Abstract
Haiti is one of the most food-insecure (FIS) nations in the world, with increasing rates of overweight and obesity. This study aimed to characterize FIS among households in urban Haiti and assess the relationship between FIS and body mass index (BMI) using enrollment data from the Haiti Cardiovascular Disease Cohort Study. FIS was characterized as no/low, moderate/high, and extreme based on the Household Food Security Scale. Multinomial logistic generalized estimating equations were used to evaluate the association between FIS categories and BMI, with obesity defined as BMI ≥ 30 kg/m2. Among 2972 participants, the prevalence of moderate/high FIS was 40.1% and extreme FIS was 43.7%. Those with extreme FIS had higher median age (41 vs. 38 years) and were less educated (secondary education: 11.6% vs. 20.3%) compared to those with no/low FIS. Although all FIS categories had high obesity prevalence, those with extreme FIS compared to no/low FIS (15.3% vs. 21.6%) had the lowest prevalence. Multivariable models showed an inverse relationship between FIS and obesity: moderate/high FIS (OR: 0.77, 95% CI: 0.56, 1.08) and extreme FIS (OR: 0.58, 95% CI: 0.42, 0.81) versus no/low FIS were associated with lower adjusted odds of obesity. We found high prevalence of extreme FIS in urban Haiti in a transitioning nutrition setting. The inverse relationship between extreme FIS and obesity needs to be further studied to reduce both FIS and obesity in this population.
Keywords: household food insecurity, obesity, overweight, double burden of malnutrition, under-nutrition, over-nutrition, Haiti
1. Introduction
Haiti, home to approximately 11.5 million people in 2021, is the poorest country in the Caribbean and Latin American region and has been continuously afflicted by high levels of food insecurity (FIS) [1]. FIS, the lack of regular access to sufficient safe and nutritious food for healthy living, is initially indicated by first worrying about having enough food, and may progress to making dietary changes to stretch food, and lastly, to decreasing food consumption in adults first and then children [2,3]. In 2021, over 80% of Haitians were estimated as facing moderate-to-severe FIS, and almost half were experiencing acute or severe FIS. Approximately 37% of Haitians live in the urban capital of Port-au-Prince. Urban areas had more young adults aged 20–39 years (35.5% vs. 28.8%) and more females (66.3% vs. 54.8%) than the total population in 2017 [4]. Education levels in urban Haiti are low, with an estimated 5% of adults completing secondary education [4]. Food insecurity is rapidly increasing in Haiti, from an estimated 29% of residents in the capital in 2016 [5], to current estimates from October 2022 indicating that Haitian residents now face “catastrophic” food insecurity—a designation that is a first for Haiti and for any country in the Western Hemisphere [6]. Reasons for FIS in Haiti are complex and multifactorial, spanning issues such as lack of food availability, access, and stability, due to the historical lack of sustainable development from geopolitical and environmental factors over several decades [7,8]. From its independence, Haiti’s infrastructure development was hampered by an unfair debt to France, supported by exploitive policies in Western countries [9]. In the 20th century, US occupation, coupled with Haiti’s national government, did not invest in sustainable institutions, detracting from business investment and resulting in a loss of fertile agricultural lands and farming infrastructure. Moreover, food tariffs and commoditization of foods have led to an overdependence on expensive, often poor-quality food imports, reducing the access and availability of fresh and nutritious foods in Haiti [10,11]. Environmental factors, such as climate-driven disasters and conflict, deepen the already weak food system by disrupting local agricultural production. Deforestation also left the land vulnerable to soil erosion from weather events, making it difficult to have sustainable local food [12,13]. In 2019, Haiti had the third-highest climate risk index in the world [14]. Earthquakes in Port-au-Prince in 2010 and in the Tiburon Peninsula in 2021, as well as Hurricane Matthew in 2016 and Tropical Storm Grace, each led to increased FIS [15,16,17,18,19]. During the COVID-19 pandemic, one study estimated that 85.5% of Haitians were worried about not having enough to eat the following week [20]. In urban Port-au-Prince, rival gangs disrupt food access by blocking roadways and other critical systems providing humanitarian aid [18,21]. Structural poverty and wealth inequity also play a role, with an estimated 60% of Haitians living in poverty [22]. As a result, an average working person in Haiti would need to pay 35% of their daily income to eat a basic meal [23]. Although Haiti’s Global Hunger Index slightly improved from alarming to serious in 2021 [24], the fragile state of Haiti due to these factors result in food instability.
Many lower-income countries (LIC) are experiencing a double burden of malnutrition, in which undernutrition and obesity co-exist [25]. Almost half of the population of Haiti were undernourished, while an estimated 31.2% of adult women and 22.2% of adult men were obese in 2020 [24,26]. FIS may manifest as both low and high BMI. One meta-analysis demonstrated that FIS was associated with 15% higher odds of obesity (pooled odds ratio: 1.15, 95% CI 1.06–1.23); however, severe FIS was associated with undernutrition [27]. When foods are not available, FIS may lead to undernutrition and weight loss, while when foods are available, individuals may compensate by eating cheaper foods that are higher in salt, fat, and refined carbohydrates, leading to weight gain. FIS may also cause adverse psychological stress, which increases cardiovascular disease risk [28,29,30]. In LIC, where severe FIS is more prevalent, the FIS–obesity relationship has been inconsistent [30,31]. A study among individuals living with HIV in a rural area in Haiti found that those with severe FIS had a less diverse diet but did not have lower BMI status compared to those with low FIS [32]. Globalization of the food system has increased access to fast food and processed food in LIC, creating conditions for a nutritional and epidemiologic transition to higher prevalence of non-communicable diseases [33].
Few studies have evaluated the effect of FIS in an urban area of Haiti on malnutrition, despite its high prevalence. To address this gap, this study investigates the relationship between FIS and malnutrition (defined as underweight or overweight/obese) in Port-au-Prince, Haiti. We aim to (1) characterize FIS among households in a population-based cohort from Port-au-Prince and (2) evaluate the association between FIS and malnutrition. We hypothesized that individuals from households with moderate/high and extreme FIS have higher prevalence of malnutrition compared to those with low FIS.
