Abstract
Background:
Granular cell tumors (GCTs) are uncommon peripheral nerve sheath tumors of Schwann cell origin that may occur throughout the body. However, they rarely occur in the spinal canal.
Case Description:
A 49-year-old male presented with burning sensation in the left knee. The MRI of the lumbar spine showed an L3-L4 intradural extramedullary tumor. Complete surgical resection was successfully performed and the L3 root burning improved. Histopathologically, the lesion proved to be a benign GCT.
Conclusion:
Spinal GCTs are rare benign tumors that may be found in an intradural extramedullary location in the spine. The preferred treatment is complete surgical resection as subtotal/partial resection may result in recurrence warranting radiation therapy.
Keywords: Granular cell tumor, Intradural extramedullary, Intramedullary, Nerve sheath tumor, Spinal canal
INTRODUCTION
Granular cell tumors (GCTs) are uncommon soft-tissue tumors that were initially described as granular cell myoblastoma by Abrinkossoff in 1926.[15] They most commonly occur in the deep dermis and subcutaneous tissue of the head-and-neck region, trunk, and proximal extremities.[18] They may also arise in visceral sites such as the gastrointestinal and respiratory tracts.[18] GCTs of the spinal canal are extremely rare with only few cases reported in the literature. We report a case of a 49-year-old man who was found to have an intradural extramedullary GCT at the L3-L4 level.
CASE DESCRIPTION
A 49-year-old male presented with burning sensation and pain in the left knee for 2 years’ duration. The pain was severe and refractory to pain medications. The lumbar MRI showed a well-circumscribed soft-tissue lesion in the left L3-L4 neural foramen along the course of the left L3 nerve root. It was isointense to hypointense on T1W, hypointense on T2W images [Figure 1] and enhanced with contrast.
Figure 1:
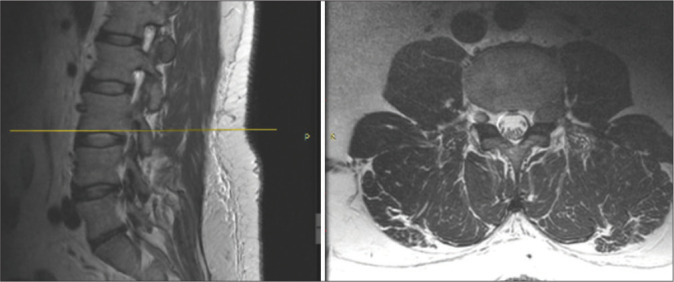
Lumbosacral spine MRI T2 sequence showing soft tissue lesion at the level of L3-L4 (yellow bar).
Surgery
Under fluoroscopic guidance, a bilateral L3-L4 laminectomy was performed. The pedicles of L3 and L4 were exposed along with the transverse processes. The traversing L3 nerve root was identified and the tumor was completely dissected and resected off the root. Postoperatively, the patient sustained improvement in the burning sensation and exhibited no new motor deficit.
Histology
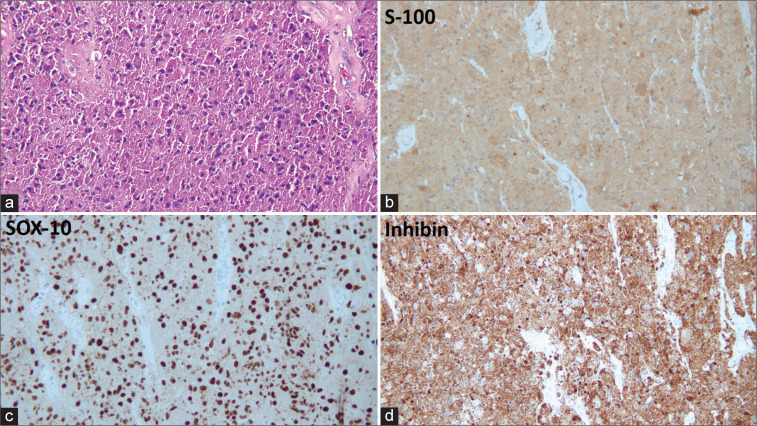
The histological examination was consistent with a benign GCT. It revealed polygonal tumor cells with abundant, eosinophilic, and granular cytoplasm arranged in sheets [Figure 2a]. There was no mitotic activity, necrosis, marked pleomorphism, or tumor spindling. Immunohistochemically, the tumor cells were diffusely positive for S-100, SOX-10, and inhibin [Figures 2b-d] and showed patchy positivity for CD68. They were negative for CD34 and EMA. In addition, the Ki-67 proliferation index was approximately 5%.
