Abstract
Herbal medicine and nutritional supplements are suggested to treat premenstrual somatic and psycho-behavioural symptoms in clinical guidelines; nonetheless, this is at present based on poor-quality trial evidence. Hence, we aimed to design a systematic review and meta-analysis for their effectiveness in alleviating premenstrual symptoms. The published randomized controlled trials (RCTs) were extracted from Google scholar, PubMed, Scopus and PROSPERO databases. The risk of bias in randomized trials was assessed by Cochrane risk-of-bias tool. The main outcome parameters were analysed separately based on the Premenstrual Symptom Screening Tool and PMTS and DRSP scores. Secondary parameters of somatic, psychological, and behavioural subscale symptoms of PSST were also analysed. Data synthesis was performed assuming a random-effects model, and standardized mean difference (SMDs) was analysed using SPSS version 28.0.0 (IBM, Armonk, NY, USA). A total of 754 articles were screened, and 15 RCTs were included (n = 1211 patients). Primary results for participants randomized to an intervention reported reduced PSST (n = 9), PMTS (n = 2), and DSR (n = 4) scores with (SMD = −1.44; 95% CI: −1.72 to −1.17), (SMD = −1.69; 95% CI: −3.80 to 0.42) and (SMD = 2.86; 95% CI: 1.02 to 4.69) verses comparator with substantial heterogeneity. Physical (SMD = −1.61; 95% CI = −2.56 to −0.66), behavioural (SMD = −0.60; 95% CI = −1.55 to 0.35) and mood (SMD = 0.57; 95% CI = −0.96 to 2.11) subscale symptom groupings of PSST displayed similar findings. Fifty-three studies (n = 8) were considered at low risk of bias with high quality. Mild adverse events were reported by four RCTs. Based on the existing evidence, herbal medicine and nutritional supplements may be effective and safe for PMS.
Keywords: dietary supplements, female health, herbal medicine, PMS, PRISMA, reproductive health, unani medicine, Web of Science, software
1. Introduction
Premenstrual somatic and psycho-behavioural symptoms are categorized by a cyclic pattern that is obvious within the luteal phase [1], and they significantly affect quality of life with more frequent visits to hospitals parenting problems, decreased work productivity, and impaired individual and societal relationships [2,3,4]. It is a common and recurrent gynaecological problem [1], and 20–30% of reproductive-age women experience clinically significant premenstrual syndrome (PMS) symptoms [5]. The main psychological range of PMS symptoms includes anxiety and depression [3,6].
The aetiology of PMS is unclear; hence, definitive treatment is not available. However, several possible treatments have been established based on symptomatic relief [1,6]. Despite a rational success rate of pharmacotherapies (GnRH agonists OCP, selective serotonin reuptake inhibitors benzodiazepines) and non-pharmacological management (aerobic exercise, cognitive behavioural therapy, reduction in caffeine intake, education, and increased calcium and carbohydrate intake) for PMS, these therapies have considerable side effects [5,7,8]. Women may also prefer and are inclined towards complementary and alternative treatment/therapies (CAMS), including nutritional supplements and herbal medicines over medical or surgical treatment [9,10,11]. Various Unani medicinal plants [12] have been expected to lessen PMS symptoms, as they are beneficial natural substitutes [6]. RCTs on Unani medicinal plants such as Crocus sativus Linn (saffron/zafran), Borage officinalis Linn (borage/gouzaban), Vitex agnus castus Linn (chaste berry/shambalu), Matricaria chamomilla Linn (chamomile/baboona), Zingiber officinale Roscoe (ginger/zanjabeel), Foeniuclum vulgare Mill (fennel/saunf), and Pimpinella anisum Linn (anise seed/anisoon) were investigated for PMS symptoms [13]. These herbs and nutritional supplements are proven to have anti-depressant, anti-anxiety, sedative, SSRIs inhibitor and GABA A receptor effects together with antioxidant, anti-inflammatory and analgesic properties [14].
Earlier, systematic reviews were conducted on PMS including herbal medicine and acupuncture [15], including M. chamomilla [6], and V. agnus castus [16]. Canning et al. [17] explored herbs and dietary supplements for PMS. Pearce et al. (2020) conducted a systematic review and meta-analysis on exercises for PMS. Research [18] explored the efficacy of Rosa damascena Mill (rose/gul surkh) on anxiety and other symptoms. Csupor et al. [19], for the management of PMS, compared the efficacy of BNO 1095 and Ze 440 to placebo. The researchers systematically reviewed and included 18 RCTs of Iranian herbal medicines and their effectiveness and safety for PMS [20]. Tu et al. [21] suggested that communication with parents and education probably reduce parental stress and anxiety. However, a current update on the systematic review and meta-analysis of RCTs on herbs and nutritional supplements lessening premenstrual somatic and psycho-behavioural symptoms as per the modified Cochrane risk-assessment tool was not accessible as per our information. Therefore, we explored RCTs for systematic review, meta-analysis and risk of bias assessment as per the modified Cochrane risk assessment tool to provide objective data for the efficacy and safety of herbs and nutritional supplements in relieving premenstrual somatic and its psycho-behavioural symptoms. Additionally, we summarized plant metabolites and their mechanism of action in selected RCTs.
1.1. Study Aim and Research Question
This research is proposed to determine the safety and efficacy of herbs and nutritional supplements on premenstrual somatic and psycho-behavioural symptoms. An up-to-date systematic review and meta-analysis of RCTs that compare herbal medicine and nutritional supplements to placebo/conventional medical treatment were conducted. We examined the effect of herbal medicine/nutritional supplements on overall premenstrual symptoms, as well as the three symptoms’ domains: somatic, psychological and behavioural.
Hence, this paper explains the following research questions (RQs):
-
(i)
What is the role of a systematic review with risk assessment on PMS?
-
(ii)
How to design the meta-analysis of RCTs based on high-quality studies related to PMS with herbal medicine and nutritional supplements?
-
(iii)
What is the comprehensive presentation of the mechanism of action in plant metabolites and bioactive molecules?
-
(iv)
How to design a database based on network visualization, world cloud, and previously published articles?
-
(v)
What is the main research gap and what is the future in the area of PMS regarding herbal medicine and nutritional supplements?
1.2. Main Contributions of This Study
Our key contributions here are:
-
(i)
To design an up-to-date systematic review and meta-analysis of RCTs to determine the efficacy and safety of herbal medicines and nutritional supplements with their mechanism of action on premenstrual somatic and psycho-behavioural symptoms.
-
(ii)
To determine the risk of bias in randomized controlled trials.
-
(iii)
To design a database such as the number of authors, university/institution, research area-wise and country-wise on previously published publications.
-
(iv)
To design a comprehensive picture based on previous studies and present a study using network visualization and word cloud.
-
(v)
To explore the research breaches and prospects.
1.3. Paper Structure
This study is organized as follows: a systematic review, risk of bias assessment and meta-analysis using PRISMA with Consort statement [22], world clouds [23], network visualization based on keywords, discussion including major findings, comparison with previous literature, mechanism of action, strength, research gap, implication of research in clinical practices, and conclusions.
2. Methods
A complete method was thoroughly organized with the collection of data and steps of analysis, including PRISMA guidelines for RCTs [22,23,24,25,26] per the checklist [27]. The protocol was registered at PROSPERO, University of New York (CRD42022344752, dated 17 July 2022).
The following steps were performed in the methods: (a) planning and developing a protocol, (b) registry of the protocol in PROSPERO as per PRISMA-P for the protocol [28] and PRISMA checklist for publication, (c) performed a complete literature search for information source and search strategies, (d) data extraction (selection, data management and collection process), (e) outcomes, (f) risk bias and quality assessment as per the Cochrane risk assessment guidelines, (g) strategy for data analyses and measures of effect, (h) analysis of subgroups or subsets, and (i) reporting results [28,29,30].
2.1. Eligibility Criteria, Study Selection, and Participants
The articles were selected for eligibility in two steps. After a thorough review to avoid bias, two researchers independently analysed the data, which were extracted from the screened articles, and the data were organized. In the first step, the articles were screened based on keywords, titles and abstracts. Published and unpublished RCTs from indexed journals with considerable reliability were included. The duplicate publications were deleted. The inclusion criteria were participants of reproductive age reporting regular menstrual cycle (21–35 days) with premenstrual somatic and psycho-behavioural symptoms diagnosed by DSM, DSRP, ACOG or other diagnostic scales using either herbal medicine and/or nutritional supplements in RCTs. At least two cycles of intervention were given per oral. As for the control interventions, a patient who did not receive any treatment as a placebo control, or those who accepted simple Western medicine as a control intervention were included. Furthermore, clinical trials where at least 8 weeks of intervention were administered were included. Full-text access to English language articles was included to validate the description of an article more specifically. There was no limitation to whether they study was published or not. Additionally, there were no restrictions on citizenship, nationality, region, and source of cases. Patients with severe systemic diseases, known psychiatric patients, pregnancy or lactation were excluded. We also excluded other routes of administration of the medicine. The experiments were limited to humans. Non-RCTs, quasi-RCTs, series of case reports, conference papers, posters, editorials, and unreliable data were excluded. In addition, the botanical name of the plants was verified and spelled according to the source World Flora Online (http://www.worldfloraonline.org, accessed on 9 October 2022).
2.2. Information Data Source and Search Strategies
We explored online databases (Google Scholar, PubMed, Scopus, and PROSPERO) to collect data from 2008 to 2022, focusing on randomized controlled trials on premenstrual somatic and psycho-behavioural symptoms among women. The MeSH keywords, title and abstract explored for the literature search were: “Premenstrual Dysphoric Disorders”, “Premenstrual Syndrome”, “Nutritional supplements and premenstrual syndrome”, “Herbal medicine and premenstrual syndrome”, and “psycho-behavioural and premenstrual syndrome”. Rayyan online software (https://www.rayyan.ai, accessed on 3 August 2022) was used to identify duplication, randomized controlled trials and exclusion from the publication.
2.3. Data Extraction
To determine eligibility and relevance, we explored the titles, abstracts, and keywords of all articles to be included in this paper. Then, a systematic examination of the full articles was performed. The final decisions on inclusion were made, and articles were selected from 2008 to 2022. Four researchers independently analysed and extracted the data. For any disagreement, a fifth researcher reviewed the data for the confirmation. The PRISMA and Consort Statement for the randomized controlled trial checklist was referred for assessment. Detailed records regarding authors, sample size, participants, research design, tools for data collection, randomization allocation, blinding, intervention type, duration of intervention, outcome, and adverse effects were documented. Extraneous studies and inadequate quantitative data were excluded. Studies that provided post-treatment data were estimated as per meta-analysis guidelines.
2.4. Outcomes
The main outcome parameters were analysed separately based on premenstrual symptom screening tool (PSST), premenstrual tension score (PMTS) and daily severity reporting of symptom overall scores. Secondary parameters of somatic, psychological, and behavioural subscale symptoms of PSST were also analysed. Adverse events/side effects/withdrawals for adverse effects were also reviewed. Additional outcomes were adverse events and cure rate.
