Abstract
With the support of modern biotechnology, vaccine technology continues to iterate. The safety and efficacy of vaccines are some of the most important areas of development in the field. As a natural substance, chitosan is widely used in numerous fields—such as immune stimulation, drug delivery, wound healing, and antibacterial procedures—due to its good biocompatibility, low toxicity, biodegradability, and adhesion. Chitosan-based nanoparticles (NPs) have attracted extensive attention with respect to vaccine adjuvants and delivery systems due to their excellent properties, which can effectively enhance immune responses. Here, we list the classifications and mechanisms of action of vaccine adjuvants. At the same time, the preparation methods of chitosan, its NPs, and their mechanism of action in the delivery system are introduced. The extensive applications of chitosan and its NPs in protein vaccines and nucleic acid vaccines are also introduced. This paper reviewed the latest research progress of chitosan-based NPs in vaccine adjuvant and drug delivery systems.
Keywords: chitosan, chitosan-based nanoparticles, vaccine adjuvant, delivery system
1. Introduction
Vaccines are biological products made from pathogenic microorganisms and parasites and their components or metabolites [1]. Vaccination can prevent and control the spread of infectious diseases by generating a sufficient protective immune response, which greatly reduces mortality and extends life expectancy [2]. Traditional vaccines, such as live attenuated vaccines, can elicit strong immune responses but present significant safety concerns. The safety of inactivated vaccines far superior, but their immune effects are poor [3,4,5]. Novel vaccines, such as subunit vaccines, can contain one or more protective antigens, but one of their disadvantages is low immunogenicity [6,7,8,9,10]. Nucleic acid vaccines include DNA vaccines and mRNA vaccines. DNA vaccines are relatively simple to construct and easy to produce on a large scale, but they have low immunogenicity due to the low rate of transfection and subsequent protein expression [11,12,13]. mRNA vaccines can be directly translated into the cytoplasm without concern for insertional mutagenesis and can be transiently expressed, possessing high transfection efficiency, fast production, relatively low cost, and versatility regarding vaccine design [11,14]. However, they are unstable, prone to degradation in the body, and lack an effective delivery vehicle [15,16,17]. Based on the characteristics of various vaccines, we summarize the advantages and disadvantages of several existing vaccines in Table 1.
Table 1.
Preparation, advantages, and disadvantages of existing vaccines.
| Existing Vaccine | Preparation | Advantages | Disadvantages | References |
|---|---|---|---|---|
| Attenuated vaccines | Produced from pathogenic isolates via serial passage in embryonated, specific, pathogen-free eggs | Cause a strong immune response; long-lasting immune response; can survive the low-pH enzymatic environment of the stomach | Risk of toxic recovery in immunocompromised individuals; low safety profile | [3,4] |
| Inactivated vaccines | Formaldehyde inactivates live virus production | Compared with live attenuated vaccines, the safety is improved, and the production process is mature | Weak immune response; short duration; destruction or alteration of antigens; high cost; multiple vaccinations required | [4] |
| Subunit vaccines | Antigenic proteins from pathogens | High safety; modulated immune response; clear target antigen | Low immunogenicity | [4,5,6,7] |
| DNA vaccines | Transfection of DNA encoding a certain antigenic protein into animal cells | Simple to build; easy to mass-produce; high security and high stability | Cannot be used in humans; naked-pelleted DNA has low immunogenicity | [8,9,10,11] |
| mRNA vaccines | Transfection of RNA encoding a certain antigenic protein into animal cells | High transfection rate and simple process | Unstable; lack of effective delivery vehicles in vivo | [8,14,15,16,17,18,19] |
Traditional vaccination mainly relies on two specific types of microbiological preparations (attenuated and inactivated) to develop vaccines. Advances in vaccine technology fields have provided alternative methods of developing safer and improved vaccines, such as subunit vaccines, recombinant vaccines, and nucleic acid vaccines. Subunit vaccines and nucleic acid vaccines, as emerging platforms, have low toxicity and a long-expression time but also suffer from low immunogenicity and low efficacy. Therefore, there is an urgent need to develop new vaccine adjuvants and delivery systems to increase the enormous potency of vaccines. Nowadays, the research and development of nano-biomaterials and the advancement of molecular biotechnology play important roles in the rational design of vaccines and in our understanding of the molecular mechanism of immune response [2,7].
Chitin is obtained from the exoskeletons of crustaceans and insects and is also a significant component of the bodies of fungi, yeasts, algae, and other lower plants’ cell walls [20,21]. Chitosan is the product of the removal of part of the acetyl group from the natural polysaccharide chitin ((1-4)-2-acetamido-2-deoxy-β-d-glucan). Chemically, chitosan (α-(1-4)-2-amino-2-deoxy-β-d-glucan) is the second most abundant polysaccharide in nature, which is composed of glucosamine and N-acetyl-d-glucosamine linked with a β-1-4-glycosidic linkage [22]. Chitosan has numerous properties, such as low-toxicity, biodegradability, and antibacterial activity, and it has been extensively studied for its biomaterial properties and use in various areas such as drug delivery, cosmetics, vaccines, antibacterial agents, and antifungal procedures [20,23]. However, because of chitosan D-glucosamine residue and a high degree of crystallinity in intermolecular and intramolecular hydrogen bonds, chitosan can only be dissolved in most diluted acids (hydrochloric acid, nitric acid, and other inorganic acids or most organic acids), and it is insoluble in neutral and alkali solutions, which limits its applications [20,22].
Therefore, it is important to improve the water solubility of chitosan. To overcome this shortcoming, researchers have proposed various methods to modify chitosan to improve its solubility. At present, the common method is to chemically modify chitosan using, for example, quaternization, alkylation, phosphorylation, acylation, etc. Modified chitosan maintains its desirable properties; moreover, it also has good water solubility due to the loss of its crystallization ability resulting from the hydrogen bond in the amino position. The increase in the positive charge of the modified chitosan provides it with good mucoadhesive and antibacterial properties. In addition, its cytotoxicity is reduced, and its immunogenicity is enhanced [24,25,26].
Currently, chitosan and its derivatives have been widely researched due to their significant characteristics [27,28,29]. Numerous studies have demonstrated that they are promising vaccine adjuvants and delivery vehicles due to their high positive charge and their ease in crossing biological barriers, which can effectively bind drugs and cells [30,31,32,33,34,35,36]. For example, compared with an avian influenza virus vaccine loaded with chitosan, an avian influenza virus vaccine encapsulated in chitosan NPs can stimulate lymphocyte proliferation [37]. A chitosan-derived-nanoparticle-loaded Newcastle disease virus (NDV) vaccine can also better enhance mucosal immune responses and antibody immune responses compared with the traditional NDV vaccine [38]. N-2-Hydroxypropyl trimethyl ammonium chloride chitosan (N-2-HACC) and N, O-carboxymethyl chitosan (CMCS) are two of the most effective chitosan derivatives. To further improve chitosan derivatives properties, our group synthesized N-2-HACC/CMCS NPs that retain chitosan’s desirable properties and are soluble in common organic solvents and water. The chitosan derivative’s NPs were used as adjuvants and delivery carriers for vaccines that protect against Newcastle disease and infectious bronchitis. The results showed that N-2-HACC/CMCS NPs can induce higher levels of anti-NDV IgG and anti-IBV IgG antibodies and higher levels of IL-2, IL-4, and IFN-γ [39,40,41]. Poly-ε-caprolactone (PCL)/chitosan NPs, an adjuvant for the hepatitis B surface antigen (HBsAg), can promote a cellular immune response against HBsAg, characterized by the production of IFN-γ and IL-17 [42]. Chitosan nanoparticles containing fusion protein (Hspx-PPE44-EsxV; HPE) and resiquimod adjuvant (HPERC) employed as a vaccine in BALB/c mice could produce significant amounts of IFN-γ, IL-17, and IgG2a [43].
Here, we focus on the potential of chitosan and its derivatives as adjuvants and delivery vehicles, and, subsequently, we will elucidate their preparation methods, immune mechanisms, and applications in detail for vaccine development.
2. Vaccine Adjuvant and Delivery System
An adjuvant is an essential component of a vaccine, and the delivery system is designed to improve vaccines’ effectiveness by delivering antigens to target organs or cells [44]. Ideal vaccine delivery systems can not only deliver and protect antigens but also act as adjuvants [45,46,47].
2.1. Vaccine Adjuvant
The vaccine adjuvants in development or use mainly include aluminum salts, oil emulsions, saponins, immune-stimulating complexes, liposomes, microparticles, nonionic block copolymers, polysaccharides, cytokines, and bacterial derivatives. For example, liposomes can target immune cells, cause lysosome escape, and promote antigen cross-presentation, thereby greatly improving vaccine efficacy; polysaccharides can activate the complement system and enhance the function of macrophages and natural killer cells to enhance the host’s immune defense; aluminum adjuvant agents have depot effects and prophagocytic effects and activate the pro-inflammatory NLRP3 pathway, stimulating innate and adaptive immune responses and activating the complement system; and saponins enhance CD4+ T cell-mediated immune and antibody responses and can also cause antigen cross-presentation. Details of the classification and mechanisms of vaccine adjuvants are shown in Table 2.
Table 2.
Classification and mechanisms of vaccine adjuvants.
| Classification | Subdivision | Example | Mechanism |
|---|---|---|---|
| Inorganic | Aluminum salt | Aluminum hydroxide; Alhydrogel; Aluminum phosphate; Adju-Phos; Merck aluminum; AAHSA; Nano aluminum | Prolonged interactions between antigens and immune cells; prophagocytosis; induction of Th2 immune-biased responses; activation of the pro-inflammatory NLRP3 pathway [45,48] |
| Calcium salt | Calcium phosphate; Calcium phosphate NPs | Induces a more balanced Th1 and Th2 immune response [49] | |
| Other inorganic substances | Mn2+ | Enhancement of immune responses through the STING pathway in dendritic cells [50] | |
| Organic matter | Oil-in-water emulsion | MF59; AS03; AF03; SE | Induction of a Th2 immune bias response; local activation of the innate immune system [51] |
| Bacterially derived molecules | Monophosphoryl lipid A (MPL); Pyranose-based lipid adjuvant (GLA); RC529; CpG; stable toxin (LT); Cholera toxin (CT); TDB; Flagellin | Activates Toll-like receptor 4; triggers cells expressing Toll-like receptor 9 (including human plasmacytoid dendritic cells and B cells); induces Th1/Th2/Th17 responses; promotes dendritic cell uptake and maturation; activates the ERK1/2 pathway via PLC-γ1/PKC signaling [52,53,54,55,56,57,58,59] | |
| Virus-derived molecules | Poly I: C | Activation of TLR3; melanoma differentiation-associated gene 5 (MDA-5); cellular immunity and type I interferon response [60] | |
| Plant-derived molecules | QS21; Delta inulin | Promotes CD4+ T cell-mediated immune responses; induces a more balanced Th1/Th2 response [61,62]. | |
| Endogenous molecules | Cytokine | Activates dendritic cells [63] | |
| Synthesis of artificial small molecules | Imiquimod; R848; Cyclosporine | Activates TLR7/8 receptors and T cell co-stimulator CD40 [64,65] | |
| Composite adjuvant | Aluminum-based composite adjuvant | AS04 | Rapidly triggers local and transient cytokine responses to enhance humoral and cell-mediated responses, resulting in increased activation of antigen-presenting cells and promoting antigen presentation in CD4+ T lymphocytes [66] |
| Emulsion-based compound adjuvant | AS02 (AS03 + MPL+QS21), GLA-SE | Activation of TLR-4 regulates immune homeostasis and promotes Th1-type immune responses [67] | |
| Lipid group compound adjuvant | AS01 (liposome+MPL+QS21); AS15 (AS01+CpG); ISCOMs | Effectively promotes CD4+ T lymphocyte-mediated immune response [68] | |
| Polymer particles | CaCO3-LNT; Chitosan | Enhances the expression of MHC-II and CD86 in dendritic cells and increases the ratio of CD4+ to CD8+ T lymphocytes; provides a depot for the antigen to slowly release; facilitates the antigen’s targeting of immune cells; improves phagocytosis, modulation, and enhancement of the immune response induced by the antigen alone [69,70,71]. | |
2.2. Vaccine Delivery System
Vaccine delivery systems, including viral vectors, polymeric microparticles/NPs, liposomes, and other microparticles or NPs, can protect the antigens encapsulated in NPs from degradation. A vaccine delivery carrier mainly includes viral vectors and non-viral vectors [72,73,74,75,76].
2.2.1. Viral Carrier for the Delivery of Vaccine
COVID-19 is a major infectious disease that emerged in 2019. Due to the rapid mutation rate of the new coronavirus, vaccination for the infection’s prevention and treatment is integral. The high level of antigen expression produced by viral vectors lays the foundation for modern vaccine development. Viral vectors have high transduction efficiency and a wide host range [77,78,79]. However, their use is limited by toxicity and safety concerns [80,81]. Moreover, large-scale optimization is not possible due to concerns regarding reproducibility, immunogenicity, potential carcinogenicity, and the inflammation of viral vectors [82,83,84]. The viral vectors for improving the immunogenic effect of COVID-19 vaccines include adenovirus vectors, vaccinia virus vectors, measles virus vectors, rhabdovirus vectors, influenza virus vectors, and lentiviral vectors. Among them, adenoviral vectors are the most commonly used and effective, and other viral vectors are in clinical development [77,79].
Vaccines based on retroviral vectors are stably integrated into the host genome with high gene transduction efficiency. However, once infected, the probability of eradicating the virus is very low. There are studies suggesting that simple, retrovirus-based vectors could be used in gene therapy in the future [85,86]. Vaccines based on herpes simplex virus vectors can enhance the cellular, and humoral immune responses. Herpes simplex virus vaccines are rarely used in clinical practice, though one study pointed out that the combination vaccine method can improve its treatment effectiveness. However, it is highly cytotoxic [75,87,88]. The adenoviral vector vaccine induces moderate innate immunity and is highly thermostable. However, one of its disadvantages is that it can cause acute liver toxicity. It is used to prevent infectious diseases, including the Ebola virus disease, acquired immunodeficiency syndrome (AIDS), and COVID-19 [89,90,91]. Vaccines based on lentiviral vectors induce durable humoral immunity but are prone to insertional mutagenesis and have low viral titers, which easily degrade. The adenoviral vector vaccine can be used effectively in preclinical and clinical settings as a vector for gene therapy or vaccine applications (Table 3) [92,93].
Table 3.
