Abstract
Background:
The subdural evacuation port system (SEPS) is a rapid, bedside, and less invasive option for subdural hemorrhage management. Proper procedure planning and understanding of the relevant vascular anatomy is important for minimizing complications and future procedures.
Case Description:
We describe a case where following placement of a SEPS, there was immediate development of a new dural arteriovenous fistula (dAVF) between the middle meningeal artery (MMA) and middle meningeal vein. Angiography confirmed site of shunting to be at the proximity of the twist drill hole placement. Subsequent MMA embolization was performed and follow-up MRI confirmed resolution of the dAVF.
Conclusion:
SEPS-associated dAVF is an underreported complication with potential long-term consequences. This case describes the complication and advocates avoiding SEPS anterior to the coronal suture.
Keywords: Case report, Dural arteriovenous fistula, Middle meningeal, Subdural hemorrhage
INTRODUCTION
Dural arteriovenous fistula (dAVF) is an extracranial arterial blood flow shunt within the leaflets of the dura mater.[8] Both congenital and acquired pathophysiological origins have been described. Acquired dAVFs have shared origins in some alteration of blood flow that leads to a new shunted and equilibrium. These include venous occlusion or trauma that predispose the existing vascular network to neoangiogenesis and/or inflammatory reactions.[8,14]
Here, we present the first reporting of a dAVF following subdural evacuation port system (SEPS) placement for the evacuation of a subdural hematoma (SDH). Patient consent was obtained. The case provides insight into the possible development timeline of an acquired dAVF. Moreover, this case report offers anatomic guidance on the surgical planning of SEPS for hematoma management and relevant postoperative treatment for postsurgical dAVF.
CLINICAL DESCRIPTION
A 93-year-old female on apixaban for atrial fibrillation presented after a ground level fall with difficulty speaking and an otherwise intact neurological examination. Her head computed tomography (CT) was trended until stable and identified a 16 mm SDH with 9 mm midline shift (MLS; [Figure 1]). She was at first managed conservatively with outpatient follow-up but returned after 1 week for worsening headache, confusion, and aphasia. A new head CT head imaging showed an enlarged mixed density SDH measuring 2.1 cm in thickness with a 12 mm MLS.
Figure 1:
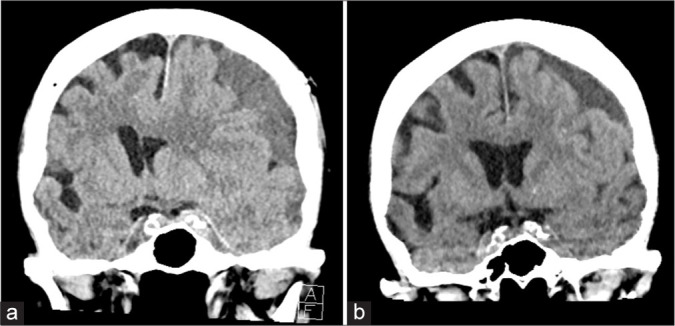
Coronal computed tomography (CT) head imaging of the patient at (a) initial presentation and (b) 2-week follow-up, after discharge from her subdural evacuation and middle meningeal embolization. Initial presentation demonstrated a 15 mm midline shift. Final follow-up CT described a 3 mm midline shift.
She had a frontal SEPS drainage placement and a postprocedural CT head showed interval decrease in the SDH to 1.7 cm with an 11 mm MLS [Figure 2]. The following day, she underwent a middle meningeal artery (MMA) embolization, where a MMA to middle meningeal vein (MMV) dAVF at the site of SEPS placement was identified [Figure 3]. A postembolization DSA immediately after and MRI the following day confirmed elimination of the dAVF.
Figure 2:
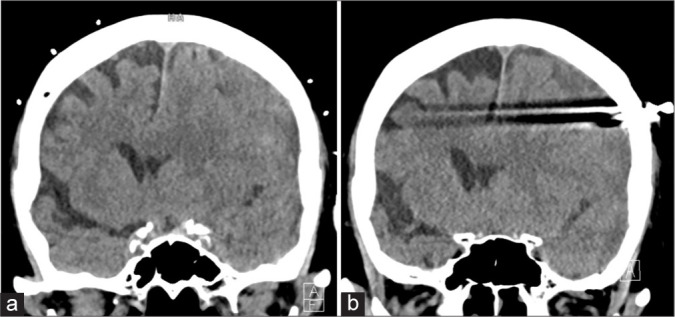
Coronal CT head imaging of the patient immediately before (a) and after (b) subdural evacuation port system (SEPS) placement. The subdural hemorrhage and midline shift decreased from 2.1 cm to 1.7 cm and 12 mm to 11 mm, respectively.
