Abstract
Background
Despite the significant benefits of digital health technologies (ITs), developing countries are lagging behind their developed counterparts in the adoption of electronic medical records (EMRs) in a healthcare setting. EMRs have long been considered essential elements in improving the quality of healthcare. However, the rate of utilization of EMRs among healthcare providers still remains low, particularly in developing countries.
Objective
This study aimed at exploring EMR use and its determinants among healthcare providers at public health facilities in Dire Dawa, eastern Ethiopia.
Methods
A quantitative cross-sectional study was conducted among 402 health professionals working at public health facilities supplemented with an exploratory qualitative study in Dire Dawa, Ethiopia. Descriptive summary statistics and binary and multivariable logistic regression analysis were used to explore the determinant factors of EMR use, while qualitative data were thematically analyzed.
Results
Overall, about a quarter (26.6%) of health professionals were using electronic medical records. A work experience of 6 years or less [adjusted odds ratio (AOR) = 2.23; 95% confidence interval (CI): [1.15–4.31]], a discussion on EMR (AOR = 14.47; 95% CI: [5.58–7.57]), the presence of an EMR manual (AOR = 3.10; 95% CI: [1.28–7.38]), and a positive attitude toward the EMR system (AOR = 11.15; 95% CI: [4.90–25.36]) and service quality (AOR = 8.02; 95% CI: [4.09–15.72]) were independent determinants of EMR use. Poor collaboration among stakeholders and dependence on the software programs of NGOs were the main challenges cited by key informants.
Conclusion
The findings of this study indicate that EMR use by health professionals in the study area is very low. Several organizational, technical, and behavioral factors were identified for this low utilization. Therefore, there is a need to leverage EMRs through continuous technical support and commitment to enhance its use, which has the potential to improve health service performance. Developing locally applicable EMR software should be considered.
Keywords: electronic medical record use, perceived EMR system quality, public health facilities, eastern Ethiopia, perceived service quality
Introduction
The ever-increasing integration of highly diversified technologies in the healthcare field has resulted in the need for gathering organized and accurate data for informed decision-making in the health sector (1–4). Evidence shows that health facilities with electronic notes, records, test results, and clinical decision support lead to an effective overall healthcare delivery system (5–9). One of the record number of automations being implemented in a healthcare setting is the electronic medical record (EMR), which is the “legal record created in hospitals and ambulatory environments that enables health facilities to capture, store, analyze and communicate patient health information in an electronic format” (10, 11).
Despite large investments to support the adoption of EMRs, the adoption rate of such systems is still low, and little progress has been made to harness the benefits of EMRs, particularly in developing countries (12). The implementation of the EMR is not consistent across healthcare facilities and its use is met with an alarming rate of failure in resource-poor settings (13–15). Due to limited resources, most electronic systems are still being used side by side with paper documentation, which is creating a burden on health service providers (16–18).
In developed countries such as the USA, more than three-quarter of health professionals (81.7%) are using EMRs, while in developing countries like Ethiopia, the use of EMR by health professionals is very low (19, 20). A study in sub-Saharan countries showed “the complexity and impact of social considerations, outweighing product and EMR system limitations” (21). Similarly, the utilization of digital health investments for planning and decision-making in Ethiopia has not been a priority so far and generally inadequately supported and poorly managed (3).
The current health sector transformation plan (HSTP) of Ethiopia envisioned “all of its citizens enjoying equitable and affordable access to all types of health services” through the transformation agenda of the Information Revolution (3). In this regard, the use of the electronic medical record represents one of the key instruments in improving healthcare delivery (6, 7, 22). The Ethiopian “Ministry of Health with support of the Tulane University Technical Assistance Project in Ethiopia (TUTAPE) and CDC started the development and implementation of a comprehensive EMR system for hospitals called SmartCare in 2009. The system was deployed in 5 hospitals in Addis Ababa and other hospitals in regional cities. In 2013, the Ministry of Health adapted the system as a national EMR for all hospitals, and planned to scale it up to further hospitals and regions” (23, 24). All urban health facilitates in the Diredawa Administration were selected for the initial phase of implementation and chosen as a pilot site (23).
However, the current rate of utilization since EMR implementation in Dire Dawa is unknown (24). Moreover, no study has been conducted on the utilization status of EMRs and individual and organization determinants in the study area. Therefore, this study is aimed to fill the knowledge gaps related to EMR utilization and its determinants among healthcare providers in the Dire Dawa city administration in eastern Ethiopia.
Methods
Study design and setting
An institution-based quantitative cross-sectional study supplemented with an exploratory qualitative approach was conducted at public health facilities in the Dire Dawa city administration from April 7 to May 7, 2019. Dire Dawa, an industrial hub and home to several market centers, is located in eastern Ethiopia and has 14 health centers, 2 hospitals, and 32 health posts with a total of 629 health professionals including health extension workers.
