Abstract
Background:
The emergence or re-emergence of several orthobunyaviruses (order: Bunyavirales; family: Peribunyaviridae), including Cache Valley virus (CVV) and Oropouche virus, warrants the development and evaluation of candidate live-attenuated vaccines (LAVs). Ideally, these vaccines would elicit long-lasting immunity with one single immunization.
Materials and Methods:
Since the deletion of two virulence factors, NSs and NSm, has been shown to attenuate the virulence phenotype of orthobunyaviruses, phleboviruses, and nairoviruses, genetic manipulation of the viral genome is considered an effective strategy for the rational design of candidate LAVs for bunyaviruses across multiple families. In addition, the deletion of Rift Valley fever virus NSs and NSm genes has been shown to reduce transmission by mosquitoes.
Results:
In this study, the ability of a CVV mutant lacking the NSs and NSm genes (2delCVV) to replicate in intrathoracically injected Aedes albopictus was compared with the parental wild-type CVV (wtCVV) 6V633 strain. In contrast to the robust replication of wtCVV in injected mosquitoes, the multiplication kinetics of the 2delCVV mutant was reduced by more than a 100-fold.
Conclusion:
These results suggest that the deletion of NSm and NSs genes is a feasible approach to rationally design candidate orthobunyavirus LAVs that are highly attenuated in mosquitoes and, therefore, pose little risk of reversion to virulence and transmission.
Keywords: Cache Valley virus, live-attenuated vaccine, Aedes albopictus
Introduction
The Orthobunyavirus genus contains several human and animal pathogens. One emerging virus in this genera is Cache Valley virus (CVV), which is a zoonotic orthobunyavirus that causes abortions and teratogenic effects in large animals and rare but severe encephalitis in humans (Campbell et al, 2006; Nguyen et al, 2013; Sexton et al, 1997; Wilson et al, 2017; Yang et al, 2018). CVV has been isolated from several mosquito species and animals such as Aedes, Anopheles, Coquillettidia, Culiseta, Ochlerotatus, and Psorophora (Andreadis et al, 2014; Yang et al, 2018) and cattle, sheep, and caribou (Calisher et al 1986). Serological evidence of potential infections has also been found in horse, elk, and white-tailed deer (Calisher et al, 1986).
Although CVV has caused significant agroeconomic losses, no research has truly investigated the economic burden from the disease (Lopez et al, 2021). Currently, there are no licensed vaccines commercially available for the control of CVV in animals or humans. As observed with several viral diseases, live-attenuated vaccines (LAVs) are the most effective tool for disease control (Davis et al, 2019). This is because many LAVs can potentially elicit a long-lasting protective immunity with one single immunization such as the yellow fever (YF) 17D LAV (Collins and Barrett, 2017).
A live-attenuated candidate vaccine for CVV was evaluated in this study to not only aid in the event of an outbreak but also to advance our knowledge in vaccine development for other related bunyaviruses. Because all orthobunyaviruses are evolutionarily related and possess common motifs encoded by shared sequences, the attenuation process of CVV caused by genetic deletions can be a proof of concept for the development of candidate LAV for other related viruses such as La Crosse virus. The gene deletions are hypothesized to attenuate the virulence phenotype of CVV, thus restricting the vaccine viruses' ability to replicate in mosquitoes.
Most live-attenuated arbovirus vaccines with excellent safety profiles have been shown to lose the ability to infect and replicate in mosquitoes to prevent the possible transmission due to the deployment of LAVs in the field (Monath et al, 2020). For example, two highly effective LAVs for arboviruses, YF 17D vaccine and Japanese encephalitis SA14-14-2 vaccine, are unable to replicate and disseminate in mosquitoes (Chen and Beaty, 1982; Danet et al, 2019). In contrast, vaccine strains that did not reach a safe level of attenuation can often infect, multiply, and disseminate in mosquitoes.
One example of this was the Venezuelan equine encephalitis virus LAV TC-83, which is capable of infecting biting mosquitoes after equine vaccination (Pedersen et al, 1972). Similarly, the partially attenuated Rift Valley fever virus (RVFV) Smithburn LAV was transmitted by Culex pipiens and caused outbreaks in Egypt, which demonstrates the risk for vaccine viruses to mutate and ultimately revert to the virulence phenotype (Ahmed Kamal, 2011; Kamal et al, 2018).
