Abstract
Background
The mortality rate of acute myocardial infarction (AMI) has improved dramatically because of reperfusion therapy during the last 40 years; however, recent temporal trends for AMI have not been fully clarified in Japan.
Objectives
The purpose of this study was to elucidate the temporary trend in in-hospital mortality and treatment of AMI for the last decade in the Tokyo Metropolitan area.
Methods
We enrolled 30,553 patients from the Tokyo Cardiovascular Care Unit Network Registry, diagnosed with AMI from 2007 to 2016, as part of an ongoing, multicenter, cohort study. We analyzed the temporal trends in basic characteristics, treatment, and in-hospital mortality of AMI.
Results
The overall emergency percutaneous coronary intervention (PCI) rate significantly increased (P < 0.001). In particular, it remarkably increased in patients older than 80 years of age (58.3% to 70.3%, P < 0.001) and patients with Killip III or IV (Killip III, 46.9% to 65.7%; Killip IV, 65.2% to 76.6%, P < 0.001 for both). The crude and age-adjusted in-hospital mortality remained low (5.2% to 8.2% and 3.4% to 5.5%, respectively) and significantly decreased during the decade (P < 0.001). The in-hospital mortality remarkably decreased in patients older than 80 years of age (17.3% to 12.7%, P < 0.001) and in those with cardiogenic shock (38.5% to 27.3%, P < 0.001).
Conclusions
This large cohort study from Tokyo revealed that in-hospital mortality of AMI significantly decreased with the increase in emergency percutaneous coronary intervention rate over the decade, particularly for high-risk patients such as older patients and those with cardiogenic shock.
Key Words: in-hospital mortality, older patients, percutaneous coronary intervention, sex, temporal trends
Abbreviations and Acronyms: AMI, acute myocardial infarction; CABG, coronary artery bypass grafting; CAG, coronary angiography; CCU, cardiovascular care unit; D2B, door to balloon; ECMO, extracorporeal membrane oxygenation; FMC, first medical contact; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction
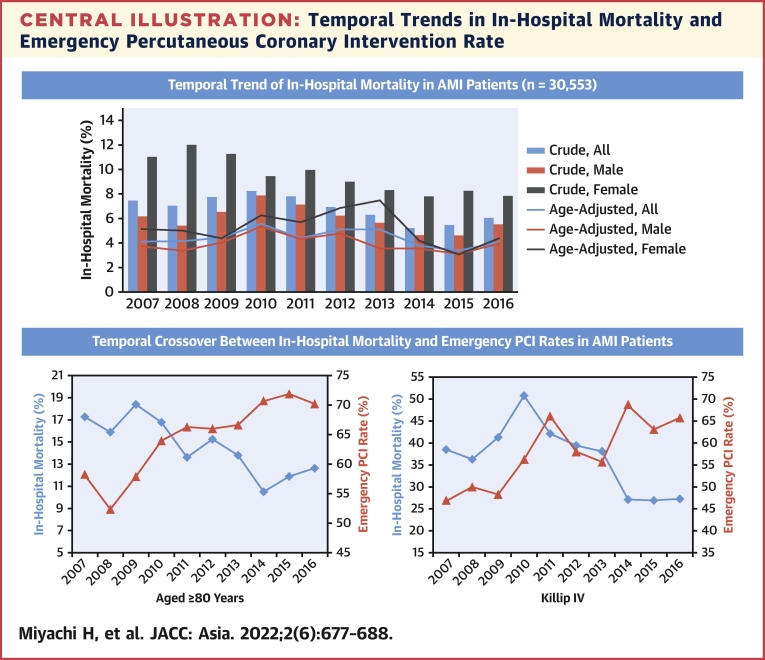
Central Illustration
Acute myocardial infarction (AMI) remains a major cause of morbidity and mortality, with approximately 805,000 new attacks and recurrent AMI every year in the United States, and decreasing trends in the incidence and mortality of AMI have been reported over the past decade.1 Although decreasing trends in the incidence and mortality of AMI have been reported over the past decade in the United States and Europe, the temporal trends of AMI in Japan have not been fully clarified.1,2
Japan has one of the most advanced aging populations in the world. According to the Ministry of Health, Labour and Welfare of Japan, life expectancy at birth in 2018 was 81.3 and 87.3 years for males and females, respectively.3 Thus, AMI data from Japan may provide important information about the future of other countries.
A few regional Japanese registries have shown that in-hospital mortality has plateaued in the last decade.4,5 In contrast, the Tokyo Cardiovascular Care Unit (CCU) network recently revealed that in-hospital mortality decreased slightly but significantly during the last decade using the AMI demographic survey.6 However, detailed data regarding the characteristics and treatment of patients in that survey have not yet been analyzed. Thus, the purpose of this study was to elucidate the temporary trends in in-hospital mortality, emergency percutaneous coronary intervention (PCI), and sex differences among patients with AMI over the last decade in the Tokyo metropolitan area.