Study participants
The participants for this study were all healthcare providers selected randomly across two hospitals and seven health centers. A sample size of 446 was estimated with an assumption of a 95% confidence level, 80% power, and 10% non-response rate. However, as the numbers of healthcare providers were manageable (489), all healthcare providers were included in the data collection process. To better understand what factors influence EMR use, we also conducted in-depth interviews with nine key informants who had better knowledge and experience of the EMR in their organizations. The key informants were purposefully selected on the basis of their role in Health Management Information System (HMIS) and healthcare data quality issues. All healthcare providers who were selected randomly across health facilities and who served for at least 6 months were approached to fill up the questionnaire.
Data collection and quality control methods
A pretested semistructured questionnaire was used, which was supplemented with in-depth interview guides. These tools were adapted and constructed from PRISM tools (25) and from previously conducted studies (24, 26, 27). Data were divided into two types, namely, quantitative data and qualitative data; five clinical nurses and five health officers were employed for collecting quantitative data, whereas two data collectors experienced with qualitative data collection carried out the in-depth interviews. Healthcare providers who were unavailable at the time of study were repeatedly visited to minimize the rate of high non-responses. Three item questions with in-depth probing were adopted and contextualized from other studies (28, 29). The key informant interviews were sound-recorded using the Sony ICD PX470 sound recorder. To avoid desirability bias, none of the study participants were made to know about the data collectors in person. Upon completion of each in-depth interview, a trained biostatistician produced a complete transcript and translation. Strict supervision and double data entry were made for data quality control.
Measurements
The dependent variable: EMR use was measured if a participant used the EMR for one or more of the following functions: (1) finding patients with certain characteristics, (2) making notes (history and physical exam), (3) entering orders (lab, radiology), (4) reviewing/obtaining lab and radiology results, (5) updating diagnosis, (6) reviewing currently received medications, (7) writing prescriptions, (8) admitting a patient, (9) referring a patient, (10) viewing/scheduling appointment for a patient, (11) communicating using Smart Care’s communication/report sending, and (12) producing patient summary reports/report generating. The respondent's computer skills were assessed using a 10-question score as follows: Internet browsing, calculations, email communication, database management, ability to check data accuracy, plot data by months or years, compute trends from bar charts, explain findings and their implications, use data for identifying gaps and setting targets, and use data for making various types of decisions and providing feedback. A mean score >95 denoted excellent, 80–95, very good, 65–80 good, 50–64 fair, and <50 poor. Perceived EMR system quality was assessed using five-item questions (please check the Questionnaire in Supplementary Materials), and a two-scale score was used to classify it as good or poor. Perceived service quality was assessed using nine-item questions (please check the Questionnaire in supplementary materials), and a two-scale score was used to classify it as good or poor. Similarly, perceived information quality was assessed using seven-item questions (please check the Questionnaire in Supplementary Materials), and a two-scale score was used to classify it as good or poor.
Data analysis
All analyses were performed using STATA 14.1 version. Descriptive summary statistics were used to describe the characteristics of study participants with EMR use. Bivariate and multivariable logistic regression was employed to identify factors affecting EMR use. All statistics with a p-value <0.05 were declared significant. The collected qualitative data were transcribed, coded, and thematically analyzed using ATLAS ti 7.5.4. Coding was made inductively during data analysis. The inductive approach was used by semantically analyzing the explicit content of the data to determine our themes.
Ethical considerations
This study was done following the principles stated in the Declaration of Helsinki. This study was approved by the Institutional Health Research Ethics Review Committee of Haramaya University with Reference number IHRERC/104/2019. Permission for data collection was obtained from health facilities. Written and signed informed consent was obtained from the study participants in a form provided with the Questionnaire.
Results
Socio-demographic characteristics of study participants
Out of the 489 study participants, 402 (82.2%) responded to the questionnaires. The majority (55%) of the respondents were females (Table 1). The mean age of the respondents was 31.30 (±6.61 SD) years. More than one-third of the participants (37.8%) had more than 6 years of experience, whereas about three-quarter (76.6%) of the respondents were degree holders. For the qualitative in-depth interviews, seven HMIS/health informatics technicians (HIT) staff members and two health facility heads were involved. Five of the key informants were females. All of them were married; six of them were degree holders.
Table 1.
Socio-demographic characteristics of the study participants, Dire Dawa, Ethiopia, 2019 (n = 402).
| Variable | Category | Freq. | Percent |
|---|---|---|---|
| Sex | Female | 219 | 54.48 |
| Male | 183 | 45.52 | |
| Age (years) | 20–24 | 36 | 8.96 |
| 25–29 | 151 | 37.56 | |
| 30–34 | 123 | 30.60 | |
| 35 and above | 92 | 22.89 | |
| Residence | Urban | 342 | 85.07 |
| Rural | 60 | 14.93 | |
| Marital status | Single | 160 | 39.80 |
| Married | 231 | 57.46 | |
| Others | 11 | 2.74 | |
| Education | Diploma | 77 | 11.16 |
| Degree | 308 | 76.62 | |
| Masters and above | 17 | 4.23 | |
| Work experience | ≤ 6 years | 250 | 62.19 |
| >6 years | 152 | 37.81 | |
| Profession | All Nurses | 256 | 63.68 |
| Laboratory technicians | 45 | 11.2 | |
| Physicians | 38 | 9.46 | |
| Health Officers | 32 | 7.96 | |
| Pharmacist | 31 | 7.71 | |
| Average monthly Income in ETB | 601–1,650 | 10 | 2.49 |
| 1,651–3,200 | 50 | 12.44 | |
| 3,201–5,250 | 186 | 46.27 | |
| 5,251–7,800 | 97 | 24.13 | |
| 7,801–10,900 | 43 | 10.70 | |
| Over 10900 | 16 | 3.98 |
ETB, Ethiopian birr.