Viral vectors and their advantages and disadvantages.
| Virus Vectors | Advantages | Disadvantages | References |
|---|---|---|---|
| Retroviral-vector-based vaccines | Stable integration into the host genome; high gene transduction efficiency | Once infected, the likelihood of eliminating the virus is low | [86] |
| Herpes simplex virus vector vaccine | Enhances cellular and humoral immunity; Induces lasting immune response. | High cytotoxicity | [75,88,89] |
| Adenovirus vector vaccine | Induces moderate innate immunity; high thermal stability | Cause acute hepatotoxicity | [90,91,92] |
| Lentiviral vector vaccine | Induces durable humoral immunity | Insertional mutagenesis; yields low viral titers; easily degradable | [93,94] |
2.2.2. Nonviral Carriers for the Delivery of Vaccines
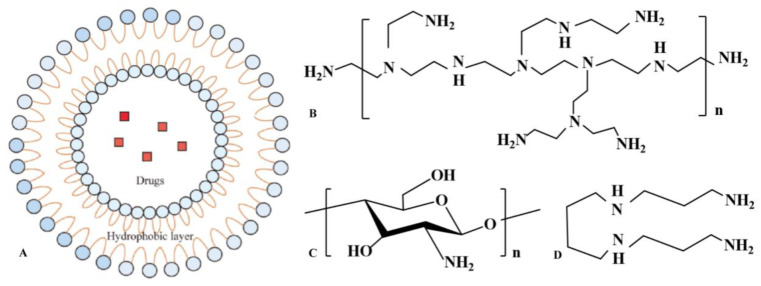
The nonviral carriers used for the delivery of vaccines are easy to prepare and have low toxicity, which has attracted widespread attention. Figure 1 shows the structures of nonviral vectors that have been frequently studied in recent years [76,95,96]. Chitosan-based delivery systems have been shown to have mucoadhesive properties, and they have the unique ability to open tight junctions between natural portal epithelial cells and can promote antigen transport through another effective antigen delivery pathway, thereby stimulating powerful immune responses [22].
Figure 1.
Well-studied nonviral vectors. (A). liposome; (B). polyethyleneimine; (C). chitosan; (D). spermine.
Chitosan is a promising nonviral delivery vector because of its biocompatibility, biodegradability, low immunogenicity, and ease of manufacture. It can effectively enhance both humoral and cellular immunity, and even mucosal immune responses. Chitosan nano-vaccines are efficient carrier systems for pIL-12, and combined with HBsAg, they can induce higher levels of anti-HBsIgG, IgG1, and IgG2b; promote the maturation and presentation of dendritic cells; and enhance HBV-specific CD8+ and CD4+ T lymphocyte responses [97]. The N-(2-hydroxy-3-trimethyl ammonium) propyl chitosan NPs used as adjuvants for anthrax vaccine adsorption strongly stimulate humoral immunity. By using it, the level of anti-protective antigen titers in mice were significantly increased, and the survival rate was significantly improved [98]. It was difficult for macrophages to absorb Salmonella typhi porin; however, it was significantly absorbed by macrophages and increased the release rate of TNF-α and IL-6 after being combined with chitosan [99]. When chitosan was used in combination with IFN-β, IgG, and IgA antibodies, mucosal IgA antibodies and antitoxin titers were all stronger than those using IFN-β alone as a mucosal adjuvant [100].
Chitosan-based NPs have advantages as nonviral carriers for the delivery of vaccines [101]. Compared with monolayer-shaped liposome NPs, chitosan-based NPs have larger shapes due to the aggregation of small particles, which are more favorable for antigen delivery. For example, chitosan and liposomal NPs used as auxiliary co-delivery agents can enhance the production of IgG-class antibodies compared to liposomal NPs [102]. Chitosan-based NPs can deliver antigens and provide noninvasive routes of administration, such as oral, nasal, muscular, and ocular pathways.
The pathogens delivered by chitosan and its nanocomplexes via ocular, oral, intranasal, and intramuscular routes in recent years are shown in Table 4. It has been shown that the opening of tight junctions between chitosan cells favors the paracellular transport of hydrophilic macromolecular drug macromolecules such as peptides and proteins [103,104]. Oral vaccines are the easiest route of administration with the least risk of contamination. However, due to the influence of the gastrointestinal environment, protein antigens are inactive and have poor absorption properties as well as low bioavailability. Chitosan mesoporous silica NPs have potential as oral vaccine carriers. The NPs effectively protect proteins from degradation due to pepsin and trypsin. Plasmid DNA containing lymphovirus genes was encapsulated in chitosan-based microspheres, which also prevented the hydrolytic denaturation of DNA vaccines in the gastrointestinal tract [104,105]. The cross-presentation of foreign antigens is a prerequisite for cytotoxic T lymphocyte responses. Chitosan/calcium phosphate nanosheets are used as vaccine carriers to effectively cross-present exogenous antigens. The water solubility of chitosan greatly limits its application as a delivery vehicle [106]. An antigen-coated with n-phosphochitosan not only solves the problem of water solubility but also significantly improves the level of the antigen-specific immune response, and it can be used as an antigen carrier for immune prevention and treatment [107].
Table 4.
A summary of chitosan and its nanocomplexes for pathogen delivery.
| Immunization Pathway | Pathogens |
|---|---|
| Intramuscular immunization | Chlamydia [108], Mycoplasma [109], Influenza virus [65], Bacillus anthracis [110], Mycobacterium tuberculosis [111], HIV [112] Treponema pallidum [113], Herpes virus [75], Japanese encephalitis virus [114], Cholera virus [115], Avian influenza virus [37], Edwardsiella tarda [116] |
| Intranasal immunization | Campylobacter jejuni [117], Foot-and-mouth disease [118], PR8 influenza virus [119], Escherichia coli [87], Diphtheria toxin [120], Influenza A virus [119], Newcastle disease virus [9], Streptococcus pneumoniae [121], Coxsackievirus [122], Vibrio cholerae [123] |
| Oral immunization | Salmonella [99], Brucella [124], Hepatitis B virus [21], Recombinant enterovirus [125], Koi herpesvirus [126], Schisoma mansoni [127], Vibrio cholerae [123], tetanus toxoid [128], diphtheria toxin [129], Schistosomiasis [130] |
| Ocular immunization | Cyclosporin A [131], Herpes simplex virus [132] |
| Subcutaneous immunization | Hepatitis B virus [133], Hepatitis B surface antigen [134], Mycoplasma pneumoniae [135], E. Coli [136], Tetanus toxoid [137], Toxoplasma gondii histones [138], Echinococcus granulosus [139], Influenza virus [37], Leishmania antigen [140], Mycobacterium tuberculosis [141] |
3. Preparation of Chitosan-Based NPs for Vaccine Delivery
Chitosan-based NPs can be prepared for vaccine delivery using both physical and chemical methods. Although both methods have pros and cons, the physical methods used to yield particles are preferred over chemical crosslinking methods because the proteins are chemically modified with crosslinking agents, proteins are degraded in organic solvents, and it is difficult to remove the unreacted crosslinkers from the formulations. The ion-crosslinking method uses the positive charge of chitosan and other negatively charged substances as part of an electrostatic effect in order to prepare NPs. The cross-linking agent used has low toxicity and avoids the toxicity caused by the use of organic solvents [142]. Polyelectrolyte recombination is caused by the interaction between polyelectrolytes with opposite charges. This method also does not use a chemical crosslinking agent, and its process is simple, but its stability is easily affected by pH, thus affecting the charge and size of the NPs [143,144]. The desolvation method uses the insolubility of chitosan in an alkaline medium to form sediment. Its nanoparticle formation rate is high, but the nanoparticles produced are large [145]. The emulsification method is based on the method of removing the organic solvent and comprises techniques such as the emulsification solvent evaporation method and the emulsification solvent diffusion method [146]. This method is simple, but if the organic solvent is not completely removed, it will affect cells and tissues. In addition, the selection of the surfactant has a great impact on the stability of the system [147,148,149,150]. The spray-drying method is used to dissolve and disperse chitosan in an acidic solution, and then spray it in a hot gas flow to rapidly evaporate the solvent into gas [151,152]. This method is simple, but the size of the NPs is not easy to control. The covalent cross-linking method [153,154] uses the formation of covalent bonds between chitosan NPs and cross-linking agents. The cross-linking agents used in the preparation process are highly toxic. The reverse micelle method involves grafting chitosan and lipophilic substances, with the graft copolymer dispersed in an organic solvent, which is a process that is simple to carry out. However, the use of some organic solvents has certain toxic effects on cells [155]. Here, various antigen formulation techniques are discussed, such as ionic crosslinking, polyelectrolyte complexation, spray drying, reverse micellization, covalent crosslinking, and so on. Ion crosslinking is one of the most widely used methods for the preparation of chitosan NPs (Table 5). Each method, of which ionic crosslinking method is the most commonly used, has advantages and disadvantages. Schematic diagrams of these methods and preparation procedures can be found in the literature [156].
Table 5.
Preparation methods of chitosan NPs.
| Preparation Methods | Mechanism | Advantages | Disadvantages |
|---|---|---|---|
| Ion crosslinking [142] | Interaction between crosslinking agent and the amino or carboxyl groups of chitosan NPs. | The preparation process itself has no organic solvent; the reaction conditions are simple, mild, and controllable. | Not completely immune to gastric acid degradation; low solubility. |
| Polyelectrolyte complexation [143,144] | Interactions between oppositely charged polyelectrolytes. | Two- or three-step process; the equipment requirements are not demanding, and the conditions are mild. | Stability is susceptible to pH. |
| Desolvation [145] | Insolubility of chitosan in alkaline media. | High nanoparticle formation rate; improved physical stability. | Inhomogeneous distribution of NPs; difficulty in synthesizing smaller-sized chitosan NPs. |
| Emulsification [146,147,148,149,150] | The oil and water phases are emulsified; then, the solvent is removed. | Two- to three-step process; no need for sonication or homogenizers. | Causes significant toxicity to tissues or cells; poor stability. |
| Spray drying [151,152] | Amino groups can be protonated by acids. | Re-dispersibility; enables easier synthesis of smaller sizes compared other methods; low toxicity. | The particle size is not easy to control; the particles are irregularly shaped and sticky. |
| Covalent crosslinking [153,154] | Formation of covalent bonds between chitosan NPs and crosslinking agents. | Controllable drug release. | Cytotoxic. |
| Reverse micelle [153,155] | Trans-interaction between chitosan NPs and crosslinking agent. | One-step process; good dispersion. | Causes significant toxicity in tissues or cells. |
Moreover, many factors can influence the effects of vaccine adjuvants and delivery systems. For example, the size of the NPs will affect their absorption in the body, the particle size will affect the transmembrane transport ability of the NPs, and the positive charge characteristic of chitosan will easily interact with negatively charged surfaces (such as mucous membranes), thereby influencing the immune effect [157]. Among the current methods for preparing NPs, some are toxic to cells due to their use of organic solvents. The removal of organic solvents is very important. In addition, the selection of surfactants also has a great influence on the particle size, morphology, and stability of NPs, so the research and development requirements of surfactants are becoming more stringent in order to enable the application of nanomaterials in different fields. In the development of chitosan derivatives, using different chemical reagents to synthesize NPs will produce different degrees of toxicity. In addition, preclinical studies need to evaluate the safety of chitosan-based nanocarriers. Therefore, an appropriate synthesis method must be selected according to the different applications of the NPs, and more non-toxic NPs should be prepared [158].
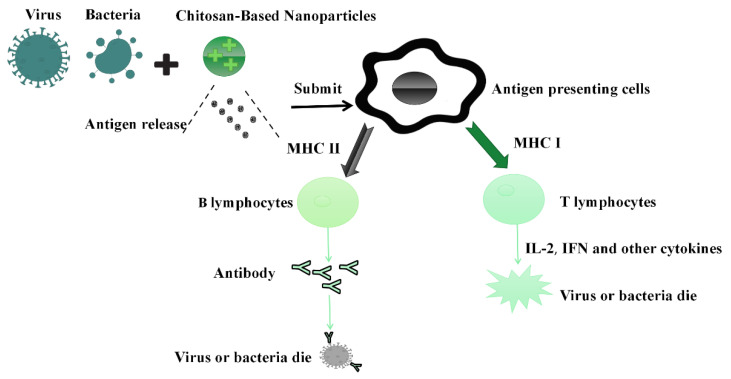
4. Immune Mechanism of Chitosan and Its Nanocomposites as the Vaccine Adjuvants/Delivery System
The immune enhancement mechanism of chitosan NPs mainly includes its effect on the antigen, enhancing the targeting of antigen-presenting cells, and provoking macrophages to secrete related inflammatory factors and regulate Th1/Th2 propensity to regulate the immune response. Since antigens are negatively charged, chitosan NPs readily bind to antigens for the purposes of storing and slowing antigen release and activating antigen-presenting cells to make Th1/Th2 responses more balanced for use as vaccine adjuvants/delivery systems [159,160,161]. NPs can enhance cell-mediated immune responses as well as humoral immune responses. In addition, they induce superior uptake via antigen-presenting cells because of their positive charge and their ionic interactions with negatively charged cell membranes (Figure 2) [161,162,163]. The chemical modification of chitosan can also enhance the immune effects of vaccines. For example, N,N,N-trimethyl chitosan can induce the maturation of DCs and improve the cell uptake of vaccine antigens, while HTCC (or HACC) can induce the Th2 type response to reduce allergic reactions. N-phosphonium chitosan stimulates Th1 and Th2 responses; however, the secretion of IFN-γ and IL-12 is downregulated compared to the Freund’s adjuvant. Glycol chitosan induced stronger immune responses than chitosan NPs after nasal immunization, which suggests the GC NPs have the potential to become promising immune-related materials for mucosal administration [30].
Figure 2.
Immune mechanism of chitosan against viruses and bacteria.
The successful activation of antigen-presenting cells is a key factor in effective adjuvants/delivery systems. Chitosan allows antigen-presenting cells to deliver immunomodulatory molecules without causing adverse immune responses. Chitosan can promote dendritic cell maturation and enhances antigen-specific helper T cell 1 (ThA) responses by participating in the sting–cGAS pathway [67]. Ovalbumin (OVA)/Kirdran sulfate/O-HTCC NPs induce the activation and maturation of antigen-presenting cells, stimulate the proliferation and differentiation of lymphocytes, and induce higher levels of OVA-specific antibodies in mice [164]. Studies have also shown that O-Sulfate/o-quaternary chitosan NPs can efficiently enter swine macrophages, escape from lysosomes, promote cytokine production in immune cells, and activate PI3K/AKT and MAPK pathways, as well as promote lymphocyte proliferation, dendritic cell phenotypes, and functional maturation. Furthermore, chitosan can enhance the immunogenicity of the porcine circovirus vaccine against infectious pathogens that are associated with the over-expression of TLR2 and TLR4 in macrophages [165].