2. Materials and Methods
2.1. Data Source and Study Sample
A cross-sectional study using baseline data from the Haiti Cardiovascular Disease (CVD) Cohort Study, a population-based cohort of Port-au-Prince residents, was conducted [34]. The Haiti CVD Cohort used a multistage random sampling design to randomly select participants in Port-au-Prince using GPS waypoints across census blocks, with the number of waypoints per block proportional to the estimated population size [35]. Participants were eligible if they were >18 years old, had a primary residence in Port-au-Prince, and did not have any serious medical condition or cognitive impairment preventing participation. The study was conducted at the Groupe Haitien d’Etude du Sarcome de Kaposi et des Infections Opportunistes clinics (GHESKIO), a medical organization in Haiti which has provided clinical care for over 40 years and conducts research on HIV and chronic diseases. For this study, baseline data from participants enrolled between 15 March 2019 and 23 August 2021 were included. Participants who were pregnant were excluded (n = 33) (Figure S1).
2.2. Measures
2.2.1. Household Food Insecurity
FIS was measured at the household level using an adapted version of the Six-Item Short Form of the Household Food Security Scale (study Cronbach’s alpha = 0.76), which measures FIS and hunger within the last 12 months and has been used in other LICs [36,37,38,39,40]. The scale consists of six questions indicating frequency of each FIS item. Traditionally, it is scored by assigning a point based on item responses of “often”, “sometimes”, “yes”, “almost every month” and “some months but not every month”, and then it is summed (range: 0–6) and categorized into high or marginal food security (0–1), low food security (2–4) and very low food security (5–6). However, given the high level of FIS in Haiti, an extreme FIS score was defined to capture differences across a population where the majority live with chronic food insecurity. The scoring was modified by assigning a point only to responses of “often”, “yes”, or “almost every month” on each item and then summing across items (range: 0–6). The score was then categorized as no/low FIS (0–2), moderate/high FIS (3–4), or extreme FIS (5–6). Classification of participants based on the original and the modified categories is found in Figure S2.
2.2.2. Malnutrition
Malnutrition was defined as underweight, overweight, and obese based on the WHO classification using body mass index (BMI) categories [41]. BMI in kg/m2 was calculated using height and weight measured in the GHESKIO clinic at the baseline visit and classified as underweight: <18.5, normal: 18.5–<25, overweight: 25–<30, and obese: ≥30.
2.2.3. Other Study Measures
Socio-demographic factors were measured on the individual level and included age, sex, education level, and individual income. Additional factors measured at the household level included total number of individuals living together. Family or neighborhood factors measured were perceived social support, social cohesion, and neighborhood violence. Perceived social support was based on the 12-item Multidimensional Scale of Perceived Social Support (MSPSS) [42]. Each item was scaled from 1: very strongly disagree-7: very strongly agree and scored as the mean of all items (range: 1–7). Social cohesion was based on the 5-item Collective Efficacy scale. Responses were coded as 1: strongly agree to 5: strongly disagree. After reverse-coding negative responses, item responses were summed to create a social cohesion score (range = 5–25). Neighborhood violence was based on the 5-item City Stress Index (CSI) [43]. Each response was scaled from 1: Never to 4: Often and the mean of all the items was calculated to determine a score (range = 1–4). An increase in perceived social support score, social cohesion score, and neighborhood violence score represented more social support, more social cohesion, or more neighborhood violence, respectively.
2.3. Statistical Analyses and Model Specification
Study characteristics were summarized by FIS categories. Unadjusted and multivariable multinomial logistic generalized estimating equations were fitted to evaluate population-averaged effects of FIS on BMI categories, using normal BMI as the referent outcome category. The multivariable model was adjusted for common variables associated with FIS and BMI (age, sex, household size, individual income, social support, neighborhood violence, and social cohesion) determined from the literature and guided using a directed acyclical graph (Figure S3). Continuous variables were mean-centered. Models accounted for clustering effects of households. Variance inflation factors < 5 for all variables, indicating that collinearity was not present. Due to missing data from BMI categories (n = 5, 0.1%), FIS (n = 62, 1.6%) and covariates (n = 33, 1.1%), complete cases (96.6%) were modeled. Unadjusted (OR) and adjusted odds ratios (aOR) and 95% confidence intervals (CI) were reported.
Several sensitivity analyses were performed. Potential effect measure modification between households with and without children, sex, and age group were also assessed by including statistical interactions between the potential modifiers and FIS. These were chosen because the six-item FIS instrument has lower validity for households with children and because of potential heterogeneity in FIS and malnutrition by demographics. R, version 4.1.2 was used for all analyses [44].
2.4. Ethical Considerations
All participants provided written informed consent before enrollment. Community, school, and religious leaders, as well as GHESKIO’s Community Advisory Board, were consulted prior to beginning the study. The institutional review boards at Weill Cornell Medicine and GHESKIO in Haiti approved all study procedures and protocols.
3. Results
3.1. Prevalence of FIS
The study included 2972 cohort participants from 1981 households who completed the baseline visit. Participants had a median age of 40 years (interquartile range (IQR): 28, 55) (Table 1). Just over half were female (57.6%), unmarried (55.2%), or had no children in the household (53.3%). Few had more than a high school education (14.9%) or earned >USD 10/day (17.7%).
Table 1.
