cytotoxicity of miscellaneous compounds from Eupatorium betonicaeforme (D.C.) Baker (Asteraceae) Chem. Biodivers. 2007;4:2835–2844. doi: 10.1002/cbdv.200790233. [DOI] [PubMed] [Google Scholar]
- 44.Zdero C., Bohlmann F., King R.M., Robinson H. Further 5-methyl coumarins and other constituents from the subtribe mutisiinae. Phytochemistry. 1986;25:509–516. doi: 10.1016/S0031-9422(00)85512-0. [DOI] [Google Scholar]
- 45.Maatooq G.T., Hoffmann J.J. Fungistatic sesquiterpenoids from Parthenium. Phytochemistry. 1996;43:67–69. doi: 10.1016/0031-9422(96)00225-7. [DOI] [Google Scholar]
- 46.Stavri M., Ford C.H., Bucar F., Streit B., Hall M.L., Williamson R.T., Mathew K.T., Gibbons S. Bioactive constituents of Artemisia monosperma. Phytochemistry. 2005;66:233–239. doi: 10.1016/j.phytochem.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 47.Gok M., Zeybek N.D., Bodur E. Butyrylcholinesterase expression is regulated by fatty acids in HepG2 cells. Chem.-Biol. Interact. 2016;259:276–281. doi: 10.1016/j.cbi.2016.04.029. [DOI] [PubMed] [Google Scholar]
- 48.Gao S., Tian W.J., Liao Z.J., Wang G.H., Zeng D.Q., Liu X.Z., Lin T. Chemical constituents from endophytic fungus Annulohypoxylon cf. stygium in leaves of Anoectochilus roxburghii (Wall.) Lindl. Chem. Biodivers. 2020;17:e2000424. doi: 10.1002/cbdv.202000424. [DOI] [PubMed] [Google Scholar]
- 49.Sun J., Zhou W., Wei C.X., Zhang Z., Jin X., Li G. A new benzofuran from Artemisia halodendron Turcz. ex Bess. Nat. Prod. Res. 2008;33:226–232. doi: 10.1080/14786419.2018.1443098. [DOI] [PubMed] [Google Scholar]
- 50.Pang N., Gu S.S., Wang J., Cui H.S., Wang F.Q., Liu X., Wu F.A. A novel chemoenzymatic synthesis of propyl caffeate using lipase-catalyzed transesterification in ionic liquid. Bioresour. Technol. 2013;139:337–342. doi: 10.1016/j.biortech.2013.04.057. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.