Chitosan and its nanocomposites can induce Th1/Th2 immune responses [166]. The Th1 immune response is a pro-inflammatory response produced by Th1 cells against intracellular microorganisms such as bacteria and viruses. The Th2 immune response is an anti-inflammatory response generated by Th2 cells against extracellular microorganisms. An excessive Th1 immune response can lead to an autoimmune response that then leads to uncontrolled tissue damage. The Th2 immune response can counteract the Th1 immune response. A balanced Th1/Th2 response is particularly important for the organism. Chitosan can promote balance in Th1/Th2 responses [25]. For example, the murine intranasal immunization of Brucella protein-loaded chitosan NPs produces Th1- and Th2-related antibodies. In one study, murine ovalbumin was encapsulated in chitosan NPs, which significantly promoted murine Th1 (IL-2 and IFN-γ) and Th2 (IL-10) cytokine production and triggered a balanced Th1/Th2 response [167,168]. Chitosan and c-di-GMP combinations skew cytokine responses toward a more balanced Th spectrum; the complexation of chitosan and heparin to prepare nano-vaccines induces strong immunity to Th1 responses, in addition to co-strong Th2 response activation; and the presence of chitosan redirects immune responses to a more balanced Th1/Th2 pathway compared to alum adjuvant [168]. Ghendon et al. used chitosan as an adjuvant of an H5 inactivated influenza vaccine. The results showed that an intramuscular injection could significantly improve antibody titer and protection efficiency and promote the increase in the number of CD3, CD3/NK, I-AK (MHCII), and H-2Db (MHCI) cells [169].
5. Application of Chitosan and Its Nanocomposites in Vaccine Delivery
5.1. Application in Protein Vaccine Delivery
Protein-encapsulated chitosan and its nanocomposite particles are being explored for a variety of biomedical applications. The size, morphology, and surface charges of NPs can modulate interactions with immune cells, which have a great influence on the immune response [170,171]. Chitosan NPs stimulate immune cells and have chemically modifiable active functional groups, all of which impart multiple advantages in vaccine delivery [95]. Nanoparticle carriers are used to transport antigenic proteins in vivo and can avoid proteolysis or the degradation of antigens. The alginate-chitosan-coated LDH nanocomposite (ALG–CHT-LDH) can effectively protect antigens from acidic degradation, significantly enhancing protein attachment and the internalization of proteins in enterocytes and macrophages, and it can be used as an oral protein vaccine carrier [172]. Oral immunization with recombinant bovine serum albumin conjugated to mannosylated chitosan NPs elicits strong systemic IgG antibody and mucosal IgA responses. The prepared NPs also reduce the effects of the gastric environment [173]. The positive charge on the nanoparticles’ surface also enhances immunogenicity. Kaneko et al. used chitosan hydrochloride to induce pneumococcal protein’s antigen expression. Negatively charged chitosan NPs generally exhibit lower immunogenicity compared with positively charged chitosan NPs, which may be related to differences in the surface charge [174].
Chitosan and its nanocomposites play an important role in the development of vaccines for animal diseases. Chitosan NPs efficiently deliver Salmonella subunit antigens via the oral route and increase the expression levels of TLRs, Th1, and Th2 cytokine mRNA in chicken immune cells [175]. Brucella is one of the most common zoonotic diseases. Compared with live attenuated vaccines, recombinant protein vaccines and subunit vaccines have been the focus of research in recent years regarding the prevention of brucellosis. Mannosylated chitosan NPs (MCN)—loaded with FliC protein as a targeted vaccine delivery system to develop subunit vaccines against brucellosis—could significantly enhance the immunogenicity of FliC protein’s highly specific IgG response and produce high levels of IFN-γ and IL-2 [176].
5.2. Application in Polypeptide Vaccine Delivery
Peptide-based vaccines have attracted enormous attention in recent years as one of the most effective disease prevention methods. However, peptide epitopes are weakly immunogenic and unstable. Nanoparticle adjuvants or delivery systems can induce highly durable immune responses against weakly immunogenic peptides [177]. A polyglutamic acid–peptide conjugate and trimethyl chitosan were used to prepare a nanoparticle peptide vaccine that could effectively improve immunogenicity [178]. The conjugation of the unstable P10 peptide to chitosan NPs promoted immune responses with Th1 and Th2 [179]. A highly efficient dendritic-cell-targeted vaccine delivery system was developed by coupling a targeting peptide (TP) with chitosan. Compared with chitosan NPs, the TP-coupled chitosan NPs (TPC-NPs) have an increased ability to target DCs and have an enhanced immune function [180]. Table 6 briefly summarizes the application of chitosan and its nanocomposite particles in the delivery of protein vaccines and polypeptide vaccines in recent years.
Table 6.
Application of chitosan in protein vaccines and polypeptide vaccines.
| Chitosan Complex | Protein/Polypeptide | Immune Mode | Target Disease |
|---|---|---|---|
| Chitosan-modified silica NPs [104] | Bovine serum albumin | Oral | Not mentioned |
| Chitosan NPs [175] | Salmonella enteritidis outer membrane proteins (OMPs) and flagellin proteins | Oral | Brucellosis |
| Chitosan NPs [181] | Fusogenic protein p10 of avian reovirus (ARV-p10) | Intramuscular injection | Melanoma |
| Mannosylated chitosan NPs [176] | FliC antigen | Subcutaneous injection | Brucellosis |
| N-2-Hydroxypropyl trimethyl ammonium chloride chitosan [39] | Porcine parvovirusVP2 protein | Intramuscular injection | Porcine parvovirus disease |
| Mannose-conjugated chitosan [182] | SwIAV antigen | Intranasal | Swine influenza |
| Chitosan [183] | Recombinant protein Pac | Oral | Dental caries |
| Chitosan polymeric NPs [179] | P10 peptide | Intranasal | Paracoccidioidomycosis |
| Chitosan–PLGA NPs [184] | rOmp22 peptide | Subcutaneous injection | Acinetobacter baumannii |
| Trimethyl chitosan [178] | A. streptococcus peptide | Intranasal | Group A Streptococcus |
| Alginate/chitosan/alginate microcapsules [185] | Probiotic expressing M cell homing peptide | Oral | Not mentioned |
| Alginate–chitosan–PLGA complex [186] | Ac-PLP-BPI-NH2-2 peptide | Subcutaneous injection | Autoimmune encephalomyelitis |
| Alginate and trimethyl chitosan [187] | Lipopeptide | Oral | Group A Streptococcus |
| Trimethyl Chitosan NPs [188] | Malaria antigens | Intramuscular injection | Malaria |
| Chitosan [189] | Receptor-binding domain (RBD) polypeptides | Subcutaneous injection | SARS-CoV-2 |
| Chitosan-mannose NPs [190] | Recombinant Art v 1 wormwood pollen protein | Intramuscular, subcutaneous, subcutaneous injection | Allergic bronchial asthma |
5.3. Application in Nucleic Acid Vaccine Delivery
5.3.1. DNA Vaccines
DNA vaccines are a promising method for the treatment and prevention of diseases because of their safety (carrying only specific antigenic genetic information), stability, and the ease of their large-scale preparation and production. The coformulation of a gene delivery vehicle with an immunostimulant enhances the therapeutic efficacy of DNA vaccines [191]. Chitosan NPs as a nano-delivery system induce high levels of IFN-γ and IL-4 and enhance the effect of the DNA vaccine, and the effect is better than that of chitosan and IL-12 alone [192].
The COVID-19 pandemic has affected nearly 210 million people around the world. A variety of COVID-19 vaccines have been approved for human applications, including live attenuated and inactivated virus and protein subunit vaccines. The immune response to the intranasal delivery of the SC2-spike DNA vaccine, transported on a modified gold–chitosan nanocarrier, demonstrates strong and consistent antibodies (IgG, IgA, and IgM) and the effective neutralization of pseudoviruses expressing the S proteins of different SC2 variants (Wuhan, beta, and D614G) [193]. The pVAX1-constructed DNA vaccine can improve the survival rate of carp, goldfish, and other fish against Aeromonas hydrophila infection [194]. In addition, PLGA–chitosan NPs induce adaptive mucosal immunity in fish, and the mRNA expression levels of IgM, IgD, and IgT are significantly upregulated compared to pDNA–PLGA–NPs [195].
Infectious bronchitis (IB) is an important infectious disease in poultry. Chitosan saponin NPs can encapsulate monovalent and bivalent DNA vaccines developed based on the S1 glycoprotein of classical and variant IBV strains (M41 and CR88), resulting in high antibody titers as well as enhanced immunity ingenuity and protection in chickens [148]. Importantly, in comparison with inactivated vaccines, multiple booster vaccinations are not required to control poultry-infectious bronchitis. Our group prepared O-2′-hydroxypropyl trimethylammonium chloride chitosan containing NDV F gene plasmid DNA and the C3d6 molecular adjuvant, which induced higher levels of anti-NDV IgG and sIgA antibody titers and significantly promoted lymphocyte proliferation, producing higher levels of IL-2, IL-4, IFN-γ, CD4+, and CD8+ T lymphocytes [41]. The intranasal delivery of O-2′-HACC/pFDNA can enhance humoral, cellular, and mucosal immune responses and protect chickens against highly toxic NDV compared to commercial live attenuated NDV vaccines. The applications of several chitosan-based complexes in DNA vaccines are listed in Table 7, which indicates the great potential of chitosan and its NPs in DNA vaccines.
Table 7.
Application of chitosan-based complexes in DNA vaccines.
| Chitosan Complex | Causative Agent | Immune Animal or Model | Immunization Mode |
|---|---|---|---|
| Chitosan–saponin [196] | Avian infectious bronchitis virus | Chicken | Intramuscular injection |
| Chitosan–trimeric phosphate [194] | pVAX-OMP and pVAX-hly | Carp | Oral |
| Polylactic-co-glycolic acid-chitosan NPs [197] | Late-onset Edwardian spp. | Fish | Immunization by immersion |
| N-2-Hydroxypropyl dimethylethyl ammonium chloride chitosan NPs [38] | Newcastle disease virus | Chicken | Intranasal |
| Mannosylated chitosan [198] | Mycobacterium pneumonia | Mouse | Intranasal |
| N-2-HACC/CMCS NPs [40] | Newcastle disease virus | Chicken | Intranasal |
| Chitosan NPs [199] | Herpes simplex virus | Duck | Intramuscular injection |
| Chitosan NPs [200] | Hepatitis B antigen | Mouse | Intranasal |
| Chitosan NPs [201] | Helicobacter pylori | Mouse | Oral |
| Mannosylated chitosan NPs [202] | Mouth disease virus | Guinea pig | Intranasal |
5.3.2. RNA Vaccines
The development of delivery systems will address many of the problems inherent to in vivo RNA delivery to improve the key efficacy of RNA drugs. mRNA vaccines are more potent and specific than protein/peptide vaccines in stimulating humoral and cellular immune responses [203]. Studies have shown that mRNA vaccines can cross the mucosal barrier and rapidly adapt to future outbreaks of new infectious diseases [204]. However, their degradation rate in vivo is fast, and their transfection efficiency is low. mRNA is also easily degraded by nucleases during delivery. The most commonly used approach is to encapsulate mRNA in cationic NPs; for example, chitosan and its NPs can deliver immunogenic antigens to antigen-presenting cells [205].
Chitosan–alginate-gel-scaffold-mediated mRNA liposomes enable T cell proliferation and high levels of IFN-γ compared to the injection of naked mRNA or mRNA liposomes. The nature of RepRNA uptake by DCs is inefficient. The encapsulation of RepRNA into chitosan NPs has demonstrated its efficient delivery to DCs and the induction of immune responses in vivo [206]. Steinle et al. incorporated synthetic humanized Gaussian luciferase (hGLuc) mRNA into a chitosan–alginate hybrid hydrogel. mRNA-containing hydrogels can be used to deliver locally and continuously synthesized mRNA to cells within weeks with a potency of up to 21 days [207]. Mannosylated-chitosan-modified ethosomes loaded with mRNA can efficiently transfect DCs and induce their maturation. The results of one study showed that mannosylated-chitosan-modified liposome has a good targeting ability and can protect mRNA from being degraded. Its transdermal ability is a good vehicle for the targeted delivery of mRNA. Compared with traditional oral or injectable mRNA vaccines, transdermal immunization is also becoming increasingly extensive. Chitosan-modified vaccines can allow antigen molecules to easily enter the epidermis to activate dendritic cells [208].
mRNA vaccines are highly effective and safe for preventing COVID-19 according to clinical trials. mRNA-1273 and BNT162b2, two COVID-19 mRNA vaccines, are approved for use in the market. Moreover, four other COVID-19 mRNA vaccines are also in clinical trials, including ARCoV (Abogen, China), CvnCoV (CurVac, Germany), ARCT-021 (Arcturus, USA), LNP-nCoVsaRNA (Imperial College London, England), and ChulaCoV19 mRNA vaccines (Chulalongkorn University, Thailand) [209,210]. As we all know, an efficient in vivo delivery is critical for mRNA vaccines to achieve prophylactic relevance. Lipid nanoparticles (LNPs) are the most widespread platform and have been shown to present the best clinical outcomes in mRNA delivery. LNPs mainly consist of ionizable lipids, cholesterol, phospholipids, and polyethylene glycol (PEG) lipids. The ionizable lipids contain amine groups, which become cationic at a low pH and, therefore, can efficiently complex negatively charged mRNA. Once delivered into the endosomes of host cells, they are thought to be ionized negatively again upon acidification, which helps to induce hexagonal phase structures and, finally, facilitates the endosomal escape of mRNA into the cytoplasm. Phospholipids play a structural role in LNPs, assisting the formulation of LNPs and the disruption of the lipid bilayer to promote the endosomal escape of mRNA. Cholesterol serves as a stabilizing element in LNPs. Lipid-anchored PEGs dominantly deposit on the LNP surface as barriers to sterically stabilize the LNP and reduce nonspecific binding to proteins [211]. This biopolymer can be a potential biomacromolecule to be employed against the SARS-CoV-2 via the preparation of antiviral vaccines and adjuvants. We hope more research will focus on this excellent nanomaterial. Table 8 lists the applications of several chitosan based complexes in RNA vaccines.
Table 8.
Application of chitosan-based complexes in RNA vaccine.
| Chitosan Complex | Causative Agent | Diseases |
|---|---|---|
| Chitosan NPs [205] | Influenza H9N2 HA2 and M2e mRNA | Influenza |
| Chitosan NPs [206] | Influenza virus | Influenza |
| Chitosan–alginate hybrid hydrogel [207] | Synthetic mRNAs for tissue-engineering applications | Tissue-engineering applications |
| Mannosylated-chitosan-modified ethosomes [208] | Tyrosinase-related protein 2 | Melanoma |
6. Future Perspectives
Although the safety of subunit vaccines and nucleic acid vaccines has been greatly improved, their immunogenicity is low. The development of adjuvants and delivery systems is critical for the improvement of these vaccines. Natural polymer chitosan and its NPs have immunoreactive and mucosal adhesion properties, and they can also improve the stability and immunogenicity of the antigen. Since they stimulate the immune response and can achieve antigen-specific release through targeted delivery, chitosan and its nanocomposites have great potential as delivery systems [41,212,213]. At the same time, the application of chitosan and its complexes in nucleic acid vaccines is also increasing. Using chitosan and its nanoparticle complexes to interact with negative charges in capsid proteins via electrostatic interactions in order to cause structural damage to the virus could potentially treat COVID-19. In addition, the direct delivery of chitosan NPs to the lungs can also help with COVID-19 drug treatments. However, the physicochemical properties of chitosan, such as deacetylation, molecular weight, and systemic pH can affect antigen delivery. As a natural polymer, the toxicological issues of chitosan NPs are still a major concern. The toxicity of all chitosan derivatives in vivo should be investigated. Pre-clinical investigations are also needed to evaluate the bioactivity and safety of chitosan-based nanocarriers. Another major concern for chitosan and its derivatives is that their immunological profiles have not been studied thoroughly. When chitosan is used with some clinical drugs, some adverse reactions will occur. For example, the positive charge of chitosan can react with lipids and bile acids; affect the absorption of vitamin A, D, E, and K; and thus enhance the anticoagulation effect of warfarin [214]. The mucosal adhesion properties of chitosan can prevent acyclovir from being transported through the gastrointestinal tract [215]. Huang et al. demonstrated that chitosan particles had a significant proinflammatory effect on lung tissue after being inhaled into the lungs [216]. Therefore, the studies of chitosan and its nanoparticle complexes are in the experimental stage and have not yet been applied in clinics.