Characteristics compared by food insecurity categories from the Haiti CVD Cohort Study, 2019–2021 (n = 2972).
| Characteristic | No/Low FIS | Mod/High FIS | Extreme FIS | Overall a |
|---|---|---|---|---|
| Total | 418 (14.1) | 1193 (40.1) | 1299 (43.7) | 2972 (100) |
| Age in years, Med (IQR), (Range) | 38 (27, 52), (18, 93) | 41 (28, 55), (18, 90) | 41 (28, 55), (18, 90) | 40 (28, 55), (18, 93) |
| Age group, n (%) | ||||
| ≤39 years | 221 (52.9%) | 557 (46.7%) | 618 (47.6%) | 1430 (48.1%) |
| 40–59 years | 138 (33.0) | 430 (36.0) | 445 (34.3) | 1028 (34.6) |
| 60+ years | 59 (14.1) | 206 (17.3) | 236 (18.2) | 514 (17.3) |
| Female Sex, n (%) | 251 (60.0) | 661 (55.4) | 766 (59.0) | 1712 (57.6) |
| Highest level of school, n (%) | ||||
| ≤Primary | 121 (29.0) | 418 (35.0) | 503 (38.7) | 1066 (35.9) |
| Secondary | 211 (50.5) | 576 (48.3) | 644 (49.6) | 1457 (49.0) |
| Higher than secondary | 85 (20.3) | 194 (16.3) | 151 (11.6) | 442 (14.9) |
| Missing | 1 (0.2) | 5 (0.4) | 1 (0.1) | 7 (0.2) |
| Current marital status, n (%) | ||||
| Single | 231 (55.3) | 648 (54.3) | 729 (56.1) | 1642 (55.2) |
| Living together | 61 (14.6) | 182 (15.3) | 244 (18.8) | 493 (16.6) |
| Married | 100 (23.9) | 291 (24.4) | 249 (19.2) | 661 (22.2) |
| Widowed/Divorced/Separated | 25 (6.0) | 67 (5.6) | 76 (5.8) | 169 (5.7) |
| Missing | 1 (0.2) | 5 (0.4) | 1 (0.1) | 7 (0.2) |
| Income, n (%) | ||||
| Less than USD 10/day | 342 (81.8) | 980 (82.1) | 1065 (82.0) | 2440 (82.1) |
| More than USD 10/day | 75 (17.9) | 208 (17.4) | 233 (17.9) | 525 (17.7) |
| Missing | 1 (0.2) | 5 (0.4) | 1 (0.1) | 7 (0.2) |
| No. people currently live in household, Med (IQR), (Range) | 3 (2, 5), (1–13) | 3 (2, 5), (1–14) | 3 (2, 5), (1–15) | 3 (2, 5), (1–15) |
| Perceives social support score, Med (IQR), (Range) | 5.64 (4.55, 6.45), (1, 7) | 5.55 (4.45, 6.45), (1, 7) | 5.55 (4.36, 6.52), (1, 7) | 5.55 (4.45, 6.45), (1, 7) |
| Missing | 3 (0.7) | 5 (0.4) | 1 (0.1) | 9 (0.3) |
| Social cohesion score, Med (IQR), (Range) | 15 (14, 16), (7, 22) | 15 (13, 16), (7, 24) | 15 (13, 16), (7, 24) | 15 (13, 16), (7, 24) |
| Missing | 1 (0.2) | 5 (0.4) | 1 (0.1) | 7 (0.2) |
| Neighborhood violence score, Med (IQR), (Range) | 9 (7, 11), (5–17) | 9 (7, 10), (5–17) | 9 (7, 11), (5–20) | 9 (7, 11), (5–20) |
| Missing | 2 (0.5) | 16 (1.3) | 14 (1.1) | 32 (1.1) |
CVD = cardiovascular disease; FIS = household food insecurity; Med = median; IQR = interquartile; HH = household. a FIS values missing for 62 participants.
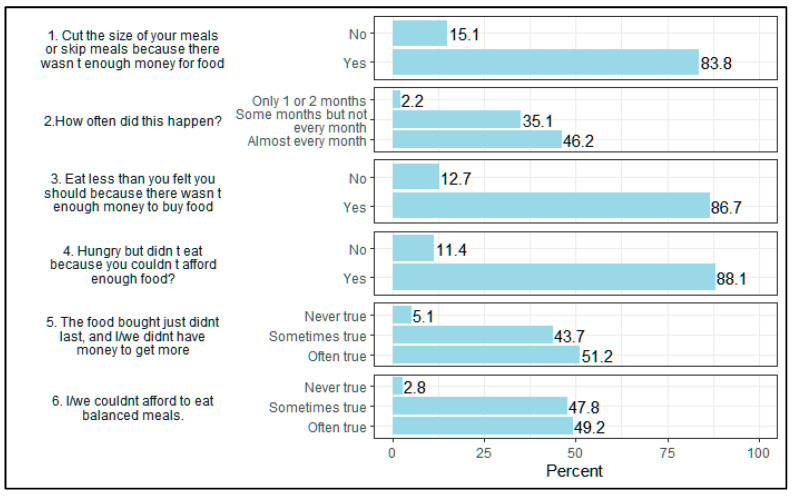
Using the modified FIS score, the prevalence of moderate/high FIS was 40.1% and extreme FIS was 43.7%. Within the past 12 months, the overwhelming majority indicated skipping a meal or cutting portion size (83.8%), eating less (86.7%) or not eating when hungry due to lack of money (88.1%) (Figure 1). About half of participants indicated that food often did not last (51.2%) and that they often could not afford balanced meals (49.2%). Compared to those with no/low FIS, those with extreme FIS were on average older (median (IQR): 41 (28, 55) vs. 38 (27, 52) years) and less educated (secondary education: 11.6% vs. 20.3%).
Figure 1.
Household Food Insecurity Item Responses from the Haiti CVD Cohort Study, 2019–2021 (N = 2972) Items with responses of unknown, refused, or missing were not presented and percent may not total 100%.
3.2. Associations between FIS and Malnutrition
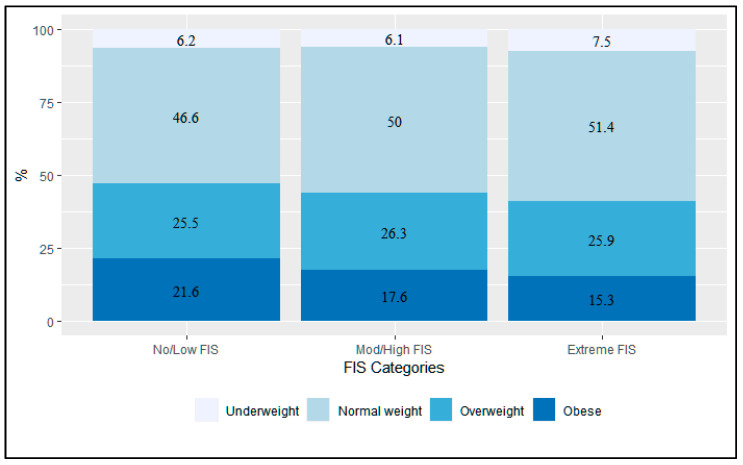
Participants with extreme FIS compared to those with no/low FIS had similar underweight prevalence (7.5% vs. 6.2%) and were less frequently obese (15.3% vs. 21.6%) (Figure 2). For participants with extreme FIS (n = 1299 (43.7%)), those who were obese (n = 198) compared to underweight (n = 97) were on average older (median (IQR): 46 (24–52) vs. 33 (24–52)) and had substantially higher proportions of females (92.9% vs. 46.4%). While still the majority, obese persons had lower proportions of earning no or little income (<USD 10/day) compared with those who were underweight (71.7% vs. 90.7%).
