Abstract
Chronic kidney disease (CKD) is a widely diffuse pathological condition which deeply impacts upon an affected patient’s quality of life and its worldwide rate is predicted to further rise. The main biological mechanism underlying CKD is renal fibrosis, a non-reversible process representing, for the affected system, a point of no return of tissue damage and dysfunction, deeply reducing the possible therapeutic strategies at the disposal of physicians. The best tool clinicians can use to address the extent of renal fibrosis at any level (glomeruli, tubule-interstitium, vasculature) is kidney biopsy that, despite its overall safety, remains an invasive procedure showing some shortcomings. Thus, the identification of novel non-invasive renal fibrosis biomarkers would be of fundamental importance. Here, when systematically reviewing the available evidence on serological biomarkers associated with renal fibrosis evaluated in patients suffering from CKD in the last five years, we found that despite the presence of several promising biomarkers, the level of observed evidence is still very scattered. Probably, the use of multiple measures capable of addressing different aspects involved in this condition would be the most suitable way to capture the high complexity characterizing the renal fibrotic process, having consequently a great impact on clinical practice by maximizing prevention, diagnosis, and management.
Keywords: chronic kidney disease, renal fibrosis, biomarkers
1. Introduction
Chronic kidney disease (CKD) is one of the most important diseases in terms of morbidity and mortality, and its progressive evolution deeply impacts on the quality of life of the affected patients. In fact, recent studies have shown that around 10% of the population is affected by CKD, and millions die every year because of the impossibility to access affordable treatment [1,2]. Despite the outstanding progress of modern medicine, the worldwide rate of CKD is predicted to further rise, given the aging of the population and the parallel increase in the prevalence of numerous diseases leading to the condition [3,4,5,6]. As reported in a recent work by the Global Burden Disease (GBD) Chronic Kidney Disease Collaboration, the prevalence of CKD is estimated as 9.1% in the general population, with CKD stages 1–2 accounting for 5%, stage 3 for 3.9%, stage 4 for 0.16%, and stage 5 for 0.07% [7]. In most cases, the outcome is nefarious and patients inevitably undergo end-stage renal disease (ESRD), dialysis, or kidney transplantation. The estimated number of patients receiving renal replacement therapy accounts for more than 2.5 million, a number that is projected to double by 2030 [7,8]. Moreover, this number may only represent 10% of people who need treatment to live [8], and the situation is even more severe if we consider that CKD represents an independent risk factor for cardiovascular disease (CVD), impacting also upon CVD mortality [7,9,10]. Thus, CKD represents a global health burden, with significant costs required to manage the clinical complexity of these patients.
While a growing body of evidence is supporting researchers worldwide to understand the magnitude of the problem, we are currently only scratching the surface of the complex systems of interactions leading to CKD. The main biological mechanisms characterizing CKD, slowly leading to kidney failure and dysfunction, are represented by renal fibrosis.
Fibrosis is a non-reversible process that represents, for the affected system, a point of no return of tissue damage and dysfunction, deeply reducing the possible therapeutic strategies at the disposal of clinicians [11,12].
The fibrotic process could be described as a “failed wound healing”, or as an excessive accumulation of extracellular matrix (ECM). Allowing tissue regeneration, which is a fundamental response to injury, is important, but the exaggeration of this event leads to a pathologic outcome [13,14]. Chronic fibrogenesis induces a shift from supportive fibrotic tissue to a microenvironment in which the increase in the number and activity of ECM-producing cells results in excessive ECM deposition, and consequently in the disruption of the normal parenchymal architecture, interfering with organ function [15,16,17].
Measurements such as serum creatinine, estimated glomerular filtration rate (eGFR), and albuminuria are routinely used when evaluating CKD patients, but they predominantly reflect glomeruli health, and they cannot fully capture all the components of kidney damage. The best tool that clinicians can use to this purpose is kidney biopsy, which allows them to evaluate the severity of tissue damage at any level: glomeruli, tubule-interstitium, and vasculature [18,19,20]. Indeed, together with glomerulosclerosis, tubulointerstitial fibrosis and atherosclerosis are common findings in most CKD forms and their severity results are reliable to predict kidney failure progression. Nonetheless, regardless of its overall safety, biopsy remains an invasive procedure [18,21,22] and its use to periodically monitor the progression of the diseases is limited to specific circumstances.
The identification of biomarkers that allow for the estimation of kidney fibrosis and damage progression in a non-invasive manner would be of fundamental importance, in order to help treating physicians to tailor strategies to improve patients’ diagnosis, management, and responsiveness to therapy. Nowadays however, evidence on new biomarkers and their association to the histological findings are still heterogeneous and a consensus is still lacking.
The aim of this systematic review was to evaluate the recent evidence supporting the use of available serologic biomarkers to investigate the degree of kidney fibrosis on kidney biopsy.
2. Methods
A detailed literature search has been developed a priori to identify articles that reported findings from clinical and laboratory studies that evaluated the prognostic or diagnostic role of serological biomarkers in pathologic conditions characterized by renal fibrosis. Keywords and subject terms included: ((“renal fibrosis”[MeSH Terms]) OR (“renal”[All Fields] AND “fibrosis”[All Fields]) OR (“renal fibrosis”[All Fields]) OR (“kidney fibrosis”[MeSH terms]) OR (“kidney”[All Fields] AND “fibrosis”[All fields]) OR (“chronic kidney disease”[MeSH terms])) AND ((“serum biomarkers”[MeSH Terms]) OR (“biomarkers”[All Fields])). The search strategy was applied to Ovid MEDLINE, In-Process, and Other Non-Indexed Citation and Ovid Medline for the last five years (from May 2017 to May 2022).
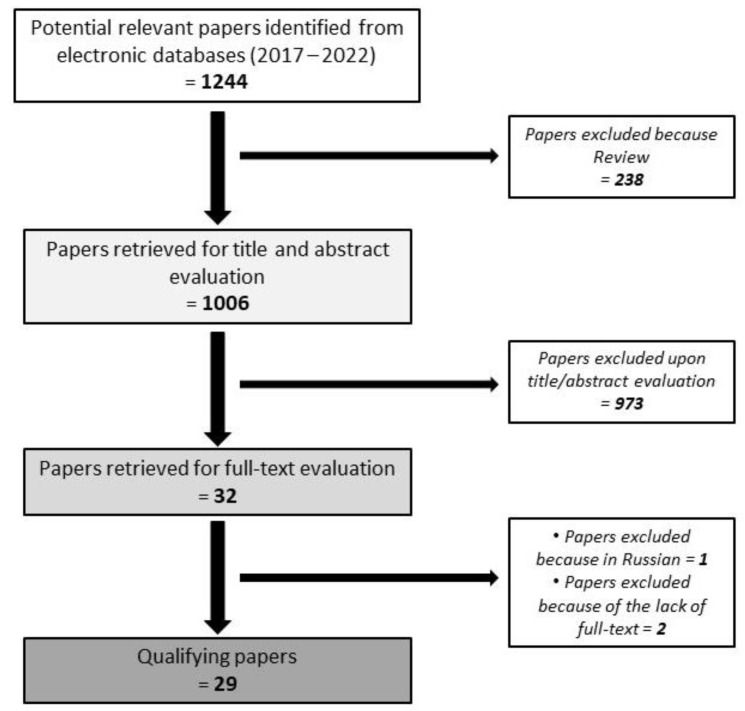
The studies identified were systematically analyzed by two independent reviewers (AB and MR). Disagreements were resolved by consensus; if consensus could not be achieved, a third party (SS) would provide an assessment of eligibility. As the data on eligibility were dichotomous (eligible: yes/no), agreement at both the title and abstract review and the full article review stages was determined by calculation of Cohen’s kappa coefficient (k = 0.92). Literature search strategy is shown in Figure 1.