During the synthesis of chitosan, temperature, time, and the repetition of the alkali step all affect the degree of deacetylation, which, in turn, affects the synthesis of chitosan. It is necessary to optimize the synthesis conditions of chitosan to reduce the error between batches of chitosan. Chitosan’s solubility can be increased by modifying it to form new derivatives. The delivery mechanism of chitosan and its NPs in vivo should also be further explored with the support of modern biotechnology. In conclusion, chitosan and its NPs have great potential and greater development prospects for vaccine delivery.
Author Contributions
K.Z. and X.G. designed and conceived the manuscript. X.G. and Y.G. conducted the article writing work under the supervision of K.Z. K.Z., X.G., Y.G., J.S. and C.Z. revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no competing financial interest.
Funding Statement
This work was supported, in part, by the “Pioneer” and “Leading Goose” R&D Programs of Zhejiang (2022C02031), the Natural Science Foundation of Heilongjiang Province (LH2020H129), the Natural Science Foundation of Zhejiang Province (LTY22E030002), and the Taizhou Science and Technology Plan Project in 2022 (22nya04).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wan X., Yin Y., Zhou C., Hou L., Cui Q., Zhang X., Cai X., Wang Y., Wang L., Tian J. Polysaccharides derived from Chinese medicinal herbs: A promising choice of vaccine adjuvants. Carbohydr. Polym. 2022;276:118739. doi: 10.1016/j.carbpol.2021.118739. [DOI] [PubMed] [Google Scholar]
- 2.Sun B., Yu S., Zhao D., Guo S., Wang X., Zhao K. Polysaccharides as vaccine adjuvants. Vaccine. 2018;36:5226–5234. doi: 10.1016/j.vaccine.2018.07.040. [DOI] [PubMed] [Google Scholar]
- 3.Tlaxca J.L., Ellis S., Remmele R.L. Live attenuated and inactivated viral vaccine formulation and nasal delivery: Potential and challenges. Adv. Drug Deliv. Rev. 2015;93:56–78. doi: 10.1016/j.addr.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 4.Guan L.J., Pei S.X., Song J.J., Zhan P.F., Han Y.N., Xue Y., Ding K., Zhao Z.Q. Screening immune adjuvants for an inactivated vaccine against Erysipelothrix rhusiopathiae. Front Vet. Sci. 2022;9:922867. doi: 10.3389/fvets.2022.922867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seo S.U., Seong B.L. Prospects on repurposing a live attenuated vaccine for the control of unrelated infections. Front Immunol. 2022;13:877845. doi: 10.3389/fimmu.2022.877845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Herck S., Feng B., Tang L. Delivery of sting agonists for adjuvanting subunit vaccines. Adv. Drug Deliv. Rev. 2021;179:114020. doi: 10.1016/j.addr.2021.114020. [DOI] [PubMed] [Google Scholar]
- 7.Bose R.J., Kim M., Chang J.H., Paulmurugan R., Moon J.J., Koh W.-G., Lee S.-H., Park H. Biodegradable polymers for modern vaccine development. J. Ind. Eng. Chem. 2019;77:12–24. doi: 10.1016/j.jiec.2019.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pirahmadi S., Afzali S., Zargar M., Zakeri S., Mehrizi A.A. How can we develop an effective subunit vaccine to achieve successful malaria eradication? Microb. Pathog. 2021;160:105203. doi: 10.1016/j.micpath.2021.105203. [DOI] [PubMed] [Google Scholar]
- 9.Mohebbi A., Ebrahimzadeh M.S., Baghban-Rahimi S., Saeidi M., Tabarraei A., Mohebbi S.R., Shirian S., Gorji A., Ghaemi A. Non-replicating newcastle disease virus as an adjuvant for DNA vaccine enhances antitumor efficacy through the induction of TRAIL and granzyme B expression. Virus Res. 2019;261:72–80. doi: 10.1016/j.virusres.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 10.Gumina E., Hall J.W., Vecchi B., Hernandez-Velasco X., Lumpkins B., Mathis G., Layton S. Evaluation of a subunit vaccine candidate (Biotech Vac Cox) against Eimeria spp. in broiler chickens. Poult. Sci. 2021;100:101329. doi: 10.1016/j.psj.2021.101329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eusébio D., Neves A.R., Costa D., Biswas S., Sousa N. Methods to improve the immunogenicity of plasmid DNA vaccines. Drug Discov. Today. 2021;26:2575–2592. doi: 10.1016/j.drudis.2021.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Watanabe Y., Takada Y., Kotake M., Zenke K., Itoh N., Yoshinaga T. Evaluation of the protective effects of DNA vaccines encoding an infection-related cysteine protease from Cryptocaryon irritans, the pathogenic organism of cryptocaryoniasis. Aquaculture. 2021;548:737641. doi: 10.1016/j.aquaculture.2021.737641. [DOI] [Google Scholar]
- 13.Zhou Z., Zhang X., Li Q., Fu L., Wang M., Liu S., Wu J., Nie J., Zhang L., Zhao C., et al. Unmethylated CpG motif-containing genomic DNA fragments of Bacillus Calmette-guerin improves immune response towards a DNA vaccine for COVID-19. Vaccine. 2021;39:6050–6056. doi: 10.1016/j.vaccine.2021.08.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gerhardt A., Voigt E., Archer M., Reed S., Larson E., Van Hoeven N., Kramer R., Fox C., Casper C. A flexible, thermostable nanostructured lipid carrier platform for RNA vaccine delivery. Mol. Ther. Methods Clin. Dev. 2022;25:205–214. doi: 10.1016/j.omtm.2022.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.He Q., Gao H., Tan D., Zhang H., Wang J.-Z. mRNA cancer vaccines: Advances, trends and challenges. Acta Pharm. Sin. B. 2022;12:107020. doi: 10.1016/j.apsb.2022.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maruggi G., Chiarot E., Giovani C., Buccato S., Bonacci S., Frigimelica E., Margarit I., Geall A., Bensi G., Maione D. Immunogenicity and protective efficacy induced by self-amplifying mRNA vaccines encoding bacterial antigens. Vaccine. 2017;35:361–368. doi: 10.1016/j.vaccine.2016.11.040. [DOI] [PubMed] [Google Scholar]
- 17.Park J.W., Lagniton P.N., Liu Y., Xu R.-H. mRNA vaccines for COVID-19: What, why and how. Int. J. Biol. Sci. 2021;17:1446–1460. doi: 10.7150/ijbs.59233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zafar S., Arshad M.S., Fatima S., Ali A., Zaman A., Sayed E., Chang M.W., Ahmad Z. COVID-19: Current developments and further opportunities in drug delivery and therapeutics. Pharmaceutics. 2020;12:945. doi: 10.3390/pharmaceutics12100945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim H.J., Seo S.K., Park H.Y. Physical and chemical advances of synthetic delivery vehicles to enhance mRNA vaccine efficacy. J. Control. Release. 2022;345:405–416. doi: 10.1016/j.jconrel.2022.03.029. [DOI] [PubMed] [Google Scholar]
- 20.Li D., Fu D., Kang H., Rong G., Jin Z., Wang X., Zhao K. Advances and potential applications of chitosan nanoparticles as a delivery carrier for the mucosal immunity of vaccine. Curr. Drug Deliv. 2017;14:27–35. doi: 10.2174/1567201813666160804121123. [DOI] [PubMed] [Google Scholar]
- 21.Bento D., Jesus S., Lebre F., Gonçalves T., Borges O. Chitosan plus compound 48/80: Formulation and preliminary evaluation as a hepatitis B vaccine adjuvant. Pharmaceutics. 2019;11:72. doi: 10.3390/pharmaceutics11020072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malik A., Gupta M., Gupta V., Gogoi H., Bhatnagar R. Novel application of trimethyl chitosan as an adjuvant in vaccine delivery. Int. J. Nanomed. 2018;13:7959–7970. doi: 10.2147/IJN.S165876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dmour I., Islam N. Recent advances on chitosan as an adjuvant for vaccine delivery. Int. J. Biol. Macromol. 2022;200:498–519. doi: 10.1016/j.ijbiomac.2021.12.129. [DOI] [PubMed] [Google Scholar]
- 24.Paula H., Silva R., Santos C.M., Dantas F., de Paula R., de Lima L., de Oliveira E., Figueiredo E., Dias F. Eco-friendly synthesis of an alkyl chitosan derivative. Int. J. Biol. Macromol. 2020;163:1591–1598. doi: 10.1016/j.ijbiomac.2020.08.058. [DOI] [PubMed] [Google Scholar]
- 25.Wang W., Meng Q., Li Q., Liu J., Zhou M., Jin Z., Zhao K. Chitosan derivatives and yheir application in biomedicine. Int. J. Mol. Sci. 2020;21:487. doi: 10.3390/ijms21020487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li X., Xing R., Xu C., Liu S., Qin Y., Li K., Yu H., Li P. Immunostimulatory effect of chitosan and quaternary chitosan: A review of potential vaccine adjuvants. Carbohydr. Polym. 2021;264:118050. doi: 10.1016/j.carbpol.2021.118050. [DOI] [PubMed] [Google Scholar]
- 27.Das S.S., Kar S., Singh S.K., Verma P., Hussain A., Beg S. Chitosan in Drug Delivery. Elsevier; India: 2021. Chitosan-based systems for oral drug delivery applications; pp. 23–53. [Google Scholar]
- 28.Song F., Kong Y., Shao C., Cheng Y., Lu J., Tao Y., Du J., Wang H. Chitosan-based multifunctional flexible hemostatic bio-hydrogel. Acta Biomater. 2021;136:170–183. doi: 10.1016/j.actbio.2021.09.056. [DOI] [PubMed] [Google Scholar]
- 29.Liu H., Wang C., Li C., Qin Y., Wang Z., Yang F., Li Z., Wang J. A functional chitosan-based hydrogel as a wound dressing and drug delivery system in the treatment of wound healing. RSC Adv. 2018;8:7533–7549. doi: 10.1039/C7RA13510F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhao J., Li J., Jiang Z., Tong R., Duan X., Bai L., Shi J. Chitosan, N,N,N-trimethyl chitosan (TMC) and 2-hydroxypropyltrimethyl ammonium chloride chitosan (HTCC): The potential immune adjuvants and nano carriers. Int. J. Biol. Macromol. 2020;154:339–348. doi: 10.1016/j.ijbiomac.2020.03.065. [DOI] [PubMed] [Google Scholar]
- 31.Norpi A., Nordin M.L., Ahmad N., Katas H., Fuaad A., Sukri A., Marasini N., Azmi F. New modular platform based on multi-adjuvanted amphiphilic chitosan nanoparticles for efficient lipopeptide vaccine delivery against group A streptococcus. Asian J. Pharm. Sci. 2022;17:435–446. doi: 10.1016/j.ajps.2022.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Şenel S. Current status and future of chitosan in drug and vaccine delivery. React. Funct. Polym. 2020;147:104452. doi: 10.1016/j.reactfunctpolym.2019.104452. [DOI] [Google Scholar]
- 33.Yang Y., Xing R., Liu S., Qin Y., Li K., Yu H., Li P. Chitosan, hydroxypropyltrimethyl ammonium chloride chitosan and sulfated chitosan nanoparticles as adjuvants for inactivated newcastle disease vaccine. Carbohydr. Polym. 2020;229:115423. doi: 10.1016/j.carbpol.2019.115423. [DOI] [PubMed] [Google Scholar]
- 34.Rizeq B.R., Younes N.N., Rasool K., Nasrallah G.K. Synthesis, bioapplications, and toxicity evaluation of chitosan-based nanoparticles. Int. J. Mol. Sci. 2019;20:5776. doi: 10.3390/ijms20225776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mehrabi M., Montazeri H., Mohamadpour Dounighi N., Rashti A., Vakili-Ghartavol R. Chitosan based nanoparticles in mucosal vaccine delivery. Arch. Razi. Inst. 2018;73:165–176. doi: 10.22092/ARI.2017.109235.1101. [DOI] [PubMed] [Google Scholar]
- 36.Quiñones J.P., Peniche H., Peniche C. Chitosan based self-assembled nanoparticles in drug delivery. Polym. Basel. 2018;10:235. doi: 10.3390/polym10030235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Samah H.M., Abdel S.A., Satar A., Wesam H.M., Hanan A.F., Lamiaa M.O., Rania E.M. Preparation and immunological evaluation of inactivated avian influenza virus vaccine encapsulated in chitosan nanoparticles. Biologicals. 2018;51:46–53. doi: 10.1016/j.biologicals.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 38.Jin Z., Li D., Dai C., Cheng G., Wang X., Zhao K. Response of live newcastle disease virus encapsulated in N -2-hydroxypropyl dimethylethyl ammonium chloride chitosan nanoparticles. Carbohydr. Polym. 2017;171:267–280. doi: 10.1016/j.carbpol.2017.05.022. [DOI] [PubMed] [Google Scholar]
- 39.Zhao K., Gao Y., Hu G., Wang L., Cui S., Jin Z. N-2-Hydroxypropyl Trimethyl ammonium chloride chitosan as adjuvant enhances the immunogenicity of a VP2 subunit vaccine against porcine parvovirus infection in sows. Vaccines Basel. 2021;9:1027. doi: 10.3390/vaccines9091027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhao K., Han J., Zhang Y., Wei L., Yu S., Wang X., Jin Z., Wang Y. Enhancing mucosal immune response of newcastle disease virus DNA vaccine using N-2-Hydroxypropyl Trimethylammonium chloride chitosan and N,O-Carboxymethyl chitosan nanoparticles as delivery carrier. Mol. Pharm. 2018;15:226–237. doi: 10.1021/acs.molpharmaceut.7b00826. [DOI] [PubMed] [Google Scholar]
- 41.Zhao K., Li S., Li W., Yu L., Duan X., Han J., Wang X., Jin Z. Quaternized chitosan nanoparticles loaded with the combined attenuated live vaccine against newcastle disease and infectious bronchitis elicit immune response in chicken after intranasal administration. Drug Deliv. 2017;24:1574–1586. doi: 10.1080/10717544.2017.1388450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jesus S., Soares E., Borchard G., Borges O. Poly-ϵ-caprolactone/chitosan nanoparticles provide strong adjuvant effect for hepatitis B antigen. Nanomed. Lond. 2017;12:2335–2348. doi: 10.2217/nnm-2017-0138. [DOI] [PubMed] [Google Scholar]
- 43.Hoseinpur R., Hasani A., Baradaran B., Abdolalizadeh J., Amini Y., Salehi R., Kafil H.S., Azizian K., Memar M.Y., Gholizadeh P., et al. Chitosan nanoparticles containing fusion protein (Hspx–PPE44–EsxV) and resiquimod adjuvant (HPERC) as a novel booster vaccine for Mycobacterium tuberculosis. J. Biomater. Appl. 2022;37:40–47. doi: 10.1177/08853282221079105. [DOI] [PubMed] [Google Scholar]