The attenuated phenotype of LAVs for flaviviruses and alphaviruses in mosquitoes has been investigated in multiple systems (Davis et al, 2022; Gorchakov et al, 2012; Kaiser et al, 2019a; Kaiser et al, 2019b; McElroy et al, 2008; McElroy et al, 2006; McElroy et al, 2005; Plante et al, 2015; Rossi et al, 2020; Wang et al, 2017), whereas there is a major gap in knowledge of the attenuation process of bunyaviruses in mosquitoes. Specific genetic loci that govern the infection process of bunyaviruses across multiple genera are not well understood, warranting the investigation of the attenuated phenotype of CVV caused by the simultaneous deletion of the NSs and NSm genes.
To date, the virulence phenotype of multiple orthobunyaviruses, including Bunyamwera virus (BUNV) and Schmallenberg virus (SBV), has been attenuated by the deliberate removal of virulence factors in the viral genome (Kraatz et al, 2015; Szemiel et al, 2012). The orthobunyavirus genome consists of three negative-sense RNA segments, small (S), medium (M), and large (L), which code for various structural and nonstructural (NS) proteins (Hughes et al, 2020). Orthobunyaviruses have two known virulence factors, the NSs gene encoded in the S segment and the NSm gene encoded in the M segment (Elliott, 2014).
Deletion of either virulence factor was previously sufficient for virulence attenuation, as demonstrated with BUNV, the prototype orthobunyavirus (Bridgen et al, 2001; Szemiel et al, 2012). The simultaneous deletion of NSs and NSm genes fully attenuated the virulence phenotype of SBV, an emerging orthobunyavirus, in immunocompromised mice (Kraatz et al, 2015). In addition, in a previous study, we demonstrated that sheep inoculated with the candidate vaccine 2delCVV, lacking the NSs and NSm genes, developed a robust neutralizing antibody response with titers that would likely protect them from infection with wild-type CVV (wtCVV) (Ayers et al, 2022).
Previously, Seligman and Gould (2004) raised concerns regarding the potential for arbovirus LAVs to infect mosquitoes. Herein, we determine the capacity of a candidate CVV LAV strain that lacks the virulence factor NSs and NSm genes (2delCVV) to replicate in mosquitoes as compared with the CVV 6V633 wild-type strain. In a previous study, CVV did not require NSs to support replication in mosquito cell lines Aag2, similar to the deletion of NSm in Oropouche virus; therefore, attenuation of CVV in mosquitoes may be possible through the simultaneous deletion of NSs and NSm (Dunlop et al, 2018; Tilston-Lunel et al, 2015). The deletion of the virulence factors has also reduced the ability of RVFV to enter, replicate, and disseminate from the midgut epithelial cells (Kading et al, 2014). In addition, the attenuated phenotype of BUNV NSs deletion mutant has also included the reduced multiplication kinetics in infected mosquitoes (Szemiel et al, 2012).
We have previously shown that Aedes (Ae.) albopictus and Culex (Cx.) tarsalis are competent vectors for CVV (Ayers et al, 2019; Ayers et al, 2018). Ae. albopictus has a broader geographic distribution throughout North America and has recently been found to be infected with CVV in New York State, potentially indicating a northeastern U.S. expansion in the range of this virus (Dieme et al, 2022; Kamal et al, 2018).
Therefore, Ae. albopictus mosquitoes are considered an important vector for the endemic transmission of CVV and an appropriate model system to study the attenuating effect caused by the simultaneous deletion of NSs and NSm. Because the multiplication kinetics of 2delCVV is significantly reduced and does not reach the threshold infectivity required for mosquito per os infection (data not shown), Ae. albopictus were intrathoracically inoculated with either CVV 6V633 or 2delCVV to investigate the replication kinetics by bypassing the viral entry process. Our results demonstrated that the double deletion mutant of CVV displayed an attenuated phenotype based on the lower multiplication kinetics when compared with the wild-type 6V633 CVV strain.
Materials and Methods
Cells and viruses
The prototype 6V633 strain of CVV, originally isolated from infected Culiseta inornata in Cache Valley, Utah, in 1956 (Holden and Hess, 1959), was used as the wild-type virus for the intrathoracic inoculation. The strain was obtained from the laboratory collection of Dr. Richard M. Elliot (Watret et al, 1985). In a previously published study, the sequences of all three genomic segments were determined (GenBank acc. nos. KX100133.1, KX100134.1, and KX100135.1) (Groseth et al, 2017). Virus stocks were propagated and titered in African green monkey kidney epithelial Vero 76 cells that were maintained in Leibovitz's L-15 media (Thermo Fisher Scientific, Waltham, MA) supplemented with 10% fetal bovine serum, 10% tryptose phosphate broth, penicillin/streptomycin, and l-glutamine (Ayers et al, 2019; Ayers et al, 2018; Huang et al, 2015). The 2delCVV candidate vaccine was created using the same methods as previously described (Ayers et al, 2022; Dunlop et al, 2018).