2.5. Risk of Bias (RoB) and Quality Assessment (QA)
Any inconsistency in the data was fixed by agreement. We evaluated the methodological quality using a modified Cochrane Risk of Bias tool for RCTs. Bias was measured based on “high, low, or unclear for individual elements from five domains, i.e., selection, reporting, performance, detection and attrition bias”.
2.6. Statistical Methods
Statistical methods were performed for the strategy of data synthesis, the measure of effect, meta-bias (es) and confidence in cumulative evidence. Assuming that the true effect sizes differed between studies as a result of study-related characteristics, the average weighted effect sizes were estimated using a random-effects model (REM). Standardized mean difference (SMD) and 95% confidence interval (CI) were used to summarize continuous outcomes. The effect size was determined by dividing the mean pre-post value difference by the SD into the experimental and control groups. To determine whether the variance between studies was greater than the variance within studies, a Q test statistic (chi-square distributed) was computed. The Q test and I2 statistics were used to evaluate heterogeneity. I2 values of 25%, 50%, and 75% were regarded as mild, moderate, and high, heterogeneity, respectively. Studies with continuous outcomes that required standard deviations not reported were disqualified from the meta-analysis. Due to the absence of pre–post correlation values from the included trials, the post-treatment SMD effect size was utilised. To account for limited sample sizes, Hedges g effect sizes were utilised together with their respective 95% CIs and were interpreted per suggestions. We performed separate meta-analyses for the subdomain group, and we reviewed the secondary/additional outcomes such as adverse effects. Egger’s test and funnel plots were performed to consider publication bias. To determine whether the pooled estimates were consistent, a sensitivity analysis was performed. If the level of heterogeneity was considerable, a meta-regression was attempted. The data were analysed by Review Manager Software (5.4.1 version; The Cochrane Collaboration, Oxford, UK).
3. Results
3.1. Literature Review of the Randomized Controlled Trials Based on PRISMA Guideline
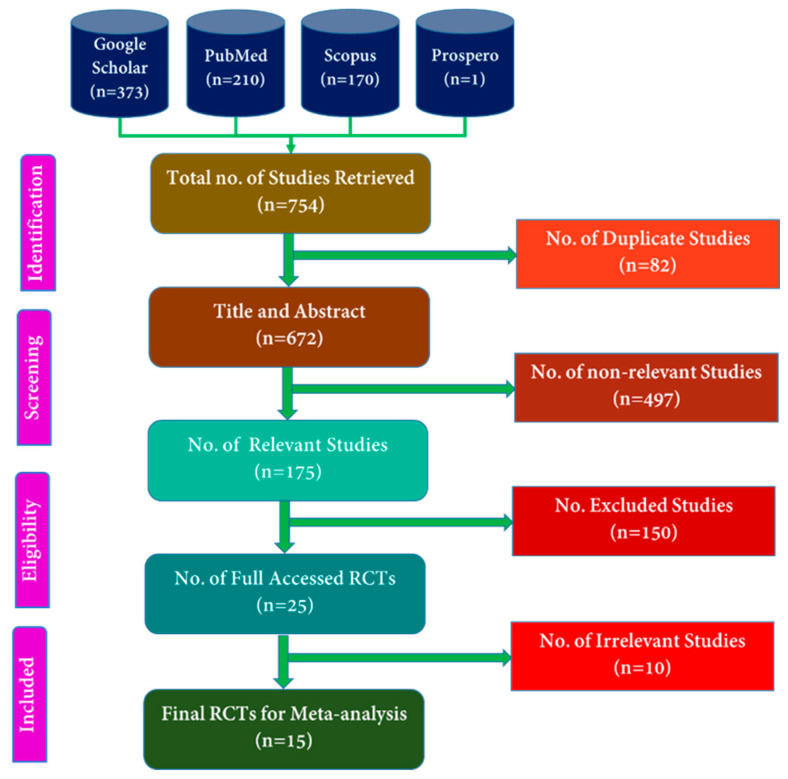
The online search retrieved 754 titles and abstracts of which 82 were duplicates (Figure 1) by using Rayyan online software (https://www.rayyan.ai, accessed on 3 August 2022).
Figure 1.
PRISMA flow chart of included publications.
Among the 672 articles, 175 articles were related to PMS, and 497 others were irrelevant. Then, 175 related articles were screened, and 25 full-length RCTs were assessed for eligibility, which were further reviewed for the extraction phase in which 15 full-length RCTs were included for systematic review and meta-analyses that met our inclusion.
We excluded the following RCTs from the meta-analysis as reasoned: Arabnezhad et al. (2022) [1] included a PSST study only before the intervention. Maskani et al. (2020) [31] and Ozgoli (2011) [32] were written in Persian Language, and the data for symptoms were presented as percentages and number. Zamani et al. (2012) [33] used a VAS score for the symptoms, and only a few symptoms were included. Retallick-Brown et al. (2020) [34] in their study on vitamin B6 and micronutrients for PMS used the DSRP tool, and the data were presented in a graph, as well as effect size estimate and 95% confidence intervals. Jafari et al. (2020) [35], in their study on zinc supplements in physical and psychological symptoms before intervention, used the DSM-VI scale; however, pre and post-intervention data for BDNF, serum zinc, hs-CRP, TAC and the average score for physical and psychological factors were calculated. Winther et al. (2018) [36], in their study, only imputed data of VAS score on irritability as a predominant PMS symptom. Delaram et al. (2011) [37], in their study on fennel in PMS, included the daily record of severity of the problem questionnaire (DRSP-Q). Canning et al. (2010) [17], in their study, included total daily symptom report scores as the primary outcome; however, the data were presented as graphs for DSRP. Gerhardsen et al. (2008) [38] studied that women with PMS and included a premenstrual sleep disturbance scale. Agha-Hosseini et al. (2008) [39] investigated Crocus sativus L. in PMS and premenstrual daily symptoms (DPS) and the Hamilton depression rating scale (HAMS); however, the data were presented in graphs. Bahrami et al. (2020) [40], in their study on curcumin in PMS, used a premenstrual symptoms scale; however, full length was not available. Esmailpour’s (2019) [41] study used a daily symptoms diary; however, post-intervention data were imputed for nutritional supplements. Ghanbari (2009) [42] studied individual symptoms, and mean and standard deviation were imputed, and a total score was not available.
3.2. Characteristics of the Included RCT Studies and Patients
A total of 15 RCTs with 1211 patients, (n = 605 and n = 606 in intervention and control groups, respectively) with mean ± SD of 80.73 ± 20.39 and CI of 69.44: 92.0 were included in this meta-analysis. Among fifteen studies on PMS, nine studies used PSST scores, two studies PMTS, and the remaining four studies used DSM scoring. Additionally, we carried out PSST scores subgroup analysis for each domain including physical, mood and behavioural symptoms. We found three RCTs on nutritional supplements and twelve RCTs on herbal medicines.
PRISMA methods only covered the given keywords in the Google Scholar, PubMed, Prospero, and Scopus databases for RCT studies. The features of previously published papers included were author name, study design, intervention group, control group, the total number of participants, participants in intervention, control participants, age limit in years, tools, route of administration, duration of intervention, results and side effects/adverse effects of nutritional supplements and herbal medicine, as summarized in Table 1. The age considered was reproductive age. The route of administration included in this study was oral.
Table 1.
The features of the published RCTs on nutritional supplements and herbal medicines.
| Authors | Study Design | Interven. | Control | Part. | Age (y) |
Tools | Route of Admin., Durat. and Dosage | Durat. of Interven. (Cycles) | Result | Adv. Event | Ref. |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ozgoli et al. (2009) | Single blind | Gingko biloba L. tablet | Placebo | 90 | 18–30 | PSST | One tablet (containing 40 mg leaf extracts) three times per day from the 16th day of the menstrual cycle to the 5th day of the next cycle | 2 | Severity of symptoms reduced significantly | Reported (Nausea and excessive sleep in intervention group) | [7] |
| Abdollahifard et al. (2014) | Double Blind |
B1 (Thiamine) | Placebo (Starch powder) | 80 | 18–30 | DSR | Two pills of Vit B1 (each pill contains 100 mg) twice daily | 3 | Reduces mental and physical symptoms | Reported (No side effects) |
[43] |
| Sharifi et al. (2014) | Double blind |
M. chamomile extract |
Mefenamic acid 250 mg TID | 90 | 18–35 | DSR | 100 mg capsules thrice daily from the 21st day until the next onset of menstruation period, three times daily for two cycles | 2 | Chamomile is more effective in relieving symptoms | Reported (Excessive bleeding in intervention group and GI complication in MA group) | [44] |
| Khayat et al. (2014) | Double blind | Z. officinale capsules | Placebo | 70 | 18–35 | PSST | Two capsules 250 mg/12 h (7 days) before menstruation to three days after menstruation | 3 | Reduction in mood, physical, and behavioural symptoms | Reported (Complaint of nausea in the intervention group) | [45] |
| Hafeeza et al. (2014) | Single blind |
V. agnus castus seed and Mentha piperita Linndistillate (Arq Pudina) 72 mL |
Placebo | 60 | 13–40 | PMTS-SR, PMTS-O | V. agnus castus seed 1 g and M. piperita distillate 36 mL were administered orally twice daily, 10 days before menstruation in every cycle | 3 | Significant reduction in PMTS score in the intervention group | Not reported | [46] |
| Akbarzadeh et al. (2015) | Double blind | Melissa. officinalis Linn (Badranjboya) essence capsules | Placebo (starch) | 100 | - | PSST | 2 capsules (1200 mg) daily from the first to the last day of their menstrualcycle | 3 | Effective in reduction of symptoms | Not reported | [47] |
| Ataollahi et al. (2015) | Triple blind |
Triticum aestivum Linn (Wheat germ) extract |
Placebo | 100 | 20–45 | DSR | I capsule (400 mg), three times per day between the 16th day of the menstrual cycle to the 5th day of the next menstrual period | 2 | Wheat germ significantly reduced physical (63.56%), psychological (66.30%), and the general score (64.99% | Reported (No side effects) |
[48] |
| Khayat et al. (2015) | Double Blind |
Curcumin from Curcuma longa Linn (haldi) | Placebo (brown sugar) | 70 | - | PSST | Two capsules (100 mg) BID daily for seven days before menstruation and three days after menstruation | 3 | Reduction in symptoms | Reported (No side effects) |
[49] |
| Saki et al. (2015) | Triple blind |
Oenothera biennis Linn (Primrose) oil |
Placebo (n = 40) | 80 | 18–30 | PSST | 3 capsules (1500 mg) TID per day | 3 | Significant relief in symptoms | Not reported | [50] |
| Fanaei et al. (2016) | Double blind | Curcumin capsules | Placebo (Brown sugar) | 70 | - | DSR Fasting Serum BDNF level |
1 capsule of 100 mg/12 h was given for 10 days (in each menstrual cycle 7 days before and 3 days after onset of menstrual bleeding) | 3 | Significant relief in symptoms and increased level of BDNF in the intervention group | Not reported | [51] |
| Malik et al. (2018) | Single blind | Nardostachys jatamansi (D. Don) DC. (jatamansi) capsules | Placebo (Roasted wheat flour) | 60 | 18–45 | PMTS-O, PMTS-SR | 3 capsules orally, BD for the 15 days before the expected date of menstruation, up until the onset of the next menstrual cycle | 2 | PTMS and VAS scores were significantly reduced in the intervention group | Reported (No side effects) |
[52] |
| Heidari et al. (2019) | Double blind |
50,000 IU of vitamin D3 | Placebo pearl fortnightly | 44 | 18–25 | PMS Daily Symptoms Rating form | 50,000 IU of vitamin D3 for fortnightly | 4 | Significant improvement in 25(OH) D, serum IL-12, and TAC levels. | Reported (No side effects) |
[53] |
| Farahmand et al. (2020) | Double blind | Flowers of Echium amoenum Fisch. & C A Mey (Gole gauzaban) |
Placebo | 84 | 20–35 | PSST | Capsules 450 mg of TID from the 21st day to the 3rd day of their next cycle | 2 | Improve PMS symptoms | Reported (No side effects) |
[54] |
| Farahmand et al. (2021) | Double blind | P. anisum seed | Placebo (starch) | 84 | 18–35 | PSST | 110 mg capsules of Anise three times per day started 7 days before the start of the menstruation and continued until 3 days after menses | 2 | Significant relief of symptoms | Reported (No side effects) |
[55] |
| Jafari et al. (2021) | Double blind |
Allium sativum Linn (lahsun) tablet (1.1 mg allicin) |
Placebo (Starch tablet) | 129 | 15–49 | PSST | One tablet (400 mg) daily | 3 | Significant reduction in symptoms | Reported (Mild complaints) | [5] |
DSR: Daily Symptom Report; DRSP-Q: Daily Record of Severity of Problem Questionnaire; PMTS-O: Premenstrual Tension Observer Questionnaire; PMTS-SR: Premenstrual Tension Self-Rating Questionnaire; PSST: Premenstrual Symptoms Screening Tool Questionnaire.