- 44.Waeckerle-Men Y., Groettrup M. PLGA microspheres for improved antigen delivery to dendritic cells as cellular vaccines. Adv. Drug Deliv. Rev. 2005;57:475–482. doi: 10.1016/j.addr.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 45.He P., Zou Y., Hu Z. Advances in aluminum hydroxide-based adjuvant research and its mechanism. Hum. Vaccines Immunother. 2015;11:477–488. doi: 10.1080/21645515.2014.1004026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Korkmaz E., Balmert S.C., Carey C.D., Erdos G., Falo L.D., Jr. Emerging skin-targeted drug delivery strategies to engineer immunity: A focus on infectious diseases. Expert Opin. Drug Deliv. 2021;18:151–167. doi: 10.1080/17425247.2021.1823964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jin Z., Gao S., Cui X., Sun D., Zhao K. Adjuvants and delivery systems based on polymeric nanoparticles for mucosal vaccines. Int. J. Pharm. 2019;572:118731. doi: 10.1016/j.ijpharm.2019.118731. [DOI] [PubMed] [Google Scholar]
- 48.Li H., Ren H., Zhou Y., Zhang Y., Cao L., Xu W. HRSV prefusion-F protein with Adju-Phos adjuvant induces long-lasting Th2-biased immunity in mice. PLoS ONE. 2022;17:e0262231. doi: 10.1371/journal.pone.0262231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lin Y., Wang X., Huang X., Zhang J., Xia N., Zhao Q. Calcium phosphate nanoparticles as a new generation vaccine adjuvant. Expert Rev. Vaccines. 2017;16:895–906. doi: 10.1080/14760584.2017.1355733. [DOI] [PubMed] [Google Scholar]
- 50.Song T., Liao Y., Zuo Q., Liu N., Liu Z. MnO2 nanoparticles as a minimalist multimode vaccine adjuvant/delivery system to regulate antigen presenting cells for tumor immunotherapy. J. Mater. Chem. B. 2022;10:3474–3490. doi: 10.1039/D1TB02650J. [DOI] [PubMed] [Google Scholar]
- 51.Ko E.-J., Kang S.-M. Immunology and efficacy of MF59-adjuvanted vaccines. Hum. Vaccines Immunother. 2018;14:3041–3045. doi: 10.1080/21645515.2018.1495301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rastakhiz S., Yazdani M., Shariat S., Arab A., Momtazi-Borojeni A.A., Barati N., Mansourian M., Amin M., Abbasi A., Saberi Z., et al. Preparation of nanoliposomes linked to HER2/neu-derived (P5) peptide containing MPL adjuvant as vaccine against breast cancer. J. Cell. Biochem. 2018;120:1294–1303. doi: 10.1002/jcb.27090. [DOI] [PubMed] [Google Scholar]
- 53.Carter D., van Hoeven N., Baldwin S., Levin Y., Kochba E., Magill A., Charland N., Landry N., Nu K., Frevol A., et al. The adjuvant GLA-AF enhances human intradermal vaccine responses. Sci. Adv. 2018;4:eaas9930. doi: 10.1126/sciadv.aas9930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kazzaz J., Singh M., Ugozzoli M., Chesko J., Soenawan E., O’Hagan D.T. Encapsulation of the immune potentiators MPL and RC529 in PLG microparticles enhances their potency. J. Control. Release. 2006;110:566–573. doi: 10.1016/j.jconrel.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 55.Bode C., Zhao G., Steinhagen F., Kinjo T., Klinman D.M. CpG DNA as a vaccine adjuvant. Expert Rev. Vaccines. 2011;10:499–511. doi: 10.1586/erv.10.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Clements J.D., Norton E.B. The mucosal vaccine adjuvant LT(R192G/L211A) or dmLT. mSphere. 2018;3:e00215–e00218. doi: 10.1128/mSphere.00215-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Qu W., Li N., Yu R., Zuo W., Fu T., Fei W., Hou Y., Liu Y., Yang J. Cationic DDA/TDB liposome as a mucosal vaccine adjuvant for uptake by dendritic cells in vitro induces potent humoural immunity. Artif. Cells Nanomed. Biotechnol. 2018;46((Suppl. 1)):852–860. doi: 10.1080/21691401.2018.1438450. [DOI] [PubMed] [Google Scholar]
- 58.Mohanraj M., Sekar P., Liou H.-H., Chang S.-F., Lin W.-W. The mycobacterial adjuvant analogue TDB attenuates neuroinflammation via mincle-independent PLC-γ1/PKC/ERK signaling and microglial polarization. Mol. Neurobiol. 2019;56:1167–1187. doi: 10.1007/s12035-018-1135-4. [DOI] [PubMed] [Google Scholar]
- 59.Cui B., Liu X., Fang Y., Zhou P., Zhang Y., Wang Y. Flagellin as a vaccine adjuvant. Expert Rev. Vaccines. 2018;17:335–349. doi: 10.1080/14760584.2018.1457443. [DOI] [PubMed] [Google Scholar]
- 60.Hafner A.M., Corthésy B., Merkle H.P. Particulate formulations for the delivery of poly(I:C) as vaccine adjuvant. Adv. Drug Deliv. Rev. 2013;65:1386–1399. doi: 10.1016/j.addr.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 61.Didierlaurent A.M., Laupeze B., Di Pasquale A., Hergli N., Collignon C., Garçon N. Adjuvant system AS01: Helping to overcome the challenges of modern vaccines. Expert Rev. Vaccines. 2017;16:55–63. doi: 10.1080/14760584.2016.1213632. [DOI] [PubMed] [Google Scholar]
- 62.Murugappan S., Frijlink H.W., Petrovsky N., Hinrichs W.L. Enhanced pulmonary immunization with aerosolized inactivated influenza vaccine containing delta inulin adjuvant. Eur. J. Pharm. Sci. 2015;66:118–122. doi: 10.1016/j.ejps.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 63.Rizza P., Capone I., Moretti F., Proietti E., Belardelli F. IFN-α as a vaccine adjuvant: Recent insights into the mechanisms and perspectives for its clinical use. Expert Rev. Vaccines. 2011;10:487–498. doi: 10.1586/erv.11.9. [DOI] [PubMed] [Google Scholar]
- 64.Sciullo P.D., Menay F., Cocozza F., Gravisaco M.J., Waldner C.I., Mongini C. Systemic administration of imiquimod as an adjuvant improves immunogenicity of a tumor-lysate vaccine inducing the rejection of a highly aggressive T-cell lymphoma. Clin. Immunol. 2019;203:154–161. doi: 10.1016/j.clim.2019.04.013. [DOI] [PubMed] [Google Scholar]
- 65.Clemens E.A., Holbrook B.C., Kanekiyo M., Yewdell J.W., Graham B.S., Alexander-Miller M.A. An R848-conjugated influenza virus vaccine elicits robust immunoglobulin G to hemagglutinin stem in a newborn nonhuman primate model. J. Infect. Dis. 2021;224:351–359. doi: 10.1093/infdis/jiaa728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Garçon N., Morel S., Didierlaurent A., Descamps D., Wettendorff M., Van Mechelen M. Development of an AS04-adjuvanted HPV vaccine with the adjuvant system approach. BioDrugs. 2011;25:217–226. doi: 10.2165/11591760-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 67.Zheng Y., Bian L., Zhao H., Liu Y., Lu J., Liu D., Zhang K., Song Y., Luo Y., Jiang C., et al. Respiratory syncytial virus F subunit vaccine with AS02 adjuvant elicits balanced, robust humoral and cellular immunity in BALB/c Mice. Front. Immunol. 2020;11:526965. doi: 10.3389/fimmu.2020.526965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Didierlaurent A.M., Collignon C., Bourguignon P., Wouters S., Fierens K., Fochesato M., Dendouga N., Langlet C., Malissen B., Lambrecht B.N., et al. Enhancement of adaptive immunity by the human vaccine adjuvant AS01 depends on activated dendritic cells. J. Immunol. 2014;193:1920–1930. doi: 10.4049/jimmunol.1400948. [DOI] [PubMed] [Google Scholar]
- 69.Carroll E.C., Jin L., Mori A., Muñoz-Wolf N., Oleszycka E., Moran H.B., Mansouri S., McEntee C., Lambe E., Agger E.M., et al. The vaccine adjuvant chitosan promotes cellular immunity via DNA sensor cGAS-STING-dependent induction of Type I interferons. Immunity. 2016;44:597–608. doi: 10.1016/j.immuni.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mallakpour S., Azadi E., Hussain C.M. Chitosan, alginate, hyaluronic acid, gums, and β-glucan as potent adjuvants and vaccine delivery systems for viral threats including SARS-CoV-2: A review. Int. J. Biol. Macromol. 2021;182:1931–1940. doi: 10.1016/j.ijbiomac.2021.05.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.He J., Liu Z., Jiang W., Zhu T., Wusiman A., Gu P., Liu J., Wang D. Immune-adjuvant activity of lentinan-modified calcium carbonate microparticles on a H5N1 vaccine. Int. J. Biol. Macromol. 2020;163:1384–1392. doi: 10.1016/j.ijbiomac.2020.08.005. [DOI] [PubMed] [Google Scholar]
- 72.Ediriweera G.R., Chen L., Yerbury J.J., Thurecht K.J., Vine K.L. Non-viral vector-mediated gene therapy for ALS: Challenges and future perspectives. Mol. Pharm. 2021;18:2142–2160. doi: 10.1021/acs.molpharmaceut.1c00297. [DOI] [PubMed] [Google Scholar]
- 73.Wang T., Zhu X., Yi H., Gu J., Liu S., Izenwasser S., Lemmon V.P., Roy S., Hao S. Viral vector-mediated gene therapy for opioid use disorders. Exp. Neurol. 2021;341:113710. doi: 10.1016/j.expneurol.2021.113710. [DOI] [PubMed] [Google Scholar]
- 74.Abdala A., Alvarez I., Brossel H., Calvinho L., Carignano H., Franco L., Gazon H., Gillissen C., Hamaidia M., Hoyos C., et al. BLV: Lessons on vaccine development. Retrovirology. 2019;16:26. doi: 10.1186/s12977-019-0488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Liu S.A., Stanfield B.A., Chouljenko V.N., Naidu S., Langohr I., Del Piero F., Ferracone J., Roy A.A., Kousoulas K.G. Intramuscular immunization of mice with the live-attenuated herpes simplex virus 1 vaccine strain VC2 expressing equine herpesvirus 1 (EHV-1) glycoprotein D generates anti-EHV-1 immune responses in mice. J. Virol. 2017;91:e02445-16. doi: 10.1128/JVI.02445-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Santana-Armas M.L., de Ilarduya C.T. Strategies for cancer gene-delivery improvement by non-viral vectors. Int. J. Pharm. 2021;596:120291. doi: 10.1016/j.ijpharm.2021.120291. [DOI] [PubMed] [Google Scholar]
- 77.Sharma O., Sultan A.A., Ding H., Triggle C.R. A review of the progress and challenges of developing a vaccine for COVID-19. Front. Immunol. 2020;11:585354. doi: 10.3389/fimmu.2020.585354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ura T., Yamashita A., Mizuki N., Okuda K., Shimada M. New vaccine production platforms used in developing SARS-CoV-2 vaccine candidates. Vaccine. 2021;39:197–201. doi: 10.1016/j.vaccine.2020.11.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Khan W.H., Hashmi Z., Goel A., Ahmad R., Gupta K., Khan N., Alam I., Ahmed F., Ansari M.A. COVID-19 pandemic and vaccines update on challenges and resolutions. Front. Cell. Infect. Microbiol. 2021;11:690621. doi: 10.3389/fcimb.2021.690621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Boroumand H., Badie F., Mazaheri S., Seyedi Z.S., Nahand J.S., Nejati M., Baghi H.B., Abbasi-Kolli M., Badehnoosh B., Ghandali M., et al. Chitosan-based nanoparticles against viral infections. Front. Cell. Infect. Microbiol. 2021;11:643953. doi: 10.3389/fcimb.2021.643953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Segura M.M., Mangion M., Gaillet B., Garnier A. New developments in lentiviral vector design, production and purification. Expert Opin. Biol. Ther. 2013;13:987–1011. doi: 10.1517/14712598.2013.779249. [DOI] [PubMed] [Google Scholar]
- 82.Luis A. The Old and the New: Prospects for non-Integrating lentiviral vector technology. Viruses. 2020;12:1103. doi: 10.3390/v12101103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Humphreys I.R., Sebastian S. Novel viral vectors in infectious diseases. Immunology. 2018;153:1–9. doi: 10.1111/imm.12829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kasala D., Yoon A.-R., Hong J., Kim S.W., Yun C.-O. Evolving lessons on nanomaterial-coated viral vectors for local and systemic gene therapy. Nanomed. Lond. 2016;11:1689–1713. doi: 10.2217/nnm-2016-0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kochhar S., Excler J.-L., Bok K., Gurwith M., McNeil M.M., Seligman S.J., Khuri-Bulos N., Klug B., Laderoute M., Robertson J.S., et al. Defining the interval for monitoring potential adverse events following immunization (AEFIs) after receipt of live viral vectored vaccines. Vaccine. 2019;37:5796–5802. doi: 10.1016/j.vaccine.2018.08.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Miller A.D. Retroviral vectors: From cancer viruses to therapeutic tools. Hum. Gene Ther. 2014;25:989–994. doi: 10.1089/hum.2014.2542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Singh V.K., Kumar S., Dhaked R.K., Ansari A.S., Lohiya N.K., Tapryal S. Generation of oligomers of subunit vaccine candidate glycoprotein D of Herpes Simplex Virus-2 expressed in fusion with IgM Fc domain(s) in Escherichia coli: A strategy to enhance the immunogenicity of the antigen. 3 Biotech. 2020;10:463. doi: 10.1007/s13205-020-02452-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chentoufi A.A., Dhanushkodi N.R., Srivastava R., Prakash S., Coulon P.A., Zayou L., Vahed H., Chentoufi H.A., Hormi-Carver K.K., BenMohamed L. Combinatorial herpes simplex vaccine strategies: From bedside to bench and back. Front Immunol. 2022;13:849515. doi: 10.3389/fimmu.2022.849515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sakurai F., Tachibana M., Mizuguchi H. Adenovirus vector-based vaccine for infectious diseases. Drug Metab. Pharmacokinet. 2022;42:100432. doi: 10.1016/j.dmpk.2021.100432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mitani K., Kubo S. Adenovirus as an integrating vector. Curr. Gene Ther. 2002;2:135–144. doi: 10.2174/1566523024605591. [DOI] [PubMed] [Google Scholar]
- 91.Shimizu K., Sakurai F., Iizuka S., Ono R., Tsukamoto T., Nishimae F., Nakamura S.-I., Nishinaka T., Terada T., Fujio Y., et al. Adenovirus vector–induced IL-6 promotes leaky adenoviral gene expression, leading to acute hepatotoxicity. J. Immunol. 2021;206:410–421. doi: 10.4049/jimmunol.2000830. [DOI] [PubMed] [Google Scholar]
