Abstract
Background:
Myxofibrosarcoma (MFS) is a type of sarcoma that mainly affects elderly people; it represents only 5% of all sarcomas and shows no line of differentiation. Intracranial MFS is a rare condition. At present, limited data exist regarding brain metastasis from MFS. This article reports a case of MFS and reviews the literature regarding MFS metastasis.
Case Description:
We report a case of brain metastasis from chest wall MFS. The patient was diagnosed with an anterior thoracic MFS and underwent surgery and radiotherapy. One year later, he noticed a tumor on his left shoulder, and more than 1 year thereafter, bilateral lung metastasis was observed. Twelve months after lung metastasis, he presented to the emergency department and underwent contrast-enhanced magnetic resonance imaging, which demonstrated a left frontal tumor suggestive of brain metastasis. Since the main hypothesis was a sarcoma metastasis at the location close to the left motor area, and the patient had a good Karnofsky performance scale, the patient underwent neuronavigation-guided surgery. After surgery, the patient developed Grade III hemiparesis and aphasia. Brain tumor histopathology confirmed a malignant neoplasm with osteosarcomatous differentiation and metastasis from MFS.
Conclusion:
We report a rare case of MFS metastasis. To the best of our knowledge, this is the eighth case of intracerebral metastasis from MFS.
Keywords: Brain metastasis, Case report, Myxofibrosarcoma, Sarcoma, Thoracic myxofibrosarcoma

INTRODUCTION
Brain metastases are common events in cancer patients, occurring in approximately 10–30% of patients, and are among the most serious complications due to the negative neurological repercussions that directly impact patient quality of life.[12,13]
Except for leukemia and lymphoma, metastasis to the brain is rare.[17] Myxofibrosarcoma (MFS) is a type of sarcoma that mainly affects the elderly, representing only 5% of all sarcomas.[17,18] At present, limited data are available regarding brain metastasis from MFS, particularly in the lungs, primarily in the chest wall. In our literature review, only seven secondary cases of intracerebral MFS were found, none from the lung site. We report a rare case of chest wall MFS with brain metastasis. This article reviews and discusses the literature on the prognosis involved in the present case.
CASE PRESENTATION
A 75-year-old man was diagnosed with anterior thoracic MFS and underwent surgery and radiotherapy. One year later, he noticed a tumor in his left shoulder. The patient was treated with neoadjuvant chemotherapy (ifosfamide + doxorubicin) followed by surgical resection and radiotherapy. One year after the shoulder metastasis diagnosis, bilateral lung metastasis was observed, and chemotherapy treatment (docetaxel + gemcitabine) was started. One year after lung metastasis, the patient presented to the emergency department with sudden onset weakness on the right side and a speech disorder. Neurological examination revealed Grade 4 hemiparesis and aphasia. He underwent brain computed tomography (CT), which revealed a hypodense left frontal lesion. He was prescribed dexamethasone and contrast-enhanced magnetic resonance imaging was performed, which revealed a left frontal tumor suggestive of brain metastasis [Figure 1]. Since the main hypothesis was a sarcoma metastasis close to the left motor area, and the patient had good clinical status (Karnofsky performance scale score of 80), surgical resection was proposed. The patient underwent neuronavigation-guided surgery. A postoperative CT scan showed a hematoma at the surgical site, and reoperation was performed to drain the hematoma [Figure 2]. After surgery, he developed Grade III hemiparesis, and the aphasia persisted. Brain tumor histopathology confirmed a malignant neoplasm with osteosarcomatous differentiation and metastasis from MFS [Figure 3]. The patient developed postoperative pleural effusion and recurrence of pulmonary metastasis was diagnosed. Surgical treatment and chemotherapy were attempted, but the patient died 3 months after the neurological surgery.
Figure 1:
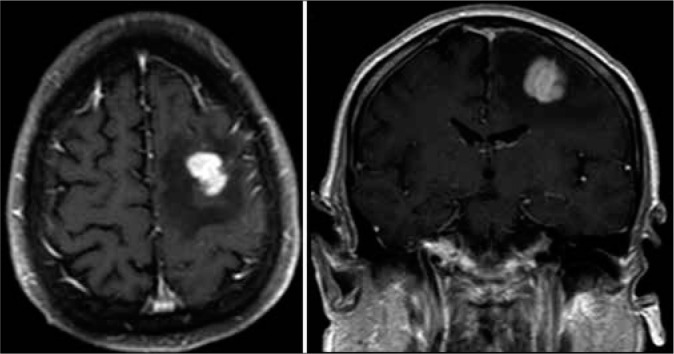
Coronal and axial planes of brain magnetic resonance reveal hypodense left frontal lesion tumor, suggestive of brain metastasis.