Methods
Study population
The Tokyo CCU network database is an ongoing, multicenter, population-based registry. As described above, the AMI demographic survey is the all-comer database that includes only patients’ age, sex, Killip classification, and in-hospital mortality. In contrast, the Tokyo CCU network database also includes their vital signs, medical history, cardiovascular risk factors, comorbidities, clinical course information, outcomes, and complications.7,8 All 73 hospitals participating in the Tokyo CCU network aim to offer 24 hours/7days a week service for emergency PCI within 1 hour of the arrival of the patient at the hospital. Because emergency medical services in the Tokyo metropolitan area do not have a pre-hospital electrocardiogram system, all patients suspected to have emergency cardiovascular diseases were transported to the nearest of the 73 hospitals participating in the Tokyo CCU network as promptly as possible using emergency medical services dispatched through the Tokyo Fire Department with the support of the Tokyo Metropolitan Government.9 The diagnosis of AMI was based on the fourth universal definition.10 The World Health Organization monitoring cardiovascular disease diagnostic criteria were permitted when troponin levels were difficult to assess.11 The management and treatment of AMI were performed by individual cardiologists in each CCU based on guidelines set forth by the Japanese Circulation Society, European Society of Cardiology, and the American College of Cardiology Foundation/American Heart Association.12, 13, 14 Because the Tokyo CCU network is an urban network comprised of PCI-capable hospitals in a relatively small area and PCI can be performed within 120 minutes, in accordance with the guidelines, primary PCI was recommended as the invasive treatment of choice. Patients diagnosed with AMI in each hospital were prospectively registered to the Tokyo CCU network registry. Deducing from the regional distribution of these 73 hospitals, the Tokyo CCU network probably covers 95% of all patients who have had AMI within the greater Tokyo metropolitan area, which has shown the uniformity of high hospital performance among all hospitals.7,15
Ethical principles
The study protocol conforms to the ethical guidelines of the Declaration of Helsinki and is in line with the Ethical Guidelines for Epidemiological Research by the Japanese government. This study was approved by the institutional review board of the Tokyo CCU Network Scientific Committee. According to the guidelines, the study satisfied the conditions for waiving the requirement for informed consent from individual participants.
Statistical analysis
To adjust for age distribution between the time periods, we used the 2010 Japanese population census as the standard population and the Tokyo metropolitan population per year reported by the Tokyo Metropolitan Municipality.16 The significance of trends in the following were analyzed using the Cochran-Armitage test for categorical data or the Jonckheere-Terpstra test for continuous data: age distribution, Killip class distribution, in-hospital mortality, emergency coronary angiography (CAG), emergency PCI, emergency coronary artery bypass grafting (CABG), time to treatment, mechanical complications, mechanical support devices, and ventilators. Emergency CAG, PCI, and CABG were defined as those performed within 24 hours of arrival at the hospital. Analyses were performed using XLSTAT software version 2017 (Addinsoft) and SPSS software version 25.0 (IBM). A value of P < 0.05 was considered statistically significant.
Results
Clinical characteristics
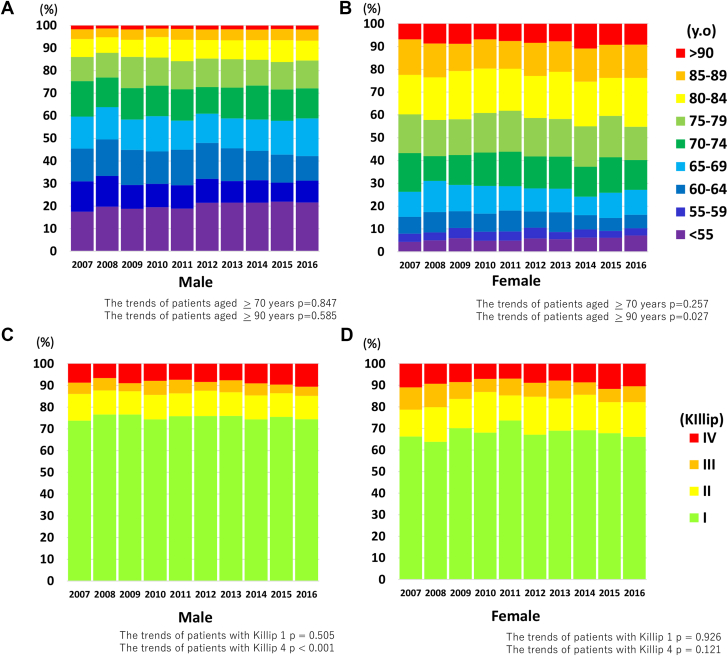
From 2007 to 2016, 30,553 patients with AMI were registered in the database. The median age was approximately 69 years, and the width of the IQR increased during the decade (Table 1). Patients with AMI who were older than 70 years of age accounted for approximately 40% and 70% of men and women, respectively (Figures 1A and 1B); however, the proportion of these patients did not increase. Furthermore, female patients who were older than 90 years of age accounted for approximately 10% of patients with AMI, and the temporal trend showed a gradual increase over the last decade (from 6.9% in 2007 to 9.1% in 2016, P = 0.027). The proportion of patients who were younger than 55 years old and had AMI also increased over these years (from 4.3% in 2007 to 7.1% in 2016, P < 0.001 and from 17.5% in 2007 to 21.6% in 2016, P = 0.043 in men and women, respectively). The proportion of men was approximately 75% and increased from 73.4% in 2007 to 76.0% in 2016 (Table 1). The prevalence of cardiovascular risk factors including hypertension, dyslipidemia, diabetes, smoking, and hyperuricemia increased significantly during the decade. Several types of medical histories, such as those of previous PCI or stroke, showed increasing trends over time (previous PCI: from 5.0% in 2009 to 8.9% in 2016 and stroke: 4.2% in 2009 to 6.1% in 2016). Patients with Killip I and IV accounted for approximately 70% and <10%, respectively, in both sexes (Table 1, Figures 1C and 1D). The proportion of Killip IV patients significantly increased each year, especially among men (from 8.7% in 2007 to 10.6 in 2016, P < 0.001). The same measure did not increase among women (from 11.0% in 2007 to 10.42% in 2016, P = 0.121).
Table 1.