Figure 1.
Literature search strategy and studies selection.
Inclusion criteria of the studies were as follow:
inclusion of at least 25 patients;
publication in the last five years;
presentation of clinical related data (not just in vitro analysis).
3. Results and Discussion
The literature search identified 29 studies that were eligible according to the inclusion criteria and they have been included in the systematic review [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51]. A detailed literature search strategy is displayed in Figure 1. Table 1 resumes the main characteristics of the included studies.
Table 1.
Summary of the main characteristics of the studies included in the systematic review.
| Ref | Authors | Year | Design | N Patients | Patients Population | Controls | Tested Biomarkers | Biomarkers Statistically Associated with Fibrosis |
|---|---|---|---|---|---|---|---|---|
| [23] | Zhang et al. | 2017 | R | 244 | IgA nephropathy | 40 HC | MMP-7 | MMP-7 |
| [24] | Stribos et al. | 2017 | R | 78 | Renal transplant recipients | NA | C3M, Pro-C3, C4M, C5M, Pro-C6, C6M | C3M, Pro-C6 |
| [25] | Akin et al. | 2017 | PR | 81 | AKI (44), CKD (37) | NA | HA | HA |
| [26] | Chen et al. | 2017 | R | 31 | CKD | 25 HC | Bcl-3 | Bcl-3 |
| [27] | Cho et al. | 2018 | R | 67 | IgA nephropathy (26), FSGS (12), MCD (7), MN (3), TBMD (3), MPGN (2), post-infectious glomerulonephritis (1), LN (1), GN (1), ATN (1), amyloidosis (1), non-specific findings (9) | NA | Klotho | Klotho |
| [28] | Luo et al. | 2018 | R | 103 | Renal transplant recipients | 127 HC | HE4 | HE4 |
| [29] | Nielsen et al. | 2018 | PR | 492 | CKD | NA | LAMC1 | LAMC1 |
| [30] | Yiang et al. | 2018 | post hoc | 230 | CKD | 67 HC | Bmi-1 | Bmi-1 |
| [31] | Zhang et al. | 2019 | R | 58 | Biopsy-proven renal fibrosis | 10 HC | miR-181 | miR-181 |
| [32] | Ren et al. | 2019 | R | 697 | DN | 150 HC | VASH-1, SIRT1, HIF1α, VEGF, CRP, TNF-α, TGF-β1 | VASH-1 |
| [33] | Ozkan et al. | 2019 | R | 131 | CKD | 34 HC | PCPE-1 | PCPE-1 |
| [34] | Basturk et al. | 2020 | R | 45 | CKD | 16 HC | PTX-2 | Pentraxin-2 (PTX-2) |
| [35] | Bieniaś et al. | 2020 | R | 45 | Unilateral hydronephrosis (children) | 21 HC | MMP-1, MMP-2, MMP-9, TIMP-1 and TIMP-2 | MMP-1, MMP-2, MMP-9, TIMP-1 and TIMP-2 |
| [36] | Ihara et al. | 2020 | PR | 1181 | Type II diabetes | NA | WFDC2, MMP-7 | WFDC2 and MMP-7 |
| [37] | Zhang et al. | 2020 | R | 202 | IgA nephropathy (43), MN (42), DN (28), hypertensive nephrosclerosis (21), MCD (16), ANCA-associated nephritis (12), minor histopathology abnormality (11), LN (8), FSGS (5), renal amyloidosis (5), cast nephropathy (5), ORG (2), TMA (2), ATN (1), uric acid nephropathy (1) | 30 HC | LOX | LOX |
| [38] | Musiał et al. | 2020 | R | 70 | Children with CKD: obstructive uropathy (23), hypo-/dysplastic kidneys (15), reflux nephropathy (14), PKD (4), other genetic disorders (5), AKI (4), and unknown factors (5) | 12 children with monosymptomatic nocturnal enuresis and normal kidney function | MCP-1, MCSF, TIMP-2, BIRC5 | MCP-1, MCSF, TIMP-2, BIRC5 |
| [39] | Schrauben et al. | 2020 | PR | 894 | DN | NA | KIM-1, TNFR-1, TNFR-2, MCP-1, suPAR, YKL-40 | KIM-1, TNFR-1, TNFR-2, MCP-1, suPAR, YKL-40 |
| [40] | Genovese et al. | 2020 | PR | 500 | CKD | NA | Pro-C3, C3M | Pro-C3, C3M |
| [41] | Jie et al. | 2021 | R | 168 | CKD | NA | UMOD | UMOD |
| [42] | Schmidt et al. | 2021 | R | 973 | CKD | snRNA-seq dataset derived from 3 healthy kidneys | CDH11, SMOC2, PEDF, MGP, TSP-2 | CDH11, SMOC2, and PEDF |
| [43] | Sun et al. | 2021 | R | 47 | CKD | 60 HC | RelB, HE4 | RelB, HE4 |
| [44] | Sparding et al. | 2021 | R | 96 | IgA nephropathy (49), ANCA-associated vasculitis (47) | 85 IgAN (validation cohort), 10 HC | ETP (Pro-C6) | ETP (Pro-C6) |
| [45] | Gutiérrez et al. | 2021 | PR | 594 | Type II diabetes | NA | TNFR1, TNFR2, suPAR, MCP-1, YKL-40, KIM-1 | TNFR1, TNFR2, YKL-40 |
| [46] | Liu et al. | 2021 | post hoc | 231 | Type II diabetes and stage 3 CKD | NA | PDGF-AA, PDGF-BB, MCD, FGF2, GMCSF, INFα2, MCP-3, IL-12p70, sCD40L, IL-2, IL-6, IL-8, MIP-1α, NGAL, cystatin C | |
| [47] | Genovese et al. | 2021 | R | 40 | LN | SLE without LN (20), HC (20), biopsy-proven histologic kidney inflammation/damage without SLE (10) | Pro-C3, Pro-C6 | Pro-C6 |
| [48] | Naicker et al. | 2021 | R | 25 | HIV-positive CKD | 25 HIV-positive without CKD, 24 HC | NGAL, cystatin C, TGF-β1, TGF-β2, TGF-β3, BMP-7 | NGAL, cystatin C, TGF-β1, TGF-β2, TGF-β3, BMP-7 |
| [49] | Enoksen et al. | 2021 | PR | 1302 | NA, general population | NA | MMP-2, MMP-7, TIMP1 | MMP-7 |
| [50] | Chan et al. | 2022 | R | 132 | Renal transplant recipients | NA | UMOD | UMOD |
| [51] | Sciascia et al. | 2022 | PR | 132 | 75 SLE, 57 SLE with LN | 50 HC | DKK-3 | DKK-3 |