Figure 2:
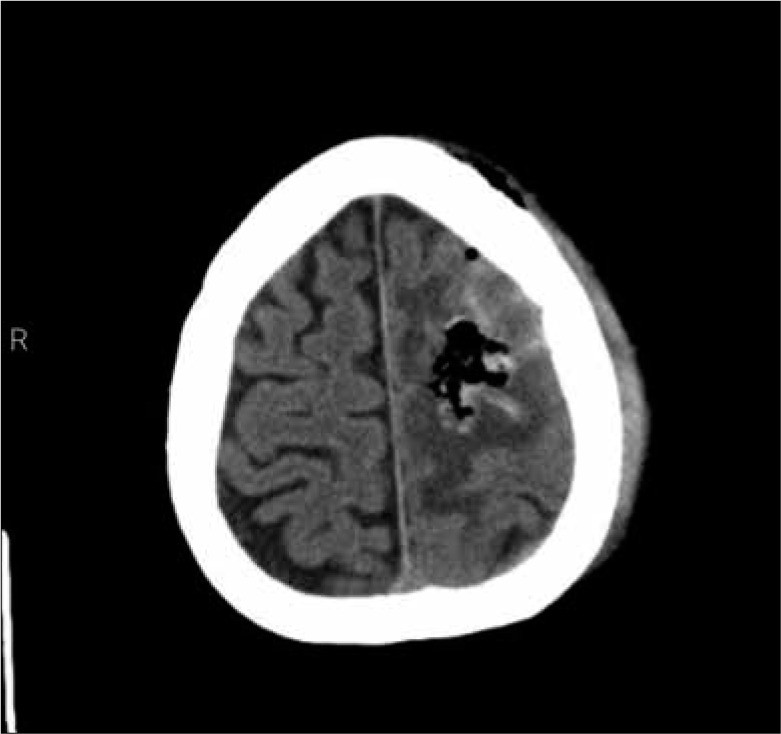
Axial plane of postoperative computed tomography scan.
Figure 3:
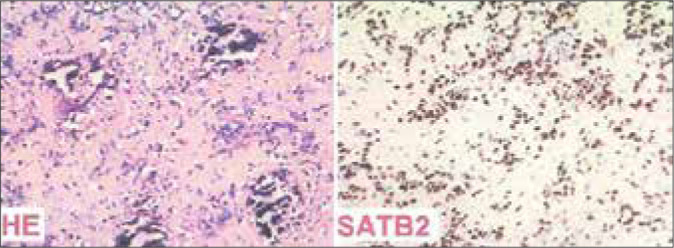
Histopathology images HE stain shows spindle and pleomorphic cells, which are observed in myxofibrosarcoma tumors. Immunohistochemical marker SATB2, which is sensitive and specific for bone and soft-tissue tumors, was positive.
DISCUSSION
MFS, formerly called malignant fibrous histiocytoma (MFH), is a soft-tissue neoplasm belonging to the sarcoma group, characterized by a diffuse infiltrative tissue pattern that can occur in any part of the body.[15] It corresponds to a tumor that originates from the mesenchyme, is aggressive, and constitutes one-third of all soft-tissue sarcomas (STSs) in adults.[9]
MFSs have a high recurrence rate, ranging from 16% to 57%.[18] The head and neck were the areas with the most local recurrence, with an overall risk of metastases between 20% and 25%.[2] In the literature, of the seven cases of secondary intracerebral MFS diagnosis that has been published, there is no chest wall site. For our patient, we elected to perform a surgical approach with neuronavigation-guided surgery of the brain lesion from the chest wall.