Figure 2:
Spinal granular cell tumor. (a) The tumor is composed of sheets of polygonal tumor cells with abundant eosinophilic granular cytoplasm (Hematoxylin and Eosin, original magnification ×20). (b-d) The tumor cells are diffusely positive for S-100, SOX-10, and inhibin (original magnification ×20).
DISCUSSION
GCTs are peripheral nerve sheath tumors that show neuroectodermal differentiation.[18] They are believed to be of Schwann cell origin based on immunohistochemical and ultrastructural findings.[17] They may occur throughout the body, with the tongue being the most common site accounting for 25% of cases.[18] Despite their Schwann cell derivation, GCTs of the spinal canal are very rare. Review of the English literature revealed 20 cases of spinal intradural GCTs [Table 1].[1-17,19] The age of the patients ranged from 9 to 49 years, with the exception of one case that was reported as an incidental autopsy finding at the age of 73. The mean age at presentation is 23 years. There is a female predominance where 16 out of 21 patients (76%) are female. GCTs can be seen throughout the spinal canal: six of the reported cases were in the cervical region, four cases in the thoracic region, three cases in the thoracolumbar region, seven cases in the lumbar region, and one case in the sacral region.
Table 1:
Summary of the reported cases of spinal intradural granular cell tumors.
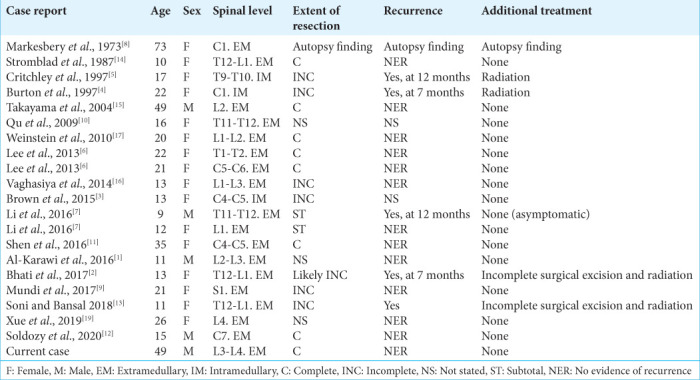
The majority of the reported cases of spinal GCTs have an intradural extramedullary location. The differential diagnosis for tumors in this location includes neurofibroma, schwannoma, meningioma, paraganglioma, epidermoid cyst, intradural dissemination, and, in the cauda equina region, myxopapillary ependymoma. Those tumors can be difficult to distinguish from GCTs on MRI.[15] Hence, histopathologic diagnosis is needed for a definitive diagnosis.
Three spinal GCTs were described as being intramedullary.[3-5] The significance of the presence of an intramedullary component is that the tumor may not be amenable to complete surgical resection because of the associated increased risk of morbidity. In the three reported cases of intramedullary GCTs, complete surgical resection was not possible and the tumors locally recurred within a year in two of the cases.[4,5] In the third case, follow-up information about the patient was not provided.[3]
The vast majority of GCTs behave in a benign fashion; however, they may recur if incompletely excised.[18] None of the reported cases of spinal GCTs was a malignant GCT and none metastasized. GCTs are treated by complete surgical excision, when feasible. Local recurrence was seen in cases that were incompletely excised.[2,4,5,7,13] Of the five cases that locally recurred, two cases were subsequently treated with surgical excision and radiation therapy, two cases were treated with radiation therapy, and one case was asymptomatic so only follow-up was performed.[2,4,5,7,13]
CONCLUSION
GCTs are peripheral nerve sheath tumors that rarely occur in the spinal canal where they are usually intradural/ extramedullary in location. The optimal treatment is gross total surgical excision, as subtotal/partial removal may result in recurrence and the need for adjuvant radiation therapy.
Footnotes
How to cite this article: Farhat L, Hodroj MH, Kawtharani S, Moussalem C, Annan TE, Assi H, et al. Spinal intradural extramedullary granular cell tumor. Surg Neurol Int 2022;13:496.
Contributor Information
Lama Farhat, Email: lf30@aub.edu.lb.
Mohammad Hassan Hodroj, Email: mh309@aub.edu.lb.
Sarah Kawtharani, Email: sk194@aub.edu.lb.
Charbel Moussalem, Email: cm48@aub.edu.lb.
Tamara El Annan, Email: te28@aub.edu.lb.
Hazem Assi, Email: ha157@aub.edu.lb.
Houssein Darwish, Email: hd17@aub.edu.lb.
Sara Sinno, Email: ss262@aub.edu.lb.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Al-Karawi S, Vassilyadi M, Michaud J. Brain Pathology Case of the Month-June 2016. Available from: https://path.upmc.edu/divisions/neuropath/bpath/cases/case334.html.