Accessibility, functional status, and computers skills of health professionals
A majority of the study participants 243 (60.45%) had access to at least one computer in their working desk (excluding the personal computer), of which about 85% were functional at the time of the study. (Table 2) More than two-third of the current users (178 (73.25%)) are using this computer (s) for data recording, and an additional 141 (58.02%) and 74 (30.45%) of them use the available computer (s) for report generating and reading, respectively.
Table 2.
Accessibility, functional status, and computer skills of healthcare professionals, Dire Dawa (n = 402).
| Variable | Categories | Frequency | Percent |
|---|---|---|---|
| Have access to computer(s) | Yes | 243 | 60.45 |
| No | 159 | 39.55 | |
| Number of accessible computer(s) | 1 | 178 | 73.25 |
| 2 | 42 | 17.28 | |
| 3 | 11 | 4.53 | |
| ≥4 | 12 | 4.94 | |
| Computer's functionality | Yes | 207 | 85.19 |
| No | 36 | 14.81 | |
| Share the available computer(s) with others | Yes | 194 | 79.84 |
| No | 49 | 20.16 | |
| Number of health professional(s) with whom they share their computers | 0 | 47 | 19.34 |
| 1 | 19 | 7.82 | |
| 2 | 38 | 15.64 | |
| 3 | 51 | 20.99 | |
| 4 and above | 88 | 36.21 | |
| Computer skill | Fair | 202 | 50.25 |
| Poor | 200 | 49.75 |
EMR use and related characteristics
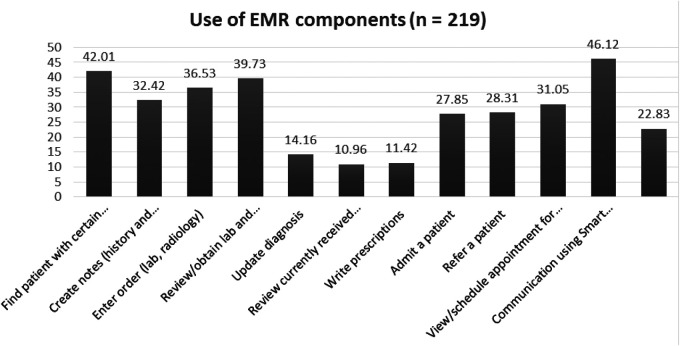
Overall, 388 (96.52%) of the participants are aware of the EMR and more than half (54.48%) of them have used it before. Just over a quarter of health professionals (107 (26.61%) are currently using EMRs. The EMR is most commonly used for sending reports (46.12%), followed by finding patients with certain characteristics 42.01% (Figure 1).
Figure 1.
Use of the basic EMR components by health professionals, Dire Dawa, Ethiopia, 2019.
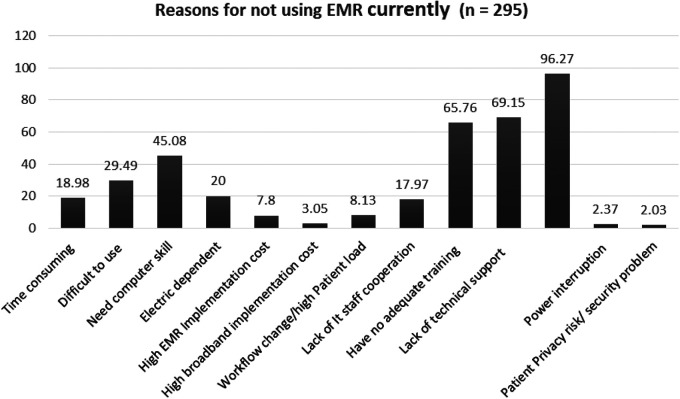
Furthermore, about two-thirds of the current users 71 (66.4%) are nurses, followed by laboratory technicians 15 (14.02%), health officers 10 (9.35%), physicians 10 (9.35%), and pharmacists. Moreover, the main reported reasons for the current non-use of the EMR are the unavailability of the functional installed EMR software program [the SmartCare installed by Tulane University is outdated due to project phase-out (Figure 2)].
Figure 2.
Reported reasons for not currently using the EMR system Dire Dawa, Ethiopia, 2019.
The majority 260 (64.68%) of the participants have received HMIS training, while 267 (66.42%) have been trained on EMR use. However, only 174 (65.17%) of the participants use EMRs after training, and only 63 (15.67%) of the participants own the EMR manual. Furthermore, only 33 (8.21%) participants hold regular discussions on the EMR during performance monitoring team meetings.