- 92.Milone M.C., O’Doherty U. Clinical use of lentiviral vectors. Leukemia. 2018;32:1529–1541. doi: 10.1038/s41375-018-0106-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Morante V., Borghi M., Farina I., Michelini Z., Grasso F., Gallinaro A., Cecchetti S., Di Virgilio A., Canitano A., Pirillo M., et al. Integrase-defective lentiviral vector is an efficient vaccine platform for cancer immunotherapy. Viruses. 2021;13:355. doi: 10.3390/v13020355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ndwandwe D., Wiysonge C.S. COVID-19 vaccines. Curr. Opin. Immunol. 2021;71:111–116. doi: 10.1016/j.coi.2021.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lee A.Y., Cho M.-H., Kim S. Recent advances in aerosol gene delivery systems using non-viral vectors for lung cancer therapy. Expert Opin. Drug Deliv. 2019;16:757–772. doi: 10.1080/17425247.2019.1641083. [DOI] [PubMed] [Google Scholar]
- 96.Ding B., Li T., Zhang J., Zhao L., Zhai G. Advances in liver-directed gene therapy for hepatocellular carcinoma by non-viral delivery systems. Curr. Gene Ther. 2012;12:92–102. doi: 10.2174/156652312800099625. [DOI] [PubMed] [Google Scholar]
- 97.Zhao H., Wang H., Hu Y., Xu D., Yin C., Han Q., Zhang J. Chitosan nanovaccines as efficient carrier adjuvant system for IL-12 with enhanced protection against HBV. Int. J. Nanomed. 2021;16:4913–4928. doi: 10.2147/IJN.S317113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chuang C.-C., Tsai M.-H., Yen H.-J., Shyu H.-F., Cheng K.-M., Chen X.-A., Chen C.-C., Young J.-J., Kau J.-H. A fucoidan-quaternary chitosan nanoparticle adjuvant for anthrax vaccine as an alternative to CpG oligodeoxynucleotides. Carbohydr. Polym. 2020;229:115403. doi: 10.1016/j.carbpol.2019.115403. [DOI] [PubMed] [Google Scholar]
- 99.Yüksel S., Pekcan M., Puralı N., Esendağlı G., Tavukçuoğlu E., Rivero-Arredondo V., Ontiveros-Padilla L., López-Macías C., Şenel S. Development and in vitro evaluation of a new adjuvant system containing Salmonella Typhi porins and chitosan. Int. J. Pharm. 2020;578:119129. doi: 10.1016/j.ijpharm.2020.119129. [DOI] [PubMed] [Google Scholar]
- 100.Lebre F., de Lima M.P., Lavelle E., Borges O. Mechanistic study of the adjuvant effect of chitosan-aluminum nanoparticles. Int. J. Pharm. 2018;552:7–15. doi: 10.1016/j.ijpharm.2018.09.044. [DOI] [PubMed] [Google Scholar]
- 101.Rabiee N., Bagherzadeh M., Ghadiri A.M., Kiani M., Ahmadi S., Jajarmi V., Fatahi Y., Aldhaher A., Tahriri M., Webster T.J., et al. Calcium-based nanomaterials and their interrelation with chitosan: Optimization for pCRISPR delivery. J. Nanostructure Chem. 2022;12:919–932. doi: 10.1007/s40097-021-00446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Haryono A., Salsabila K., Restu W.K., Harmami S.B., Safari D. Effect of chitosan and liposome nanoparticles as adjuvant codelivery on the immunoglobulin G subclass distribution in a mouse model. J. Immunol. Res. 2017;2017:9125048. doi: 10.1155/2017/9125048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Van der Lubben I.M., Verhoef J., Borchard G., Junginger H.E. Chitosan and its derivatives in mucosal drug and vaccine delivery. Eur. J. Pharm. Sci. 2001;14:201–207. doi: 10.1016/S0928-0987(01)00172-5. [DOI] [PubMed] [Google Scholar]
- 104.Wu X., Farooq M.A., Li T., Geng T., Kutoka P.T., Wang B. Cationic chitosan-modified silica nanoparticles for oral delivery of protein vaccine. J. Biomed. Mater. Res. Part A. 2021;109:2111–2119. doi: 10.1002/jbm.a.37198. [DOI] [PubMed] [Google Scholar]
- 105.Tian J., Yu J., Sun X. Chitosan microspheres as candidate plasmid vaccine carrier for oral immunisation of Japanese flounder (Paralichthys olivaceus) Vet. Immunol. Immunopathol. 2008;126:220–229. doi: 10.1016/j.vetimm.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 106.Pei M., Liang J., Zhang C., Wang X., Zhang C., Ma G., Sun H. Chitosan/calcium phosphates nanosheet as a vaccine carrier for effective cross-presentation of exogenous antigens. Carbohydr. Polym. 2019;224:115172. doi: 10.1016/j.carbpol.2019.115172. [DOI] [PubMed] [Google Scholar]
- 107.Cai J., Zhang W., Xu J., Xue W., Liu Z. Evaluation of N-phosphonium chitosan as a novel vaccine carrier for intramuscular immunization. J. Biomater. Appl. 2017;32:677–685. doi: 10.1177/0885328217735221. [DOI] [PubMed] [Google Scholar]
- 108.Li Y., Wang C., Sun Z., Xiao J., Yan X., Chen Y., Yu J., Wu Y. Simultaneous intramuscular and intranasal administration of chitosan nanoparticles-adjuvanted chlamydia vaccine elicits elevated protective responses in the lung. Int. J. Nanomed. 2019;14:8179–8193. doi: 10.2147/IJN.S218456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Boulbria G., Brilland S., Teixeira-Costa C., Brissonnier M., Charles M., Capdevielle N., Normand V., Bouchet F., Berton P., Krejci R., et al. Effectiveness of two intramuscular combined vaccines for the control of Mycoplasma hyopneu-moniae and porcine circovirus type 2 in growing pigs: A randomized field trial. Porc. Health Manag. 2021;7:41. doi: 10.1186/s40813-021-00220-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Peachman K.K., Rao M., Alving C.R., Burge R., Leppla S.H., Rao V.B., Matyas G.R. Correlation between lethal toxin-neutralizing antibody titers and protection from intranasal challenge with Bacillus Anthracis Ames strain spores in mice after transcutaneous immunization with recombinant anthrax protective antigen. Infect. Immun. 2006;74:794–797. doi: 10.1128/IAI.74.1.794-797.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Thakur A., Pinto F.E., Hansen H.S., Andersen P., Christensen D., Janfelt C., Foged C. Intrapulmonary (i.pulmon.) pull immunization with the tuberculosis subunit vaccine candidate H56/CAF01 after intramuscular (i.m.) priming elicits a distinct innate myeloid response and activation of antigen-presenting cells than i.m. or i.pulmon. prime immunization alone. Front. Immunol. 2020;11:803. doi: 10.3389/fimmu.2020.00803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Viegas E.O., Tembe N., Nilsson C., Meggi B., Maueia C.G., Augusto O., Stout R., Scarlatti G., Ferrari G., Earl P.L., et al. Intradermal HIV-1 DNA immunization using needle-free zetajet injection followed by HIV-modified vaccinia virus ankara vaccination is safe and immunogenic in nozambican young adults: A phase I randomized controlled trial. AIDS Res. Hum. Retrovir. 2018;34:193–205. doi: 10.1089/aid.2017.0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zhang X., Zhao T., Zeng T., Wu N., Xiao Y., Liu S., Yu J., Jiang C., Gan L., Deng M., et al. Intramuscular primary immunization by nucleic acid vaccine pcDNA/Gpd-IL-2 and enhanced immunization with mucosal adjuvant CpG-ODN and Gpd-IL-2 recombinant protein effectively induced strong mucosal immune responses and immune protective effects against Treponema pallidum skin infection. Exp. Ther. Med. 2018;15:2533–2540. doi: 10.3892/etm.2018.5689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhai Y.Z., Li X.M., Zhou Y., Ma L., Feng G.H. Intramuscular immunization with a plasmid DNA vaccine encoding prM-E protein from Japanese encephalitis virus: Enhanced immunogenicity by co-administration of GM-CSF gene and genetic fusions of prM-E protein and GM-CSF. Intervirology. 2009;52:152–163. doi: 10.1159/000224643. [DOI] [PubMed] [Google Scholar]
- 115.Westrop S.J., Moyle G., Jackson A., Nelson M., Mandalia S., Imami N. CCR5 Antagonism impacts vaccination response and immune profile in HIV-1 Infection. Mol. Med. 2012;18:1240–1248. doi: 10.2119/molmed.2012.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Xiao J., Chen T., Wang Q., Liu Q., Wang X., Lv Y., Wu H., Zhang Y. Search for live attenuated vaccine candidate against edwardsiellosis by mutating virulence-related genes of fish pathogen Edwardsiella tarda. Lett. Appl. Microbiol. 2011;53:430–437. doi: 10.1111/j.1472-765X.2011.03126.x. [DOI] [PubMed] [Google Scholar]
- 117.Huang J.-L., Yin Y.-X., Pan Z.-M., Zhang G., Zhu A.-P., Liu X.-F., Jiao X.-A. Intranasal immunization with chitosan/pCAGGS-flaA Nanoparticles inhibits Campylobacter jejuni in a white leghorn model. J. Biomed. Biotechnol. 2010;2010:589476. doi: 10.1155/2010/589476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.De Leeuw P.W., van Bekkum J.G., Tiessink J.W.A. Excretion of foot-and-mouth disease virus in oesophageal-pharyngeal fluid and milk of cattle after intranasal infection. Epidemiol. Infect. 1978;81:415–426. doi: 10.1017/S0022172400025304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Vasilyev K., Shurygina A.-P., Sergeeva M., Stukova M., Egorov A. intranasal immunization with the influenza A virus encoding truncated NS1 protein protects mice from heterologous challenge by restraining the inflammatory response in the lungs. Microorganisms. 2021;9:690. doi: 10.3390/microorganisms9040690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mills K.H.G., Cosgrove C., McNeela E.A., Sexton A., Giemza R., Jabbal-Gill I., Church A., Lin W., Illum L., Podda A., et al. Protective levels of diphtheria-neutralizing antibody induced in healthy volunteers by unilateral priming-boosting in-tranasal immunization associated with restricted ipsilateral mucosal secretory immunoglobulin a. Infect. Immun. 2003;71:726–732. doi: 10.1128/IAI.71.2.726-732.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Van Beek L.F., Langereis J.D., van Saparoea H.V.D.B., Gillard J., Jong W.S.P., van Opzeeland F.J., Mesman R., van Niftrik L.A.M.P., Joosten I., Diavatopoulos D.A., et al. Intranasal vaccination with protein bodies elicit strong protection against Streptococcus pneumoniae colonization. Vaccine. 2021;39:6920–6929. doi: 10.1016/j.vaccine.2021.10.006. [DOI] [PubMed] [Google Scholar]
- 122.Zhao H., Yang J., Qian Q., Wu M., Li M., Xu W. Mesenteric CD103+DCs initiate switched coxsackievirus B3 VP1-Specific IgA response to intranasal chitosan-DNA vaccine through secreting BAFF/IL-6 and promoting Th17/Tfh differentiation. Front Immunol. 2018;9:2986. doi: 10.3389/fimmu.2018.02986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Schild S., Nelson E.J., Camilli A. Immunization with Vibrio cholerae outer membrane vesicles induces protective immunity in mice. Infect Immun. 2008;76:4554–4563. doi: 10.1128/IAI.00532-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Abkar M., Fasihi-Ramandi M., Kooshki H., Sahebghadam Lotfi A. Oral immunization of mice with Omp31-loaded N-trimethyl chitosan nanoparticles induces high protection against Brucella melitensis infection. Int. J. Nanomed. 2017;12:8769–8778. doi: 10.2147/IJN.S149774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhang F., Hao C., Zhang S., Li A., Zhang Q., Wu W., Liu L., Li C., Liang M., Li X., et al. Oral immunization with recombinant enterovirus 71 VP1 formulated with chitosan protects mice against lethal challenge. Virol. J. 2014;11:80. doi: 10.1186/1743-422X-11-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Huang X., Ma Y., Wang Y., Niu C., Liu Z., Yao X., Jiang X., Pan R., Jia S., Li D., et al. Oral probiotic vaccine expressing koi herpesvirus (KHV) ORF81 protein delivered by chitosan-alginate capsules is a promising strategy for mass oral vaccination of carps against KHV infection. J. Virol. 2021;95:e00415-21. doi: 10.1128/JVI.00415-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Oliveira C.R., Rezende C.M.F., Silva M.R., Borges O.M., Pêgo A.P., Goes A.M. Oral vaccination based on DNA-chitosan nanoparticles against Schistosoma mansoni infection. Sci. World J. 2012;2012:938457. doi: 10.1100/2012/938457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Milligan R., Paul M., Richardson M., Neuberger A. Vaccines for preventing typhoid fever. Cochrane Database Syst. Rev. 2018;5:CD001261. doi: 10.1002/14651858.CD001261.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chudina T., Labyntsev A., Manoilov K., Kolybo D., Komisarenko S. Cellobiose-coated poly (lactide-co-glycolide) particles loaded with diphtheria toxoid for per os immunization. Croat. Med. J. 2015;56:85–93. doi: 10.3325/cmj.2015.56.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Oliveira C.R., Rezende C.M.F., Silva M.R., Pêgo A.P., Borges O., Goes A.M. A new strategy based on Smrho Protein loaded chitosan nanoparticles as a candidate oral vaccine against Schistosomiasis. PLOS Negl. Trop. Dis. 2012;6:e1894. doi: 10.1371/journal.pntd.0001894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Periman L.M., Mah F.S., Karpecki P.M. A review of the mechanism of action of cyclosporine A: The role of cyclosporine A in dry eye disease and recent formulation developments. Clin. Ophthalmol. 2020;14:4187–4200. doi: 10.2147/OPTH.S279051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Irie H., Shimeld C., Williams N., Hill T. Protection against ocular and cutaneous infection with herpes simplex virus type 1 by intragastric immunization with live virus. J. Gen. Virol. 1993;74:1357–1362. doi: 10.1099/0022-1317-74-7-1357. [DOI] [PubMed] [Google Scholar]