(MMP-7 = matrix metalloproteinase 7; C3M = MMP-mediated degradation of collagen type III; Pro-C3 = pro-peptide of type III collagen; C4M = MMP-mediated degradation of collagen type IV; C5M = MMP-mediated degradation of collagen type V; Pro-C6 = pro-peptide of type VI collagen; C6M = MMP-mediated degradation of collagen type VI; HA = hyaluronic acid; Bcl-3 = B cell lymphoma 3; WISP-1 = WNT1-inducible signaling pathway protein-1; HE4 = human epididymis secretory protein 4; LAMC1 = laminin subunit gamma 1; Bmi-1 = polycomb complex protein BMI-1; miR-181 = microRNA-181; VASH-1 = vasohibin-1; SIRT1 = sirtuin 1; HIF1α = hypoxia-inducible factor 1α; VEGF = vascular endothelial growth factor; CRP = C-reactive Protein; TNF-α = tumor necrosis factor α; TGF-β1 = transforming growth factor β1; PCPE-1 = procollagen C-proteinase enhancer-1; PTX-2 = pentraxin-2; MMP-1 = matrix metalloproteinase 1; MMP-2 = matrix metalloproteinase 2; MMP-9 = matrix metalloproteinase 9; TIMP-1 = tissue inhibitor of matrix metallopeptidase 1; TIMP-2 = tissue inhibitor of matrix metallopeptidase 2; WFDC2 = WAP four-disulfide core domain protein 2; LOX = lysyl oxidase; MCP-1 = monocyte chemoattractant protein-1; MCSF = macrophage colony-stimulating factor; BIRC5 = surviving; KIM-1 = kidney injury molecule-1; TNF-R1 = tumor necrosis factor receptor 1; TNF-R2 = tumor necrosis factor receptor 2; suPAR = soluble urokinase plasminogen activator receptor; YKL-40 = chitinase 3-like 1; UMOD = uromodulin; CDH11 = cadherin-11; SMOC2 = sparc-related modular calcium binding protein-2; PEDF = pigment epithelium-derived factor; MGP = matrix-Gla protein; TSP2 = thrombospondin-2; RelB = transcription factor RelB; ETP = endotrophin; PDGF-AA = platelet-derived growth factor AA; PDGF-BB = platelet-derived growth factor BB; FGF-2 = fibroblast growth factor 2; MDC = macrophage-derived chemokine; GMCSF = granulocyte-macrophage colony-stimulating factor; IFNα2 = interferon α2; MCP-3 = monocyte chemoattractant protein-3; IL-12p70 = interleukin 12p70; sCD40L = soluble cluster of differentiation 40-ligand; IL-2 = interleukin 2; IL-6 = interleukin 6; IL-8 = interleukin 8; MIP-1α = macrophage inflammatory protein 1α; NGAL = neutrophil gelatinase-associated lipocalin; TGF-β2 = transforming growth factor β2; TGF-β3 = transforming growth factor β3; BMP-7 = bone morphogenetic protein 7; DKK-3 = dickkopf-related protein 3; AKI = acute kidney injury; CKD = chronic kidney disease; FSGF = focal segmental glomerulosclerosis; DN = diabetic nephropathy; MCD = minimal change disease; MN = membranous nephropathy; TBMD = thin basement membrane disease; MPGN = membranous proliferative glomerulonephritis; LN = lupus nephritis; GN = crescentic glomerulonephritis; ATN = acute tubular necrosis; ORG = obesity-related glomerulopathy; TMA = thrombotic microangiopathy; PKD = polycystic kidney disease; NA = not applicable).
When focusing on the study design, 2 out of 29 (6.9%) were post-hoc analyses, 8/29 (27.6%) were prospective, and 19/29 (65.5%) were retrospective studies.
When considering the population included in the selected studies, a total of 8889 patients were recruited. Details regarding the diagnosis of these patients are reported in Table 2.
Table 2.
Summary of patients’ diagnosis regarding the whole cohort included in the study.
| Diagnosis | Patients Number (%) |
|---|---|
| Diabetic nephropathy | 3625 (40.7) |
| CKD without specifying the underlying cause | 2675 (30.1) |
| IgA nephropathy | 362 (4.1) |
| Renal transplant recipients | 313 (3.5) |
| Lupus nephritis | 106 (1.2) |
| Systemic lupus erythematosus | 75 (0.8) |
| Generically reported as biopsy-proven renal fibrosis | 58 (0.6) |
| Acute kidney injury | 50 (0.5) |
| ANCA-associated vasculitis | 47 (0.5) |
| Unilateral hydronephrosis | 45 children (0.5) |
| Membranous nephropathy | 45 (0.5) |
| HIV-positive CKD | 25 (0.3) |
| Minimal change disease | 23 (0.25) |
| Obstructive uropathy | 23 (0.25) |
| Hypertensive nephrosclerosis | 21 (0.2) |
| Focal segmental glomerulosclerosis | 17 (0.2) |
| Hypo/dysplastic kidney | 15 (0.2) |
| Reflux nephropathy | 14 (0.15) |
| ANCA-associated nephritis | 12 (0.1) |
| Minor histopathologic abnormality | 11 (0.1) |
| Renal amyloidosis | 6 (0.05) |
| Cast nephropathy | 5 (0.05) |
| Polycystic kidney disease | 4 (0.05) |
| Thin basement membrane disease | 3 (0.03) |
| Thrombotic microangiopathy | 2 (0.02) |
| Membranous proliferative glomerulonephritis | 2 (0.02) |
| Post-infectious glomerulonephritis | 1 (0.01) |
| Crescentic glomerulonephritis | 1 (0.01) |
| Uric acid nephropathy | 1 (0.01) |
| General population (prospectively followed) | 1302 (14.6) |
Moreover, 17 studies out of 29 (58.6%) also included additional groups of subjects as controls. Most of them were healthy donors (684), while other studies included controls as subjects with renal diseases (Table 1).
A total of 65 different biomarkers were evaluated in patients’ serum to assess renal fibrosis and a statistically significant association has been found between 42 of them and/or other fibrotic biomarkers/histopathological findings (Table 1). Among these, the most frequently tested were: MCP-1 (monocyte chemoattractant protein-1) (4 studies out of 29 = 13.8%), KIM-1 (kidney injury molecule-1) (3/29 = 10.3%), MMP-7 (matrix metalloproteinase 7) (3/29 = 10.3%), Pro-C3 (pro-peptide of type III collagen) (3/29 = 10.3%), Pro-C6 (pro-peptide of type VI collagen)(3/29 = 10.3%), TNFR-1 (tumor necrosis factor receptor 1) (3/29 = 10.3%), and TNFR-2 (tumor necrosis factor receptor 2) (3/29 = 10.3%). The main findings are briefly discussed separately.