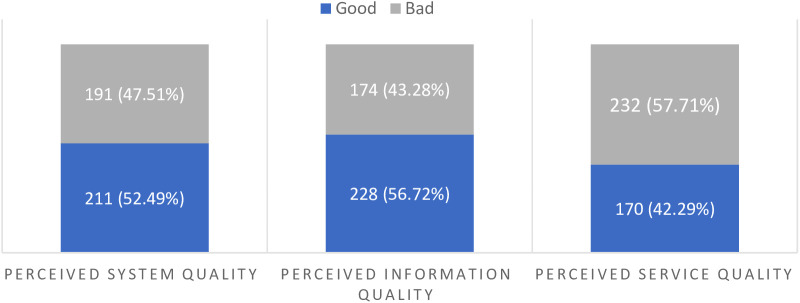
Health professionals' acceptance and attitude toward the EMR
In general, when respondents were asked about EMRs, 287 (71.39%), 256 (63.68%), 255 (63.43%), and 266 (66.17%) of them agreed that they fully accepted them, believed that they improved their productivity, preferred them over paper-based record, and agreed that electronic recording of patient data had an impact on data quality, respectively. Moreover, there were significant differences in EMR use among healthcare providers with respect to their views on EMR service quality, EMR system quality, and perceived EMR information quality (Figure 3).
Figure 3.
Study participants’ perceived EMR system, information, and EMR service quality, Dire Dawa, Ethiopia, 2019.
Factors associated with EMR use
In the final multivariable logistic regression analysis, the following variables were found to independently predict EMR use; work experience, access to the EMR manual, discussions on the EMR in meetings, positive perceived EMR system quality, perceived service quality, and perceived benefit of the EMR (Table 3).
Table 3.
Factors associated with EMR use by health professionals working in urban public health facilities, Dire Dawa, Ethiopia, 2019 (n = 402).
| Variables | Response | EMR use (%) |
COR (95% CI) | AOR (95% CI) | p-Value | |
|---|---|---|---|---|---|---|
| Use | Do not use | |||||
| Work experience | >6 years | 31 (20.4) | 121 (79.6) | 1 | 1 | |
| ≤6 years | 76 (30.4) | 174 (69.6) | 1.70 (1.06–2.75) | 2.13 (1.08–4.20) | 0.03 | |
| Computer skill | Poor | 40 (20.0) | 160 (80.0) | 1 | 1 | |
| Fair | 67 (33.2) | 135 (66.8) | 1.98 (1.26–3.12) | 1.32 (0.68–2.56) | 0.41 | |
| Smart care training | No | 26 (19.3) | 109 (80.7) | 1 | 1 | |
| Yes | 81 (30.3) | 186 (69.7) | 1.82 (1.10–3.01) | 0.45 (0.20–1.01) | 0.06 | |
| Presence of EMR manual | No | 66 (19.5) | 273 (80.5) | 1 | 1 | |
| Yes | 41 (65.1) | 22 (34.9) | 7.71 (4.30–13.82) | 3.01 (1.23–7.40) | 0.02 | |
| Having discussions on EMRs in any meeting | No | 62 (17.9) | 284 (82.1) | 1 | 1 | |
| Yes | 45 (80.4) | 11 (19.6) | 18.74 (9.2–38.3) | 15.23(5.70–40.74) | 0.001 | |
| Perceived service quality | Poor | 23 (9.9) | 209 (90.1) | 1 | 1 | |
| Good | 84 (49.4) | 86 (50.6) | 8.88 (5.25–15.00) | 8.31 (4.11–16.80) | 0.001 | |
| Perceived information quality | Poor | 25 (14.4) | 149 (85.6) | 1 | 1 | |
| Good | 82 (36.0) | 146 (64.0) | 3.35 (2.02–5.53) | 1.87 (0.85–4.08) | 0.12 | |
| Perceived system quality | Poor | 13 (6.8) | 178 (93.2) | 1 | 1 | |
| Good | 94 (44.6) | 117 (55.4) | 11.00 (5.9–20.55) | 7.38 (2.97–18.34) | 0.001 | |
| Perceived EMR benefits to facilities | Do not benefit | 67 (23.4) | 219 (76.6) | 1 | 1 | |
| Benefit | 40 (34.5) | 76 (65.5) | 1.72 (1.07–2.75) | 0.33 (0.06–1.65 | 0.18 | |
| Perceived EMR benefits to patients | Do not benefit | 65 (22.0) | 231 (78.0) | 1 | 1 | |
| Benefit | 42 (39.6) | 64 (60.4) | 2.33 (1.45–3.76) | 5.51 (1.10–27.67) | 0.04 | |
EMR, electronic medical record; AOR, adjusted odds ratio; CI, confidence intervals: COR, crude odds ratio.