Clinical Characteristics Over Time
| 2007 (n = 2,096) | 2008 (n = 1,832) | 2009 (n = 2,094) | 2010 (n = 2,744) | 2011 (n = 2,809) | 2012 (n = 3,192) | 2013 (n = 3,440) | 2014 (n = 4,080) | 2015 (n = 4,079) | 2016 (n = 4,187) | P Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | |||||||||||
| Age, y | 69 (60-78) | 68 (59-77) | 69 (60-78) | 69 (60-78) | 69 (60-78) | 69 (59-79) | 69 (59-78) | 69 (59-79) | 69 (59-78) | 69 (59-79) | 0.035 |
| Male | 1,539 (73.4) | 1,367 (74.6) | 1,558 (74.4) | 2,087 (76.1) | 2,135 (76.0) | 2,335 (73.2) | 2,609 (75.8) | 3,088 (75.7) | 3,122 (76.5) | 3,180 (76.0) | 0.009 |
| BMI, kg/m2 | Not available | Not available | 23.4 (21.2-25.5) | 23.4 (21.3-25.8) | 23.5 (21.3-26.0) | 23.5 (21.1-25.9) | 23.5 (21.3-26.0) | 23.4 (21.2-25.9) | 23.4 (21.2-26.0) | 23.5 (21.3-26.0) | 0.736 |
| STEMI | 1,602 (76.4) | 1,450 (79.1) | 1,428 (68.2) | 1,856 (67.6) | 1,975 (70.3) | 2,234 (70.0) | 2,561 (74.4) | 3,012 (73.8) | 3,134 (76.8) | 3,129 (74.7) | <0.001 |
| Risk factor | |||||||||||
| Hypertension | Not available | Not available | 949 (45.3) | 1,581 (57.6) | 1,652 (58.8) | 1,813 (56.8) | 2,069 (60.1) | 2,353 (57.7) | 2,484 (60.9) | 2,521 (60.2) | <0.001 |
| Diabetes mellitus | Not available | Not available | 494 (23.6) | 865 (31.5) | 899 (32.0) | 973 (30.5) | 1,043 (30.3) | 1,241 (30.4) | 1,294 (31.7) | 1,304 (31.1) | <0.001 |
| Dyslipidemia | Not available | Not available | 654 (31.2) | 1,119 (40.8) | 1,259 (44.8) | 1,279 (40.1) | 1,386 (40.3) | 1,633 (40.0) | 1,726 (42.3) | 1,780 (42.5) | <0.001 |
| Current smoker | Not available | Not available | Not available | Not available | Not available | Not available | 774 (24.0) | 1,134 (27.9) | 1,204 (29.5) | 1,185 (28.3) | <0.001 |
| Hyperuricemia | Not available | Not available | 103 (4.9) | 97 (3.5) | 129 (4.6) | 164 (5.1) | 183 (5.3) | 206 (5.0) | 240 (5.9) | 269 (6.4) | <0.001 |
| Cardiovascular and renal disease | |||||||||||
| Previous MI | Not available | Not available | 135 (6.4) | 241 (8.8) | 259 (9.2) | 274 (8.6) | 293 (8.5) | 338 (8.2) | 328 (8.0) | 298 (7.1) | 0.238 |
| Previous PCI | Not available | Not available | 105 (5.0) | 241 (8.8) | 273 (9.7) | 278 (8.7) | 334 (9.7) | 410 (10.0) | 425 (10.4) | 373 (8.9) | <0.001 |
| Previous CABG | Not available | Not available | 23 (1.1) | 50 (1.8) | 50 (1.8) | 44 (1.4) | 50 (1.5) | 63 (1.5) | 48 (1.2) | 80 (1.9) | 0.612 |
| Previous CHF | Not available | Not available | 28 (1.3) | 51 (1.9) | 38 (1.4) | 70 (2.2) | 57 (1.7) | 99 (2.4) | 79 (1.9) | 75 (1.8) | 0.091 |
| Previous stroke | Not available | Not available | 88 (4.2) | 142 (5.2) | 174 (6.2) | 177 (5.5) | 225 (6.5) | 247 (6.1) | 274 (6.7) | 254 (6.1) | <0.001 |
| Previous PAD | Not available | Not available | 32 (1.5) | 82 (3.0) | 73 (2.6) | 99 (3.1) | 79 (2.3) | 118 (2.9) | 97 (2.4) | 135 (3.2) | 0.050 |
| Hemodialysis | Not available | Not available | 22 (1.1) | 34 (1.2) | 43 (1.5) | 54 (1.7) | 50 (1.5) | 67 (1.6) | 53 (1.3) | 71 (1.7) | 0.136 |
| Killip classification | |||||||||||
| n | 1,724 | 1,550 | 1,753 | 2,382 | 2,448 | 2,960 | 3,293 | 3,954 | 4,011 | 4,140 | |
| I | 1,237 (71.8) | 1,138 (73.4) | 1,315 (75.0) | 1,741 (73.1) | 1,844 (75.3) | 2,180 (73.6) | 2,446 (74.3) | 2,891 (73.1) | 2,957 (73.7) | 2,999 (72.4) | 0.598 |
| II | 213 (12.4) | 191 (12.3) | 200 (11.4) | 307 (12.9) | 264 (10.8) | 391 (13.2) | 390 (11.8) | 488 (12.3) | 470 (11.7) | 498 (12.0) | 0.734 |
| III | 113 (6.6) | 108 (7.0) | 83 (4.7) | 151 (6.3) | 162 (6.6) | 138 (4.7) | 205 (6.2) | 221 (5.6) | 179 (4.5) | 207 (5.0) | <0.001 |
| IV | 161 (9.3) | 113 (7.3) | 155 (8.8) | 183 (7.7) | 178 (7.3) | 251 (8.5) | 252 (7.7) | 354 (9.0) | 405 (10.1) | 436 (10.5) | <0.001 |
Values are median (IQR) or n (%). P values were tested by Jonckheere-Terpstra trend test for continuous data and Cochran-Armitage trend test for categorical data.
BMI = body mass index; CABG = coronary artery bypass graft; CHF = congestive heart failure; MI = myocardial infarction; PAD = peripheral artery disease; PCI = percutaneous coronary intervention; STEMI = ST-segment elevation myocardial infarction.
Figure 1.