Figure 2.
Prevalence of malnutrition by FIS from the Haiti CVD Cohort Study, 2019–2021 (N = 2972).
From the multivariable models shown in Table 2, there was an inverse dose response relationship, with moderate/high FIS (OR: 0.77, 95% CI: 0.56, 1.08) and extreme FIS vs. no/low FIS (OR: 0.58, 95% CI: 0.42, 0.81) associated with decreasing odds of being obese vs. normal weight. No association between FIS categories and being underweight were found. These effects were not modified by having children in the household, participant sex, or age (interaction p values > 0.10).
Table 2.
Association between FIS categories a and malnutrition b, from multinomial logistic general estimating equations.
| BMI Categories | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Underweight vs. Normal | ||
| No/Low FIS | Ref | Ref |
| Mod/High FIS | 0.90 (0.56, 1.44) | 0.96 (0.60, 1.55) |
| Extreme FIS | 1.07 (0.68, 1.69) | 1.12 (0.70, 1.78) |
| Overweight vs. Normal | ||
| No/Low FIS | Ref | Ref |
| Mod/High FIS | 0.97 (0.74, 1.26) | 0.94 (0.71, 1.24) |
| Extreme FIS | 0.93 (0.71, 1.21) | 0.88 (0.67, 1.16) |
| Obese vs. Normal | ||
| No/Low FIS | Ref | Ref |
| Mod/High FIS | 0.77 (0.57, 1.04) | 0.77 (0.56, 1.08) |
| Extreme FIS | 0.65 (0.48, 0.87) | 0.58 (0.42, 0.81) |
BMI = body mass index; FIS = food insecurity; OR = odds ratio; CI = confidence interval; Ref = reference level. a FIS categories based on the modified version of the Six-Item Short Form of the Household Food Security Scale. No/low FIS (0–2), moderate/high FIS (3–4), and extreme FIS (5–6). b Estimates based on unadjusted and multivariable multinomial logistic general estimating equations of the effects of FIS on BMI categories, using normal BMI as the reference outcome. The multivariable model adjusted for age, sex, household size, income, social support, neighborhood violence, and social cohesion.
4. Discussion
Our study fills an important knowledge gap in the relationship between food insecurity and malnutrition, measured as underweight, overweight, and obese based on BMI categories, using a large community-based cohort in Port-au-Prince, Haiti. We found that the prevalence of moderate/high or extreme FIS was extremely high at 83.8% and that both moderate/high and extreme FIS compared to low FIS were associated with lower odds of being obese versus normal weight in a dose–response fashion, but were not associated with underweight versus normal weight.
The prevalence of moderate/high or extreme FIS in Port-au-Prince found in this study was similar to Haiti’s 2021 national estimate of >80%, though it was measured using different scales [45]. Although such high prevalence (72–95%) of moderate or severe FIS had been documented among vulnerable groups such as rural residents, pregnant women, and those living with HIV, [32,46,47], urban areas historically had lower prevalence of FIS [5,48]. However, a 2021 report noted a change in acute FIS during 2018–2021 from minimal to crisis designation in Port-au-Prince [49]. This alarming shift was likely the result of the 2021 earthquake and political instability during this period. After these events, rival gangs blocked major roads into Port-au-Prince and inflation of staple foods increased, worsening both food availability and food access [18,49].
Consistent with prior studies, the prevalence of moderate/high and extreme FIS was higher among those with lower education [32]. Although younger age was sometimes noted as a risk factor for FIS, in our sample, extreme FIS was more common among older adults [20]. Older participants may be especially vulnerable to FIS and its impact, possibly due to a higher likelihood of living alone without social support, and a greater difficulty accessing transportation to go to markets [50]. Although gender was correlated with FIS in other LIC, we did not find this association in our sample, and differences were previously found in rural communities among female farmers and widows and may not generalize to all women or women in urban settings [48,51]. The high overall prevalence of FIS in this region may also obscure smaller differences between subgroups.
While FIS has recently been associated in LICs with overweight/obesity due to excess consumption of low-quality calories from refined sugars and carbohydrates, facilitated by increased availability and access to cheap, edible oils and excess empty calories [33], we found the opposite association of extreme FIS associated with lower prevalence of obesity. In sub-Saharan Africa, high prevalence of overweight status (15.8%) was found among participants with FIS [31]. Severe FIS has also been associated with 30% higher odds for fast-food consumption in other LICs [52]. Our study found a lack of association between FIS and being underweight in a general urban population and builds on past studies showing this lack of association in special populations like persons living with HIV in rural Haiti [32].