Intracranial MFS is rare and some reports have described cases without extracranial sites.[3,6,14,16] Sarrami et al. reported a case of MFS with infiltration of the pons, cerebellum, and basal surface of the left temporal lobe without any visible masses.[16] A 55-year-old man presented with MFS presenting as an acute cerebral hemorrhage, with subsequent development of lung metastases.[14] Thirty-nine previously reported cases were related to location/origin in the brain, treatment, and follow-up, which showed a consensus regarding the diagnosis and treatment of the primary tumor.[6] Brain metastasis was associated with a higher risk when multiple metastases to bone, liver, and lung were reported by a population-based cohort study with 0.26% of the cases with brain metastasis of the 8.433 patients with STS.[6] Other risk factors for brain metastasis in STS were being female and American Indian/ Alaska Native.[6]
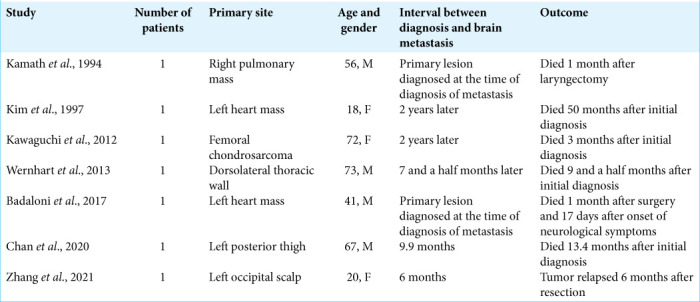
To the best of our knowledge, only seven cases of brain metastasis as a consequence of MFS have been reported, and this is the first case of metastasis from the chest wall.[3,4,10-12,17,18] The study, number of patients, primary site, age, sex, and outcome of these studies are summarized in Table 1.
Table 1:
Data from literature review of brain metastasis from myxofibrosarcoma.
In this case, several prognostic factors were identified. The previous data showed that factors believed to negatively influence survival are advanced patient age, greater tumor size at resection, positive surgical resection margins, higher tumor grading, greater tumor necrosis, higher mitotic rate, low degree of myxoid areas, and intracerebral manifestations.[7]
The clinical manifestations of intracranial MFH vary and are largely dependent on the location of the tumor.[16]
The prognosis tends to be poor and survival is generally short.[1] Our literature review showed a poor prognosis <1 year after the initial diagnosis. Lung metastasis appears to be a high-risk factor for brain metastasis.[6] This is consistent with our case, which did not respond to chemotherapy and the patient died 3 months after the diagnosis of brain metastasis.
Although we showed a single case study with a rare primary site of metastasis, wide resection of MFS appears to be associated with a lower recurrence rate.[5,8]
CONCLUSION
According to the literature regarding metastasis in the frontal lobe, specifically in the motor area due to MFS, this is a very rare case. This is the eighth case reporting intracerebral metastases from MFS and the first report from a lung site. Furthermore, more studies may aid in elucidating the prognostic parameters of this malignant condition, which may improve the quality of life of patients.
Footnotes
How to cite this article: Ferreira Neto OC, Bezerra RB, Silva RP, Silva MR, Alencar Neto JF, Lopes AM. Brain metastasis from a thoracic myxofibrosarcoma: A case report and literature review. Surg Neurol Int 2022;13:537.
Contributor Information
Otávio da Cunha Ferreira Neto, Email: otaviocferreiraneto@gmail.com.
Roberto Borges Bezerra, Email: robertoborgesb@gmail.com.
Rhuann Pontes dos Santos Silva, Email: rhuannpontes02@gmail.com.
Melissa Helena Rodrigues Silva, Email: melissahelenars@gmail.com.
Joaquim Fechine de Alencar Neto, Email: joaquimfechine.n@gmail.com.