Respondents with a work experience of 6 years or less were about two times more likely to use EMRs than those with a work experience of greater than 6 years [adjusted odds ratio (AOR) = 2.13; 95% confidence interval (CI) = [1.08–4.20]]. Study participants who had access to the EMR manual were three times more likely to use the EMR system than those who had no EMR manual (AOR = 3.01; 95% CI = [1.23–7.40]). Those health professionals who reported having a discussion on EMRs in any meeting were about 15 times more likely to use them compared with those who did not have any discussion on them (AOR = 15.23; 95% CI = [5.70–40.74]). Respondents with good perceived EMR service quality were eight times more likely to use EMRs than those with a poor perception of EMR service quality (AOR = 8.31; 95% CI = [4.11–16.80]). Similarly, respondents with good EMR system quality were about seven times more likely to use EMRs than those with poor perceived EMR system quality (AOR = 7.38; 95% CI [2.97–18.34]).
Health professionals who thought EMRs will benefit patients were about 5.5 times more likely to use them than those who said they will not benefit patients [AOR: 5.51; 95%CI (1.10–27.67)] (Table 3).
Challenges of EMR use (qualitative finding)
Multiple factors that influence EMR use were cited by key informants during the in-depth interviews. Common themes were organized as organizational, technical, and behavioral factors during analysis (Table 4). The most common significant barrier cited by key informants for not using EMRs was the lack of EMR software installed on computers as well as lack of management commitment to integrate EMRs into patient data recording.
Table 4.
Common themes identified during in-depth interviews on factors affecting health professionals’ EMR use.
| Organizational factors | sGood governance problems, (ii) lack of budget for training and maintenance, (iii) dual documentation system, (iv) poor supervision and support, (v) work overload/shortage of time, (vi) inadequate HIT professionals, (vii) lack of incentives for good performance, (viii) poor coordination and mentoring process, (ix) ownership problems from health institutions. |
| Technical factors | (i) lack of a locally designed EMR software program, (ii) old and non-functional computers, (iii) electricity interruption, (iv) Inadequate EMR training, (v) lack of timely maintenance and repair of computers, (vi) expired EMR software program. |
| Behavioral factors | (i) lack of computer skills and knowledge, (ii) poor commitment from users and management, (iii) lack of interest in adapting to a computerized system, (iv) challenges in motivating staff, (v) carelessness from staff and management, (vi) intentional resistance to use EMRs. |
| Environmental factors | (i) Poor collaboration from stakeholders, (ii) dependence on NGOs’ software program, (iii) hot weather conditions. |
HMIS focal person from the Dire Dawa City Health Bureau reported: “Poor commitment from all health professionals and governing body working in the facilities takes the major share of barriers. Some health professionals are not even interested and motivated to manually record patient data. Some health professionals also consider working with computer as an extra burden.” This finding is supplemented by the quantitative finding where despite receiving training on EMR use, most health professionals were not using it.
Another point raised by key informants is health professionals’ attitude toward the EMR (Table 4). Some respondents cited that some health professionals get agitated with filling data in computers and rather prefer to use paper-based record.
Technical factors were also cited as one factor for the non-use of EMRs. A 32-year-old HIT staff at one of the health facilities said, “If the program malfunctioned or gets corrupted, there was no timely maintenance.” He added, “There was no replacement for even a single malfunctioned Socket or divider.”
Discussion
This study revealed that only a quarter of health professionals were using EMRs. This finding indicated low use compared with a finding in the USA (13), Hyder hospital in Tigray, and Amhara states in Ethiopia (24, 30, 31). None of the urban health facilities had a fully functional EMR system. A few service delivery units such as antiretroviral treatment (ART) clinics and patient registration offices were using the EMR system in conjunction with paper-based records. This resulted from technical challenges related to EMRs, non-functional computers, electricity interruption, and the lack of timely maintenance and repair of computers. Moreover, healthcare providers’ behavioral factors such as poor computer literacy, poor commitment, and lack of interest in adapting to electronic recording were mentioned.
This study also found that poor collaboration from stakeholders and dependence on NGOs for the EMR program were cited as major factors. The respondents indicated that the software was designed by a non-governmental organization (NGO) (Tulane University), and after the project was phased out, the EMR service was also stopped due to the lack of necessary infrastructure for integrating the EMR with other existing information systems. Other studies indicated that the dependence of developing countries on third-party vendor systems for EMRs, which usually involve unsustainable IT infrastructure and software management, were identified as significant barriers in EMR implementation (23, 32–34).
However, this study finding is in line with those of other studies conducted in Ethiopia's Amhara Region (30) and in Addis Ababa (24). The lack of administrative and policy support and lack of available funding are cited by key informants as major barriers to EMR use. More than two-third of the respondents are in favor of EMR implementation and its positive effects on quality of care, which is supported by studies conducted in the Tigray region (27) and USA (35). The literature indicates that most health professionals have accepted the role of automated notes and records in improving healthcare quality (5, 36), though the lack of infrastructure has hindered the full implementation of the system. In general, barriers associated with hardware and software resources are the most commonly cited barriers to EMR use by health professionals in this study.