A simple relationship between FIS, underweight, and overweight/obese status may not exist across multiple contexts, as caloric intake may change over time across populations and even within the same person due to fluctuating income, food availability, and access. Consumption of caloric-rich Western foods are suggested as the mechanism between FIS and obesity [30]. In Haiti, a transition to a Western diet has been noted, as well as an increase in obesity prevalence and a decrease in underweight prevalence [26,53]. Both those with extreme FIS and low FIS likely consume these foods, but not with the same regularity. The extreme FIS, who are extremely poor, may live in homes with inadequate means to cook regularly, such as indoor stoves, and may rely on prepackaged, highly processed foods rich in carbohydrates when available. However, they may not eat consistently due to frequent periods of reduced food availability and access. Neighborhood safety and lack of transportation in poor communities limit access to markets, street vendors, and restaurants selling nutrient-dense foods. Further, this vulnerable group is disproportionately affected by instability of the food supply due to geopolitical and environmental factors. When food can be purchased, there may be increased empty caloric intake, but when food availability and access are disrupted, those with extreme FIS go hungry, bounding their obesity prevalence. Those with low FIS, however, have more means to regularly consume high-caloric foods, leading to higher BMI. One study showed that Haitians who frequently ate high-caloric diets also had higher income and higher educational status [53]. Increased income was also associated with increased obesity prevalence in this cohort and those who were obese were more likely to eat from a street vendor [54]. Further, although those with extreme FIS may be less obese on average, they may still be at risk for cardiometabolic complications [55,56,57]. There was a 20% increase in cardiovascular disease (CVD) in Haiti from 2009–2019 and CVD was the leading cause of death in 2019 [58]. Focusing on BMI categories to reduce CVD may exclude this vulnerable group.
Both long-term and short-term resilience to food insecurity is needed. Multilateral organizations, in coordination with the government of Haiti, have adopted a systems approach to improve food security with long-term policy goals [12,13,59]. Short-term interventions include emergency aid programs, increased screening within clinics and schools, and increased health-care provider training on malnutrition treatment. Longer-term interventions must strengthen the education, healthcare systems, and supply of local agriculture in Haiti. In addition, larger structural interventions that encourage and incentivize local agriculture sector growth of local nutritious foods that are more affordable than expensive exports are needed. Food insecurity is also increasing due to climate change [60]. Programs for local and safe food storage and food distribution plans may provide resilience to interruptions to the food supply from natural disasters [60]. Climate-smart agriculture, such as water retention plans, hillside terracing, greenhouses, and food gardens should expand to urban areas [11,61]. These potential local sources of food may be resistant to internal obstacles of food delivery. Additionally, novel community-based models of care should be considered, including Haiti’s success with using community health workers to provide education, screening, and food distribution. Community health workers have been used by GHESKIO for over 20 years during public health epidemics to provide emergency cholera vaccination, tuberculosis screening, and malnutrition screening. Data specifically from our study found that policies should target older adults and those with low education, as they were more vulnerable to extreme FIS. Examples of policies or interventions could include public media and education campaigns, primary-school-based food insecurity assessment and aid, and community-organization-based education and aid programs targeting these specific groups.
By quantifying FIS, as well as identifying groups vulnerable to extreme FIS in urban Haiti, this study may support policy-makers in designing interventions and allocating resources to address FIS. This study also highlights the complexity of the nutritional transition in Haiti by evaluating the relationship between FIS and malnutrition. However, some limitations of our work should be considered. First, the six-item Household Food Security Scale from the last 12 months was not validated in Haiti, and measurement from other studies using the Household Hunger Scale, which prompted responses within the last 4 months, may contribute to prevalence differences; however, our modified scale was restrictive, and most participants endorsed food-insecure behaviors occurring often and almost every month. The six-item scale also did not directly ask about child hunger, which is an indication of the most severe household food insecurity. The sensitivity analyses, however, did not demonstrate differences in effects by the presence of children in the household. Second, results from an urban area of Haiti may not be generalizable to other populations in Haiti with different socio-economic status, higher income, or to other time periods given the influential events in 2019–2021. Third, BMI has been shown to misclassify participants as overweight or obese [62]. Future analyses using other anthropomorphic measures such as the waist-to-hip or waist-to-height ratio should be considered [63]. Lastly, since this is a cross-sectional study, no temporal or causal relationships can be inferred.
5. Conclusions
In summary, we found high proportions of extreme FIS in an urban region of Haiti, which is higher among the less-educated and older adults. Extreme FIS is a metric that may be a useful in identifying the most vulnerable and in need of immediate interventions in extremely low-income countries with large prevalence of food insecurity. The inverse relationship between FIS and obesity underscores the complexity of malnutrition, suggesting that policies and interventions are needed to confront FIS and obesity as dual health targets. Haiti and similar low-income countries facing dual challenges of FIS and obesity need immediate and long-term interventions, ranging from FIS and obesity screening programs with direct food subsidies to longer-term plans for development of agricultural infrastructure, increased education, and food safety nets. As the ongoing food insecurity crisis in Haiti continues, these interventions to improve the resilience to food insecurity, as well as studies evaluating their effectiveness, are paramount for improving health outcomes across the region.
Acknowledgments
The authors would like to formally acknowledge our study participants and the research team and field workers who ensured the viability of high-quality data for this study.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14224854/s1, Figure S1: Flow diagram; Figure S2: Comparison of USDA Household FIS categories and Modified Household FIS Categories, Figure S3: Proposed causal relationship between FIS and malnutrition.
Author Contributions
Conceptualization, R.R., D.N., D.W.F. and M.L.M.; methodology, R.R., D.N., D.W.F., I.J. and M.L.M.; validation, M.L.M. and V.R.; formal analysis, R.R.; investigation, R.S., V.R., M.M.D., D.W.F., I.J. and J.W.P.; resources, J.W.P. and M.L.M.; data curation, M.L.M., S.S., N.M., I.J. and L.D.Y.; writing—original draft preparation, R.R., D.N. and M.L.M.; writing—review and editing, all authors; visualization, R.R.; supervision, M.L.M. and D.N.; project administration, N.M.; funding acquisition, M.L.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Weill Cornell Medicine (protocol number 1803019037, approved on 6 July 2018) and GHESKIO (approved on 23 June 2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data contain potentially identifying and sensitive patient information. Deidentified data used for this analysis are available upon request after signing a data access and use agreement, provision of approval by the GHESKIO ethics board, and demonstration that the external investigative team is qualified and has documented evidence of human research protection training. Requests may be addressed to the authors or to irb@med.cornell.edu.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Funding for this study comes from the National Heart, Lung, and Blood Institute, grant numbers R01HL143788 (M.L.M, V.R., J.W.P., D.N.), R01HL143788-S1 (M.L.M., V.R.) and D43TW011972 (R.S.). The funders had no role in the study design or execution of this protocol.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Bank . Macro Poverty Outlook (MPO) World Bank Group; Washington, DC, USA: 2022. Macro Poverty Outlook for Haiti: April 2022 (English) [Google Scholar]
- 2.Clay E. Chapter 2. Food Security: Concepts and Measurement. FAO; Rome, Italy: 2003. [(accessed on 2 June 2022)]. Trade Reform and Food Security: Conceptualizing the Linkages. Available online: https://www.fao.org/3/y4671e/y4671e06.htm. [Google Scholar]
- 3.FAO . Rome Declaration on World Food Security, World Food Summit. FAO; Rome, Italy: 1996. [Google Scholar]
- 4.Institut Haïtien de l’Enfance—IHE/Haiti. ICF . Haiti Enquête Mortalité, Morbidité et Utilisation des Services 2016–2017—EMMUS-VI. IHE/Haiti, ICF; Port-au-Prince, Haïti: 2018. [Google Scholar]
- 5.Haitian National Coordination for Food Security, World Food Programme Haiti Country Office Haiti Urban Food Security Assessment. 2016. [(accessed on 1 June 2021)]. Available online: https://www.wfp.org/publications/haiti-urban-food-security-assessment-august-2016.