3.1. MCP-1 (Monocyte Chemoattractant Protein-1) and KIM-1 (Kidney Injury Molecule-1)
MCP-1 has been tested in 4 studies out of 29 (13.8%), while KIM-1 has been in tested in 3 out of 29 (10.3%). MCP-1 belongs to the C-C chemokine family. It is produced by many cell types, but it is mainly expressed by activated monocytes/macrophages, T cells, and natural killer cells, and plays a role in leukocyte infiltration to the kidney [52,53]. KIM-1 is a transmembrane protein of proximal tubule cells whose expression results to be strongly upregulated during tubule damage [54,55]. These two biomarkers are indeed used to evaluate tubule injury when facing patients affected by renal pathological conditions. In particular, MCP-1 seems to be useful to assess the extent of inflammation and fibrotic activity, while KIM-1 seems reliable for quantifying the severity of tubule cell injury [19,56].
3.2. MMP-7 (Matrix Metalloproteinase 7)
MMP-7, or matrilysin, has been tested in 3 studies out of 29 (10.3%). It is a secreted zinc- and calcium-dependent endopeptidase able to degrade different substrates, both of the extracellular matrix and the basement membrane [57,58]. It is indeed a downstream target gene of Wnt/β-catenin signaling and growing evidence indicates that MMP-7 seems to play an important role in the pathogenesis of kidney fibrosis and it is a useful biomarker to predict kidney disease progression [59,60].
3.3. Pro-C3 (Pro-Peptide of Type III Collagen)
Pro-C3 has been tested in 3 studies out of 29 (10.3%). Pro-C3, represents the N-terminal pro-peptide of type III procollagen that detects the formation of type III collagen which, together with collagen type I, constitutes the major component of the ECM. Excessive ECM deposition is a hallmark of fibrosis and collagen type III seems to be dominant in the early stages of this pathological process. As a result, Pro-C3 has gained interest in the last years when assessing fibrogenesis [40,61].
3.4. Pro-C6 (Pro-Peptide of Type VI Collagen)
Pro-C6 has been tested in 3 studies out of 29 (10.3%). It is produced by fibroblasts and is found at the interface between the interstitial matrix and the glomerular basement membrane in the kidney [62]. Pro-C6 has been observed to be expressed at low levels in healthy individuals and overexpressed in patients with renal fibrosis. Interistingly, its released fragment (endothropin-ETP) has been demonstrated to increase TGF-β expression, to promote EMT, chemotaxis of macrophages, adipose tissue fibrosis and metabolic dysfunction [63].
3.5. TNFR-1 (Tumor Necrosis Factor Receptor 1) and TNFR-2 (Tumor Necrosis Factor Receptor 2)
TNFR-1 and TNFR-2 have both been tested in 3 studies out of 29 (10.3%). It has been observed that by binding their ligand TNF-α, they play a role in the kidney fibrotic process. TNF-α is indeed a potent mediator of the inflammatory response produced by various cell types, including macrophages, mesangial cells, and tubular epithelial cells [64,65]. High serum levels of TNF-α have been observed in human CKD and experimental kidney disease models, and they also positively correlated with the severity of kidney injury. Besides this, in unilateral ureteral obstruction models, the inhibition of TNFR-1 has been associated with an anti-fibrotic response [66,67].
3.6. Serum Biomakers and Their Relationship with Histologic Findings at Kidney Biopsy
When analyzing the included studies more in depth, it was possible to further divide them in two sub-groups based on the availability of the comparison between serologic biomarkers and histologic findings. In detail, the first group comprises those studies in which a comparison between circulating biomarkers and the findings from kidney biopsy has been performed (14 studies out of 29 = 48.3%).
Moreover, in 8 out of 14 studies (57.1%) the grading of fibrosis was specified, while 6/14 (42.9%) did not apply any scoring system or grading of kidney fibrosis. Table 3 summarizes the studies that included kidney biopsy in the analysis and the scores used to assess the grade of fibrosis. The second group did not compare the biomarkers to histological features (15 studies out of 29 = 51.7%), but to other biomarkers that are presumed to have a role in CKD and fibrosis according to the literature.
Table 3.
Summary of the studies that included kidney biopsy in their analysis and their scores to assess the grade of fibrosis.
| Ref | Author | Year | N Patients | Biomarkers Tested | Biomarkers Statistically Associated with Fibrosis | Fibrosis Grade Assessment |
|---|---|---|---|---|---|---|
| [23] | Zhang et al. | 2017 | 244 | MMP-7 | MMP-7 | MEST-C (Oxford classification) [68] |
| [24] | Stribos et al. | 2017 | 78 | C3M, Pro-C3, C4M, C5M, Pro-C6, C6M | C3M, Pro-C6 | Not specified |
| [27] | Cho et al. | 2020 | 67 | Klotho | Klotho |
|
| [28] | Luo et al. | 2018 | 103 | HE4 | HE4 | Banff classification [69] |
| [31] | Zhang et al. | 2019 | 58 | miR-181 | miR-181 | Not specified |
| [34] | Basturk et al. | 2020 | 45 | PTX-2 | PTX-2 | Not specified |
| [37] | Zhang et al. | 2020 | 202 | LOX | LOX | Not specified |
| [42] | Schmidt et al. | 2021 | 973 | CDH11, SMOC2, PEDF, MGP, TSP2 | CDH11, SMOC2, PEDF | IFTA was graded as involvement of <10%, 11–25%, 26–50%, or >50% of total cortical volume. |
| [43] | Sun et al. | 2021 | 47 | RelB, HE4 | RelB, HE4 | Not specified |
| [44] | Sparding et al. | 2021 | 96 | ETP | ETP | MEST-C (Oxford classification) [68], Banff classification [69] |
| [47] | Genovese et al. | 2021 | 40 | Pro-C3, Pro-C6 | Pro-C6 |
|
| [48] | Naicker et al. | 2021 | 25 | NGAL, cystatin C, TGF-β1, TGF-β2, TGF-β3, BMP-7 | NGAL, cystatin C, TGF-β1, TGF-β2, TGF-β3, BMP-7 | Not specified |
| [50] | Chan et al. | 2022 | 132 | Uromodulin | Uromodulin | Areas with fibrosis were determined at 5% level for each visual field and 1% level for averaged values. There was a high degree of concordance in IF% scores between the investigators, with intra- and inter-observer variability <5% in all but three cases. |
| [51] | Sciascia et al. | 2022 | 132 | DKK-3 | DKK-3 | ISN/RPS |
(MMP-7 = matrix metalloproteinase 7; C3M = MMP-mediated degradation of collagen type III; Pro-C3 = pro-peptide of type III collagen; C4M = MMP-mediated degradation of collagen type IV; C5M = MMP-mediated degradation of collagen type V; Pro-C6 = pro-peptide of type VI collagen; C6M = MMP-mediated degradation of collagen type VI; HE4 = human epididymis secretory protein 4; miR-181 = microRNA-181; PTX-2 = pentraxin-2; LOX = lysyl oxidase; UMOD = uromodulin; CDH11 = cadherin-11; SMOC2 = sparc-related modular calcium binding protein-2; PEDF = pigment epithelium-derived factor; MGP = matrix-Gla protein; TSP2 = thrombospondin-2; RelB = transcription factor RelB; ETP = endotrophin; NGAL = neutrophil gelatinase-associated lipocalin; TGF-β2 = transforming growth factor β2; TGF-β3 = transforming growth factor β3; BMP-7 = bone morphogenetic protein 7; DKK-3 = dickkopf-related protein 3; Not specified = did not report any score or information regarding the way used to assess the grading of fibrosis).