Arthur José Maia Lopes, Email: arthurjlopes@gmail.com.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Amezcua-Gutiérrez MA, Gómez SE. Intracranial malignant fibrous histiocytoma. Med Clin (Barc) 2018;151:e61. doi: 10.1016/j.medcli.2018.02.021. [DOI] [PubMed] [Google Scholar]
- 2.Angervall L, Kindblom LG, Merck C. Myxofibrosarcoma. A study of 30 cases. Acta Pathol Microbiol Scand. 1977;85A:127–40. [PubMed] [Google Scholar]
- 3.Badaloni F, Pozzati E, Marucci G, Fiaschi P, Fioravanti A. Primary cardiac high-grade myxofibrosarcoma presenting with multiple brain metastases: A case report. Cureus. 2017;9:e1866. doi: 10.7759/cureus.1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan CM, Lindsay AD, Spiguel AR, Scarborough MT, Gibbs CP. Brain metastases from Truncal and extremity bone and soft tissue sarcoma: Single institution study of oncologic outcomes. Rare Tumors. 2020;12:2036361320960060. doi: 10.1177/2036361320960060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daniels J, Green CM, Freemont A, Paul A. The management of myxofibrosarcoma-a ten-year experience in a single specialist centre. Acta Orthop Belg. 2014;80:436–41. [PubMed] [Google Scholar]
- 6.Gonzalez MR, Bryce-Alberti M, Leon-Abarca JA, Pretell-Mazzini J. Brain metastases in patients with soft-tissue sarcomas: Management and survival-a SEER population-based cohort study. J Am Acad Orthop Surg Glob Res Rev. 2021;5:e21.00219. doi: 10.5435/JAAOSGlobal-D-21-00219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haglund KE, Raut CP, Nascimento AF, Wang Q, George S, Baldini EH. Recurrence patterns and survival for patients with intermediate-and high-grade myxofibrosarcoma. Int J Radiat Oncol Biol Phys. 2012;82:361–7. doi: 10.1016/j.ijrobp.2010.08.042. [DOI] [PubMed] [Google Scholar]
- 8.Hong NJ, Hornicek FJ, Harmon DC, Choy E, Chen YL, Yoon SS, et al. Neoadjuvant chemoradiotherapy for patients with high-risk extremity and truncal sarcomas: A 10-year single institution retrospective study. Eur J Cancer. 2013;49:875–83. doi: 10.1016/j.ejca.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Imampanahi M, Seifi S, Motllebnejad M, Kiani M, Pournabi RA. Malignant fibrous histiocytoma-a case report. J Cancer Res Ther. 2020;16:657–60. doi: 10.4103/jcrt.JCRT_352_18. [DOI] [PubMed] [Google Scholar]
- 10.Kamath SV, Tenreiro-Picon OR, Ragland R, Smith TW, Weaver JP, Knorr JR. Brain metastases from primary lung malignant fibrous histiocytoma: A case report. J Neuroimaging. 1995;5:133–4. doi: 10.1111/jon199552133. [DOI] [PubMed] [Google Scholar]
- 11.Kawaguchi T, Yamanouchi Y, Numa Y, Sakurai Y, Yamahara T, Seno T, et al. A case of metastatic brain tumor causing multifocal cerebral embolism. Brain Tumor Pathol. 2012;29:63–7. doi: 10.1007/s10014-011-0056-y. [DOI] [PubMed] [Google Scholar]
- 12.Kim DG, Lee SY, Chung SK, Park SK, Chun YK, Chi JG. Brain metastasis from myxofibrosarcoma of the heart. Acta Neurochir (Wien) 1997;139:88–9. doi: 10.1007/BF01850875. [DOI] [PubMed] [Google Scholar]
- 13.Norden AD, Wen PY, Kesari S. Brain metastases. Curr Opin Neurol. 2005;18:654–61. doi: 10.1097/01.wco.0000191514.37498.2b. [DOI] [PubMed] [Google Scholar]
- 14.Pimentel J, Fernandes AC, Silva R, Ferro J, Cattoni B. Brain metastases of a malignant fibrous histiocytoma presenting as an acute cerebral hemorrhage. Clin Neuropathol. 2001;20:64–9. [PubMed] [Google Scholar]
- 15.Roland CL, Wang WL, Lazar AJ, Torres KE. Myxofibrosarcoma. Surg Oncol Clin N Am. 2016;25:775–88. doi: 10.1016/j.soc.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 16.Sarrami AH, Setareh M, Afshar-Moghaddam N, Izadinejad M, Saadatnia M. A case of intracranial malignant fibrous histiocytoma. J Res Med Sci. 2011;16:6. [PMC free article] [PubMed] [Google Scholar]
- 17.Wernhart S, Woernle CM, Neidert MC, Bode B, Rushing EJ, Studer G, et al. A deeply seated brain metastasis from a primary myxofibrosarcoma: Case report. Clin Neurol Neurosurg. 2013;115:2296–8. doi: 10.1016/j.clineuro.2013.07.031. [DOI] [PubMed] [Google Scholar]
- 18.Zhang B, Bai M, Tian R, Hao S. Idiopathic and radiation-induced myxofibrosarcoma in the head and neck-case report and literature review. Chin Neurosurg J. 2021;7:48. doi: 10.1186/s41016-021-00267-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