- 6.FAO . Haiti Response Overview October 2022. FAO; Rome, Italy: 2022. [Google Scholar]
- 7.Kianersi S., Jules R., Zhang Y., Luetke M., Rosenberg M. Associations between hurricane exposure, food insecurity, and microfinance; a cross-sectional study in Haiti. World Dev. 2021;145:105530. doi: 10.1016/j.worlddev.2021.105530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sripad P., Casseus A., Kennedy S., Isaac B., Vissieres K., Warren C.E., Ternier R. “Eternally restarting” or “a branch line of continuity”? Exploring consequences of external shocks on community health systems in Haiti. J. Glob. Health. 2021;11:07004. doi: 10.7189/jogh.11.07004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Porter C.M.C., Apuzzo M., Gebrekidan S. The Root of Haiti’s Miseries: Reparations to Enslavers. The New York Times. May 20, 2022. [(accessed on 2 June 2022)]. Available online: https://www.nytimes.com/2022/05/20/world/americas/haiti-history-colonized-france.html.
- 10.NYU School of Law Center for Human Rights and Global Justice, Partners in Health, RFK Center for Justice & Human Rights, Zanmi Lasante Sak Vid Pa Kanpe: The Impact of U.S. Food Aid on Human Rights in Haiti. 2010. [(accessed on 2 June 2022)]. Available online: https://www.pih.org/practitioner-resource/sak-vid-pa-kanpe-the-impact-of-u.s.-food-aid-on-human-rights-in-haiti/sak-vid-pa-kanpe-the-impact-of-u.s.-food-aid-on-human-rights-in-haiti.
- 11.USAID . USAID Office of Food for Peace: Haiti USAID-Best Analysis. USAID; Washington DC, USA: 2013. [Google Scholar]
- 12.USAID . Haiti Strategic Framework December 23, 2020—December 23, 2022 Extended Through: December 23, 2024. USAID; Washington, DC, USA: 2020. [(accessed on 17 October 2022)]. Available online: https://www.usaid.gov/sites/default/files/documents/Strategic_Framework_-_Haiti_-_December_2020-2022.pdf. [Google Scholar]
- 13.The United Nations World Food Programme . Haiti Annual Country Report 2021, Country Strategic Plan. World Food Programme; Rome, Italy: 2021. [(accessed on 17 October 2022)]. Available online: https://www.wfp.org/operations/ht02-haiti-country-strategic-plan-2019-2023. [Google Scholar]
- 14.Eckstein D., Kunzel V., Shafer L. Global Climate Risk Index 2021, Who Suffers Most from Extreme Weather Events? Weather Related Loss Events in 2019 and 2000–2019. Germanwatch e.V.; Bonn, Germny: Berlin, Germny: 2021. [Google Scholar]
- 15.Hutson R.A., Trzcinski E., Kolbe A.R. Features of child food insecurity after the 2010 Haiti earthquake: Results from longitudinal random survey of households. PLoS ONE. 2014;9:e104497. doi: 10.1371/journal.pone.0104497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirsch T.D., Leidman E., Weiss W., Doocy S. The impact of the earthquake and humanitarian assistance on household economies and livelihoods of earthquake-affected populations in Haiti. Am. J. Disaster Med. 2012;7:85–94. doi: 10.5055/ajdm.2012.0084. [DOI] [PubMed] [Google Scholar]
- 17.Kolbe A.R., Hutson R.A., Shannon H., Trzcinski E., Miles B., Levitz N., Puccio M., James L., Noel J.R., Muggah R. Mortality, crime and access to basic needs before and after the Haiti earthquake: A random survey of Port-au-Prince households. Med. Confl. Surviv. 2010;26:281–297. doi: 10.1080/13623699.2010.535279. [DOI] [PubMed] [Google Scholar]
- 18.Daniels J.P. Earthquake compounds Haiti’s health challenges. Lancet. 2021;398:944–945. doi: 10.1016/S0140-6736(21)02009-2. [DOI] [PubMed] [Google Scholar]
- 19.The Integrated Food Security Phase Classification HAITI: Grand Sud, Areas Affected by the Latest Shocks (Earthquake and Floods), IPC Acute Food Insecurity Analysis. [(accessed on 21 December 2021)]. Available online: https://reliefweb.int/report/haiti/haiti-grand-sud-areas-affected-latest-shocks-earthquake-and-floods-ipc-acute-food.