Health professionals with a work experience of 6 years or less are twice more likely to use EMRs compared with those with work experience greater than 6 years. This finding is similar to that of a study conducted in northern Ethiopia (27). Studies have shown that the gap in the knowledge and skills of health workers significantly influences data management processes (3, 37). Variations in terms of computer literacy, educational level, and personal commitment in this study could be an explanation for low EMR use among health professionals. Having discussions on EMRs in any meeting and the presence of the EMR manual are predictors of EMR use in this study. These findings are in line with those of other studies elsewhere in Ethiopia (20, 24, 27) and the USA (38).
In contrast to studies conducted in different regions of Ethiopia (24, 27, 37), Iran (39), the USA (38), and Cyprus (40), training in the EMR system had no influence on EMR use in our study. From the logical point of view, training can improve the knowledge, attitude, and skills of health professionals. However, having adequate training by itself cannot be a driving factor unless the EMR system is continuously maintained and the staff are motivated to use EMR. In addition, key informants stated that the benefits of training have not reached those who actively engage in EMR use, including card room and ART units. Inadequate IT professionals have also been cited by key informants as a reason for low EMR utilization.
Further, this study revealed that the attitude toward EMR system quality influences the utilization of the EMR system. Health professionals with good opinion on EMR service quality and EMR system quality are more likely to use EMRs than their counterparts are. This finding is consistent with that of a study conducted in Addis Ababa (24). This is evident as users' acceptance is the primary determinant of effective utilization of any program (41, 42).
The qualitative finding identified major organizational, technical, and behavioral factors as the major obstacles to EMR use by health professionals. These determinants have also been cited by other studies from the USA (43), Saudi Arabia (28), and the UK (29). Organizational (13, 35, 39, 44), technical, and most importantly behavioral (38, 39) factors were identified to be important determinants hindering effective and efficient utilization of EMRs.
This cross-sectional study included only urban public health facilities. An extensive overview of overall EMR utilization status requires an inclusion of health posts and rural and private health facilities. The generalizability of the finding of this study may not apply to these facilities. Further, use was not assessed from a multilevel perspective across individual and organizational levels.
Conclusions
The immense benefits offered by EMRs were very poorly utilized in this study area. Only a quarter of the respondents surveyed said that they used EMRs in their day-to-day activities. Organizational determinants (EMR manual presence, absence of EMR software program, smart care training, and attending regular discussions on the EMR) and individual factors (views on the benefits of the EMR to patients, perceived system quality, and service quality) had a significant influence on the utilization of the EMR. Successful utilization of the EMR requires the support and commitment of all stakeholders. Interventions should focus on improving user support, stabilizing power fluctuations, improving computer infrastructure, and providing continuous training.
Acknowledgments
The authors are grateful to data collectors and participating facilities in Dire Dawa for their assistance during data collection. We would also like to thank Haramaya University for funding this study.
Funding
This work was funded by Haramaya University.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Health Research Ethics Review Committee (IHRERC) of Haramaya University, College of Health and Medical Sciences (Ref. No. IHRERC/104/2019). The patients/participants provided their written informed consent to participate in this study.
Author contributions
AT initiated the study. LO, TD, AA, and HSR assisted in the design, collection, analysis, and interpretation and thoroughly revised the manuscript. AT prepared the first draft manuscript, and LO, TD, AA, and HSR thoroughly revised the draft and substantially contributed to the finalization of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdgth.2022.935945/full#supplementary-material.
References
- 1.Beyette FR, Gaydos CA, Kost GJ, Weigl BH. Point-of-Care technologies for health care. IEEE Trans Biomed Eng. (2011) 58(3):732–5. 10.1109/TBME.2011.2109251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiuchisan I, Costin H, Geman O. Adopting the internet of things technologies in health care systems. 2014 International Conference and Exposition on Electrical and Power Engineering (EPE) (2014). [Google Scholar]
- 3.EFMoH. (Ethiopian Federal ministry of Health); “Information Revolution Roadmap” Addis Ababa, Ethiopia (2016).