Age and Killip Class Distribution of AMI Patients
(A, B) The temporal trend of age distribution in male and female patients with acute myocardial infarction (AMI), respectively. (C, D) The temporal trend of Killip class distribution in males and females, respectively.
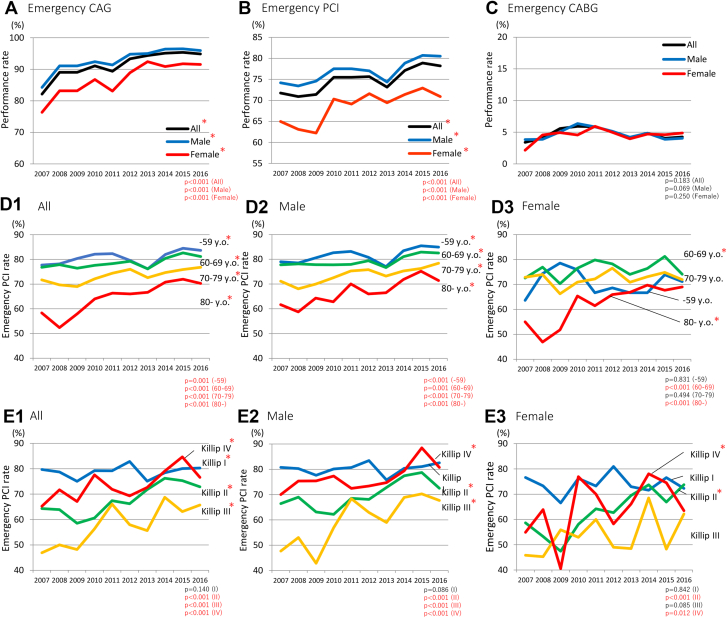
Temporal trends in therapeutic approach
The rate of emergency CAG increased from 84.3% in 2007 to 95.9% in 2016 (men), from 76.3% to 91.6% (women), and from 82.2% to 94.8 (all) (P < 0.001, respectively) (Figure 2A). The emergency CAG rate in women was lower than that in men at any year. Similarly, the rate of emergency PCI also increased from 74.2% in 2007 to 80.5% in 2016 (men), from 65.0% to 70.9% (women), and from 71.7% to 78.2% (all) (P < 0.001, respectively) (Figure 2B). The rate in women was also lower than that in men at any year. In contrast, the rates of emergency CABG did not increase and were approximately 5% in both sexes (Figure 2C). When the patients were divided into 4 age groups, the emergency PCI rates were found to be increased in all groups (from 77.7% to 83.6%, P = 0.001 in the <60-year-old age group; from 76.8% to 81.2%, P < 0.001 in the 60- to 69-year-old age group; from 81.7% to 76.8%, P < 0.001 in the 70- to 79-year-old age group; and from 58.3% to 70.3%, P < 0.001 in the ≥80-year-old age group) (Figure 2D-1). The emergency PCI rate drastically increased in patients aged ≥80 years. In female patients aged ≥80 years, it increased from 55.0% to 69. 0% (Figure 2D-3). Further, it significantly increased among the patients belonging to Killip classes II, III, and IV (Killip II: from 64.3% in 2007 to 72.9% in 2016; Killip III: from 46.2% to 65.7%; and Killip IV: from 65.2% to 76.6%; P < 0.001, respectively) (Figure 2E-1). The tendency was similar among sexes (Figures 2E-2 and 2E-3). The usage rate of intra-aortic balloon pumps and/or venoarterial (VA) extracorporeal membrane oxygenation (ECMO) increased from 21.2% to 36.2% in patients with Killip class III AMI. Furthermore, the usage rate of ventilators decreased in patients with Killip I, II, and IV (Supplemental Figure 1). Limited to ST-segment elevation myocardial infarction (STEMI) patients, the temporal trends of emergency PCI rate were divided into 4 age groups, and Killip classification was similar to that of AMI patients (Supplemental Figure 2).
Figure 2.
Temporal Trends of Emergency PCI, Emergency CAG, and CABG
(A to C) The temporal trend of emergency percutaneous coronary intervention (PCI), emergency coronary angiography (CAG), and coronary artery bypass grafting (CABG), respectively. (D) The temporal trends of emergency PCI rates classified by 4 age groups. (E) The temporal trends of emergency PCI rates according to Killip classification. y.o. = years old.