- 20.Benites-Zapata V.A., Urrunaga-Pastor D., Solorzano-Vargas M.L., Herrera-Añazco P., Uyen-Cateriano A., Bendezu-Quispe G., Toro-Huamanchumo C.J., Hernandez A.V. Prevalence and factors associated with food insecurity in Latin America and the Caribbean during the first wave of the COVID-19 pandemic. Heliyon. 2021;7:e08091. doi: 10.1016/j.heliyon.2021.e08091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor L. Doctors targeted and hospitals close amid gang violence in Haiti. BMJ. 2022;377:o1366. doi: 10.1136/bmj.o1366. [DOI] [PubMed] [Google Scholar]
- 22.World Bank . The World Bank in Haiti. World Bank; Washington, DC, USA: 2021. [Google Scholar]
- 23.The United Nations World Food Programme The Cost of a Plate of Food—2020. [(accessed on 21 December 2021)]. Available online: https://cdn.wfp.org/2020/plate-of-food/?_ga=2.88527769.367035939.1637077491-560390614.1637077491.
- 24.Global Hunger Index Global Hunger Index 2021: Haiti. 2021. [(accessed on 15 September 2021)]. Available online: https://www.globalhungerindex.org/haiti.html.
- 25.World Health Organization . The Double Burden of Malnutrition Policy Brief. World Health Organization; Geneva, Switzerland: 2017. [Google Scholar]
- 26.Global Nutrition Report . 2021 Global Nutrition Report: The State of Global Nutrition. Development Initiatives; Bristol, UK: 2021. [Google Scholar]
- 27.Moradi S., Mirzababaei A., Dadfarma A., Rezaei S., Mohammadi H., Jannat B., Mirzaei K. Food insecurity and adult weight abnormality risk: A systematic review and meta-analysis. Eur. J. Nutr. 2019;58:45–61. doi: 10.1007/s00394-018-1819-6. [DOI] [PubMed] [Google Scholar]
- 28.Palakshappa D., Ip E.H., Berkowitz S.A., Bertoni A.G., Foley K.L., Miller D.P., Jr., Vitolins M.Z., Rosenthal G.E. Pathways by Which Food Insecurity Is Associated with Atherosclerotic Cardiovascular Disease Risk. J. Am. Heart Assoc. 2021;10:e021901. doi: 10.1161/JAHA.121.021901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Derose K.P., Ríos-Castillo I., Fulcar M.A., Payán D.D., Palar K., Escala L., Farías H., Martínez H. Severe food insecurity is associated with overweight and increased body fat among people living with HIV in the Dominican Republic. AIDS Care. 2018;30:182–190. doi: 10.1080/09540121.2017.1348597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Farrell P., Thow A.M., Abimbola S., Faruqui N., Negin J. How food insecurity could lead to obesity in LMICs: When not enough is too much: A realist review of how food insecurity could lead to obesity in low- and middle-income countries. Health Promot. Int. 2018;33:812–826. doi: 10.1093/heapro/dax026. [DOI] [PubMed] [Google Scholar]
- 31.Nkambule S.J., Moodley I., Kuupiel D., Mashamba-Thompson T.P. Association between food insecurity and key metabolic risk factors for diet-sensitive non-communicable diseases in sub-Saharan Africa: A systematic review and meta-analysis. Sci. Rep. 2021;11:5178. doi: 10.1038/s41598-021-84344-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rebick G.W., Franke M.F., Teng J.E., Gregory Jerome J., Ivers L.C. Food Insecurity, Dietary Diversity, and Body Mass Index of HIV-Infected Individuals on Antiretroviral Therapy in Rural Haiti. AIDS Behav. 2016;20:1116–1122. doi: 10.1007/s10461-015-1183-y. [DOI] [PubMed] [Google Scholar]
- 33.Popkin B.M., Adair L.S., Ng S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012;70:3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lookens J., Tymejczyk O., Rouzier V., Smith C., Preval F., Joseph I., Baptiste R.J., Victor J., Severe P., Apollon S., et al. The Haiti cardiovascular disease cohort: Study protocol for a population-based longitudinal cohort. BMC Public Health. 2020;20:1633. doi: 10.1186/s12889-020-09734-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Institut Haitien de Statistique et D’Informatique (IHSI) Population Totale, De 18 Ans Et Plus Menages Et Densites Estimes en 2015. Ministere de L’Economie et des Finances (MEF); Port-au-Prince, Haiti: 2015. [Google Scholar]
- 36.Blumberg S.J., Bialostosky K., Hamilton W.L., Briefel R.R. The effectiveness of a short form of the Household Food Security Scale. Am. J. Public Health. 1999;89:1231–1234. doi: 10.2105/AJPH.89.8.1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bickel G., Nord M., Price C., Hamilton W., Cook J. Guide to Measuring Household Food Security: Revised 2000. USDA Food and Nutrition Service, Office of Analysis, Nutrition, and Evaluation, and USDA Economic Research Service, Food and Rural Economics Division; Alexandria, VA, USA: 2000. [Google Scholar]
- 38.Coates J., Frongillo E.A., Rogers B.L., Webb P., Wilde P.E., Houser R. Commonalities in the experience of household food insecurity across cultures: What are measures missing? J. Nutr. 2006;136:1438s–1448s. doi: 10.1093/jn/136.5.1438S. [DOI] [PubMed] [Google Scholar]
- 39.Melgar-Quinonez H.R., Zubieta A.C., MkNelly B., Nteziyaremye A., Gerardo M.F., Dunford C. Household food insecurity and food expenditure in Bolivia, Burkina Faso, And the Philippines. J. Nutr. 2006;136:1431s–1437s. doi: 10.1093/jn/136.5.1431S. [DOI] [PubMed] [Google Scholar]
- 40.Pérez-Escamilla R., Dessalines M., Finnigan M., Pachón H., Hromi-Fiedler A., Gupta N. Household food insecurity is associated with childhood malaria in rural Haiti. J. Nutr. 2009;139:2132–2138. doi: 10.3945/jn.109.108852. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization . WHO STEPS Surveillance Manual: The WHO STEPwise Approach to Chronic Disease Risk Factor Surveillance. World Health Organization; Geneva, Switzerland: 2017. [Google Scholar]
- 42.Zimet G.D., Powell S.S., Farley G.K., Werkman S., Berkoff K.A. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1990;55:610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 43.Ewart C.K., Suchday S. Discovering how urban poverty and violence affect health: Development and validation of a Neighborhood Stress Index. Health Psychol. 2002;21:254–262. doi: 10.1037/0278-6133.21.3.254. [DOI] [PubMed] [Google Scholar]
- 44.R Core Team . R Foundation for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2021. R: A Language and Environment for Statistical Computing. [Google Scholar]
- 45.Integrated Food Security Phase Classification Haiti: Integrated Food Security Phase Classification Snapshot September 2021–June 2022; Integrated Food Security Phase Classification: 2021. [(accessed on 2 June 2022)]. Available online: https://www.ipcinfo.org/ipc-country-analysis/details-map/en/c/1155096/?iso3=HTI.