Figure 3:
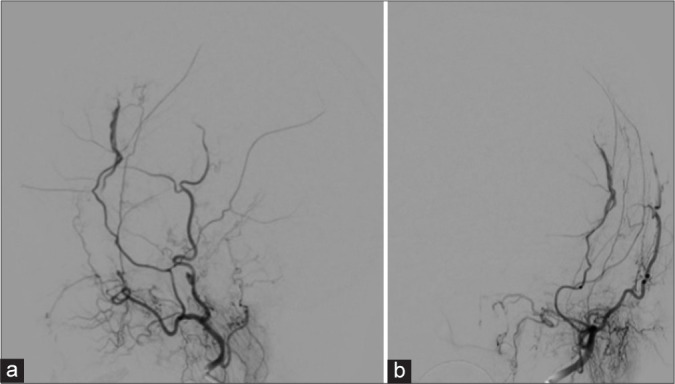
Dual subtraction angiography of the left external carotid from (a) lateral and (b) anterior-posterior views following SEPS drainage demonstrating the anterior left middle meningeal artery supplying a postsurgical arteriovenous fistula with drainage into the left middle meningeal vein, without cortical venous drainage.
A week later, she was at her normal neurological baseline. After additional monitoring, she was ultimately discharged with recommendations to hold anticoagulation for 6 weeks. At 2-week follow-up, a repeat CT head scan identified further reduction in the SDH, measuring 1.5 cm with a 3 mm MLS.
DISCUSSION
Iatrogenic dural arteriovenous fistula have been associated with surgical interventions, but primarily intracranial procedures.[7] The pathology is not without potential sequelae and carry a 2% risk of cerebrovascular accident.[12] This case report represents the first instance where a dAVF could be attributed to a SEPS placement. The sequence of events shows how these fistulae can form within the same day as the surgical procedure entailing dural trauma. The hypothetical alternative mechanisms of neoangiogenesis or inflammation could not produce such an acute presentation.
Similar traumatic MMA-MMV dAVF have been described and have radiographically been characterized to have a “tram-track” presentation.[3,6,11] This development has been attributed to the intimate relationship of the MMV with the meningeal groove along the inner table.[2] Thus, intracranial access that sufficiently disrupts the arterial integrity, while still preserving its proximity to the venous recipient could lead to a dAVF.[13] Such was evidenced in a prior case where a bone flap fixation screw injured the MMA and MMV leading to a similar fistula.[6]
Two case reports of ventriculostomy associated dAVF have been described; however, both were associated with aneurysmal subarachnoid hemorrhage.[3,15] This presented case confirms the possibility of arteriovenous shunting even without the pressure dynamics of postaneurysmal rupture hyperemia. Several other cases of dAVF have been described, but they involve more invasive craniotomies or managements of vascular lesions.[1-6,9-11,16,17]
This case also demonstrates the possible significance of SEPS site selection. The coronal suture is an important landmark as the MMA trajectory runs posterior to it.[4] While ventriculostomy placement usually occurs at Kocher’s point, anterior to the coronal suture, SEPS placement often requires a more posterior site to drain a dependent SDH. Thus, patients may be at greater risk of MMA dAVF with posterior SEPS twist-drill access. As many SEPS placements do not have follow-up DSA, site selections that are adequately anterior to the coronal suture may provide added protection.
CONCLUSION
Dural injury with a twist drill can lead to formation of a dural arteriovenous fistula within the same day of the associated dural trauma. Surgical planning should incorporate the underlying arterial and venous anatomy to reduce the need for subsequent follow-up and treatment.
Footnotes
How to cite this article: Zhang M, Fatemi P, Ghajar J. Acquired dural arteriovenous fistula after subdural evacuation port system placement: A case report. Surg Neurol Int 2022;13:540.
Contributor Information
Michael Zhang, Email: zhangm@stanford.edu.
Parastou Fatemi, Email: parastou@stanford.edu.