3.3. Risk of Bias Assessment of the Data
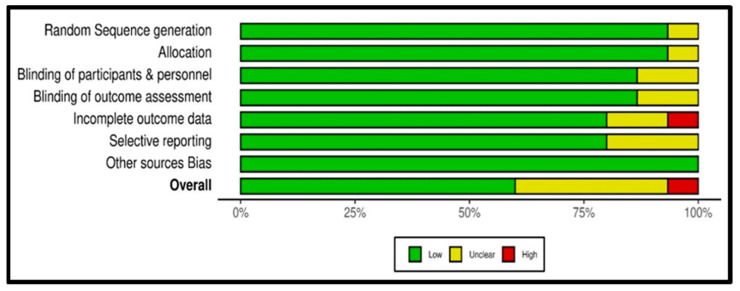
The risk of bias assessment of the data was depicted through the online software Robvis (https://mcguinlu.shinyapps.io/robvis/, accessed on 12 August 2022) in a generic database, which is a web app designed for visualizing risk-of-bias assessment. Figure 2 (traffic light plot) and Figure 3 (summary plot) summarize the risk of bias assessment of the data of the 15 included studies as per methodological quality using a modified Cochrane Risk of Bias tool for RCTs.
Figure 2.
Traffic light plot of randomized controlled trials showing the risk of bias assessment [5,7,43,44,45,46,47,48,49,50,51,52,53,54,55].
Figure 3.
Summary plot of RCTs showing risk of bias.
Bias was measured based on high, low, or unclear individual elements for each domain using a modified Cochrane Risk of Bias tool for RCTs. The red colour in the traffic light plot shows high risk, green colour shows low risk and yellow colour shows unclear risk of bias. The studies of Ozgoli et al. [7], Sharifi et al. [44], Akbarzadeh et al. [47], Fanaei et al. [51], Malik et al. [52], Heidari et al. [53], Farahmand et al. [54], Farahmand et al. [55], and Jafari et al. [5] all had overall low risk of bias, whereas Saki et al. [50] showed an overall high risk of bias (see Figure 2). The studies of Abdollahifard et al. (2014) [43], Khayat et al. (2014) [45], Hafeeza et al. (2014) [46], Ataollahi et al. (2015) [48], and Khayat et al. (2015) [49], showed an overall risk of bias assessment that was unclear. Further, it was observed that studies conducted from 2016 to 2021 showed a low risk of bias.
The quality of included studies was high. All the trials were randomized, three were single-blind, ten studies were double-blind, and two were triple-blind. Out of 15 studies, 4 studies did not report adverse events/side effects, and 11 studies reported adverse events/side effects.
The systematic review showed that 53% of studies (n = 8) had a low risk of bias with high quality. One hundred per cent of the studies were randomized. The appropriate method of randomization was reported by 93.33% of studies, while 86.67% reported participant blinding, personnel and blinding outcome assessment. Outcome data incompleteness and selective reporting were reported by 80%, and 100% of studies reported other sources of bias (see Figure 3).
3.4. Efficacy of Nutritional Supplements and Herbal Medicine on PMS
3.4.1. Primary Parameters
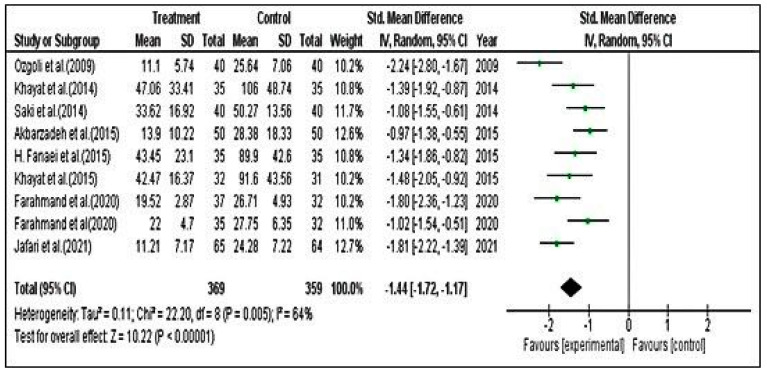
Meta-Analysis for PSST Scores
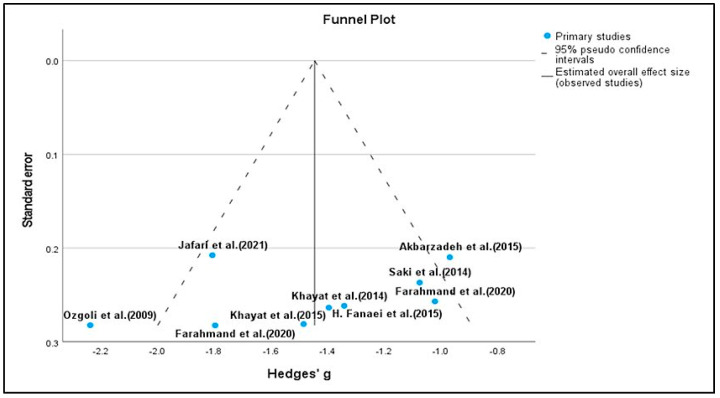
For PSST scores, we included nine studies. The effect estimate was calculated using standardized mean difference with Hedges g and an applied random effect model with inverse variance. The estimation method applied was restricted maximum likelihood (REML) with no adjustment for standard error. Heterogeneity was considered by the Q test and I2. In the study, Q = 18.81 (df = 6, p = 0.004), which specifies that the true effect size is similar in all the trials. The Q statistic has poor power to detect actual heterogeneity when a small number of studies are included in the meta-analysis. When many studies are included, it has excessive power to discover trivial variability to then circumvent the limitations of the Q test. The I2 statistic is 64% in our study, which shows that variance in the observed effects imitates variance of the true effects to a certain extent versus sampling error. In our analysis, we could not observe significant evidence of high heterogeneity. The Q statistics showed p = 0.005; however, in only nine studies, the power to detect heterogeneity was negligible. The variance in the true effect was 0.11. We also employed the Eggers test to determine the degree of funnel plot asymmetry. We found that, in addition to the larger deviation in the intercept, a significant amount of asymmetry was present, as indicated by a p value of 0.982. It is also true that this test has poor power, especially when there are fewer than 10 studies and a minimal amount of asymmetry.
The SMD was −1.44. On average, herbal treatments (intervention group) decreased the PSST score for premenstrual symptoms by −1.44 compared with the control group. The CI for the SMD was [−1.72–−1.17]. This range does not contain an effect size; hence, the mean effect size was not zero. Likewise, the z value for testing the null hypothesis was 10.22, with a corresponding p value of <0.0001. Therefore, we conclude that (on average) the herbal drug decreased the PSST score in the population and rejected the null hypothesis, and the true effect size will drop in this range. The prediction interval suggests that in 95% of populations, it is comparable to those in the analysis (Figure 4 and Figure 5).
Figure 4.
Forest plot for premenstrual screening tool (PSST) [5,7,45,47,49,50,51,54,55].
Figure 5.
Meta-Analysis for DSR Scores
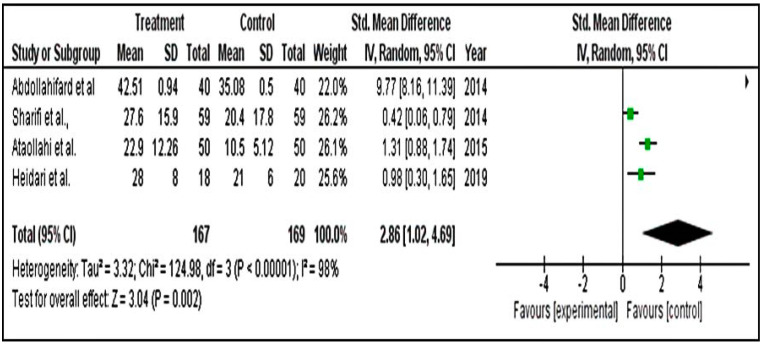
For DSR analysis, we included only four studies. The standardized mean difference obtained was 2.86. The overall effect of 2.86 was seen on average compared with the control group. The confidence interval was from 1.02 to 4.69. This range tells us that the mean effect size is not zero. The z value for testing the null hypothesis for effect size, d = 0, is 3.04, with a corresponding p = 0.002. Hence, we conclude that herbal drugs decreased the DSR score in the population. Therefore, the impact of the treatment on the DSR score for PMS may not be valid in the population at large. The prediction interval is wide because the number of studies is small (Figure 6).
Figure 6.
Forest plot for premenstrual screening tool using DSR [43,44,48,53].