- 133.Peng J., Yao X., Yuan C., Liu X., Xia R., He J., Li R., Yao Y. The investigation of hepatitis B vaccine immune responses in occult hepatitis B virus-infected patients. Front. Immunol. 2022;13:903685. doi: 10.3389/fimmu.2022.903685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mishra H., Mishra D., Mishra P.K., Nahar M., Dubey V., Jain N.K. Evaluation of solid lipid nanoparticles as carriers for delivery of hepatitis B surface antigen for vaccination using subcutaneous route. J. Pharm. Pharm. Sci. 2010;13:495–509. doi: 10.18433/J3XK53. [DOI] [PubMed] [Google Scholar]
- 135.Greenberg H., Helms C.M., Grizzard M.B., James W.D., Horswood R.L., Chanock R.M. Immunoprophylaxis of experimental Mycoplasma pneumoniae disease: Effect of route of administration on the immunogenicity and protective effect of inactivated M. pneumoniae vaccine. Infect. Immun. 1977;16:88–92. doi: 10.1128/iai.16.1.88-92.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Boland K.G., Hayles A.N., Miller C.B., Kerr T., Brown W.C., Lahmers K.K. Regional immune response to immunization with Escherichia coli O157:H7-Derived intimin in cattle. Clin. Vaccine Immunol. 2013;20:562–571. doi: 10.1128/CVI.00743-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Barisani-Asenbauer T., Inić-Kanada A., Belij S., Marinković E., Stojićević I., Montanaro J., Stein E., Bintner N., Stojanović M. The ocular conjunctiva as a mucosal immunization route: A profile of the immune response to the model antigen tetanus toxoid. PLoS ONE. 2013;8:e60682. doi: 10.1371/journal.pone.0060682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yu Z., Zhou T., Luo Y., Dong L., Li C., Liu J., Luo J., Yan R., Xu L., Song X., et al. Modulation effects of Toxoplasma gondii histone H2A1 on murine macrophages and encapsulation with polymer as a vaccine candidate. Vaccines. 2020;8:731. doi: 10.3390/vaccines8040731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Zhu M., Gao F., Li Z., Wang X., Wang H., Wang Z., Zhao J., Zhao W. Immunoprotection of recombinant Eg.myophilin against Echinococcus granulosus infection in sheep. Exp. Ther. Med. 2016;12:1585–1590. doi: 10.3892/etm.2016.3501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Beyrodt C.G., Pinto A.R., Freymüller E., Barbiéri C.L. Characterization of an antigen from Leishmania amazonensis amastigotes able to elicit protective responses in a murine model. Infect. Immun. 1997;65:2052–2059. doi: 10.1128/iai.65.6.2052-2059.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Muflihah H., Flórido M., Lin L.C.W., Xia Y., Triccas J.A., Stambas J., Britton W.J. Boosting BCG with recombinant influenza A virus tuberculosis vaccines increases pulmonary T cell responses but not protection against Mycobacterium tuberculosis infection. PLoS ONE. 2021;16:e0259829. doi: 10.1371/journal.pone.0259829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Yang J., Liang G., Xiang T., Situ W. Effect of crosslinking processing on the chemical structure and biocompatibility of a chitosan-based hydrogel. Food Chem. 2021;354:129476. doi: 10.1016/j.foodchem.2021.129476. [DOI] [PubMed] [Google Scholar]
- 143.Deng X., Zhao J., Liu K., Wu C., Liang F. Stealth PEGylated chitosan polyelectrolyte complex nanoparticles as drug delivery carrier. J. Biomater. Sci. Polym. Ed. 2021;32:1387–1405. doi: 10.1080/09205063.2021.1918043. [DOI] [PubMed] [Google Scholar]
- 144.Bravo-Anaya L.M., Fernández-Solís K.G., Rosselgong J., Nano-Rodríguez J., Carvajal F., Rinaudo M. Chitosan-DNA polyelectrolyte complex: Influence of chitosan characteristics and mechanism of complex formation. Int. J. Biol. Macromol. 2019;126:1037–1049. doi: 10.1016/j.ijbiomac.2019.01.008. [DOI] [PubMed] [Google Scholar]
- 145.Chandra Hembram K., Prabha S., Chandra R., Ahmed B., Nimesh S. Advances in preparation and characterization of chitosan nanoparticles for therapeutics. Artif. Cells Nanomed. Biotechnol. 2016;44:305–314. doi: 10.3109/21691401.2014.948548. [DOI] [PubMed] [Google Scholar]
- 146.Tahara K., Yamamoto H., Hirashima N., Kawashima Y. Chitosan-modified poly(D,L-lactide-co-glycolide) nanospheres for improving siRNA delivery and gene-silencing effects. Eur. J. Pharm. Biopharm. 2010;74:421–426. doi: 10.1016/j.ejpb.2009.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Tahara K., Sakai T., Yamamoto H., Takeuchi H., Hirashima N., Kawashima Y. Improvements in transfection efficiency with chitosan modified poly(DL-lactide-co-glycolide) nanospheres prepared by the emulsion solvent diffusion method, for gene delivery. Chem. Pharm. Bull Tokyo. 2011;59:298–301. doi: 10.1248/cpb.59.298. [DOI] [PubMed] [Google Scholar]
- 148.Gentile P., Nandagiri V.K., Pabari R., Daly J., Tonda-Turo C., Ciardelli G., Ramtoola Z. Influence of parathyroid hormone-loaded PLGA nanoparticles in porous scaffolds for bone regeneration. Int. J. Mol. Sci. 2015;16:20492–20510. doi: 10.3390/ijms160920492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wang C., Ye W., Zheng Y., Liu X., Tong Z. Fabrication of drug-loaded biodegradable microcapsules for controlled release by combination of solvent evaporation and layer-by-layer self-assembly. Int. J. Pharm. 2007;338:165–173. doi: 10.1016/j.ijpharm.2007.01.049. [DOI] [PubMed] [Google Scholar]
- 150.Zheng K., Xiao S., Li W., Wang W., Chen H., Yang F., Qin C. Chitosan-acorn starch-eugenol edible film: Physico-chemical, barrier, antimicrobial, antioxidant and structural properties. Int. J. Biol. Macromol. 2019;135:344–352. doi: 10.1016/j.ijbiomac.2019.05.151. [DOI] [PubMed] [Google Scholar]
- 151.Zhang Z.-L., Li L.-J., Sun D., Wang M., Shi J.-R., Yang D., Wang L.-H., Zou S.-C. Preparation and properties of chitosan-based microspheres by spray drying. Food Sci. Nutr. 2020;8:1933–1941. doi: 10.1002/fsn3.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Wei Y., Huang Y.-H., Cheng K.-C., Song Y.-L. Investigations of the influences of processing conditions on the properties of spray dried chitosan-tripolyphosphate particles loaded with theophylline. Sci. Rep. 2020;10:1155. doi: 10.1038/s41598-020-58184-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Garg U., Chauhan S., Nagaich U., Jain N. Current advances in chitosan nanoparticles based drug delivery and targeting. Adv. Pharm. Bull. 2019;9:195–204. doi: 10.15171/apb.2019.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Saeed R.M., Dmour I., Taha M.O. Stable Chitosan-based nanoparticles using polyphosphoric acid or hexametaphosphate for tandem ionotropic/covalent crosslinking and subsequent investigation as novel vehicles for drug delivery. Front. Bioeng. Biotechnol. 2020;8:4. doi: 10.3389/fbioe.2020.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Orellano M.S., Porporatto C., Silber J.J., Falcone R.D., Correa N.M. AOT reverse micelles as versatile reaction media for chitosan nanoparticles synthesis. Carbohydr. Polym. 2017;171:85–93. doi: 10.1016/j.carbpol.2017.04.074. [DOI] [PubMed] [Google Scholar]
- 156.Mikušová V., Mikuš P. Advances in chitosan-based nanoparticles for drug delivery. Int. J. Mol. Sci. 2021;22:9652. doi: 10.3390/ijms22179652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Koppolu B., Zaharoff D.A. The effect of antigen encapsulation in chitosan particles on uptake, activation and presentation by antigen presenting cells. Biomaterials. 2013;34:2359–2369. doi: 10.1016/j.biomaterials.2012.11.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Imam S.S., Alshehri S., Ghoneim M.M., Zafar A., Alsaidan O.A., Alruwaili N.K., Gilani S.J., Rizwanullah M. Recent advancement in chitosan-based nanoparticles for improved oral bioavailability and bioactivity of phytochemicals: Challenges and perspectives. Polym. Basel. 2021;13:4036. doi: 10.3390/polym13224036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kim T.H., Nah J.W., Cho M.-H., Park T.G., Cho C.S. Receptor-mediated gene delivery into antigen presenting cells using mannosylated chitosan/DNA nanoparticles. J. Nanosci. Nanotechnol. 2006;6:2796–2803. doi: 10.1166/jnn.2006.434. [DOI] [PubMed] [Google Scholar]
- 160.Kojarunchitt T., Baldursdottir S., Dong Y.-D., Boyd B.J., Rades T., Hook S. Modified thermoresponsive Poloxamer 407 and chitosan sol–gels as potential sustained-release vaccine delivery systems. Eur. J. Pharm. Biopharm. 2015;89:74–81. doi: 10.1016/j.ejpb.2014.11.026. [DOI] [PubMed] [Google Scholar]
- 161.Karthick Raja Namasivayam S., Nishanth A.N., Arvind Bharani R.S., Nivedh K., Syed N.H., Samuel R.R. Hepatitis B-surface antigen (HBsAg) vaccine fabricated chitosan-polyethylene glycol nanocomposite (HBsAg-CS-PEG- NC) preparation, immunogenicity, controlled release pattern, biocompatibility or non-target toxicity. Int. J. Biol. Macromol. 2020;144:978–994. doi: 10.1016/j.ijbiomac.2019.09.175. [DOI] [PubMed] [Google Scholar]
- 162.Ishii-Mizuno Y., Umeki Y., Onuki Y., Watanabe H., Takahashi Y., Takakura Y., Nishikawa M. Improved sustained release of antigen from immunostimulatory DNA hydrogel by electrostatic interaction with chitosan. Int. Pharm. 2017;516:392–400. doi: 10.1016/j.ijpharm.2016.11.048. [DOI] [PubMed] [Google Scholar]
- 163.Fan Q., Miao C., Huang Y., Yue H., Wu A., Wu J., Wu J., Ma G. Hydroxypropyltrimethyl ammonium chloride chitosan-based hydrogel as the split H5N1 mucosal adjuvant: Structure-activity relationship. Carbohydr. Polym. 2021;266:118139. doi: 10.1016/j.carbpol.2021.118139. [DOI] [PubMed] [Google Scholar]
- 164.Zhang S., Huang S., Lu L., Song X., Li P., Wang F. Curdlan sulfate-O-linked quaternized chitosan nanoparticles: Potential adjuvants to improve the immunogenicity of exogenous antigens via intranasal vaccination. Int. J. Nanomed. 2018;13:2377–2394. doi: 10.2147/IJN.S158536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zhang G., Jia P., Liu H., Hu T., Du Y. Conjugation of chitosan oligosaccharides enhances immune response to porcine circovirus vaccine by activating macrophages. Immunobiology. 2018;223:663–670. doi: 10.1016/j.imbio.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 166.Shim S., Soh S.H., Im Y.B., Park H.-E., Cho C.-S., Kim S., Yoo H.S. Elicitation of Th1/Th2 related responses in mice by chitosan nanoparticles loaded with Brucella abortus malate dehydrogenase, outer membrane proteins 10 and 19. Int. J. Med. Microbiol. 2020;310:151362. doi: 10.1016/j.ijmm.2019.151362. [DOI] [PubMed] [Google Scholar]
- 167.Wen Z.-S., Xu Y.-L., Zou X.-T., Xu Z.-R. Chitosan nanoparticles act as an adjuvant to promote both Th1 and Th2 immune responses induced by ovalbumin in mice. Mar. Drugs. 2011;9:1038–1055. doi: 10.3390/md9061038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Svindland S.C., Pedersen G.K., Pathirana R.D., Bredholt G., Nøstbakken J.K., Jul-Larsen Å., Guzmán C.A., Montomoli E., Lapini G., Piccirella S., et al. A study of chitosan and c-di-GMP as mucosal adjuvants for intranasal influenza H5N1 vaccine. Influ. Other Respir. Viruses. 2013;7:1181–1193. doi: 10.1111/irv.12056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Ghendon Y., Markushin S., Vasiliev Y., Akopova I., Koptiaeva I., Krivtsov G., Borisova O., Ahmatova N., Kurbatova E., Mazurina S., et al. Evaluation of properties of chitosan as an adjuvant for inactivated influenza vaccines administered parenterally. J. Med. Virol. 2009;81:494–506. doi: 10.1002/jmv.21415. [DOI] [PubMed] [Google Scholar]
- 170.Chua B.Y., Al Kobaisi M., Zeng W., Mainwaring D., Jackson D.C. Chitosan microparticles and nanoparticles as biocompatible delivery vehicles for peptide and protein-based immunocontraceptive vaccines. Mol. Pharm. 2012;9:81–90. doi: 10.1021/mp200264m. [DOI] [PubMed] [Google Scholar]
- 171.Boraschi D., Italiani P., Palomba R., Decuzzi P., Duschl A., Fadeel B., Moghimi S.M. Nanoparticles and innate immunity: New perspectives on host defence. Semin. Immunol. 2017;34:33–51. doi: 10.1016/j.smim.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 172.Yu X., Wen T., Cao P., Shan L., Li L. Alginate-chitosan coated layered double hydroxide nanocomposites for enhanced oral vaccine delivery. J. Colloid Interface Sci. 2019;556:258–265. doi: 10.1016/j.jcis.2019.08.027. [DOI] [PubMed] [Google Scholar]
- 173.Xu B., Zhang W., Chen Y., Xu Y., Wang B., Zong L. Eudragit® L100-coated mannosylated chitosan nanoparticles for oral protein vaccine delivery. Int. J. Biol. Macromol. 2018;113:534–542. doi: 10.1016/j.ijbiomac.2018.02.016. [DOI] [PubMed] [Google Scholar]
- 174.Kaneko K., Miyaji E.N., Gonçalves V.M., Ferreira D.M., Solórzano C., MacLoughlin R., Saleem I. Evaluation of polymer choice on immunogenicity of chitosan coated PLGA NPs with surface-adsorbed pneumococcal protein antigen PspA4Pro. Int. J. Pharm. 2021;599:120407. doi: 10.1016/j.ijpharm.2021.120407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Renu S., Han Y., Dhakal S., Lakshmanappa Y.S., Ghimire S., Feliciano-Ruiz N., Senapati S., Narasimhan B., Selvaraj R., Renukaradhya G.J. Chitosan-adjuvanted Salmonella subunit nanoparticle vaccine for poultry delivered through drinking water and feed. Carbohydr. Polym. 2020;243:116434. doi: 10.1016/j.carbpol.2020.116434. [DOI] [PubMed] [Google Scholar]
- 176.Sadeghi Z., Fasihi-Ramandi M., Azizi M., Bouzari S. Mannosylated chitosan nanoparticles loaded with FliC antigen as a novel vaccine candidate against Brucella melitensis and Brucella abortus infection. J. Biotechnol. 2020;310:89–96. doi: 10.1016/j.jbiotec.2020.01.016. [DOI] [PubMed] [Google Scholar]