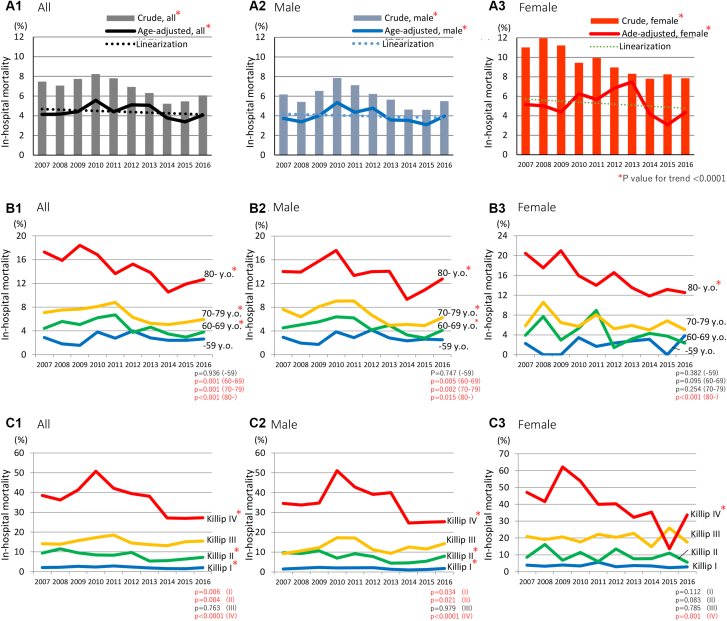
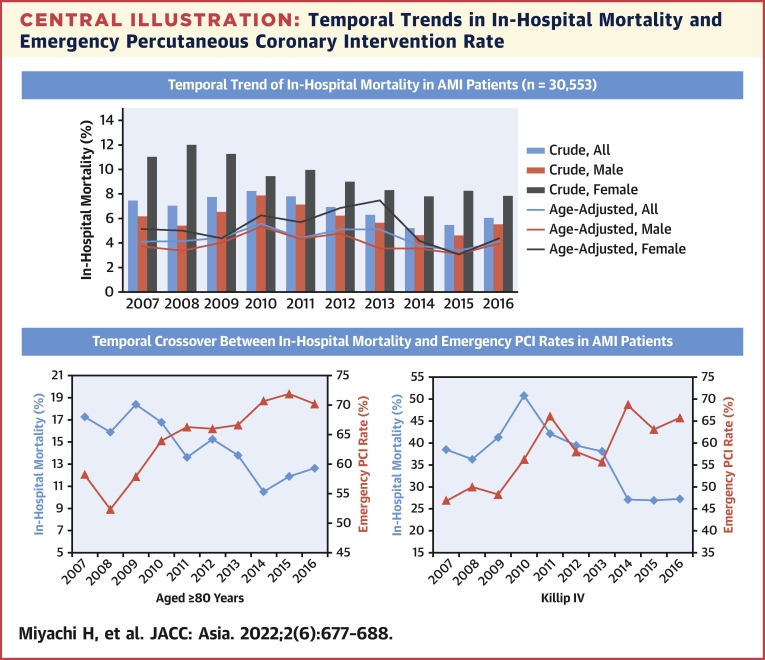
Temporal trends of in-hospital mortality
There were decreasing trends in both crude and age-adjusted in-hospital mortality among the overall (crude: from 7.5% to 6.1%, age-adjusted: from 4.13% to 4.07%), male (crude: 6.2% to 5.5%, age-adjusted: from 3.7% to 4.0%), and female patient groups (crude: 11.0% to 7.8%, age-adjusted: from 5.1% to 4.3%) (P < 0.001, all) (Figure 3A, bar and line graphs). Among STEMI patients, the trends of crude and age-adjusted in-hospital mortalities decreased and were similar to those of AMI patients (Supplemental Figure 3).
Figure 3.
Temporal Trends of In-Hospital Mortality
(A) The temporal trends of crude and age-adjusted in-hospital mortality (A-1, all; A-2, male; A-3, female). The crude in-hospital mortality showed decreasing trends in the overall, male, and female (all; P < 0.001). The age-adjusted in-hospital mortality also showed decreasing trends in the overall (black), male (blue), and female (red) (all; P < 0.001). (B) The temporal trends of age-specific in-hospital mortality in all (B-1), male (B-2), and female (B-3). (C) The temporal trends of in-hospital mortality classified by Killip class in all (C-1), male (C-2), and female (C-3).
Age-specific mortality significantly decreased from 17.3% to 12.7% in older patients aged ≥80 years (P < 0.001), from 7.1% to 5.9% in patients aged 70 to 79 years (P = 0.001), and from 4.4% to 3.8% in patients aged 60 to 69 years (P = 0.001) (Figure 3B-1). In female patients, the mortality decreased from 20.5% to 12.5% (Figure 3B-3). Further, the in-hospital mortality significantly decreased in patients with Killip I (from 2.1% to 2.0%, P = 0.006), Killip II (from 9.4% to 7.2%, P = 0.004), and Killip IV (from 38.5% to 27.2%, P < 0.001) (Figure 3C-1). In female patients, the mortality in Killip IV significantly decreased from 47.1% to 33.7% (Figure 3C-3). Similar trends were observed in patients with STEMI (Supplemental Figure 4). In patients with AMI, the incidence of mechanical complications (ie, free wall rupture, ventricular septal rupture, or papillary muscle rupture) significantly decreased from 1.2% to 0.9% during the decade (P = 0.029) (Supplemental Figure 5).
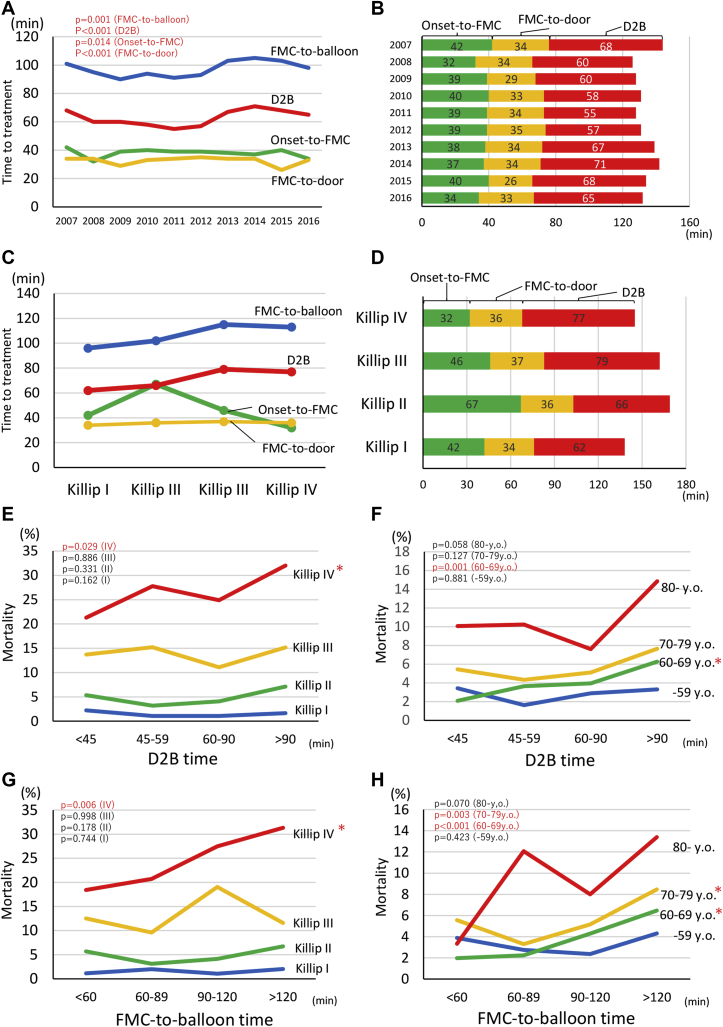
Trends of time to treatment in STEMI patients
In patients with STEMI who underwent PCI within 24 hours from onset of symptoms, the temporal trends of onset-to-first medical contact (FMC), FMC-to-door, door-to-balloon (D2B), and FMC-to-balloon time did not decrease during the decade (from 42.0 [IQR: 18.0-119.0] minutes in 2007 to 33.5 [IQR: 11.0-110.0] minutes in 2016, from 34.0 [IQR: 27.3-42.0] minutes to 33.0 [IQR: 28.0-48.0] minutes, from 68.0 [IQR: 49.0-103.0] minutes to 65.0 [IQR: 46.0-91.0] minutes, and from 101.0 [IQR: 80.0-132.0] minutes to 98.0 [IQR: 80.0-125.5] minutes, respectively) (Figures 4A and 4B). The trends were similar in both sexes (Supplemental Figures 6A and 6B). The proportion of patients achieving D2B time <60 minutes and FMC-to-balloon time <90 minutes also did not increase during the decade (Supplemental Figures 6C and 6D). However, when all STEMI patients who underwent PCI within 24 hours of onset were categorized according to Killip classification in all years, the longer D2B time and FMC-to-balloon time tended to increase with higher Killip classes (D2B: from 62 [IQR: 43-88] minutes in Killip I to 77 [IQR: 52-111] minutes in Killip IV; FMC-to balloon: from 96 [IQR: 77-123] minutes to 113 [IQR: 86-146] minutes) (Figures 4C and 4D). Regarding the association of in-hospital mortality with D2B time and FMC-to-balloon, D2B time and FMC-to-balloon time showed a significant positive association with in-hospital mortality in Killip IV patients (Figures 4E and 4F). In-hospital mortality in patients with Killip IV significantly increased with D2B time (from 21.3% in <45 minutes to 32.0% in >90 minutes) and FMC-to-balloon time (from 18.4% to 31.3%). Furthermore, the D2B and FMC-to-balloon times tended to be associated with in-hospital mortality in patients older than 60 years of age (Figures 4G and 4H).
Figure 4.
Temporal Trends of Time to Treatment in Patients With STEMI
(A) The temporal trends of onset-to-first medical contact (FMC) (green line), FMC-to-door (yellow line), door to balloon (D2B) (red line), and FMC-to-balloon time (blue line) in all patients with ST-segment elevation myocardial infarction (STEMI). (B) The time course of treatment in all years. (C, D) The time to treatment and time course according to the Killip classification, respectively. (E to H) The association of in-hospital mortality with D2B and FMC-to-balloon times according to four Killip classes and 4 age groups.