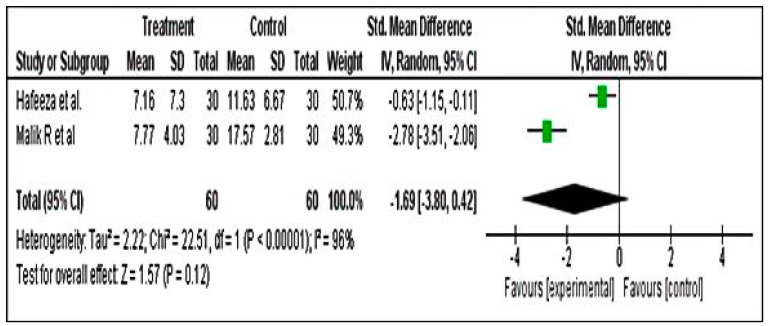
Meta-Analysis for PMTS Scores
The PMTS analysis was carried out including two studies only. The results revealed an overall effect estimate of −1.69 (−3.80–−0.42). The overall effect showed a z value of 1.57 with corresponding p = 0.12 (Figure 7).
Figure 7.
Forest plot for premenstrual screening tool using PMTS [46,52].
3.4.2. Secondary Parameters
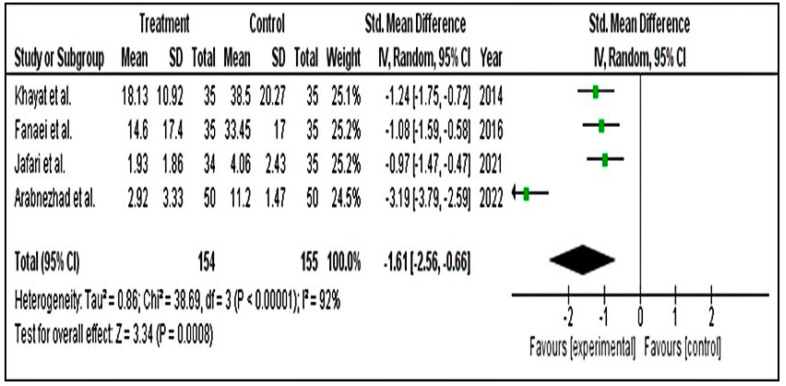
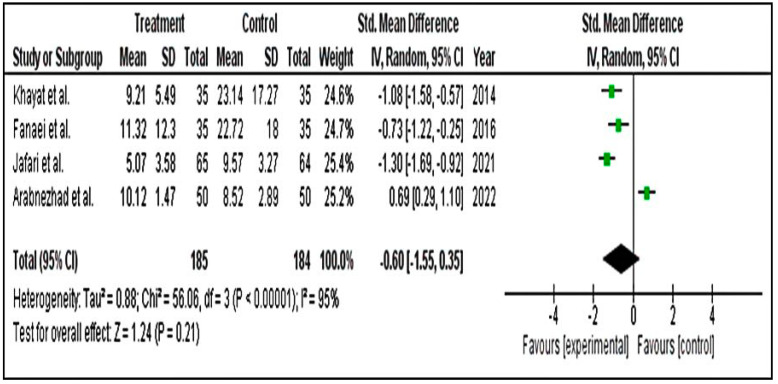
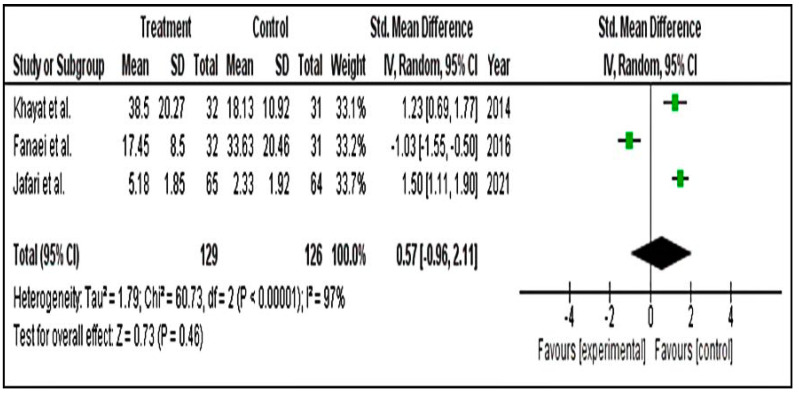
We ran a subgroup group analysis based on the results of physical, behavioural and mood symptoms. Secondary results for physical (SMD = −1.61; 95% CI = −2.56 to −0.66) (Figure 8), behavioural (SMD = −0.60; 95% CI = −1.55 to 0.35) (Figure 9) and mood (SMD = −0.59; 95% CI = −0.96 to 2.11) (Figure 10) symptom groupings of PSST displayed similar findings. From the above finding, we can conclude that, overall, there is a decrease in the symptoms score in the intervention groups. Although the effect size is small, the results are statistically significant.
Figure 8.
Forest plot for subgroup physical symptoms of PSST scale [1,5,45,51].
Figure 9.
Forest plot for subgroup behavioural symptoms of PSST scale [1,5,49,51].
Figure 10.
Forest plot for subgroup mood symptoms of PSST scale [5,45,51].
3.5. Safety of Nutritional Supplements and Herbal Medicine
The meta-analysis of the studies showed that nutritional supplements and herbal medicine are relatively safe for PMS. In 15 studies, 11 studies mentioned side effects. Abdollahifard et al. (2014) [43], Ataollahi et al. (2015) [48], Heidari et al. (2019) [53], Farahmand et al. (2020) [54], and Farahmand et al. (2021) [55] reported no side effects (Table 1). However, Ozgoli et al. (2009) [7] reported that G. biloba showed mild side effects such as nausea and excessive sleep. Only one patient complained of nausea, and two participants reported an increased desire for sleep, and in the placebo group, four participants reported nausea. Khayat et al. (2014) [45] observed that the ginger group had the only side effect of nausea in one patient. Sharifi et al. (2014) [44] reported that the chamomile group had side effects such as an increase in menstrual bleeding and more severe gastrointestinal problems in the mefenamic group with no other side effects in both groups. Jafari et al. (2021) [5] reported mild effects in the garlic group such as itching, acne and flushing.
3.6. Synthesis and Analysis of Previous Studies Related to Herbal Medicine and Nutritional Supplements Related to Premenstrual Syndrome
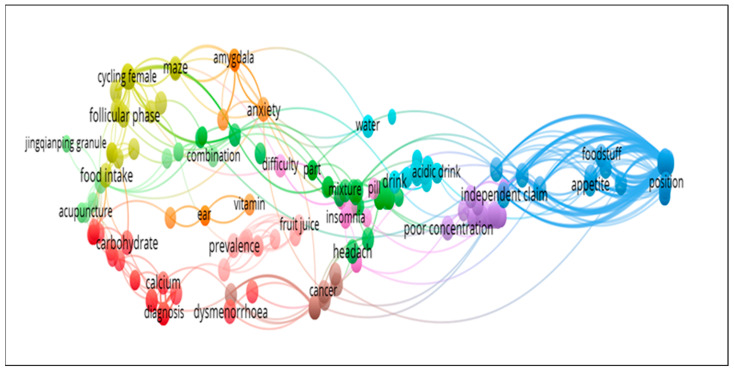
We designed a database based on previously published studies. It is divided into two parts; (i) Based on Web of Science (WoS) and Scopus websites; (ii) Based on network visualization, and word cloud. The WoS and Scopus are more popular and are authentic indexing websites for research work. Additionally, network visualization and word cloud are more popular now because they are based on software and are easy to implement.
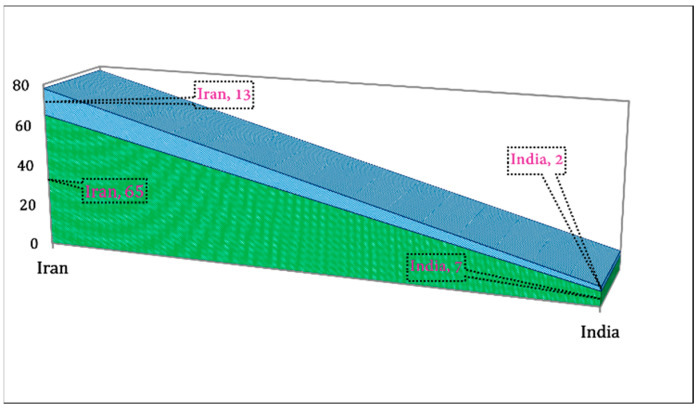
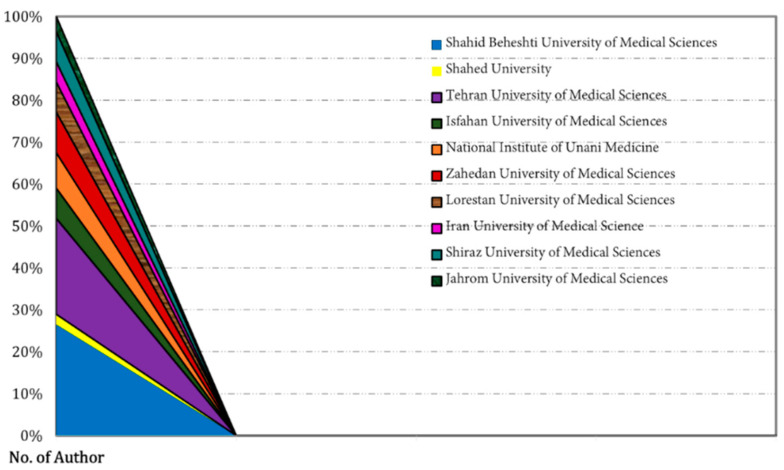
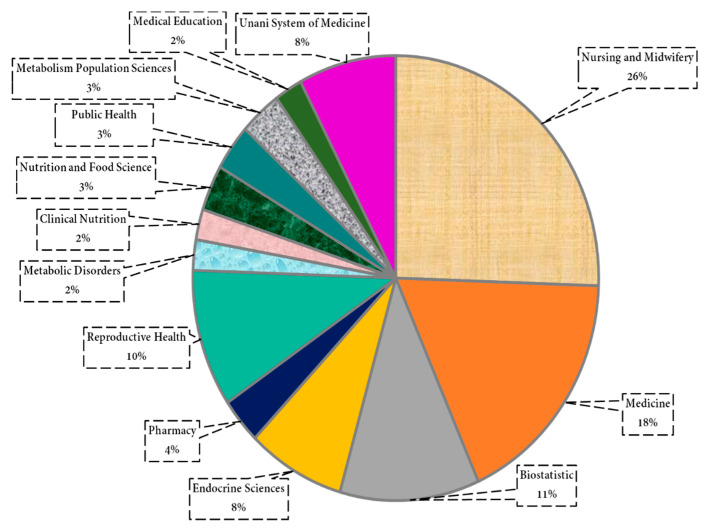
We extracted the data related to the country-wise research area and university/institutions from WoS and Scopus. We found that the Iranian and Indian researchers only worked in this area (Figure 11). The Iranian researcher’s share was found to be 13 out of 15 publications. Additionally, in the university/institution, the highest number of researchers were from Shahid Beheshti University of Medical Sciences (~28%), and the lowest were from Shahed University (~2%) (Figure 12). In the research area, the highest number of researchers were from Nursing and Midwifery (26%) and the lowest from Metabolic Disorders (2%), Clinical Nutrition (2%), and Medical Education (2%), as shown in Figure 13.