Mosquitoes and challenge
Intrathoracic injection of mosquitoes was performed with 7- to 10-day-old Ae. albopictus (F4), which were derived from eggs collected from the city of Trenton, Mercer County, NJ, in July 2016. Mosquitoes were reared at 28°C, relative humidity of 80%, and a 12 h light:12 h dark photoperiod.
For intrathoracic inoculation, mosquitoes were cold anesthetized and inoculated with ∼0.5 μL of either the CVV 6V633 strain or the 2delCVV strain, as previously described (Huang et al, 2020). The experimentally challenged mosquitoes were maintained at conditions as described earlier for 7 days. Up to three mosquitoes were collected after injection and titrated to confirm the presence of infectious viruses. Intrathoracically inoculated mosquitoes were then collected by mechanical aspiration at 7 days postinfection (dpi) for analysis.
Detection of infectious viruses
Infection status of each mosquito was determined by the detection of CVV using the tissue culture infectious dose 50% (TCID50)-based titration method with Vero76 cells, as previously described (Ayers et al, 2019; Higgs et al, 2006; Huang et al, 2015). Infectivity of mosquitoes was used to determine the infection rate and multiplication kinetics of the wtCVV 6V633 strain and the 2delCVV strain. Infection rates were then calculated using the percentage of infected mosquitoes among all mosquitoes tested at each time point. Growth kinetics of CVV in infected mosquitoes was determined based on the titers of CVV in the whole mosquitoes at 7 dpi.
Statistical analysis
The infection rate percentages were compared using chi-squared test with Yate's correction. Titers of infected mosquitoes were compared with Mann–Whitney rank sum test between the two groups with the infectious titers after non-normal distribution. All statistical analyses were conducted using GraphPad (San Diego, CA) and Excel software (Redmond, WA).
Results
As expected, intrathoracic injection with either the CVV 6V633 strain or the 2delCVV candidate vaccine led to the establishment of infection in Ae. albopictus. There was no significant difference in the infection rates produced by 2delCVV and the CVV 6V633 strain at 7 dpi (CVV 6V633: 83.1% [49/59] vs. 2delCVV: 97.5% [39/40], chi-squared test with Yates's correction: χ2 = 3.682, df = 1, p = 0.0550) (Table 1). Mosquitoes injected with the 2delCVV candidate vaccine had significantly lower infectivity at 7 dpi than mosquitoes infected with wtCVV (CVV 6V633: 6.0 log10TCID50/mL vs. 2delCVV [median titer]: 3.5 log10TCID50/mL; Mann–Whitney test: U = 75.5, p < 0.0010) (Fig. 1). In conclusion, the deletion of NSs and NSm genes significantly reduces the multiplication kinetics of CVV in mosquitoes.
Table 1.
Comparison of Infection Rates in Aedes albopictus Mosquitoes Intrathoracically Injected with CVV 6V633 or 2delCVV
| Group | Mosquitoes tested | 7 dpi |
|---|---|---|
| CVV-6V633 | 59 | 83.1% (49/59) |
| 2delCVV | 40 | 97.5% (39/40) |
CVV, Cache Valley virus; dpi, days postinfection.
FIG. 1.