- 2.Bhati AS, Tyagi A, Tyagi SK. Recurrent granular cell tumor: A case report and review of literature. J Spine Surg. 2017;3:484–8. doi: 10.21037/jss.2017.08.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown KG, Rao PJ, Oo TH, Fowler A. Granular cell tumors of the spinal canal: Intramedullary case report and a review of the literature. J Spine Surg. 2015;1:94–8. doi: 10.3978/j.issn.2414-469X.2015.08.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burton BJ, Kumar VG, Bradford R. Granular cell tumour of the spinal cord in a patient with Rubenstein-taybi syndrome. Br J Neurosurg. 1997;11:257–9. doi: 10.1080/02688699746375. [DOI] [PubMed] [Google Scholar]
- 5.Critchley GR, Wallis NT, Cowie RA. Granular cell tumour of the spinal cord: Case report. Br J Neurosurg. 1997;11:452–4. doi: 10.1080/02688699746005. [DOI] [PubMed] [Google Scholar]
- 6.Lee CH, Hyun SJ, Lee JW, Rhim SC. Granular cell tumor of the intradural extramedullary spinal cord: Report of two cases with respect to radiological differential diagnosis. J Korean Neurosurg Soc. 2013;53:121–4. doi: 10.3340/jkns.2013.53.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li P, Yang Z, Wang Z, Zhou Q, Li S, Wang X, et al. Granular cell tumors in the central nervous system: A report on eight cases and a literature review. Br J Neurosurg. 2016;30:611–8. doi: 10.1080/02688697.2016.1181152. [DOI] [PubMed] [Google Scholar]
- 8.Markesbery WR, Duffy PE, Cowen D. Granular cell tumors of the central nervous system. J Neuropathol Exp Neurol. 1973;32:92–109. doi: 10.1097/00005072-197301000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Mundi I, Pathak A, Banerjee AK, Brar R. Granular cell tumor at an unusual site masquerading as a neurofibroma. Neurol India. 2017;65:1159–61. doi: 10.4103/neuroindia.NI_67_17. [DOI] [PubMed] [Google Scholar]
- 10.Qu J, Ma J, Luo L, Ai L, Li S, Dai J. Subdural granular cell tumor in thoracic vertebral canal. Neurol India. 2009;57:679–81. doi: 10.4103/0028-3886.57799. [DOI] [PubMed] [Google Scholar]
- 11.Shen J, Wang S, Shao X, Xu Z, Dai Y, Xu S, et al. Intraspinal granular cell tumor: A case report and review of literature. Int J Clin Exp Pathol. 2016;9:4013–20. [Google Scholar]
- 12.Soldozy S, Syed HR, Jha RT, O’Connell K, Ozdemirli M, Voyadzis JM. Giant granular cell tumor of the cervical spinal cord resected via anterior corpectomy with reconstruction: Technical note and review of literature. World Neurosurg. 2020;139:136–41. doi: 10.1016/j.wneu.2020.03.157. [DOI] [PubMed] [Google Scholar]
- 13.Soni A, Bansal N. Rare intradural extramedullary spinal granular cell tumor in a young female. MOJ Womens Health. 2018;7:104–7. [Google Scholar]
- 14.Stromblad LG, Brun A, Cameron R, Cronquist S. Spinal granular cell tumor with subarachnoid hemorrhage: Case report. Neurosurgery. 1987;21:230–3. doi: 10.1227/00006123-198708000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Takayama Y, Hasuo K, Takahashi N, Nishimiya M, Nonoshita T, Takita Y, et al. Granular cell tumor presenting as an intradural extramedullary tumor. Clin Imaging. 2004;28:271–3. doi: 10.1016/S0899-7071(03)00200-6. [DOI] [PubMed] [Google Scholar]
- 16.Vaghasiya VL, Nasit JG, Parikh PA, Trivedi PP. Intradural spinal granular cell tumor. Asian J Neurosurg. 2014;9:96–8. doi: 10.4103/1793-5482.136724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weinstein BJ, Arora T, Thompson LD. Intradural, extramedullary spinal cord granular cell tumor: A case report and clinicopathologic review of the literature. Neuropathology. 2010;30:621–6. doi: 10.1111/j.1440-1789.2009.01093.x. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization . WHO Classification of Tumours Series. 5th ed. Vol. 3. Geneva: World Health Organization; 2021. WHO Classification of Tumours Editorial Board. Soft Tissue and Bone Tumours Lyon (France): International Agency for Research on Cancer. Available from: https://tumourclassification.iarc.who.int/chapters/33 [Last accessed on 2022 Sep 29] [Google Scholar]
- 19.Xue J, Chen H, Yang Y, Hu J, Yang G. Granular cell tumors in the human spinal canal: A case report and literature review. Int J Clin Exp Med. 2019;12:4409–13. [Google Scholar]