Figure 11.
Country-wise and author-wise publications related to RCTs on nutritional supplements and herbal medicine in PMS.
Figure 12.
Author distribution as per university-wise related to published RCTs on nutritional supplements and herbal medicine in PMS.
Figure 13.
Research area-wise authors in a publication on nutritional supplements and herbal medicine in PMS.
We designed the network visualization [56] based on published article keywords using VOSviewer [56], as mentioned in Figure 14. Previously, Heyat’s group used network visualization in the area related to oxidative stress [13], sleep disorders [24,25], motor imagery, education [57], machine learning [58], cryptocurrency [59], and smartphone addiction [26] to write the review. In addition, word clouds based on the present study are mentioned in Figure 15. Heyat’s group also used a word cloud for anxiety [23], stress [58], inflammation [13], camphor [12], deep learning [60], augmented reality [57], and blockchain technology [59] to write the review. These techniques are beneficial to obtain the exact keywords related to any field of research. It is a new tool to analyse previously published publications. In addition, manually, it is difficult to find the closest terms for any big database. These tools will open a new way to visualize the data using VOSviewer software. They easily divide the previously published articles based on terms using the cluster.
Figure 14.
Network visualization based on previously published studies for the collection of the closest terms.
Figure 15.
Word clouds of the present study for the collection of the closest terms.
Our database would be helpful to researchers, doctors, scholars, and scientists to find the exact data based on keywords. It will also open a new way of research and attract new researchers to work in this area, because we have found a very limited number of researchers working in this area.
4. Discussion
4.1. Major Findings
Nutritional supplements and herbal medicines are used for various medicinal approaches. We explored whether nutritional supplements and herbal medicines would be efficacious and safe for the management of premenstrual somatic and psycho-behavioural symptoms. To the best of our knowledge, there has been no meta-analysis previously conducted on premenstrual somatic and psycho-behavioural symptoms with herbal medicine and nutritional supplements. Our results revealed that there was a significant reduction in the PSST, PMTS, and DSRP scores in the intervention group as the comparator. Furthermore, it was observed that physical, behavioural and mood symptom scores improved significantly in the intervention group. Included trials for the present studies were precisely selected. All studies were randomized controlled trials. All studies had a sample size of 30 and above and were well designed according to the CONSORT guidelines. Tolerable side effects related to nutritional supplements and herbs were reported in four trials. In addition, broadly, we emphasized the low risk and high quality of 15 RCTs in premenstrual somatic and psycho-behavioural symptoms. Additionally, the mechanisms of action of plant metabolites and their bioactive molecules effective in PMS symptoms were also comprehensively discussed.
4.2. Comparison with Previously Published Articles
The data of this review inclusively agreed with the published systematic review. However, a meta-analysis of single herbs was available, but none of the studies presented a meta-analysis of nutritional supplements and herbal medicines; they rather wrote the results narratively. The systematic review scrutinized 15 trials that including herbal medicine and nutritional supplements, and it had more participants compared to previous reviews; nonetheless, apprehensions about trial quality remain, along with inadequate reporting details.
Previously, systematic reviews were conducted on PMS regarding herbal medicine and acupuncture (Dante), including 10 RCTs. A systematic study was conducted on the single herb chamomile [6]. Pearce et al. (2020) [8] conducted a systematic review and meta-analysis on exercises for PMS. Other authors included 17 studies on Vitex agnus castus [16]. Another study explored dietary supplements and herbal medicines for PMS [17]. One more systematic review on R. damascena explored the efficacy of anxiety, fatigue, menstruation-related pain, bloating and headache [18]. Csupor et al. [19], for the management of PMS, compared the efficacy of BNO 1095 and Ze 440 to placebo. The researchers systematically reviewed and included 18 RCTs of Iranian herbal medicines and their effectiveness and safety for PMS [20].
Maleki-Saghooni et al. [20] in their systematic review assessed Iranian herbs for premenstrual syndrome treatment and demonstrated their efficacy and safety. The results of our meta-analysis also shed light. Even in our study, we found that herbal medicine and nutritional supplements can be alternative treatments for PMS symptoms. Verkaik et al. [16] showed that the pooled effect of Vitex agnus castus (VAC) was large (Hedges’ g: −1.21; 95% CI: −1.53 to −0.88), but heterogeneity was extremely high. In our study, we found Hedges’ g: −1.44; 95% CI: −1.72 to −1.17. The results of the effect size estimates were slightly higher in our study, and heterogeneity was less (69% vs. 91%). The study also highlighted the need for high-quality trials of suitable size to investigate the effect of vitex in comparison to placebo. In our study, the heterogeneity was comparatively less because we selected good quality studies and based the analysis on a specific scoring system for PSST.
A review by Dante and Facchinett [15] also shows that some herb remedies seem beneficial for PMS treatment. Even our study results are in line with the same. Finally, despite the widespread use of herbs in everyday life, very scarce studies have been devoted to specific clinical investigations. The evidence is scant, but it appears that the relief of only a few herbs could cause relief of PMS. Various studies on herbs showed beneficial effects in decreasing symptoms. Trials should be addressed as comprehensively and thoroughly as possible while adhering to the CONSORT guidelines.
4.3. Mechanism of Action of Plant Products
The precise mechanisms for PMS symptoms are uncertain; we hypothesized that oxidative stress probably affects intricate psycho-somatic disease processes such as PMS. Oestrogen and progesterone have antioxidant effects on healthy women, while in women with PMS, pro-oxidant activity is increased, which leads to oxidative damage [61]. Few clinical trials have confirmed that progesterone and allopregnanolone levels are related to depression in women during the premenstrual phase [62]. Still, oxidative stress and chronic inflammation are potential causes of PMS development and other gynaecological diseases. Few studies have measured the biomarkers of oxidative stress and inflammation in PMS symptoms. In addition, allopregnanolone production is altered in PMS, and its blockage ameliorates serotonin re-uptake inhibitors that also affect allopregnanolone levels [13,61]. Furthermore, psycho-somatic PMS symptoms also involve the aetiology of chronic inflammation, and higher correlations were noted for interleukins (12, 10), including their symptoms [53]. Johnson et al. [63] testified that the strongest association was between IL-10 and IL-12 levels and symptoms in PMS women. In mild to moderate premenstrual symptoms, the treatment modality is diet and lifestyle changes, which potentially is a cure. However, if the symptoms create an adversarial effect on daily life, non-pharmacological and pharmacological treatments are suggested, with the last option being surgery.
Plant products include a variety of inorganic and organic constituents (resins, flavonoids, steroids, tannins, and protein) that are proven to have smooth muscle relaxant, tranquillizing, dopamine CNS depressant, analgesic, immune-modulator, antioxidant, and anti-inflammatory effects [64,65,66,67].
Flavonoids have been proven for a higher antioxidant capacity and for scavenging free radicals [68]. They also display anti-inflammatory activity and modulate signal transduction for the synthesis of pro-inflammatory cytokines [14]. They inhibit the synthesis and release of inducible NO synthase, inflammatory IL-6, TNF-a, and MCP-1 by inhibiting NF-κB, AP-1, and other pro-inflammatory transcription factors. Flavonoids suppress the formation of inflammation mediators (arachidonic acid, leukotrienes, and prostaglandins) through second messenger modulation, and they inhibit COX and lipoxygenase activity and arachidonic acid-metabolizing enzymes [14]. Tannins also have antioxidant properties, and therefore scavenge free radicals and stop oxidative damage [64].
Ginkgo improves mood and behavioural symptoms (depression) since it inhibits MOA and TXA2 methyl esterase and increases catecholamine’s neurotransmitters and decreases the re-uptake of these molecules. It also increases blood circulation by maintaining the balance of prostacyclin. Its bioflavonoids have anti-inflammatory activity, as they inhibit cyclooxygenase and lipoxygenase (important for the production of inflammatory prostaglandins) and are stress modulators. In addition, the quercetin bioactive molecule present in Ginkgo is a potent inhibitor of histamine release. Hence, Ozgoli et al. [7] concluded that Ginkgo was able to reduce the severity of symptoms of this mechanism. The active ingredients in Ginkgo are bioflavonoids. Bioactive molecules Gingerol and shogaol, present in Z. officinalis, have gained significance, as they possess sedative, anti-inflammatory, and analgesic activities. Ginger decreases platelet aggregation and hence has antimigraine potential. It also acts as an effective PG inhibitor and enhances the release of substance P from trigeminal fibres [69]. Vitamin B1 is a coenzyme that reduces symptoms of PMS by affecting the metabolism of lipids, carbohydrates, and protein. Vitamin B1 may increase endorphin secretion, affect brain and liver function, and release ATP, thereby causing relaxation and stimulating sleep. In addition, it can possibly promote cardiovascular system function. Vit. B1 affects the urinary tract and neurological changes. Hence, relieving PMS symptoms, especially mental symptoms, is reasonable. Vitamin B1 also stimulates the CNS and elevates mood, and subsequently, causes deep relaxation [43]. The active bioactive plant metabolite, a flavonoid present in chamomile, stimulates CNS. The bioactive molecules, Apigenin and Luteolin, act as antianxiety and relief as their bind with benzodiazepine receptors [44]. Chamazulene present in chamomile extract has been found accountable for anti-inflammatory activity. Matricine and (-)-alpha-bisabolol also show anti-inflammatory and analgesic activities. (-)-alpha-bisabolol, spiroethers and apigenin exhibit a spasmolytic effect [69]. Vitex agnus castus has dopaminergic compounds, which are clinically important and improve premenstrual mastodynia and other PMS symptoms [69]. The bioactive molecule Jatamansone found in N. jatamansi in experimental animals (mice and monkeys) exerted a tranquillizing effect. In rabbits, jatamansone reduced 5HT in the brain, as it impairs the biosynthesis of serotonin, although the degradation of serotonin was unaffected. Hence, the mode of action of jatamansone was thus in variance with that of reserpine, which has a direct action on the cell to liberate serotonin. Contrary, the roots of Indian Nard’s alcoholic extract cause upsurges in central monamines levels, 5-hydroxyindole acetic acid and inhibitory amino acids, GABA, dopamine, norepinephrine, and serotonin in rat brains [69]. The bioactive molecule found in anise seed, anethole, has a structure similar to catecholamines, including noradrenaline, adrenaline, and dopamine [69]. GABA is an inhibitory neurotransmitter, acting as a neuronal suppressor. It is released from vesicles and activates the GABA receptor family in the postsynaptic membrane. It has been assumed that GABAergic deficits are related to the occurrence of depression. Earlier studies have shown that GABA concentrations in the occipital and prefrontal cortex are knowingly lower in patients with depression [62].