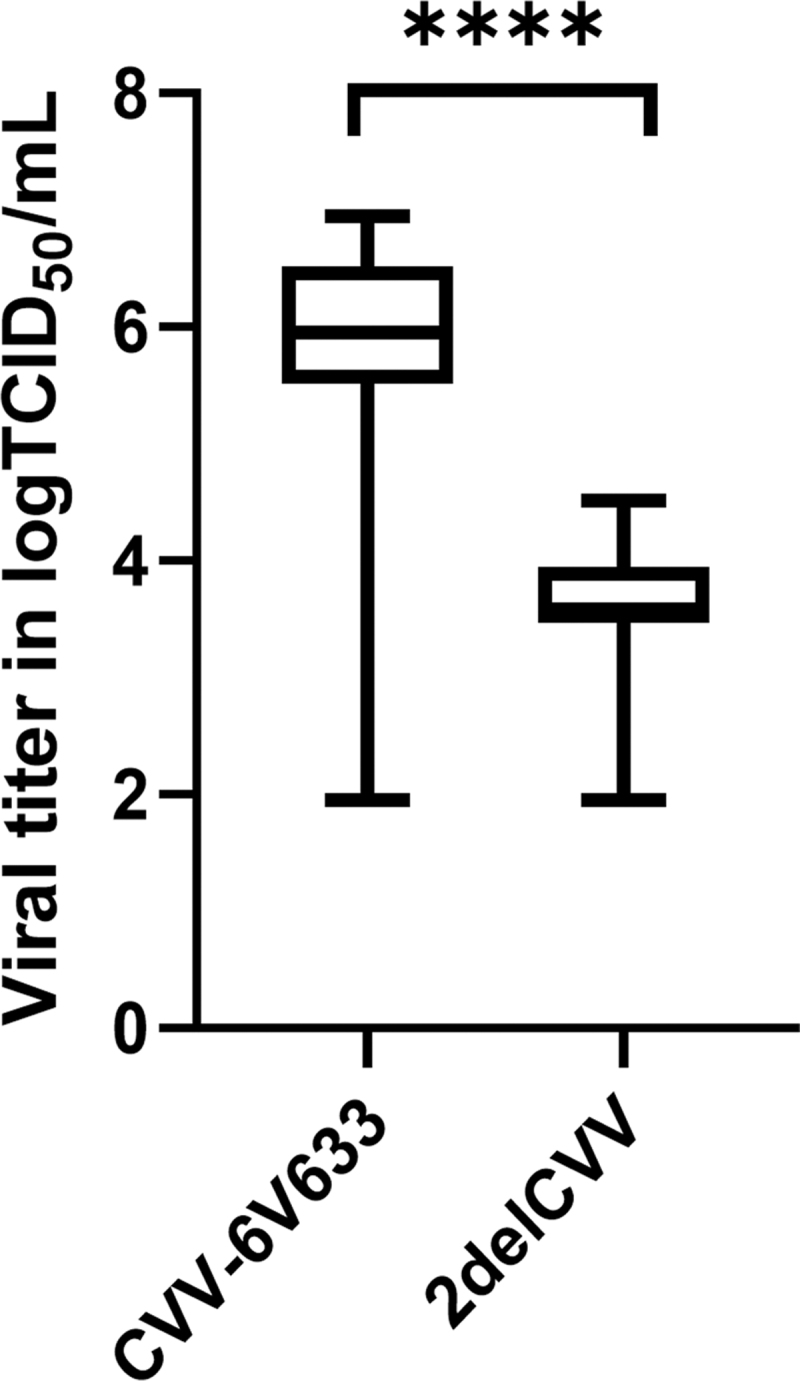
Titers of CVV in Aedes albopictus at 7 dpi. A Mann–Whitney test was used to compare the viral titers between the two groups of mosquitoes (****p < 0.001). The maximum and minimum values are displayed by the vertical lines connecting the largest and smallest viral titer in the data set. The horizontal bar represents the median titer of whole mosquitoes. CVV, Cache Valley virus; dpi, days postinfection.
Discussion
The development of safe and immunogenic LAVs for emerging bunyaviruses with minimal potential to revert to the virulence phenotype has become a priority for human and animal health in multiple geographic regions. It is also important that the bunyavirus LAVs exhibit reduced infection, dissemination, and multiplication kinetics in mosquitoes, preventing mosquitoes from transmitting vaccine viruses to livestock or humans. Data generated in this study demonstrated that the 2delCVV vaccine candidate was restricted in its replication in intrathoracically inoculated Ae. albopictus compared with the CVV 6V633 wild-type strain.
Along with the reduced multiplication kinetics of the 2delCVV strain in the vertebrate host SFT-R cells (Dunlop et al, 2018), this candidate CVV LAV has a lower potential of transmission by mosquitoes, similar to the attenuated phenotype of the YF 17D vaccine strain in Ae. aegypti. It is important to note that the simultaneous deletion of NSs and NSm genes has been proven to significantly impair the multiplication kinetics of CVV and related orthobunyaviruses in vertebrate hosts (Bridgen et al, 2001; Kraatz et al, 2015). The likelihood of 2delCVV to multiply to high viremic titers is low.
The low multiplication kinetics of 2delCVV in mosquitoes observed in this study further suggests the utility of the 2delCVV mutant as a candidate vaccine. In the unlikely but possible event that a mosquito acquires viremic bloodmeal containing the 2delCVV in nature, the low multiplication kinetics will limit the dissemination and minimize the likelihood of transmission. In addition, the yield of progeny virions is low and consequently can further reduce the risk of reassortment between the 2delCVV and wtCVV.