In particular, in-hospital mortality in patients aged 80 years or older increased with D2B time (from 10.1% in <45 minutes to 14.9% in >90 minutes) and FMC-to-balloon time (from 3.3% to 13.4%), but the difference was not significant.
Discussion
Several important findings were obtained from this large contemporary observational study regarding in-hospital mortality and invasive therapy for patients with AMI in the Tokyo metropolitan area. First, the frequency of invasive procedures has significantly increased over the last decade. Emergency PCI remarkably increased among female patients who were older than 80 years of age, and in those with acute pulmonary edema or cardiogenic shock. Second, although the crude and age-adjusted in-hospital mortalities were already low, mortality further decreased gradually. In-hospital mortality remarkably decreased in older patients (aged ≥80 years) and in those with cardiogenic shock (Killip IV) (Central Illustration). Third, although temporal trends for time to treatment did not improve among patients with STEMI who underwent emergency PCI, the D2B time and FMC-to-balloon time among patients with STEMI and in those with cardiogenic shock and/or older than 60 years of age were strongly related to in-hospital mortality.
Central Illustration.
Temporal Trends in In-Hospital Mortality and Emergency Percutaneous Coronary Intervention Rate
The crude and age-adjusted in-hospital mortality of acute myocardial infarction (AMI) tended to decrease during the last decade in both sexes. The in-hospital mortality of AMI to high-risk patients such as older and Killip IV significantly decreased over time with the increase of emergency percutaneous coronary intervention (PCI) rate.
Similar to a previous Swedish study, the present study revealed that the prevalence of cardiovascular risk factors, increasing hypertension, dyslipidemia, diabetes, smoking, and hyperuricemia, increased significantly throughout the decade (Table 1).2 Hence, prevention and strict management of cardiovascular risk factors are necessary.
In a previous study, we revealed that age-adjusted hospitalized AMI numbers were unchanged, and age-adjusted in-hospital mortality decreased slightly during the decade, consistent with the results of the present study.6 In this study, we elucidated the remarkable decrease in in-hospital mortality of patients with AMI among older patients and in those with cardiogenic shock and the inverse relation to the rate of emergency PCI. However, multiple studies have reported an upward trend in primary PCI in older patients with STEMI.17, 18, 19, 20, 21 This global upward trend in the use of PCI in older patients with AMI is associated with the evolution of PCI devices and the advancement of operator skills. Current guidelines recommend a primary PCI strategy in all patients with symptoms of ischemia of <12-hour duration and persistent ST-segment elevation independent of age and/or severity.13,22 In Japan, as more patients enter advanced age without frailty and as increases in the average life expectancy are observed, operators tend to perform PCI without hesitation in older patients compared to the previous decade.23 This study revealed that adherence to guideline-recommended therapy, such as emergency PCI, is increasing over time, but it is still suboptimal in the course of treatment. Similarly, previous studies have also revealed that guideline-recommended therapy was suboptimal in older patients.20,24
Among many attempts to reduce mortality in cardiogenic shock, early revascularization was the only method with proven efficacy in randomized clinical trials.25 The SHOCK (Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock) registry, which included 277 patients >75 years of age, showed that selected elderly patients had a lower 30-day mortality with early revascularization vs medical stabilization (which included delayed revascularization) with an adjusted odds ratio of 0.46 (95% CI: 0.28-0.75).26,27 In this study, the age-specific in-hospital mortality of Killip IV patients decreased during the decade, and the rate of emergency PCI in these patients remarkably increased. Thus, emergency PCI in Killip IV patients may contribute to the decrease in mechanical complications and in-hospital mortality.