Micronutrients also enhance QoL, and they have been beneficial to reduce PMS symptoms; nevertheless, studies of their efficacy are scarce. Zinc is an essential micronutrient required in human metabolism and is known to play antioxidant and anti-inflammatory roles in the human body [70]. Some studies support that vitamin intake is effective in reducing PMS symptoms. Arabnezhad et al. [1] reported that curcumin improves serum Vit D levels and shows a remarkable increase in serum TAC levels, reproducing an augmentation in antioxidant status in PMS women [53]. Various research studies have confirmed that flowers have gamma-linolenic acid (GLA), which has antioxidant and anti-inflammatory properties and is beneficial to the severity and duration of PMS symptoms. Evening primrose oil also contains GLA and is beneficial in relieving PMS symptom severity at 4 to 6 months follow-up after treatment [71]. In addition, PMS may cause reductions in antioxidant activity and increases in oxidative stress [72].
Various scientific studies have recognised that curcumin can control neurotransmitters (norepinephrine, dopamine, serotonin, and BDNF) accountable for behaviour and mood regulation [51,73]. Chen et al. [62] found that BDNF may be involved in the neuro steroids-mediated regulation of the hypothalamic–pituitary–adrenal (HPA) axis. A study [49] reported that curcumin inhibits the COX-2 enzyme, relieves physical symptoms during menstruation, and improves mood and behavioural symptoms of PMS. In stressed animals, curcumin exhibited strong antidepressant effects, similar to SSRIs (fluoxetine and imipramine), and prevents a decrease in BDNF levels of the hippocampus [51]. Numerous studies have established that phytoestrogens bind to oestrogen receptors and show significant oestrogenic-like effects [74]. The anise seed mechanism of action is similar to SERMs and has agonistic and antagonistic effects on the estrogenic receptors. Anethole acts as the active oestrogenic agent present in anise seed [55].
4.4. Strength of the Study
This updated study has numerous strengths. PRISMA guidelines were used. The PROSPERO-P guideline was followed to write the protocol and was registered in PROSPERO. A complete search approach, established in coordination with comparable reviews, was performed, and electronic databases and grey literature were explored. We performed the determined risk of bias assessment using the Cochrane tool for systematic reviews. For a systematic review of the present study, we also designed a database for country, number of authors, and university/institution from previously published publications. We included RCTs in this review and meta-analysis, and it is anticipated as the highest quality of evidence presently accessible. For the first time, this systematic review and meta-analysis quantitatively summarize the accessible evidence on the objectives of whether nutritional supplements and herbal medicine are effective treatments of premenstrual somatic and psycho-behavioural symptoms. In addition, side effect reporting included in the studies was discussed. Furthermore, we substantially added artificial intelligence including word clouds and network visualization based on keywords.
Nevertheless, this systematic review and meta-analysis are dissimilar to other systematic reviews, as very few publications have included both systematic reviews and meta-analyses. In addition, we summarized the mechanism of action of plant metabolites and their bioactive molecules in herbal medicines. Furthermore, we used SPSS v.28.0.0 (IBM, Armonk, NY, USA) and Rayyan software and Cochrane risk assessment to analyse the risk of assessment of randomized controlled trials. Network visualization was also performed for retrieval of articles from the Web of Science. This study will not only help academicians but also health care professionals and scientists to work in this field and use AI for data recovery from numerous databases. Additionally, our nearby terms might be supportive for academicians, students, researchers, and doctors to find the closest articles concerned with our study.
4.5. Research Gaps, Implications, and Practices
There are some potential research gaps in the study. Moderate to high heterogeneity was observed. However, with only nine studies of PSST, the power to detect heterogeneity was negligible. One of the main reasons for high heterogeneity was the inclusion of studies with various types of herbal formulations. We included nutrition studies as well. The asymmetry of the funnel plot may indicate publication bias, however, due to the limited number of trials. There is a considerable likelihood that deviations from the optimum funnel shape could be the result of chance. Furthermore, a skewed funnel plot can also be brought on by elements other than publication bias, such as the calibre of the study, the variation in intervention intensity, the variation in underlying risk, the choice of the effect measure, and chance. Finally, according to BMJ guidelines, when there are less than 10 papers included in the meta-analysis, testing for funnel plot asymmetry should generally not be utilized because the test power is typically insufficient to distinguish between chance and actual asymmetry [75]. Nevertheless, this meta-analysis can be seen as a first step in providing a formal examination of the hypothesis. The effect size values for PSST and the prediction interval reveal that there will be some populations where the impact of the treatment is large, and somewhere it is trivial. We could not generate evidence which proves that there could be a large effect or impact on the population as a whole. However, it shows relatedly better results in the improvement of various symptoms as compared to the control group.
This systematic review and meta-analysis were conducted through four electronic databases with restrictions to the English language that probably affect the results. In addition, there are a low number of studies for each included study per outcome that perhaps preclude us from assessing publication bias, and the results are relatively suggestive versus conclusive, for which larger RCTs are recommended to study in the future. We would also like to caution the readers that some of the included studies have a high risk of bias based on the Cochrane quality assessment tool for randomized trials. We found that the most recent studies (58%) were low risk. However, future RCTs should stand by methodological standards to reduce bias as much as practicable.
In this paper, the research gap is obvious and consequently should necessitate further investigation. In addition, future trials should plan time concerning the CONSORT guidelines to improve the trial’s quality. Furthermore, larger-scale studies with a large sample size among females from various backgrounds and community socioeconomic levels, utilizing various herbal medicine dosages for longer periods, are recommended. Some studies that do not use a placebo suggested achieving more definitive results concerning the effectiveness and safety of herbal medicine for PMS relief symptoms. Certainly, additional research is crucial to investigate the connection between a given mechanism of action of herbs and nutritional supplements in clinical trials, although limited animal studies have proven anti-inflammatory, sedative, dopamine, antidepressant, SSRIs and antioxidant properties of herbs and nutritional supplements at the molecular level. Hence, additional investigation is needed. Researchers should develop more precise scales to outline PMS. Furthermore, emerging technologies, such as block chain technology, computer vision, quantum techniques, machine learning, and brain network can help to analyse experimental RCT data.
This updated systematic review and meta-analysis supports the suggestion that physicians and healthcare workers caring for PMS women may consider the use of nutritional supplements and herbal medicine as part of their care plan. This may potentially help PMS symptoms and do so with carefulness until good quality evidence is available. The research recommendations are focused to refine writing practices and procedures to enhance the quality of forthcoming trials. It is recommended that forthcoming research in this field must use either the PSST or the DSR alone or both and report global symptom changes such as those reported here. Additional information related to the perseverance of the positive effects of nutritional supplements and herbal medicines beyond the end of the trial period could be studied. If the sample size is large, then subgroup analysis by contraceptive use, age, or other demographic factors might be performed by further systematic reviewers.
5. Conclusions
This updated systematic review and meta-analysis can be a breakthrough towards investigating nutritional supplements and herbal medicines that are possibly effective natural substitutes to relieve premenstrual somatic and psycho-behavioural symptoms. However, there is to date inadequate evidence to conclude whether nutritional supplements and herbal medicine can treat PMS. In addition, we concluded that network visualization and word cloud techniques are easy to use to design a comprehensive diagram of any study. This diagram would be more helpful to upcoming researchers to work in this area and to easily collect exact data. Further study should be designed for the meta-analysis and systematic review of clinical trials of other female disorders.
Acknowledgments
The authors are grateful to Abdul Wadud, Wu, Singh, Naseem, Gul, Nasir, and Ehatsham for the useful discussion and improvement of our article. We also acknowledge the editors, reviewers, and publishers for the useful comments and suggestions for the improvement of this article.
Author Contributions
A.S.: Conceptualization, Data Curation, Formal Analysis, Methodology, Validation, Software, and Writing; M.B.B.H.: Conceptualization, Formal Analysis, Funding Acquisition, Methodology, Validation, Software, Writing, and Resources; K.R., R.K., M.J.A.F. and F.A.: Investigation, Project Administration, Resources, and Supervision; S., J.L.V.M., C.L.R. and I.D.L.T.D.: Funding Acquisition and Supervision. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare that there are no conflict of interest regarding the publication of this study.