- 177.Koppolu B.P., Smith S.G., Ravindranathan S., Jayanthi S., Suresh-Kumar T.K., Zaharoff D.A. Controlling chitosan-based encapsulation for protein and vaccine delivery. Biomaterials. 2014;35:4382–4389. doi: 10.1016/j.biomaterials.2014.01.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Nevagi R.J., Khalil Z.G., Hussein W.M., Powell J., Batzloff M.R., Capon R.J., Good M.F., Skwarczynski M., Toth I. Polyglutamic acid-trimethyl chitosan-based intranasal peptide nano-vaccine induces potent immune responses against group A streptococcus. Acta Biomater. 2018;80:278–287. doi: 10.1016/j.actbio.2018.09.037. [DOI] [PubMed] [Google Scholar]
- 179.Junior S.R.D.S., Da Silva F.K.L., Dias L.S., Souza A.C.O., De Araujo M.V., Da Silva L.B.R., Travassos L.R., Amaral A.C., Taborda C.P. Intranasal vaccine using P10 peptide complexed within chitosan polymeric nanoparticles as experimental therapy for paracoccidioidomycosis in murine model. J. Fungi Basel. 2020;6:160. doi: 10.3390/jof6030160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Jung S.-N., Kang S.-K., Yeo G.-H., Li H.-Y., Jiang T., Nah J.-W., Bok J.-D., Cho C.-S., Choi Y.-J. Targeted delivery of vaccine to dendritic cells by chitosan nanoparticles conjugated with a targeting peptide ligand selected by phage display technique. Macromol. Biosci. 2015;15:395–404. doi: 10.1002/mabi.201400352. [DOI] [PubMed] [Google Scholar]
- 181.Robles-Planells C., Barrera-Avalos C., Rojo L.E., Spencer E., Martin M.C.-S., Matiacevich S., Pavez J., Milla L.A., Navarro F.D., Martínez B.A., et al. Chitosan-based delivery of avian reovirus fusogenic protein p10 gene: In vitro and in vivo studies towards a new vaccine against melanoma. Biomed. Res. Int. 2020;2020:4045760. doi: 10.1155/2020/4045760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Renu S., Feliciano-Ruiz N., Patil V., Schrock J., Han Y., Ramesh A., Dhakal S., Hanson J., Krakowka S., Renukaradhya G.J. Immunity and protective efficacy of mannose conjugated chitosan-based influenza nanovaccine in maternal antibody positive pigs. Front. Immunol. 2021;12:584299. doi: 10.3389/fimmu.2021.584299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Bi Y., Xu Q., Su L., Xu J., Liu Z., Yang Y., Tang H., Li Y., Fan M. The combinations chitosan-Pam3CSK4 and chitosan-monophosphoryl lipid A: Promising immune-enhancing adjuvants for anticaries vaccine PAc. Infect. Immun. 2019;87:e00651-19. doi: 10.1128/IAI.00651-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Du X., Xue J., Jiang M., Lin S., Huang Y., Deng K., Shu L., Xu H., Li Z., Yao J., et al. A multiepitope peptide, rOmp22, encapsulated in chitosan-PLGA nanoparticles as a candidate vaccine against Acinetobacter baumannii infection. Int. J. Nanomed. 2021;16:1819–1836. doi: 10.2147/IJN.S296527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Jiang T., Singh B., Maharjan S., Li H.S., Kang S.K., Bok J.D., Cho C.S., Choi Y.J. Oral delivery of probiotic expressing M cell homing peptide conjugated BmpB vaccine encapsulated into alginate/chitosan/alginate microcapsules. Eur. J. Pharm. Biopharm. 2014;88:768–777. doi: 10.1016/j.ejpb.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 186.Büyüktimkin B., Wang Q., Kiptoo P., Stewart J.M., Berkland C., Siahaan T.J. Vaccine-like controlled-release delivery of an immunomodulating peptide to treat experimental autoimmune encephalomyelitis. Mol. Pharm. 2012;9:979–985. doi: 10.1021/mp200614q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Zhao L., Jin W., Cruz J.G., Marasini N., Khalil Z.G., Capon R.J., Hussein W.M., Skwarczynski M., Toth I. Development of polyelectrolyte complexes for the delivery of peptide-based subunit vaccines against group A Streptococcus. Nanomater. Basel. 2020;10:823. doi: 10.3390/nano10050823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Xu Y., Zhou Z., Brooks B., Ferguson T., Obliosca J., Huang J., Kaneko I., Iwanaga S., Yuda M., Tsuji Y., et al. Layer-by-layer delivery of multiple antigens using trimethyl chitosan nanoparticles as a malaria vaccine candidate. Front. Immunol. 2022;13:900080. doi: 10.3389/fimmu.2022.900080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Nguyen K.G., Mantooth S.M., Vrabel M.R., Zaharoff D.A. Intranasal delivery of thermostable subunit vaccine for cross-reactive mucosal and systemic antibody responses against SARS-CoV-2. Front. Immunol. 2022;13:858904. doi: 10.3389/fimmu.2022.858904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Tabynov K., Babayeva M., Nurpeisov T., Fomin G., Nurpeisov T., Saltabayeva U., Renu S., Renukaradhya G.J., Petrovsky N., Tabynov K. Evaluation of a novel adjuvanted vaccine for ultrashort regimen therapy of artemisia pollen-induced allergic bronchial asthma in a mouse model. Front. Immunol. 2022;13:828690. doi: 10.3389/fimmu.2022.828690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Silva-Marrero J.I., Villasante J., Rashidpour A., Palma M., Fàbregas A., Almajano M.P., Viegas I., Jones J.G., Miñarro M., Ticó J.R., et al. The administration of chitosan-tripolyphosphate-DNA nanoparticles to express exogenous SREBP1a enhances conversion of dietary carbohydrates into lipids in the liver of sparus aurata. Biomolecules. 2019;9:297. doi: 10.3390/biom9080297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Tahamtan A., Barati M., Tabarraei A., Mohebbi S.R., Shirian S., Gorji A., Ghaemi A. Antitumor immunity induced by genetic immunization with chitosan nanoparticle formulated adjuvanted for HPV-16 E7 DNA vaccine. Iran. J. Immunol. 2018;15:269–280. doi: 10.22034/IJI.2018.39396. [DOI] [PubMed] [Google Scholar]
- 193.Kumar U.S., Afjei R., Ferrara K., Massoud T.F., Paulmurugan R. Gold-nanostar-chitosan-mediated delivery of SARS-CoV-2 DNA vaccine for respiratory mucosal immunization: Development and proof-of-principle. ACS Nano. 2021;15:17582–17601. doi: 10.1021/acsnano.1c05002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Thirumalaikumar E., Lelin C., Sathishkumar R., Vimal S., Anand S.B., Babu M.M., Citarasu T. Oral delivery of pVAX-OMP and pVAX-hly DNA vaccine using Chitosan-Tripolyphosphate (Cs-TPP) nanoparticles in Rohu, (Labeo rohita) for protection against Aeromonas hydrophila infection. Fish Shellfish Immunol. 2021;115:189–197. doi: 10.1016/j.fsi.2021.06.004. [DOI] [PubMed] [Google Scholar]
- 195.Leya T., Ahmad I., Sharma R., Tripathi G., Kurcheti P.P., Rajendran K.V., Bedekar M.K. Bicistronic DNA vaccine macromolecule complexed with poly lactic-co-glycolic acid-chitosan nanoparticles enhanced the mucosal immunity of Labeo rohita against Edwardsiella tarda infection. Int. J. Biol. Macromol. 2020;156:928–937. doi: 10.1016/j.ijbiomac.2020.04.048. [DOI] [PubMed] [Google Scholar]
- 196.Bande F., Arshad S.S., Bejo M.H., Omar A.R., Moeini H., Khadkodaei S., Wei T.S., Keong Y.S., Abba Y., Anka I.A. Development and immunogenic potentials of chitosan-saponin encapsulated DNA vaccine against avian infectious bronchitis coronavirus. Microb. Pathog. 2020;149:104560. doi: 10.1016/j.micpath.2020.104560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Dubey S., Avadhani K., Mutalik S., Sivadasan S.M., Maiti B., Girisha S.K., Venugopal M.N., Mutoloki S., Evensen Ø., Karunasagar I., et al. Edwardsiella tarda OmpA encapsulated in chitosan nanoparticles shows superior protection over inactivated whole cell vaccine in orally vaccinated fringed-lipped peninsula carp (Labeo fimbriatus) Vaccines Basel. 2016;4:40. doi: 10.3390/vaccines4040040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Wu M., Zhao H., Li M., Yue Y., Xiong S., Xu W. Intranasal vaccination with mannosylated chitosan formulated DNA vaccine enables robust IgA and cellular response induction in the lungs of mice and improves protection against pulmonary mycobacterial challenge. Front. Cell. Infect. Microbiol. 2017;7:445. doi: 10.3389/fcimb.2017.00445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Sun K., Li X., Jiang J., Cheng A., Wang M., Zhu D., Jia R., Chen S., Zhou Y., Chen X., et al. Distribution characteristics of DNA vaccine encoded with glycoprotein C from anatid herpesvirus 1 with chitosan and liposome as deliver carrier in ducks. Virol. J. 2013;10:89. doi: 10.1186/1743-422X-10-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Lebre F., Borchard G., Faneca H., Pedroso de Lima M.C., Borges O. Intranasal administration of novel chitosan nanoparticle/DNA complexes induces antibody response to Hepatitis B surface antigen in mice. Mol. Pharm. 2016;13:472–482. doi: 10.1021/acs.molpharmaceut.5b00707. [DOI] [PubMed] [Google Scholar]
- 201.Chehelgerdi M., Doosti A. Effect of the cagW-based gene vaccine on the immunologic properties of BALB/c mouse: An efficient candidate for Helicobacter pylori DNA vaccine. J. Nanobiotechnol. 2020;18:63. doi: 10.1186/s12951-020-00618-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Nanda R.K., Hajam I.A., Edao B.M., Ramya K., Rajanga M., Sekar S.C., Ganesh K., Bhanuprakash V., Kishore S. Immunological evaluation of mannosylated chitosan nanoparticles based foot and mouth disease virus DNA vaccine, pVAC FMDV VP1-OmpA in guinea pigs. Biologicals. 2014;42:153–159. doi: 10.1016/j.biologicals.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 203.Yan J., Chen R., Zhang H., Bryers J.D. Injectable biodegradable chitosan-alginate 3D porous gel scaffold for mRNA vaccine delivery. Macromol. Biosci. 2019;19:e1800242. doi: 10.1002/mabi.201800242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Crommelin D.J., Anchordoquy T.J., Volkin D.B., Jiskoot W., Mastrobattista E. Addressing the cold reality of mRNA vaccine stability. J. Pharm. Sci. 2021;110:997–1001. doi: 10.1016/j.xphs.2020.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Hajam I.A., Senevirathne A., Hewawaduge C., Kim J., Lee J.H. Intranasally administered protein coated chitosan nanoparticles encapsulating influenza H9N2 HA2 and M2e mRNA molecules elicit protective immunity against avian influenza viruses in chickens. Veter-Res. 2020;51:37. doi: 10.1186/s13567-020-00762-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Démoulins T., Englezou P.C., Milona P., Ruggli N., Tirelli N., Pichon C., Sapet C., Ebensen T., Guzmán C.A., McCullough K.C. Self-Replicating RNA vaccine delivery to dendritic cells. Methods Mol. Biol. 2017;1499:37–75. doi: 10.1007/978-1-4939-6481-9_3. [DOI] [PubMed] [Google Scholar]
- 207.Steinle H., Ionescu T.-M., Schenk S., Golombek S., Kunnakattu S.-J., Özbek M.T., Schlensak C., Wendel H.P., Avci-Adali M. Incorporation of synthetic mRNA in injectable chitosan-alginate hybrid hydrogels for local and sustained expression of exogenous proteins in cells. Int. J. Mol. Sci. 2018;19:1313. doi: 10.3390/ijms19051313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Wang K., Wang X., Jiang D., Pei Y., Wang Z., Zhou X.G., Wu G.L., Mo X.M., Wang H.S. Delivery of mRNA vaccines and anti-PDL1 siRNA through non-invasive transcutaneous route effectively inhibits tumor growth. Compos. B Eng. 2022;233:109648. doi: 10.1016/j.compositesb.2022.109648. [DOI] [Google Scholar]
- 209.Zhang N.N., Li X.F., Deng Y.Q., Zhao H., Huang Y.J., Yang G., Huang W.J., Gao P., Zhou C., Zhang R.R., et al. A thermostable mRNA vaccine against COVID-19. Cell. 2020;182:1271–1283. doi: 10.1016/j.cell.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Kremsner P.G., Mann P., Kroidl A., Leroux-Roels I., Schindler C., Gabor J.J., Schunk M., Leroux-Roels G., Bosch J.J., Fendel R., et al. Safety and immunogenicity of an mRNA-lipid nanoparticle vaccine candidate against SARS-CoV-2: A phase 1 randomized clinical trial. Wien. Klin. Wochenschr. 2021;133:931–941. doi: 10.1007/s00508-021-01922-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Linares-Fernández S., Lacroix C., Exposito J.-Y., Verrier B. Tailoring mRNA vaccine to balance innate/adaptive immune response. Trends Mol. Med. 2020;26:311–323. doi: 10.1016/j.molmed.2019.10.002. [DOI] [PubMed] [Google Scholar]
- 212.Han Y., Renu S., Patil V., Schrock J., Feliciano-Ruiz N., Selvaraj R., Renukaradhya G.J. Immune response to Salmonella enteritidis infection in broilers immunized orally with chitosan-based salmonella subunit nanoparticle vaccine. Front. Immunol. 2020;11:935. doi: 10.3389/fimmu.2020.00935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Safarzadeh M., Sadeghi S., Azizi M., Rastegari-Pouyani M., Pouriran R., Haji Molla Hoseini M. Chitin and chitosan as tools to combat COVID-19: A triple approach. Int. J. Biol. Macromol. 2021;183:235–244. doi: 10.1016/j.ijbiomac.2021.04.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Huang S.S., Sung S.H., Chiang C.E. Chitosan potentiation of warfarin effect. Ann. Pharmacother. 2007;41:1912–1914. doi: 10.1345/aph.1K173. [DOI] [PubMed] [Google Scholar]
- 215.Srinivas N.R. The interesting case of acyclovir delivered using chitosan in humans: Is it a drug issue or formulation Issue? Pharm. Res. 2016;33:543–547. doi: 10.1007/s11095-015-1811-2. [DOI] [PubMed] [Google Scholar]
- 216.Huang Y.C., Vieira A., Huang K.L., Yeh M.K., Chiang C.H. Pulmonary inflammation caused by chitosan microparticles. J. Biomed. Mater. Res. A. 2005;75:283–287. doi: 10.1002/jbm.a.30421. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.