Reperfusion time is also especially important for survival in patients with cardiogenic shock compared with those who were hemodynamically stable. However, this study did not reveal a significant improvement in time to treatment for patients with STEMI. Similarly, the American Heart Association Mission: Lifeline STEMI System Accelerator project did not observe improvements in the FMC-to-device times for patients directly presenting with cardiogenic shock.28 The increased use of emergency PCI in older and Killip IV patients may have prolonged the time to treatment because those patients often have complex lesions and require mechanical support devices for hemodynamic stability. The present study showed that D2B and FMC-to-balloon times were associated with in-hospital mortality in Killip IV and older patients. In a previous study, we revealed that the combined use of VA-ECMO and intra-aortic balloon pump was associated with better neurological outcomes in patients in acute coronary syndrome after the return of spontaneous circulation than was VA-ECMO alone.29 Therefore, when clinicians treat older STEMI patients and/or those with cardiogenic shock, they must provide mechanical circulatory support devices and/or administer vasopressors and perform emergency PCI as soon as possible.
Study limitations
First, this is a nonrandomized and observational study; therefore, it is impossible to prove causality. Furthermore, the association in the trends of in-hospital mortality and PCI rate may be affected by confounders. Second, selection bias should be considered. Low-risk patients with AMI that were admitted to a general ward or a part of patients with non-STEMI may have been excluded. Because the ratio of STEMI was extremely high at any year in this study, which was 70% to 80% (Table 1), the results of the present study might have been strongly influenced by STEMI. Third, important information such as medical therapy, left ventricular ejection fraction, and long-term mortality was not assessed. Fourth, geographical factors and/or sociodemographic factors, including income and educational situation, were not considered in the present study. Finally, this study was based on data from 2007 to 2016 and might not reflect the latest results.
Conclusions
This study shows that in-hospital AMI mortality has been decreasing with the increasing rate of emergency PCI, particularly in older patients and in those with cardiogenic shock. Furthermore, shorter D2B and FMC-to-balloon times in patients with STEMI, cardiogenic shock, and those older than 60 years of age were associated with lower in-hospital mortality rates. Thus, the increase in emergency PCI performed on such patients may correlate with favorable early outcomes. Further improvements in adherence to guideline-recommended therapy and reductions in time to treatment are required to improve outcomes.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE: This study revealed the decreasing tendency of in-hospital mortality among patients with AMI and the increasing rate of emergency PCI, even from 2017 to 2016, particular among older patients and patients with cardiogenic shock.
TRANSLATIONAL OUTLOOK: Further studies are warranted to certify the effectiveness of emergency PCI for Asian patients at high risk for AMI, such as older patients and those with cardiogenic shock.
Funding Support and Author Disclosures
The Tokyo CCU network database for this study was financially supported by the Tokyo Metropolitan Government. The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgments
The authors thank Ms Nobuko Yoshida, Ms Kozue Murayama (Tokyo CCU Network Office), and all staff participating in the Tokyo CCU network for data acquisition.
Footnotes
Adrian Low, MBBS, served as Guest Associate Editor for this paper.
William F. Fearon, MD, served as Guest Editor-in-Chief for this paper.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental figures, please see the online version of this paper.
Appendix
References
- 1.Virani S.S., Alonso A., Aparicio H.J., et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021;143:e254–e743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 2.Szummer K., Wallentin L., Lindhagen L., et al. Improved outcomes in patients with ST-elevation myocardial infarction during the last 20 years are related to implementation of evidence-based treatments: experiences from the SWEDEHEART registry 1995-2014. Eur Heart J. 2017;38:3056–3065. doi: 10.1093/eurheartj/ehx515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Long-term care, health and welfare services for the elderly. Ministry of Health, Labour and Welfare. Government of Japan. https://www.mhlw.go.jp/english/policy/care-welfare/care-welfare-elderly/index.html
- 4.Cui Y., Hao K., Takahashi J., et al. Age-specific trends in the incidence and in-hospital mortality of acute myocardial infarction over 30 years in Japan — report from the Miyagi AMI Registry Study. Circ J. 2017;81:520–528. doi: 10.1253/circj.CJ-16-0799. [DOI] [PubMed] [Google Scholar]
- 5.Kojima S., Matsui K., Ogawa H. Temporal trends in hospitalization for acute myocardial infarction between 2004 and 2011 in Kumamoto, Japan. Circ J. 2013;77:2841–2843. doi: 10.1253/circj.cj-13-1011. [DOI] [PubMed] [Google Scholar]
- 6.Yamamoto T., Yoshida N., Takayama M. Temporal trends in acute myocardial infarction incidence and mortality between 2006 and 2016 in Tokyo — report from the Tokyo CCU Network. Circ J. 2019;83:1405–1409. doi: 10.1253/circj.CJ-19-0187. [DOI] [PubMed] [Google Scholar]