- 46.Richterman A., Franke M.F., Constant G., Jerome G., Ternier R., Ivers L.C. Food insecurity and self-reported cholera in Haitian households: An analysis of the 2012 Demographic and Health Survey. PLoS Negl. Trop Dis. 2019;13:e0007134. doi: 10.1371/journal.pntd.0007134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Richterman A., Raymonville M., Hossain A., Millien C., Joseph J.P., Jerome G., Franke M.F., Ivers L.C. Food insecurity as a risk factor for preterm birth: A prospective facility-based cohort study in rural Haiti. BMJ Glob. Health. 2020;5:e002341. doi: 10.1136/bmjgh-2020-002341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Duvivier P., Fontin M.L. CTA Working Paper 17/09. State University of Haiti/Technical Centre for Agricultural and Rural Cooperation (CTA); Wageningen, The Netherlands: 2017. [(accessed on 1 June 2022)]. Building the evidence base on the agricultural nutrition nexus: Haiti. Available online: https://www.cta.int/fr/issue/building-the-evidence-base-on-the-agricultural-nutrition-nexus-haiti-sid02f2889e9-8f6d-429e-bf1e-f2d67abf162f. [Google Scholar]
- 49.IPC . Haiti: Acute Food Insecurity Analysis, March–June 2021. IPC; Rome, Italy: 2020. [Google Scholar]
- 50.Yan L.D., Dévieux J.G., Pierre J.L., Dade E., Sufra R., St Preux S., Tymejczyk O., Nash D., Metz M., Lee M.H., et al. The relationship between perceived stress and support with blood pressure in urban Haiti: A cross-sectional analysis. PLoS Glob. Public Health. 2022;2:e0000263. doi: 10.1371/journal.pgph.0000263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Botreau H., Cohen M.J. Gender inequality and food insecurity: A dozen years after the food price crisis, rural women still bear the brunt of poverty and hunger. Adv. Food Secur. Sustain. 2020;5:53–117. doi: 10.1016/bs.af2s.2020.09.001. [DOI] [Google Scholar]
- 52.Smith L., Barnett Y., López-Sánchez G.F., Shin J.I., Jacob L., Butler L., Cao C., Yang L., Schuch F., Tully M., et al. Food insecurity (hunger) and fast-food consumption among 180 164 adolescents aged 12-15 years from sixty-eight countries. Br. J. Nutr. 2022;127:470–477. doi: 10.1017/S0007114521001173. [DOI] [PubMed] [Google Scholar]
- 53.Mabchour A.E., Delisle H., Vilgrain C., Larco P., Sodjinou R. Abdominal obesity and other cardiometabolic risk biomarkers: Influence of socioeconomic status and lifestyle on two African-origin population groups, Cotonou (Benin) and Port-au-Prince (Haiti) Pan Afr. Med. J. 2016;24:306. doi: 10.11604/pamj.2016.24.306.8530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Clermont A., Sufra R., Pierre J.L., Mourra M.N., Fox E.L., Rouzier V., Dade E., St-Preux S., Inddy J., Erline H., et al. Dietary Risk Factors for Cardiovascular Disease among Low-Income Haitian Adults: Findings from a Population-Based Cohort. Nutrients. 2022;14:789. doi: 10.3390/nu14040787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Castillo D.C., Ramsey N.L., Yu S.S., Ricks M., Courville A.B., Sumner A.E. Inconsistent Access to Food and Cardiometabolic Disease: The Effect of Food Insecurity. Curr. Cardiovasc. Risk Rep. 2012;6:245–250. doi: 10.1007/s12170-012-0236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu Y., Eicher-Miller H.A. Food Insecurity and Cardiovascular Disease Risk. Curr. Atheroscler. Rep. 2021;23:24. doi: 10.1007/s11883-021-00923-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thomas M.K., Lammert L.J., Beverly E.A. Food Insecurity and its Impact on Body Weight, Type 2 Diabetes, Cardiovascular Disease, and Mental Health. Curr. Cardiovasc. Risk Rep. 2021;15:15. doi: 10.1007/s12170-021-00679-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.The United Nations World Food Programme . Haiti Country Strategic Plan (2019–2023) World Food Programme; Rome, Italy: 2019. [Google Scholar]
- 60.Romanello M., Di Napoli C., Drummond P., Green C., Kennard H., Lampard P., Scamman D., Arnell N., Ayeb-Karlsson S., Ford L.B., et al. The 2022 report of the Lancet Countdown on health and climate change: Health at the mercy of fossil fuels. Lancet. 2022;400:1619–1654. doi: 10.1016/S0140-6736(22)01540-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.World Bank. IFC. MIGA . World Bank Group Climate Change Action Plan 2016–2020. World Bank; Washington, DC, USA: 2016. [Google Scholar]
- 62.Rothman K.J. BMI-related errors in the measurement of obesity. Int. J. Obes. 2008;32((Suppl. S3)):S56–S59. doi: 10.1038/ijo.2008.87. [DOI] [PubMed] [Google Scholar]
- 63.Swainson M.G., Batterham A.M., Tsakirides C., Rutherford Z.H., Hind K. Prediction of whole-body fat percentage and visceral adipose tissue mass from five anthropometric variables. PLoS ONE. 2017;12:e0177175. doi: 10.1371/journal.pone.0177175. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data contain potentially identifying and sensitive patient information. Deidentified data used for this analysis are available upon request after signing a data access and use agreement, provision of approval by the GHESKIO ethics board, and demonstration that the external investigative team is qualified and has documented evidence of human research protection training. Requests may be addressed to the authors or to irb@med.cornell.edu.