When focusing on the first group, we observed that the following serum biomarkers were associated with fibrosis: MMP-7 (matrix metalloproteinase 7), C3M (MMP-mediated degradation of collagen type III), Pro-C6 (pro-peptide of type VI collagen), Klotho, HE4 (human epididymis secretory protein 4), miR-181 (microRNA-181), PTX-2 (pentraxin-2), LOX (lysyl oxidase), CDH11 (cadherin-11), SMOC2 (sparc-related modular calcium binding protein-2), PEDF (pigment epithelium-derived factor), RelB (transcription factor RelB), ETP (endotrophin), NGAL (neutrophil gelatinase-associated lipocalin), cystatin C, TGF-β1 (transforming growth factor β1), TGF-β2 (transforming growth factor β2), TGF-β3 (transforming growth factor β3), BMP-7 (bone morphogenetic protein 7), uromodulin, and DKK-3 (dickkopf-related protein 3). Two of them have been used in more than one study, indeed in two studies (Pro-C6 and HE4), while the others have been used in only one work. Interestingly, among those biomarkers that were found to be associated with fibrosis in the overall cohort of patients included in the present systematic review, only MMP-7 maintained this association with biopsy-proven renal fibrosis.
Renal fibrosis represents the main pathological process leading to CKD. The scarring can affect every compartment of the kidney structure, separately or in concomitance, resulting in glomerulosclerosis, tubule-interstitial fibrosis, atherosclerosis causing parenchymal damage, ultimately leading to kidney dysfunction [11,12]. Fibrosis is a complex and dynamic process, in which the crosstalk between different cell types is crucial along with multiple cellular and molecular cascade. After an initial injury, the kidney attempts to repair the damage by activating the resident cells, inducing the production of pro-inflammatory cytokines and chemokines. Consequently, infiltration of inflammatory monocytes/macrophages and T-cells is promoted, which in turn stimulate mesangial cells, fibroblasts and tubular epithelial cells to undergo a phenotypic activation or transition, leading to the production of ECM components [11,12].
A renal fibrosis targeted therapy is still in its beginnings, nevertheless this growing knowledge at cellular and molecular level holds considerable hope for the future and a few points are worth to be considered. Direct or indirect quantitative assessment of the degree of kidney fibrosis damage and progression would be extremely important to identify patients more prone to undergo a worsening of their condition and also to identify safe and effective treatments for renal fibrosis in the course of various type of CKD.
In this setting, biomarkers of fibrosis have gained an increasing importance when facing CKD, from a diagnostic to a therapeutic point of view. The relative lack of non-invasive surrogate outcome measures that specifically assess renal fibrosis in general represents one of the major barriers to clinical interventional trials. The currently used non-invasive parameters such as the eGFR, on one hand lack to fully capture all the components of kidney damage and in particular tubule damage, which has been observed to be the most reliable aspect for predicting kidney failure progression [18,19], and on the other hand, their utility can be limited by the sluggish evolution of some renal diseases. Kidney biopsy thus, still represents the gold standard for this purpose. However, it is an invasive, although overall safe, procedure that can be repeated only a limited number of times [21,22].
In this systematic review, we analyzed the available evidence on serological biomarkers associated with renal fibrosis in patients suffering from renal diseases. A study with a similar purpose has been carried out in 2017 by Mansour and colleagues, where an association between renal fibrosis and MMP-2, MCP-1 and TGF-β was reported. When analyzing the 29 included studies, in which a total of 65 biomarkers have been tested, 42 potential biomarkers were showed to have a significant positive association with fibrosis in the analysed patients. Not surprisingly, the most frequently tested molecules were known circulating biomarkers associated to the inflammatory process (e.g., MCP-1, TNFR-1 and TNFR-2), kidney damage, (e.g. KIM-1), and extracellular matrix remodeling (e.g., MMP-7, Pro-C3 and Pro-C6). However, most of these studies did not confirm their findings histologically. When focusing specifically on the sub-group of studies in which a direct comparison of serologic and histologic findings was performed, the results were very heterogenous and the only analytes that were confirmed to be significantly associated with fibrosis were MMP-7 and Pro-C6.
Some limitations must be acknowledged. First, this systematic review included data derived from studies with different design and methods, therefore limiting direct comparability. Second, the population evaluated was highly heterogeneous, showing patients affected by diverse kidney-related diseases. Further, most of the studies did not compare their results to histological findings. Nonetheless, it should also be considered that the scope of this work was to investigate the serum biomarkers most used in the last years to evaluate renal fibrosis. We acknowledge also that some arbitrary choices have been performed when implementing our a priori research strategy, such as including only literature from the last five years or limiting our analysis to studies with more than 25 patients. However, these implementations were applied to improve the novelty and comparability of the results.
4. Conclusions
To date, evidence regarding potential novel biomarkers to assess kidney fibrosis is still very scattered and none of the biomarkers are routinely employed in clinical practice. Thus, further studies are needed. Nonetheless, this systematic review highlighted how the idea of a panel combining different biomarkers, rather than the employment of a single one, could be the best path to follow. Multiple measures capable of addressing the different aspects involved in this pathological condition, such as glomerular and tubular injury and dysfunction, and inflammation could be the most suitable way to capture the high complexity characterizing renal fibrotic process, having consequently a great impact on clinical practice by maximizing prevention, diagnosis, and management.
In the near future, more specialized tools (ranging from molecular imaging to laboratory testing) will be integrated into clinical practice to assess the ongoing pathological processes within the kidneys ultimately improving disease staging and prognosis, monitoring treatment responses. Such developments will change how clinicians treat and manage patients suffering from renal fibrosis and will bring nephrology precision medicine closer.