- 7.Miyachi H., Takagi A., Miyauchi K., et al. Current characteristics and management of ST elevation and non-ST elevation myocardial infarction in the Tokyo metropolitan area: from the Tokyo CCU network registered cohort. Heart Vessels. 2016;31:1740–1751. doi: 10.1007/s00380-015-0791-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Higuchi S., Suzuki M., Horiuchi Y., et al. Higher non-cardiac mortality and lesser impact of early revascularization in patients with type 2 compared to type 1 acute myocardial infarction: results from the Tokyo CCU Network registry. Heart Vessels. 2019;34:1140–1147. doi: 10.1007/s00380-019-01350-z. [DOI] [PubMed] [Google Scholar]
- 9.Takano T., Ida T., Tanaka K., Obayashi K., Kimura E. Prehospital care (CCU network) of acute myocardial infarction and treatment of cardiogenic shock by intra-aortic balloon pumping. Jpn Circ J. 1981;45:623–635. doi: 10.1253/jcj.45.623. [DOI] [PubMed] [Google Scholar]
- 10.Thygesen K., Alpert J.S., Jaffe A.S., et al. Fourth universal definition of myocardial infarction (2018) J Am Coll Cardiol. 2018;72:2231–2264. doi: 10.1016/j.jacc.2018.08.1038. [DOI] [PubMed] [Google Scholar]
- 11.Tunstall-Pedoe H., Kuulasmaa K., Amouyel P., et al. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90:583–612. doi: 10.1161/01.cir.90.1.583. [DOI] [PubMed] [Google Scholar]
- 12.Kimura K., Kimura T., Ishihara M., et al. JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ J. 2019;83:1085–1196. doi: 10.1253/circj.CJ-19-0133. [DOI] [PubMed] [Google Scholar]
- 13.Ibanez B., James S., Agewall S., et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 14.O'Gara P.T., Kushner F.G., Ascheim D.D., et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;61(4):e78–e140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 15.Yamamoto T., Otsuka T., Yoshida N., et al. Hospital performance in a large urban acute myocardial infarction emergency care system: Tokyo Cardiovascular Care Unit network. J Cardiol. 2021;78:177–182. doi: 10.1016/j.jjcc.2021.04.002. [DOI] [PubMed] [Google Scholar]
- 16.Statistics Bureau Ministry of Internal Affairs and Communications. Government of Japan. http://www.stat.go.jp/english/index.html
- 17.Bromage D.I., Jones D.A., Rathod K.S., et al. Outcome of 1,051 octogenarian patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention: observational cohort from the London Heart Attack Group. J Am Heart Assoc. 2016;5 doi: 10.1161/JAHA.115.003027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elbadawi A., Elgendy I.Y., Ha L.D., et al. National trends and outcomes of percutaneous coronary intervention in patients ≥70 years of age with acute coronary syndrome (from the National Inpatient Sample Database) Am J Cardiol. 2019;123:25–32. doi: 10.1016/j.amjcard.2018.09.030. [DOI] [PubMed] [Google Scholar]
- 19.Kim J.Y., Jeong M.H., Choi Y.W., et al. Temporal trends and in-hospital outcomes of primary percutaneous coronary intervention in nonagenarians with ST-segment elevation myocardial infarction. Korean J Intern Med. 2015;30:821–828. doi: 10.3904/kjim.2015.30.6.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schoenenberger A.W., Radovanovic D., Windecker S., et al. Temporal trends in the treatment and outcomes of elderly patients with acute coronary syndrome. Eur Heart J. 2016;37:1304–1311. doi: 10.1093/eurheartj/ehv698. [DOI] [PubMed] [Google Scholar]
- 21.Velders M.A., James S.K., Libungan B., et al. Prognosis of elderly patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention in 2001 to 2011: a report from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) registry. Am Heart J. 2014;167:666–673. doi: 10.1016/j.ahj.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 22.Levine G.N., Bates E.R., Blankenship J.C., et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J Am Coll Cardiol. 2016;67:1235–1250. doi: 10.1016/j.jacc.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 23.Kojima S., Nishihira K., Takegami M., et al. Nationwide real-world database of 20,462 patients enrolled in the Japanese Acute Myocardial Infarction Registry (JAMIR): impact of emergency coronary intervention in a super-aging population. Int J Cardiol Heart Vasc. 2018;20:1–6. doi: 10.1016/j.ijcha.2018.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malkin C.J., Prakash R., Chew D.P. The impact of increased age on outcome from a strategy of early invasive management and revascularisation in patients with acute coronary syndromes: retrospective analysis study from the ACACIA registry. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2011-000540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thiele H., Allam B., Chatellier G., Schuler G., Lafont A. Shock in acute myocardial infarction: the Cape Horn for trials? Eur Heart J. 2010;31:1828–1835. doi: 10.1093/eurheartj/ehq220. [DOI] [PubMed] [Google Scholar]
- 26.Dzavik V., Sleeper L.A., Cocke T.P., et al. Early revascularization is associated with improved survival in elderly patients with acute myocardial infarction complicated by cardiogenic shock: a report from the SHOCK trial registry. Eur Heart J. 2003;24:828–837. doi: 10.1016/s0195-668x(02)00844-8. [DOI] [PubMed] [Google Scholar]
- 27.Hochman J.S., Sleeper L.A., Webb J.G., et al. Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction. JAMA. 2006;295:2511–2515. doi: 10.1001/jama.295.21.2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kochar A., Al-Khalidi H.R., Hansen S.M., et al. Delays in primary percutaneous coronary intervention in ST-segment elevation myocardial infarction patients presenting with cardiogenic shock. J Am Coll Cardiol Intv. 2018;11:1824–1833. doi: 10.1016/j.jcin.2018.06.030. [DOI] [PubMed] [Google Scholar]
- 29.Kuroki N., Nagao K., Otsuka T., et al. Combined use of venoarterial extracorporeal membrane oxygenation and intra-aortic balloon pump after cardiac arrest. Resuscitation. 2021;167:345–354. doi: 10.1016/j.resuscitation.2021.07.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.