Funding Statement
This work was supported by the Fundación Universidad Europea Del Atlántico, Calle Isabel Torres, Santander, Cantabria, Spain.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Arabnezhad L., Mohammadifard M., Rahmani L., Majidi Z., Ferns G.A., Bahrami A. Effects of curcumin supplementation on vitamin D levels in women with premenstrual syndrome and dysmenorrhea: A randomized controlled study. BMC Complement. Med. Ther. 2022;22:19. doi: 10.1186/s12906-022-03515-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Purnawati J., Sinrang A.W., Jusuf E.C., Limoa E., Ahmad M., Usman A.N. Nutrition, mental status and level of 8-hydroxy-2-deoxyguanosine (OHDG) urine as predictors of premenstrual syndrome (PMS) in adolescent girls. Int. J. Curr. Res. Rev. 2020;12:7–13. doi: 10.31782/IJCRR.2020.122315. [DOI] [Google Scholar]
- 3.Abay H., Kaplan S. Current approaches in premenstrual syndrome management. Bezmialem Sci. 2019;7:150–156. doi: 10.14235/bas.galenos.2018.2358. [DOI] [Google Scholar]
- 4.Masoumi S.Z., Ataollahi M., Oshvandi K. Effect of combined use of calcium and vitamin B6 on premenstrual syndrome symptoms: A randomized clinical trial. J. Caring Sci. 2016;5:67–73. doi: 10.15171/jcs.2016.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jafari F., Tabarrai M., Abbassian A., Jafari F., Ayati M.H. Effect of garlic (Allium sativum) supplementation on premenstrual disorders: A randomized, double-blind, placebo-controlled trial. Evid. Based Complement. Altern. Med. 2021;2021:9965064. doi: 10.1155/2021/9965064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khalesi Z.B., Beiranvand S.P., Bokaie M. Efficacy of chamomile in the treatment of premenstrual syndrome: A systematic review. J. Pharmacopunct. 2019;22:204–209. doi: 10.3831/KPI.2019.22.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ozgoli G., Selselei E.A., Mojab F., Majd H.A. A randomized, placebo-controlled trial of Ginkgo biloba L. in treatment of premenstrual syndrome. J. Altern. Complement. Med. 2009;15:845–851. doi: 10.1089/acm.2008.0493. [DOI] [PubMed] [Google Scholar]
- 8.Pearce E., Jolly K., Jones L.L., Matthewman G., Zanganeh M., Daley A. Exercise for premenstrual syndrome: A systematic review and meta-analysis of randomised controlled trials. BJGP Open. 2020;4:bjgpopen20X101032. doi: 10.3399/bjgpopen20X101032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kang W., Ishida E., Amita M., Tatsumi K., Yonezawa H., Yohtsu M., Katano D., Onozawa K., Kaneko E., Iwasaki W., et al. Trehalose suppresses lysosomal anomalies in supporting cells of oocytes and maintains female fertility. Nutrients. 2022;14:2156. doi: 10.3390/nu14102156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frankel R.A., Michels K.A., Kim K., Kuhr D.L., Omosigho U.R., Wactawski-Wende J., Levine L., Perkins N.J., Mumford S.L. Serum antioxidant vitamin concentrations and oxidative stress markers associated with symptoms and severity of premenstrual syndrome: A prospective cohort study. BMC Womens Health. 2021;21:49. doi: 10.1186/s12905-021-01187-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saeedi R., Sultana A., Rahman K., Heyat B.B.M., Kamal M.A., Ishawu M. Efficacy of Acacia nilotica Linn. Pod’s Sitz Bath plus vaginal pessary in syndromic management of abnormal vaginal discharge: A randomized controlled trial. Evid. Based Complement. Altern. Med. 2022;2022:5769555. doi: 10.1155/2022/5769555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fazmiya M.J.A., Sultana A., Rahman K., Heyat M.B.B., Sumbul, Akhtar F., Khan S., Appiah S.C.Y. Current Insights on bioactive molecules, antioxidant, anti-inflammatory, and other pharmacological activities of Cinnamomum camphora Linn. Oxid. Med. Cell. Longev. 2022;2022:9354555. doi: 10.1155/2022/9354555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sultana A., Rahman K., Heyat M.B.B., Sumbul, Akhtar F., Muaad A.Y. Role of inflammation, oxidative stress, and mitochondrial changes in premenstrual psychosomatic behavioral symptoms with anti-inflammatory, antioxidant herbs, and nutritional supplements. Oxid. Med. Cell. Longev. 2022;2022:3599246. doi: 10.1155/2022/3599246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naoi M., Shamoto-Nagai M., Maruyama W. Neuroprotection of multifunctional phytochemicals as novel therapeutic strategy for neurodegenerative disorders: Antiapoptotic and antiamyloidogenic activities by modulation of cellular signal pathways. Future Neurol. 2019;14:FNL9. doi: 10.2217/fnl-2018-0028. [DOI] [Google Scholar]
- 15.Dante G., Facchinetti F. Herbal treatments for alleviating premenstrual symptoms: A systematic review. J. Psychosom. Obstet. Gynecol. 2011;32:42–51. doi: 10.3109/0167482X.2010.538102. [DOI] [PubMed] [Google Scholar]
- 16.Verkaik S., Kamperman A.M., van Westrhenen R., Schulte P.F.J. The treatment of premenstrual syndrome with preparations of Vitex agnus castus: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2017;217:150–166. doi: 10.1016/j.ajog.2017.02.028. [DOI] [PubMed] [Google Scholar]
- 17.Canning S., Waterman M., Orsi N., Ayres J., Simpson N., Dye L. The efficacy of Hypericum perforatum (St. John’s wort) for the treatment of premenstrual syndrome: A randomized, double-blind, placebo-controlled trial. CNS Drugs. 2010;24:207–225. doi: 10.2165/11530120-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 18.Koohpayeh S., Hosseini M., Nasiri M., Rezaei M. Effects of Rosa damascena (Damask rose) on menstruation-related pain, headache, fatigue, anxiety, and bloating: A systematic review and meta-analysis of randomized controlled trials. J. Educ. Health Promot. 2021;10:272. doi: 10.4103/jehp.jehp_18_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Csupor D., Lantos T., Hegyi P., Benkő R., Viola R., Gyöngyi Z., Csécsei P., Tóth B., Vasas A., Márta K., et al. Vitex agnus-castus in premenstrual syndrome: A meta-analysis of double-blind randomised controlled trials. Complement. Ther. Med. 2019;47:102190. doi: 10.1016/j.ctim.2019.08.024. [DOI] [PubMed] [Google Scholar]
- 20.Maleki-Saghooni N., Karimi F.Z., Behboodi Moghadam Z., Mirzaii Najmabadi K. The effectiveness and safety of Iranian herbal medicines for treatment of premenstrual syndrome: A systematic review. Avicenna J. Phytomed. 2018;8:96–113. [PMC free article] [PubMed] [Google Scholar]
- 21.Tu W.J., He J., Chen H., Shi X.D., Li Y. Psychological effects of false-positive results in expanded newborn screening in China. PLoS ONE. 2012;7:e0036235. doi: 10.1371/journal.pone.0036235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Teelhawod B.N., Akhtar F., Heyat M.B.B., Tripathi P., Mehrotra R., Asfaw A.B., Shorman O.A., Masadeh M. Machine Learning in E-health: A Comprehensive Survey of Anxiety; Proceedings of the 2021 International Conference on Data Analytics for Business and Industry; Sakheer, Bahrain. 25–26 October 2021; pp. 167–172. [Google Scholar]
- 24.Heyat M.B.B., Akhtar F., Ansari M.A., Khan A., Alkahtani F., Khan H., Lai D. Progress in detection of insomnia sleep disorder: A comprehensive review. Curr. Drug Targets. 2020;22:672–684. doi: 10.2174/1389450121666201027125828. [DOI] [PubMed] [Google Scholar]
- 25.Heyat M.B.B., Akhtar F., Khan M.H., Ullah N., Gul I., Khan H., Lai D. Detection, treatment planning, and genetic predisposition of bruxism: A systematic mapping process and network visualization technique. CNS Neurol. Disord. Drug Targets. 2020;20:755–775. doi: 10.2174/1871527319666201110124954. [DOI] [PubMed] [Google Scholar]
- 26.Akhtar F., Patel P.K., Heyat M.B.B., Yousaf S., Baig A.A., Mohona R.A., Mutoffar M.M., Bhattacharya T., Teelhawod B.N., Li J.P., et al. Smartphone addiction among students and its harmful effects on mental health, oxidative stress, and neurodegeneration towards future modulation of anti-addiction therapies: A comprehensive survey based on SLR, research questions, and network visualization. CNS Neurol. Disord. Drug Targets. 2022 doi: 10.2174/1871527321666220614121439. [DOI] [PubMed] [Google Scholar]
- 27.Hussain K., Mohd Salleh M.N., Cheng S., Shi Y. Metaheuristic research: A comprehensive survey. Artif. Intell. Rev. 2019;52:2191–2233. doi: 10.1007/s10462-017-9605-z. [DOI] [Google Scholar]
- 28.Shamseer L., Moher D., Clarke M., Ghersi D., Liberati A., Petticrew M., Shekelle P., Stewart L.A., Altman D.G., Booth A., et al. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015: Elaboration and explanation. BMJ. 2015;349:g7647. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 29.Abelha M., Fernandes S., Mesquita D., Seabra F., Ferreira-Oliveira A.T. Graduate employability and competence development in higher education-A systematic literature review using PRISMA. Sustainability. 2020;12:5900. doi: 10.3390/su12155900. [DOI] [Google Scholar]
- 30.Singh S., Kumar K. Review of literature of lean construction and lean tools using systematic literature review technique (2008–2018) Ain Shams Eng. J. 2020;11:465–471. doi: 10.1016/j.asej.2019.08.012. [DOI] [Google Scholar]
- 31.Maskani S., Tafazoli M., Rakhshandeh H., Esmaily H. Effect of nigella sativa seeds on the severity of symptoms of premenstrual syndrome: A randomized clinical trial. Koomesh. 2020;22:33–40. doi: 10.29252/koomesh.22.1.33. [DOI] [Google Scholar]
- 32.Ozgoli G., Shahveh M., Esmaielli S., Nassiri N. Essential oil of citrus sinensis for the treatment of premenstrual syndrome; a randomized double-blind placebo-controlled trial. J. Reprod. Infertil. 2011;12:123–129. [Google Scholar]
- 33.Zamani M., Neghab N., Torabian S. Therapeutic effect of Vitex agnus castus in patients with premenstrual syndrome. Acta Med. Iran. 2012;50:101–106. [PubMed] [Google Scholar]
- 34.Retallick-Brown H., Blampied N., Rucklidge J.J. A pilot randomized treatment-controlled trial comparing vitamin B6 with broad-spectrum micronutrients for premenstrual syndrome. J. Altern. Complement. Med. 2020;26:88–97. doi: 10.1089/acm.2019.0305. [DOI] [PubMed] [Google Scholar]
- 35.Jafari F., Amani R., Tarrahi M.J. Effect of zinc supplementation on physical and psychological symptoms, biomarkers of inflammation, oxidative stress, and brain-derived neurotrophic factor in young women with premenstrual syndrome: A randomized, double-blind, placebo-controlled trial. Biol. Trace Elem. Res. 2020;194:89–95. doi: 10.1007/s12011-019-01757-9. [DOI] [PubMed] [Google Scholar]
- 36.Winther K., Campbell-Tofte J., Motawei A.M., Pedersen F., Roos S.B., Hansen A.S.V., Fornitz G.G., Killi M., Gerhardsen G. A double-blinded, randomized, placebo controlled, parallel study of pollen pistil extract (Sèrèlys) on women reporting irritability as predominant PMS symptom. J. Herb. Med. 2018;12:23–32. doi: 10.1016/j.hermed.2018.02.002. [DOI] [Google Scholar]