Author Contributions
Conceptualization, A.B. and S.S.; methodology, A.B., M.R. and S.S.; investigation, A.B.; data curation, A.B., M.R., I.C., S.G.F. and E.R.; writing—original draft preparation, A.B.; writing—review and editing, M.R., I.C., S.G.F., E.R., D.R. and S.S.; supervision, D.R. and S.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data can be shared upon reasonable request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jha V., Garcia-Garcia G., Iseki K., Li Z., Naicker S., Plattner B., Saran R., Wang A.Y.-M., Yang C.-W. Chronic kidney disease: Global dimension and perspectives. Lancet. 2013;382:260–272. doi: 10.1016/S0140-6736(13)60687-X. [DOI] [PubMed] [Google Scholar]
- 2.Levey A.S., Atkins R., Coresh J., Cohen E.P., Collins A.J., Eckardt K.U., Nahas M.E., Jaber B.L., Jadoul M., Levin A., et al. Chronic kidney disease as a global public health problem: Approaches and initiatives—A position statement from Kidney Disease Improving Global Outcomes. Kidney Int. 2007;72:247–259. doi: 10.1038/sj.ki.5002343. [DOI] [PubMed] [Google Scholar]
- 3.Charles C., Ferris A.H. Chronic Kidney Disease. Prim. Care. 2020;47:585–595. doi: 10.1016/j.pop.2020.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Wang Y.N., Ma S.X., Chen Y.Y., Chen L., Liu B.L., Liu Q.Q., Zhao Y.Y. Chronic kidney disease: Biomarker diagnosis to therapeutic targets. Clin. Chim. Acta. 2019;499:54–63. doi: 10.1016/j.cca.2019.08.030. [DOI] [PubMed] [Google Scholar]
- 5.Wang V., Vilme H., Maciejewski M.L., Boulware L.E. The Economic Burden of Chronic Kidney Disease and End-Stage Renal Disease. Semin Nephrol. 2016;36:319–330. doi: 10.1016/j.semnephrol.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Lv J.C., Zhang L.X. Prevalence and Disease Burden of Chronic Kidney Disease. Adv. Exp. Med. Biol. 2019;1165:3–15. doi: 10.1007/978-981-13-8871-2_1. [DOI] [PubMed] [Google Scholar]
- 7.Bikbov B., Purcell C.A., Levey A.S., Smith M., Abdoli A., Abebe M., Adebayo O.M., Afarideh M., Agarwal S.K., Agudelo-Botero M., et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–733. doi: 10.1016/S0140-6736(20)30045-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Couser W.G., Remuzzi G., Mendis S., Tonelli M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011;80:1258–1270. doi: 10.1038/ki.2011.368. [DOI] [PubMed] [Google Scholar]
- 9.Liu M., Li X.-C., Lu L., Cao Y., Sun R.-R., Chen S., Zhang P.-Y. Cardiovascular disease and its relationship with chronic kidney disease. Eur. Rev. Med. Pharmacol. Sci. 2014;18:2918–2926. [PubMed] [Google Scholar]
- 10.Jankowski J., Floege J., Fliser D., Böhm M., Marx N. Cardiovascular Disease in Chronic Kidney Disease: Pathophysiological Insights and Therapeutic Options. Circulation. 2021;143:1157–1172. doi: 10.1161/CIRCULATIONAHA.120.050686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Panizo S., Martínez-Arias L., Alonso-Montes C., Cannata P., Martín-Carro B., Fernández-Martín J., Naves-Díaz M., Carrillo-López N., Cannata-Andía J. Fibrosis in Chronic Kidney Disease: Pathogenesis and Consequences. Int. J. Mol. Sci. 2021;22:408. doi: 10.3390/ijms22010408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nogueira A., Pires M.J., Oliveira P.A. Pathophysiological Mechanisms of Renal Fibrosis: A Review of Animal Models and Therapeutic Strategies. In Vivo. 2017;31:1. doi: 10.21873/invivo.11019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henderson N.C., Rieder F., Wynn T.A. Fibrosis: From mechanisms to medicines. Nature. 2020;587:555–566. doi: 10.1038/s41586-020-2938-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weiskirchen R., Weiskirchen S., Tacke F. Organ and tissue fibrosis: Molecular signals, cellular mechanisms and translational implications. Mol. Asp. Med. 2019;65:2–15. doi: 10.1016/j.mam.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 15.Djudjaj S., Boor P. Cellular and molecular mechanisms of kidney fibrosis. Mol. Asp. Med. 2019;65:16–36. doi: 10.1016/j.mam.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Gu Y.Y., Liu X.S., Huang X.R., Yu X.Q., Lan H.Y. TGF-β in renal fibrosis: Triumphs and challenges. Future Med. Chem. 2020;12:853–866. doi: 10.4155/fmc-2020-0005. [DOI] [PubMed] [Google Scholar]
- 17.Black L.M., Lever J.M., Agarwal A. Renal Inflammation and Fibrosis: A Double-edged Sword. J. Histochem. Cytochem. 2019;67:663–681. doi: 10.1369/0022155419852932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wong M.G., Pollock C.A. Biomarkers in kidney fibrosis: Are they useful? Kidney Int. Suppl. 2014;4:79–83. doi: 10.1038/kisup.2014.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ix J.H., Shlipak M.G. The Promise of Tubule Biomarkers in Kidney Disease: A Review. Am. J. Kidney Dis. 2021;78:719–727. doi: 10.1053/j.ajkd.2021.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bagnasco S.M., Rosenberg A.Z. Biomarkers of Chronic Renal Tubulointerstitial Injury. J. Histochem. Cytochem. 2019;67:633–641. doi: 10.1369/0022155419861092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Restrepo-Escobar M., Granda-Carvajal P.A., Jaimes F. Systematic review of the literature on reproducibility of the interpretation of renal biopsy in lupus nephritis. Lupus. 2017;26:1502–1512. doi: 10.1177/0961203317706556. [DOI] [PubMed] [Google Scholar]
- 22.Poggio E.D., McClelland R.L., Blank K.N., Hansen S., Bansal S., Bomback A.S., Canetta P.A., Khairallah P., Kiryluk K., Lecker S.H., et al. Systematic Review and Meta-Analysis of Native Kidney Biopsy Complications. Clin. J. Am. Soc. Nephrol. 2020;15:1595–1602. doi: 10.2215/CJN.04710420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang J., Ren P., Wang Y., Feng S., Wang C., Shen X., Weng C., Lang X., Chen Z., Jiang H., et al. Serum Matrix Metalloproteinase-7 Level is Associated with Fibrosis and Renal Survival in Patients with IgA Nephropathy. Kidney Blood Press Res. 2017;42:541–552. doi: 10.1159/000477132. [DOI] [PubMed] [Google Scholar]
- 24.Stribos E.G.D., Nielsen S.H., Brix S., Karsdal M.A., Seelen M.A., Van Goor H., Bakker S.J.L., Olinga P., Mutsaers H.A.M., Genovese F. Non-invasive quantification of collagen turnover in renal transplant recipients. PLoS ONE. 2017;12:e0175898. doi: 10.1371/journal.pone.0175898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Akin D., Ozmen S., Yilmaz M.E. Hyaluronic Acid as a New Biomarker to Differentiate Acute Kidney Injury from Chronic Kidney Disease. Iran. J. Kidney Dis. 2017;11:409–413. [PubMed] [Google Scholar]