- 4.Hillestad R, Bigelow J, Bower A, Girosi F, Meili R, Scoville R, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff. (2005) 24(5):1103–17. 10.1377/hlthaff.24.5.1103 [DOI] [PubMed] [Google Scholar]
- 5.Amarasingham R, Plantinga L, Diener-West M, Gaskin DJ, Powe NR. Clinical information technologies and inpatient outcomes: A multiple hospital study. Arch Intern Med. (2009) 169(2):108–14. 10.1001/archinternmed.2008.520 [DOI] [PubMed] [Google Scholar]
- 6.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. (2006) 144(10):742–52. Available from 10.7326/0003-4819-144-10-200605160-00125 [DOI] [PubMed] [Google Scholar]
- 7.Krist AH, Green LA, Phillips RL, Beasley JW, DeVoe JE, Klinkman MS, et al. Health information technology needs help from primary care researchers. J Am Board Fam Med. (2015) 28(3):306–10. 10.3122/jabfm.2015.03.140246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin SC, Jha AK, Adler-Milstein J. Electronic health records associated with lower hospital mortality after systems have time to mature. Health Aff. (2018) 37(7):1128–35. 10.1377/hlthaff.2017.1658 [DOI] [PubMed] [Google Scholar]
- 9.Tomasi E, Facchini LA, Maia MF. Health information technology in primary health care in developing countries: A literature review. Bull World Health Organ. (2004) 82(11):867–74. s0042-96862004001100012 [PMC free article] [PubMed] [Google Scholar]
- 10.Garets D, Davis M. Electronic medical records vs. Electronic health records: Yes, there is a difference. Policy white paper. Chicago, HIMSS Analytics. (2006): 1–14. [Google Scholar]
- 11.Häyrinen K, Saranto K, Nykänen P. Definition, structure, content, use and impacts of electronic health records: A review of the research literature. Int J Med Inform. (2008) 77(5):291–304. 10.1016/j.ijmedinf.2007.09.001 [DOI] [PubMed] [Google Scholar]
- 12.O’Donnell A, Kaner E, Shaw C, Haighton C. Primary care physicians’ attitudes to the adoption of electronic medical records: A systematic review and evidence synthesis using the clinical adoption framework. BMC Med Inform Decis Mak. (2018) 18(1):101. 10.1186/s12911-018-0703-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gabriel MH, Jones EB, Samy L, King JJHA. Progress and challenges: Implementation and use of health information technology among critical-access hospitals. Health Aff. (2014) 33(7):1262–70. 10.1377/hlthaff.2014.0279 [DOI] [PubMed] [Google Scholar]
- 14.Meinert DB. Resistance to electronic medical records(EMRs): A barrier to improved quality of care. Informing Science: The International Journal of an Emerging Transdiscipline (InformingSciJ). (2005) 2:493–504. 10.28945/2896 [DOI] [Google Scholar]
- 15.Russo E, Sittig DF, Murphy DR, Singh H. Challenges in patient safety improvement research in the era of electronic health records. Healthcare. (2016) 4(4):285–90. 10.1016/j.hjdsi.2016.06.005 [DOI] [PubMed] [Google Scholar]
- 16.Abiy R, Gashu K, Asemaw T, Mitiku M, Fekadie B, Abebaw Z, et al. A comparison of electronic records to paper records in Antiretroviral Therapy Clinic in Ethiopia: What is affecting the quality of the data? Online J Public Health Inform. (2018) 10(2):e212. 10.5210/ojphi.v10i2.8309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saleem JJ, Russ AL, Justice CF, Hagg H, Ebright PR, Woodbridge PA, et al. Exploring the persistence of paper with the electronic health record. Int J Med Inf. (2009) 78(9):618–28. 10.1016/j.ijmedinf.2009.04.001 [DOI] [PubMed] [Google Scholar]
- 18.Sikhondze NC, Erasmus L. Electronic medical records: A developing and developed country analysis. Research Space, the institutional repository of the CSIR. (2016). Available from http://iamot2016.org/proceedings/papers/IAMOT_2016_paper_32.pdf; http://hdl.handle.net/10204/9204 [Google Scholar]
- 19.Adler-Milstein J, DesRoches CM, Kralovec P, Foster G, Worzala C, Charles D, et al. Electronic health record adoption in US hospitals: Progress continues, but challenges persist. Health Aff. (2015) 34(12):2174–80. 10.1377/hlthaff.2015.0992 [DOI] [PubMed] [Google Scholar]
- 20.Biruk S, Melesse T, Andualem M, Tilahun B. Health professionals readiness to implement electronic medical record system at three hospitals in Ethiopia: A cross sectional study. BMC Med Inform Decis Mak. (2014) 14(1):1–8. 10.1186/s12911-014-0115-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jawhari B, Ludwick D, Keenan L, Zakus D, Hayward R. Benefits and challenges of EMR implementations in low resource settings: A state-of-the-art review. BMC Med Inform Decis Mak. (2016) 16(1):116. 10.1186/s12911-016-0354-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kemkarl O, Dahikar D. Can electronic medical record systems transform health care? Potential health benefits, savings, and cost using latest advancements in ict for better interactive healthcare learning. Health Aff. (2012) 2(3/6):453–5. 10.1377/hlthaff.24.5.1103 [DOI] [Google Scholar]
- 23.Mengesha T. Electronic solutions for Ethiopian health sector. Autumn: Oulu University (2011).
- 24.Tilahun B, Fritz F. Comprehensive evaluation of electronic medical record system use and user satisfaction at five low-resource setting hospitals in Ethiopia. JMIR Med Inform. (2015) 3(2):e22–e22. 10.2196/medinform.4106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.USAID. (United States Agency for International Development) Performance of Routine Information System Management (PRISM) Toolkit, ISBN: 978-1-64232-065-7; Available at: https://www.measureevaluation.org/ resources/tools/rhis-rat/routine-health-information-system-rapid-assessment-tool) (2019).