- 37.Delaram M., Heydarnejad M.S. Herbal remedy for premenstrual syndrome with fennel (Foeniculum vulgare)—Randomized, placebo-controlled study. Adv. Clin. Exp. Med. 2011;20:509–512. [Google Scholar]
- 38.Gerhardsen G., Hansen A.V., Killi M., Fornitz G.G., Pedersen F., Roos S.B. The efficacy of Femal in women with premenstrual syndrome: A randomised, double-blind, parallel-group, placebo-controlled, multicentre study. Adv. Ther. 2008;25:595–607. doi: 10.1007/s12325-008-0072-4. [DOI] [PubMed] [Google Scholar]
- 39.Agha-Hosseini M., Kashani L., Aleyaseen A., Ghoreishi A., Rahmanpour H., Zarrinara A.R., Akhondzadeh S. Crocus sativus L. (saffron) in the treatment of premenstrual syndrome: A double-blind, randomised and placebo-controlled trial. BJOG Int. J. Obstet. Gynaecol. 2008;115:515–519. doi: 10.1111/j.1471-0528.2007.01652.x. [DOI] [PubMed] [Google Scholar]
- 40.Bahrami A., Bahrami-Taghanaki H., Khorasanchi Z., Timar A., Jaberi N., Azaryan E., Tayefi M., Ferns G.A., Sadeghnia H.R., Ghayour-Mobarhan M. Menstrual problems in adolescence: Relationship to serum vitamins A and E, and systemic inflammation. Arch. Gynecol. Obstet. 2020;301:189–197. doi: 10.1007/s00404-019-05343-1. [DOI] [PubMed] [Google Scholar]
- 41.Esmaeilpour M., Ghasemian S., Alizadeh M. Diets enriched with whole grains reduce premenstrual syndrome scores in nurses: An open-label parallel randomised controlled trial. Br. J. Nutr. 2019;121:992–1001. doi: 10.1017/S0007114519000333. [DOI] [PubMed] [Google Scholar]
- 42.Ghanbari Z., Haghollahi F., Shariat M., Foroshani A.R., Ashrafi M. Effects of calcium supplement therapy in women with premenstrual syndrome. Taiwan. J. Obstet. Gynecol. 2009;48:124–129. doi: 10.1016/S1028-4559(09)60271-0. [DOI] [PubMed] [Google Scholar]
- 43.Abdollahifard S., Rahmanian Koshkaki A., Moazamiyanfar R. The effects of vitamin B1 on ameliorating the premenstrual syndrome symptoms. Glob. J. Health Sci. 2014;6:144–153. doi: 10.5539/gjhs.v6n6p144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sharifi F., Simbar M., Mojab F., Majd H.A. Comparison of the effects of Matricaria chamomila (Chamomile) extract and mefenamic acid on the intensity of premenstrual syndrome. Complement. Ther. Clin. Pract. 2014;20:81–88. doi: 10.1016/j.ctcp.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 45.Khayat S., Kheirkhah M., Behboodi Moghadam Z., Fanaei H., Kasaeian A., Javadimehr M. Effect of treatment with ginger on the severity of premenstrual syndrome symptoms. ISRN Obstet. Gynecol. 2014;2014:792708. doi: 10.1155/2014/792708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Naveed W., Shameem I., Tabassum K. Clinical study of Mutlazima Qabl Haiz (Premenstrual Syndrome) and its management with unani formulation—A randomized controlled trial. Int. J. Cur. Res. Rev. 2014;6:51–57. [Google Scholar]
- 47.Akbarzadeh M., Dehghani M., Moshfeghy Z., Emamghoreishi M., Tavakoli P., Zare N. Effect of Melissa officinalis capsule on the intensity of premenstrual syndrome symptoms in high school girl students. Nurs. Midwifery Stud. 2015;4:e27001. doi: 10.17795/nmsjournal27001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ataollahi M., Ali Akbari S.A., Mojab F., Majd H.A. The effect of wheat germ extract on premenstrual syndrome symptoms. Iran. J. Pharm. Res. 2015;14:159–166. [PMC free article] [PubMed] [Google Scholar]
- 49.Khayat S., Fanaei H., Kheirkhah M., Moghadam Z.B., Kasaeian A., Javadimehr M. Curcumin attenuates severity of premenstrual syndrome symptoms: A randomized, double-blind, placebo-controlled trial. Complement. Ther. Med. 2015;23:318–324. doi: 10.1016/j.ctim.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 50.Saki M., Akbari S., Saki M., Tarrahi M., Gholami M., Pirdadeh S. The effect of primrose oil on the premenstrual syndrome among the female students in Lorestan University of Medical Sciences: A triple blind study. J. Nurs. Midwifery Sci. 2015;2:20. doi: 10.4103/2345-5756.231415. [DOI] [Google Scholar]
- 51.Fanaei H., Khayat S., Kasaeian A., Javadimehr M. Effect of curcumin on serum brain-derived neurotrophic factor levels in women with premenstrual syndrome: A randomized, double-blind, placebo-controlled trial. Neuropeptides. 2016;56:25–31. doi: 10.1016/j.npep.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 52.Malik R., Firdose K.F., Bhat M.D.A. Efficacy of Nardostachys jatamansi DC. in the management of premenstrual syndrome: A randomized controlled study. J. Herb. Med. 2018;14:17–21. doi: 10.1016/j.hermed.2018.09.003. [DOI] [Google Scholar]
- 53.Heidari H., Amani R., Feizi A., Askari G., Kohan S., Tavasoli P. Vitamin D Supplementation for Premenstrual Syndrome-Related inflammation and antioxidant markers in students with vitamin D deficient: A randomized clinical trial. Sci. Rep. 2019;9:14939. doi: 10.1038/s41598-019-51498-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Farahmand M., Khalili D., Ramezani Tehrani F., Amin G., Negarandeh R. Effectiveness of Echium amoenum on premenstrual syndrome: A randomized, double-blind, controlled trial. BMC Complement. Med. Ther. 2020;20:295. doi: 10.1186/s12906-020-03084-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Farahmand M., Khalili D., Ramezani Tehrani F., Amin G., Negarandeh R. Could Anise decrease the intensity of premenstrual syndrome symptoms in comparison to placebo? A double-blind randomized clinical trial. J. Complement. Integr. Med. 2021;17:20190077. doi: 10.1515/jcim-2019-0077. [DOI] [PubMed] [Google Scholar]
- 56.van Eck N.J., Waltman L. Measuring Scholarly Impact. Springer; Cham, Switzerland: 2014. Visualizing bibliometric networks; pp. 285–320. [DOI] [Google Scholar]
- 57.Sheikh S., Heyat M.B.B., AlShorman O., Masadeh M., Alkahatni F. A review of usability evaluation techniques for augmented reality systems in education; Proceedings of the 2021 Innovation and New Trends in Engineering, Technology and Science Education Conference (IETSEC); Amman, Jordan. 16–18 May 2021; pp. 1–6. [Google Scholar]
- 58.Akhtar F., Bin Heyat M.B., Li J.P., Patel P.K., Rishipal, Guragai B. Role of machine learning in human stress: A review; Proceedings of the 2020 17th International Computer Conference on Wavelet Active Media Technology and Information Processing (ICCWAMTIP); Chengdu, China. 18–20 December 2020; pp. 170–174. [Google Scholar]
- 59.Akhtar F., Li J.P., Heyat M.B.B., Quadri S.L., Ahmed S.S., Yun X., Haq A.U. Potential of Blockchain technology in digital currency: A review; Proceedings of the 2019 16th International Computer Conference on Wavelet Active Media Technology and Information Processing (ICCWAMTIP); Chengdu, China. 14–15 December 2019; pp. 85–91. [Google Scholar]
- 60.Guragai B., Alshorman O., Masadeh M., Heyat M.B.B. A survey on deep learning classification algorithms for motor imagery; Proceedings of the 2020 32nd International Conference on Microelectronics (ICM); Aqaba, Jordan. 14–17 December 2020; pp. 1–4. [Google Scholar]
- 61.Granda D., Szmidt M.K., Kaluza J. Is premenstrual syndrome associated with inflammation, oxidative stress and antioxidant status? A systematic review of case-control and cross-sectional studies. Antioxidants. 2021;10:604. doi: 10.3390/antiox10040604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chen S., Gao L., Li X., Ye Y. Allopregnanolone in mood disorders: Mechanism and therapeutic development. Pharmacol. Res. 2021;169:105682. doi: 10.1016/j.phrs.2021.105682. [DOI] [PubMed] [Google Scholar]
- 63.Bertone-Johnson E.R., Ronnenberg A.G., Houghton S.C., Nobles C., Zagarins S.E., Takashima-Uebelhoer B.B., Faraj J.L., Whitcomb B.W. Association of inflammation markers with menstrual symptom severity and premenstrual syndrome in young women. Hum. Reprod. 2014;29:1987–1994. doi: 10.1093/humrep/deu170. [DOI] [PubMed] [Google Scholar]
- 64.Mannan A., Khan R.A., Asif M. Pharmacodynamic studies on Polypodium vulgare (Linn.) Indian J. Exp. Biol. 1989;27:556–560. [PubMed] [Google Scholar]
- 65.Saeedi M., Babaie K., Karimpour-Razkenari E., Vazirian M., Akbarzadeh T., Khanavi M., Hajimahmoodi M., Shams Ardekani M.R. In vitro cholinesterase inhibitory activity of some plants used in Iranian traditional medicine. Nat. Prod. Res. 2017;31:2690–2694. doi: 10.1080/14786419.2017.1290620. [DOI] [PubMed] [Google Scholar]
- 66.Sofiane G., Wafa N., Ouarda D. Antioxidant, antimicrobial and anti-inflammatory activities of flavonoids and tannins extracted from Polypodium vulgare L. Asian J. Biochem. Pharm. Res. 2015;5:114–122. [Google Scholar]
- 67.Naz S.B., Chaudhry M.A., Rahaman M.S.U. Dual receptors blocked mechanism arbitrates smooth muscles relaxant effect of Polypodium vulgare. Bangladesh J. Pharmacol. 2016;11:414–420. doi: 10.3329/bjp.v11i2.25777. [DOI] [Google Scholar]
- 68.Farràs A., Mitjans M., Maggi F., Caprioli G., Vinardell M.P., López V. Polypodium vulgare L. (Polypodiaceae) as a source of bioactive compounds: Polyphenolic profile, cytotoxicity and cytoprotective properties in different cell lines. Front. Pharmacol. 2021;12:727528. doi: 10.3389/fphar.2021.727528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kīrtikara K.R., Basu B.D. Indian Medicinal Plants. Springer; Berlin/Heidelberg, Germany: 2017. [Google Scholar]
- 70.Mousavi S.M., Hajishafiee M., Clark C.C.T., do Nascimento I.J.B., Milajerdi A., Amini M.R., Esmaillzadeh A. Clinical effectiveness of zinc supplementation on the biomarkers of oxidative stress: A systematic review and meta-analysis of randomized controlled trials. Pharmacol. Res. 2020;161:105166. doi: 10.1016/j.phrs.2020.105166. [DOI] [PubMed] [Google Scholar]
- 71.Mahboubi M. Evening Primrose (Oenothera biennis) Oil in Management of Female Ailments. J. Menopausal Med. 2019;25:74. doi: 10.6118/jmm.18190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Duvan C.I., Cumaoglu A., Turhan N.O., Karasu C., Kafali H. Oxidant/antioxidant status in premenstrual syndrome. Arch. Gynecol. Obstet. 2011;283:299–304. doi: 10.1007/s00404-009-1347-y. [DOI] [PubMed] [Google Scholar]
- 73.Lopresti A.L., Hood S.D., Drummond P.D. Multiple antidepressant potential modes of action of curcumin: A review of its anti-inflammatory, monoaminergic, antioxidant, immune-modulating and neuroprotective effects. J. Psychopharmacol. 2012;26:1512–1524. doi: 10.1177/0269881112458732. [DOI] [PubMed] [Google Scholar]
- 74.Parhizkar S., Latiff L.A., Rahman S.A., Dollah M.A., Parichehr H. Assessing estrogenic activity of nigella sativa in ovariectomized rats using vaginal cornification assay. Afr. J. Pharm. Pharmacol. 2011;5:137–142. doi: 10.5897/AJPP10.276. [DOI] [Google Scholar]
- 75.Sterne J.A.C., Sutton A.J., Ioannidis J.P.A., Terrin N., Jones D.R., Lau J., Carpenter J., Rücker G., Harbord R.M., Schmid C.H., et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. doi: 10.1136/bmj.d4002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.