- 26.Chen R., Wang L., Liu S., Chen X., Hu Y., Liu H., Zhang H., Jiang Y., Wang Q., Ye D., et al. Bcl-3 is a novel biomarker of renal fibrosis in chronic kidney disease. Oncotarget. 2017;8:97206–97216. doi: 10.18632/oncotarget.21692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cho N.J., Han D.J., Lee J.H., Jang S.H., Kang J.S., Gil H.W., Park S., Lee E.Y. Soluble klotho as a marker of renal fibrosis and podocyte injuries in human kidneys. PLoS ONE. 2018;13:e0194617. doi: 10.1371/journal.pone.0194617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luo J., Wang F., Wan J., Ye Z., Huang C., Cai Y., Liu M., Wu B.Q., Li L. Serum human epididymis secretory protein 4 as a potential biomarker of renal fibrosis in kidney transplantation recipients. Clin. Chim. Acta. 2018;483:216–221. doi: 10.1016/j.cca.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 29.Holm Nielsen S., Guldager Kring Rasmussen D., Brix S., Fenton A., Jesky M., Ferro C.J., Karsdal M., Genovese F., Cockwell P. A novel biomarker of laminin turnover is associated with disease progression and mortality in chronic kidney disease. PLoS ONE. 2018;13:e0204239. doi: 10.1371/journal.pone.0204239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang X., Bai M., Ning X., Ma F., Liu L., Liu T., Liu M., Wang H., Sun S. The associations of Bmi-1 with progression of glomerular chronic kidney disease. Clin. Nephrol. 2018;89:93–103. doi: 10.5414/CN109117. [DOI] [PubMed] [Google Scholar]
- 31.Zhang X., Yang Z., Heng Y., Miao C. MicroRNA-181 exerts an inhibitory role during renal fibrosis by targeting early growth response factor-1 and attenuating the expression of profibrotic markers. Mol. Med. Rep. 2019;19:3305–3313. doi: 10.3892/mmr.2019.9964. [DOI] [PubMed] [Google Scholar]
- 32.Ren H., Shao Y., Ma X., Yang M., Liu Y., Wang Q. Expression levels of serum vasohibin-1 and other biomarkers in type 2 diabetes mellitus patients with different urinary albumin to creatinine ratios. J. Diabetes Complicat. 2019;33:477–484. doi: 10.1016/j.jdiacomp.2019.04.008. [DOI] [PubMed] [Google Scholar]
- 33.Özkan G., Güzel S., Atar R.V., Fidan Ç., Kara S.P., Ulusoy Ş. Elevated serum levels of procollagen C-proteinase enhancer-1 in patients with chronic kidney disease is associated with a declining glomerular filtration rate. Nephrology. 2019;24:938–942. doi: 10.1111/nep.13521. [DOI] [PubMed] [Google Scholar]
- 34.Basturk T., Ojalvo D., Mazi E.E., Hasbal N.B., Ozagari A.A., Ahbap E., Sakaci T., Koc Y., Sevinc M., Unsal A. Pentraxin-2 is Associated with Renal Fibrosis in Patients Undergoing Renal Biopsy. Clinics. 2020;75:1–5. doi: 10.6061/clinics/2020/e1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bieniaś B., Sikora P. Selected Metal Matrix Metalloproteinases and Tissue Inhibitors of Metalloproteinases as Potential Biomarkers for Tubulointerstitial Fibrosis in Children with Unilateral Hydronephrosis. Dis. Markers. 2020;2020:9520309. doi: 10.1155/2020/9520309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ihara K., Skupien J., Kobayashi H., Md Dom Z.I., Wilson J.M., O’neil K., Badger H.S., Bowsman L.M., Satake E., Breyer M.D., et al. Profibrotic Circulating Proteins and Risk of Early Progressive Renal Decline in Patients With Type 2 Diabetes with and Without Albuminuria. Diabetes Care. 2020;43:2760–2767. doi: 10.2337/dc20-0630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang X.-Q., Li X., Zhou W.-Q., Liu X., Huang J.-L., Zhang Y.-Y., Lindholm B., Yu C. Serum Lysyl Oxidase Is a Potential Diagnostic Biomarker for Kidney Fibrosis. Am. J. Nephrol. 2020;51:907–918. doi: 10.1159/000509381. [DOI] [PubMed] [Google Scholar]
- 38.Musiał K., Zwolińska D. Monocyte chemoattractant protein-1, macrophage colony stimulating factor, survivin, and tissue inhibitor of matrix metalloproteinases-2 in analysis of damage and repair related to pediatric chronic kidney injury. Adv. Clin. Exp. Med. 2020;29:1083–1090. doi: 10.17219/acem/123350. [DOI] [PubMed] [Google Scholar]
- 39.Schrauben S.J., Shou H., Zhang X., Anderson A.H., Bonventre J.V., Chen J., Coca S., Furth S.L., Greenberg J.H., Gutierrez O.M., et al. Association of Multiple Plasma Biomarker Concentrations with Progression of Prevalent Diabetic Kidney Disease: Findings from the Chronic Renal Insufficiency Cohort (CRIC) Study. J. Am. Soc. Nephrol. 2021;32:115–126. doi: 10.1681/ASN.2020040487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Genovese F., Rasmussen D.G.K., Karsdal M.A., Jesky M., Fenton A., Cockwell P. Imbalanced turnover of collagen type III is associated with disease progression and mortality in high-risk chronic kidney disease patients. Clin. Kidney J. 2020;14:593–601. doi: 10.1093/ckj/sfz174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xie C., Yi-Ying Y., Miao C. Correlation of serum uromodulin levels with renal fibrosis and renal function progression in patients with CKD. Pak. J. Pharm. Sci. 2021;34:2417–2422. [PubMed] [Google Scholar]
- 42.Schmidt I.M., Colona M.R., Kestenbaum B.R., Alexopoulos L.G., Palsson R., Srivastava A., Liu J., Stillman I.E., Rennke H.G., Vaidya V.S., et al. Cadherin-11, Sparc-related modular calcium binding protein-2, and Pigment epithelium-derived factor are promising non-invasive biomarkers of kidney fibrosis. Kidney Int. 2021;100:672–683. doi: 10.1016/j.kint.2021.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sun D., Xie N., Wang X., Wu W., Li X., Chen X., Qian G., Li C., Zhang H., Jiang Y., et al. Serum RelB is correlated with renal fibrosis and predicts chronic kidney disease progression. Clin. Transl. Med. 2021;11:e362. doi: 10.1002/ctm2.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sparding N., Genovese F., Rasmussen D.G.K., Karsdal M.A., Neprasova M., Maixnerova D., Satrapova V., Frausova D., Hornum M., Bartonova L., et al. Endotrophin, a collagen type VI-derived matrikine, reflects the degree of renal fibrosis in patients with IgA nephropathy and in patients with ANCA-associated vasculitis. Nephrol. Dial. Transplant. 2022;37:1099–1108. doi: 10.1093/ndt/gfab163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gutiérrez O.M., Shlipak M.G., Katz R., Waikar S.S., Greenberg J.H., Schrauben S.J., Coca S., Parikh C.R., Vasan R.S., Feldman H.I., et al. Associations of Plasma Biomarkers of Inflammation, Fibrosis, and Kidney Tubular Injury With Progression of Diabetic Kidney Disease: A Cohort Study. Am. J. Kidney Dis. 2022;79:849–857.e1. doi: 10.1053/j.ajkd.2021.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu H., Sridhar V.S., Lovblom L.E., Lytvyn Y., Burger D., Burns K., Brinc D., Lawler P.R., Cherney D.Z. Markers of Kidney Injury, Inflammation, and Fibrosis Associated With Ertugliflozin in Patients With CKD and Diabetes. Kidney Int Rep. 2021;6:2095–2104. doi: 10.1016/j.ekir.2021.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Genovese F., Akhgar A., Lim S.S., Farris A.B., Battle M., Cobb J., Sinibaldi D., Karsdal M., White W.I. Collagen Type III and VI Remodeling Biomarkers Are Associated with Kidney Fibrosis in Lupus Nephritis. Kidney360. 