- 26.Teklegiorgis K, Tadesse K, Terefe W, Mirutse G. Level of data quality from Health Management Information Systems in a resources limited setting and its associated factors, eastern Ethiopia: Original research. S Afr J Inf Manag. (2016) 18(1):1–8. 10.1377/hlthaff.24.5.1103 [DOI] [Google Scholar]
- 27.Yehualashet G, Asemahagn M, Tilahun B. The attitude towards and use of electronic medical record system by health professionals at a referral hospital in northern Ethiopia: Cross-sectional study. J Health Inform Afr. (2015) 3:1. 10.12856/JHIA-2015-v3-i1-124 [DOI] [Google Scholar]
- 28.Khalifa M. Barriers to health information systems and electronic medical records implementation. A field study of Saudi Arabian hospitals. Procedia Comput Sci. (2013) 21:335–42. 10.1016/j.procs.2013.09.044 [DOI] [Google Scholar]
- 29.Murray E, Burns J, May C, Finch T, O'Donnell C, Wallace P, et al. Why is it difficult to implement e-health initiatives? A qualitative study. Implement Sci. (2011) 6(1):6. 10.1186/1748-5908-6-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andualem Asemahagn M. The functionality status and challenges of electronic health management information system: The case of public health centres in Amhara Region, Ethiopia. Cogent Med. (2018) 5(1):1437672. 10.1080/2331205X.2018.1437672. [DOI] [Google Scholar]
- 31.Berhe M, Tadesse K, Berhe G, Gebretsadik T. Evaluation of electronic medical record implementation from user’s perspectives in Ayder referral hospital Ethiopia. J Heal Med Informatics. (2017) 8(249):2. 10.4172/2157-7420.1000249 [DOI] [Google Scholar]
- 32.Heeks R. Information systems and developing countries: Failure, success, and local improvisations. Inf Soc. (2002) 18(2):101–12. 10.1080/01972240290075039 [DOI] [Google Scholar]
- 33.Rotich JK, Hannan TJ, Smith FE, Bii J, Odero WW, Vu N, et al. Installing and implementing a computer-based patient record system in sub-saharan Africa: The mosoriot medical record system. J Am Med Inform Assoc: JAMIA. (2003) 10(4):295–303. 10.1197/jamia.M1301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wong R, Bradley EH. Developing patient registration and medical records management system in Ethiopia. Int J Qual Health Care. (2009) 21(4):253–8. 10.1093/intqhc/mzp026 [DOI] [PubMed] [Google Scholar]
- 35.DesRoches CM, Campbell EG, Rao SR, Donelan K, Ferris TG, Jha A, et al. Electronic health records in ambulatory care—a national survey of physicians. N Engl J Med. (2008) 359(1):50–60. 10.1056/NEJMsa0802005 [DOI] [PubMed] [Google Scholar]
- 36.Sukums F, Mensah N, Mpembeni R, Kaltschmidt J, Haefeli WE, Blank A. Health workers’ knowledge of and attitudes towards computer applications in rural African health facilities. Glob Health Action. (2014) 7(1):24534. 10.3402/gha.v7.24534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gebre-Mariam M, Borycki E, Kushniruk A, Purkis ME. An Electronic Medical Record (EMR) Implementation Framework for HIV Care and Treatment Facilities in Ethiopia (2012).
- 38.Holden RJ. What stands in the way of technology-mediated patient safety improvements? A study of facilitators and barriers to physicians’ use of electronic health records. J Patient Saf. (2011) 7(4):193. 10.1097/PTS.0b013e3182388cfa [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ayatollahi H, Mirani N, Haghani H. Electronic health records: What are the most important barriers? Perspect Health Inf Manag. (2014) 11(Fall):1c. PMID: [PMC free article] [PubMed] [Google Scholar]
- 40.Samoutis G, Soteriades ES, Kounalakis DK, Zachariadou T, Philalithis A, Lionis C. Implementation of an electronic medical record system in previously computer-naive primary care centres: A pilot study from Cyprus. Inform Health Soc Care. (2007) 15(4). 10.14236/jhi.v15i4.660 [DOI] [PubMed] [Google Scholar]
- 41.Raja EEJ, Mahal R, Masih VB. An exploratory study to assess the computer knowledge, attitude and skill among nurses in health care setting of a selected hospital in Ludhiana, Punjab, India. Stud Health Technol Inform. (2004) 107(Pt 2):1304–7. 10.3233/978-1-60750-949-3-1304 [DOI] [PubMed] [Google Scholar]
- 42.Rao SR, DesRoches CM, Donelan K, Campbell EG, Miralles PD, Jha AK. Electronic health records in small physician practices: Availability, use, and perceived benefits. J Am Med Inform Assoc. (2011) 18(3):271–5. 10.1136/amiajnl-2010-000010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yoon-Flannery K, Zandieh S, Kuperman G, Langsam D, Hyman D, Kaushal R. A qualitative analysis of an electronic health record (EHR) implementation in an academic ambulatory setting. J Innov Health Inform. (2008) 16(4): 277–84. 10.14236/jhi.v16i4.703 [DOI] [PubMed] [Google Scholar]
- 44.Gyamfi A, Mensah KA, Oduro G, Donkor P, Mock CN. Barriers and facilitators to electronic medical records usage in the emergency centre at komfo anokye teaching hospital, Kumasi-Ghansa. Afr J Emerg Med. (2017) 7(4):177–82. 10.1016/j.afjem.2017.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.