Jamshid Ghajar, Email: jghajar@stanford.edu.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ahn JY, Kim OJ, Joo YJ, Joo JY. Dural arteriovenous malformation occurring after craniotomy for pial arteriovenous malformation. J Clin Neurosci. 2003;10:134–6. doi: 10.1016/s0967-5868(02)00109-1. [DOI] [PubMed] [Google Scholar]
- 2.Aminoff MJ. Vascular anomalies in the intracranial dura mater. Brain. 1973;96:601–12. doi: 10.1093/brain/96.3.601. [DOI] [PubMed] [Google Scholar]
- 3.Field M, Branstetter BF, 4th, Levy E, Yonas H, Jungreis CA. Dural arteriovenous fistula after ventriculostomy. Case illustration. J Neurosurg. 2002;97:227. doi: 10.3171/jns.2002.97.1.0227. [DOI] [PubMed] [Google Scholar]
- 4.Hwang SC, Im SB, Kim BT, Shin WH. Safe entry point for twist-drill craniostomy of a chronic subdural hematoma. J Neurosurg. 2009;110:1265–70. doi: 10.3171/2008.9.JNS08359. [DOI] [PubMed] [Google Scholar]
- 5.Igase K, Oka Y, Kumon Y, Zenke K, Iwata S, Sakaki S. A case of dural AVM detected after STA-MCA anastomosis. No Shinkei Geka. 1996;24:81–5. [PubMed] [Google Scholar]
- 6.Kim SW, Chae KS, Shim JH, Rho SJ, Choi HK, Park HS. Iatrogenic dural arteriovenous fistula after superficial temporal artery to middle cerebral artery anastomosis: A case report. Korean J Neurotrauma. 2015;11:151–3. doi: 10.13004/kjnt.2015.11.2.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luther EM, Chagani F, King H, Starke R. Rupture of a de novo dural AV fistula following adult cerebral AVM resection. BMJ Case Rep. 2021;14:e246758. doi: 10.1136/bcr-2021-246758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller TR, Gandhi D. Intracranial dural arteriovenous fistulae: Clinical presentation and management strategies. Stroke. 2015;46:2017–25. doi: 10.1161/STROKEAHA.115.008228. [DOI] [PubMed] [Google Scholar]
- 9.Miura N, Kadota K, Ogawa N, Shinohara T, Shimizu T. A case of arteriovenous communication between external and internal carotid arteries and the sinus after removal of the meningioma (author’s transl) No Shinkei Geka. 1975;3:265–9. [PubMed] [Google Scholar]
- 10.Nabors MW, Azzam CJ, Albanna FJ, Gulya AJ, Davis DO, Kobrine AI. Delayed postoperative dural arteriovenous malformations, Report of two cases. J Neurosurg. 1987;66:768–72. doi: 10.3171/jns.1987.66.5.0768. [DOI] [PubMed] [Google Scholar]
- 11.Pappas CT, Zabramski JM, Shetter AG. Iatrogenic arteriovenous fistula presenting as a recurrent subdural hematoma. Case report. J Neurosurg. 1992;76:134–6. doi: 10.3171/jns.1992.76.1.0134. [DOI] [PubMed] [Google Scholar]
- 12.Satomi J, van Dijk JM, Terbrugge KG, Willinsky RA, Wallace MC. Benign cranial dural arteriovenous fistulas: Outcome of conservative management based on the natural history of the lesion. J Neurosurg. 2002;97:767–70. doi: 10.3171/jns.2002.97.4.0767. [DOI] [PubMed] [Google Scholar]
- 13.Shotar E, Mathon B, Meyblum L, Lenck S, Premat K, Degos V, et al. Letter to the editor regarding “immediate development of dural arteriovenous fistula after middle meningeal artery embolization: First angiographic demonstration”. World Neurosurg. 2019;131:295–6. doi: 10.1016/j.wneu.2019.06.238. [DOI] [PubMed] [Google Scholar]
- 14.Tabibian BE, Liptrap E, Jones J. Incidentally discovered dural arteriovenous fistula during middle meningeal artery embolization for the treatment of chronic subdural hematoma. Surg Neurol Int. 2021;12:438. doi: 10.25259/SNI_183_2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vadivelu S, Xin X, Loven T, Restrepo G, Chalif DJ, Setton A. Iatrogenic dural arteriovenous fistula and aneurysmal subarachnoid hemorrhage. Neurosurg Focus. 2012;32:E1. doi: 10.3171/2012.2.FOCUS1229. [DOI] [PubMed] [Google Scholar]
- 16.Watanabe A, Takahara Y, Ibuchi Y, Mizukami K. Two cases of dural arteriovenous malformation occurring after intracranial surgery. Neuroradiology. 1984;26:375–80. doi: 10.1007/BF00327490. [DOI] [PubMed] [Google Scholar]
- 17.Yassari R, Jahromi B, Macdonald R. Dural arteriovenous fistula after craniotomy for pilocytic astrocytoma in a patient with protein S deficiency. Surg Neurol. 2002;58:59–64. doi: 10.1016/s0090-3019(02)00730-9. discussion 64. [DOI] [PubMed] [Google Scholar]