2021;2:1473–1481. doi: 10.34067/KID.0001132021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Naicker S., Dix-Peek T., Klar R.M., Kalunga G., Mosiane P., Dickens C., Duarte R. Profiling Biomarkers in HIV Glomerular Disease—Potential for the Non-Invasive Diagnosis of HIVAN? Int. J. Nephrol. Renovasc. Dis. 2021;14:427–440. doi: 10.2147/IJNRD.S331484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Enoksen I.T., Svistounov D., Norvik J.V., Stefansson V.T., Solbu M.D., Eriksen B.O., Melsom T. Serum Matrix Metalloproteinase 7 and accelerated GFR decline in a general non-diabetic population. Nephrol. Dial. Transplant. 2021;37:1657–1667. doi: 10.1093/ndt/gfab251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chan J., Svensson M., Tannæs T.M., Waldum-Grevbo B., Jenssen T., Eide I.A. Associations of Serum Uromodulin and Urinary Epidermal Growth Factor with Measured Glomerular Filtration Rate and Interstitial Fibrosis in Kidney Transplantation. Am. J. Nephrol. 2022;53:108–117. doi: 10.1159/000521757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sciascia S., Barinotti A., Radin M., Cecchi I., Menegatti E., Terzolo E., Rossi D., Baldovino S., Fenoglio R., Roccatello D. Dickkopf Homolog 3 (DKK3) as a Prognostic Marker in Lupus Nephritis: A Prospective Monocentric Experience. J. Clin. Med. 2022;11:2977. doi: 10.3390/jcm11112977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Singh S., Anshita D., Ravichandiran V. MCP-1: Function, regulation, and involvement in disease. Int. Immunopharmacol. 2021;101 Pt B:107598. doi: 10.1016/j.intimp.2021.107598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Deshmane S.L., Kremlev S., Amini S., Sawaya B.E. Monocyte chemoattractant protein-1 (MCP-1): An overview. J Interferon Cytokine Res. 2009;29:313–325. doi: 10.1089/jir.2008.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Karmakova T.A., Sergeeva N.S., Kanukoev K.Y., Alekseev B.Y., Kaprin A.D. Kidney Injury Molecule 1 (KIM-1): A Multifunctional Glycoprotein and Biological Marker (Review) Sovrem Tekhnologii V Meditsine. 2021;13:64–80. doi: 10.17691/stm2021.13.3.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Han W.K., Bailly V., Abichandani R., Thadhani R., Bonventre J.V. Kidney Injury Molecule-1 (KIM-1): A novel biomarker for human renal proximal tubule injury. Kidney Int. 2002;62:237–244. doi: 10.1046/j.1523-1755.2002.00433.x. [DOI] [PubMed] [Google Scholar]
- 56.Siddiqui K., Joy S.S., Al-Rubeaan K. Association of urinary monocyte chemoattractant protein-1 (MCP-1) and kidney injury molecule-1 (KIM-1) with risk factors of diabetic kidney disease in type 2 diabetes patients. Int. Urol. Nephrol. 2019;51:1379–1386. doi: 10.1007/s11255-019-02201-6. [DOI] [PubMed] [Google Scholar]
- 57.Hu Q., Lan J., Liang W., Chen Y., Chen B., Liu Z., Xiong Y., Zhong Z., Wang Y., Ye Q. MMP7 damages the integrity of the renal tubule epithelium by activating MMP2/9 during ischemia–reperfusion injury. J. Mol. Histol. 2020;51:685–700. doi: 10.1007/s10735-020-09914-4. [DOI] [PubMed] [Google Scholar]
- 58.Stene C., Polistena A., Gaber A., Nodin B., Ottochian B., Adawi D., Avenia N., Jirström K., Johnson L.B. MMP7 Modulation by Short- and Long-term Radiotherapy in Patients with Rectal Cancer. In Vivo. 2018;32:133–138. doi: 10.21873/invivo.11215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhou D., Tian Y., Sun L., Zhou L., Xiao L., Tan R.J., Tian J., Fu H., Hou F.F., Liu Y. Matrix Metalloproteinase-7 Is a Urinary Biomarker and Pathogenic Mediator of Kidney Fibrosis. J. Am. Soc. Nephrol. 2017;28:598–611. doi: 10.1681/ASN.2016030354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ke B., Fan C., Yang L., Fang X. Matrix Metalloproteinases-7 and Kidney Fibrosis. Front. Physiol. 2017;8:21. doi: 10.3389/fphys.2017.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nielsen M.J., Nedergaard A.F., Sun S., Veidal S.S., Larsen L., Zheng Q., Suetta C., Henriksen K., Christiansen C., Karsdal M.A., et al. The neo-epitope specific PRO-C3 ELISA measures true formation of type III collagen associated with liver and muscle parameters. Am. J. Transl. Res. 2013;5:303–315. [PMC free article] [PubMed] [Google Scholar]
- 62.Cescon M., Gattazzo F., Chen P., Bonaldo P. Collagen VI at a glance. J. Cell Sci. 2015;128:3525–3531. doi: 10.1242/jcs.169748. [DOI] [PubMed] [Google Scholar]
- 63.Fenton A., Jesky M.D., Ferro C.J., Sørensen J., Karsdal M.A., Cockwell P., Genovese F. Serum endotrophin, a type VI collagen cleavage product, is associated with increased mortality in chronic kidney disease. PLoS ONE. 2017;12:e0175200. doi: 10.1371/journal.pone.0175200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Al-Lamki R.S., Mayadas T.N. TNF receptors: Signaling pathways and contribution to renal dysfunction. Kidney Int. 2015;87:281–296. doi: 10.1038/ki.2014.285. [DOI] [PubMed] [Google Scholar]
- 65.Meldrum K.K., Misseri R., Metcalfe P., Dinarello C.A., Hile K.L., Meldrum D.R. TNF-alpha neutralization ameliorates obstruction-induced renal fibrosis and dysfunction. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007;292:R1456–R1464. doi: 10.1152/ajpregu.00620.2005. [DOI] [PubMed] [Google Scholar]
- 66.Taguchi S., Azushima K., Yamaji T., Urate S., Suzuki T., Abe E., Tanaka S., Tsukamoto S., Kamimura D., Kinguchi S., et al. Effects of tumor necrosis factor-α inhibition on kidney fibrosis and inflammation in a mouse model of aristolochic acid nephropathy. Sci. Rep. 2021;11:23587. doi: 10.1038/s41598-021-02864-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gupta J., Mitra N., Kanetsky P.A., Devaney J., Wing M.R., Reilly M., Shah V.O., Balakrishnan V.S., Guzman N.J., Girndt M., et al. Association between albuminuria, kidney function, and inflammatory biomarker profile in CKD in CRIC. Clin. J. Am. Soc. Nephrol. 2012;7:1938–1946. doi: 10.2215/CJN.03500412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.A Working Group of the International IgA Nephropathy Network and the Renal Pathology Society. Cattran D.C., Coppo R., Cook H.T., Feehally J., Roberts I.S., Troyanov S., Alpers C.E., Amore A., Barratt J., et al. The Oxford classification of IgA nephropathy: Rationale, clinicopathological correlations, and classification. Kidney Int. 2009;76:534–545. doi: 10.1038/ki.2009.243. [DOI] [PubMed] [Google Scholar]
- 69.Loupy A., Mengel M., Haas M. Thirty years of the International Banff Classification for Allograft Pathology: The past, present, and future of kidney transplant diagnostics. Kidney Int. 2022;101:678–691. doi: 10.1016/j.kint.2021.11.028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data can be shared upon reasonable request to the corresponding author.