Although the YF 17D vaccine was able to infect mosquitoes, it was unable to disseminate to the secondary tissues and failed to transmit to a novel host (Danet et al, 2019). This suggests that the midgut escape barrier and the midgut infection barrier restrict this LAV from replication and transmission. Similarly, Ae. aegypti and Ae. albopictus were orally challenged with ChimeriVax vaccine candidates and resulted in such low titers that it would be unlikely for these mosquitoes to facilitate transmission (Higgs et al, 2006). Restriction of 2delCVV was observed in this study.
But the detailed mechanism(s) of attenuation remains undefined. The most plausible hypothesis is that the simultaneous deletion of NSs and NSm interferes with the virus–vector interactions required for multiplication of CVV after the establishment of infection in mosquitoes. Furthermore, it is unlikely that the 2delCVV mutant is defective in the cell entry process because the 2delCVV mutant has the same coding sequence for the two structural proteins and showed no demonstrable difference in the infection rate compared with the parental wild-type 6V633 strain.
The findings in this study also suggest the NSs and NSm genes are necessary for efficient growth in Aedes species mosquitoes. The specific role of NSs and NSm in mosquitoes still needs to be defined since NSs is not essential for viral growth in cell culture and NSm has been hypothesized to be dispensable for virus replication in mosquito cell lines (Elliott, 2014; Tilston-Lunel et al, 2015). Although unnecessary for viral growth in cell lines, the presence of these genes suggest they are necessary to overcome the cellular defenses in the midgut. In a previous study, the deletion of NSs in BUNV was unable to bypass the cellular defenses; however, when these barriers were overcome the vaccine viruses were capable of spreading to the secondary tissues and salivary glands (Szemiel et al, 2012).
More recently, a human vaccine candidate for RVFV lacking the NSm gene was unable to infect, replicate, or be transmitted by multiple mosquito species (Campbell et al, 2022). Therefore, the NSs and NSm genes appear to be required for the efficient replication of bunyaviruses in mosquitoes. In conclusion, 2delCVV exhibited an attenuated phenotype in mosquitoes through the reduced replication kinetics observed when compared with the wild-type strain and this attenuated phenotype reflects the functions of the NSs and NSm genes.
Acknowledgments
Thank you to Susan M. Hettenbach for her administrative support. Research was conducted in the ACL-3 Insectary of Kansas State University's Biosecurity Research Institute at Pat Roberts Hall. This study was in part based on research performed for Victoria Ayers's 2022 doctoral degree from Kansas State University.
Authors' Contributions
Investigation and writing—original draft by V.B.A. Investigation and writing—review and editing by Y.-J.S.H. Validation, resources, and writing—review and editing by J.I.D., A.K., and B.B. Conceptualization, funding acquisition, and writing—review and editing by S.H. and D.L.V.
Author Disclosure Statement
S.H. is editor of Vector-Borne and Zoonotic Diseases. All other authors have no competing financial interests.
Funding Information
This study was supported by the National Institute of Food and Agriculture, U.S. Department of Agriculture (award number 2015-67015-22961; S.H.) and by the UK Biotechnology and Biological Sciences Research Council (award number BB/M027112/1; A.K.) as part of the joint NIFA-BBSRC Animal Health and Disease program. This study was also supported by the UK Medical Research Council (MC_UU_12014/8; A.K.). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the article.
References
- Ahmed Kamal S. Observations on Rift Valley fever virus and vaccines in Egypt. Virol J 2011;8:532; doi: 10.1186/1743-422X-8-532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreadis TG, Armstrong PM, Anderson JF, et al. Spatial-temporal analysis of Cache Valley virus (Bunyaviridae: Orthobunyavirus) infection in anopheline and culicine mosquitoes (Diptera: Culicidae) in the northeastern United States, 1997–2012. Vector Borne Zoonotic Dis 2014;14(10):763–773; doi: 10.1089/vbz.2014.1669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers VB, Huang YS, Lyons AC, et al. Culex tarsalis is a competent vector species for Cache Valley virus. Parasit Vectors 2018;11(1):519; doi: 10.1186/s13071-018-3103-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers VB, Huang YS, Lyons AC, et al. Infection and transmission of Cache Valley virus by Aedes albopictus and Aedes aegypti mosquitoes. Parasit Vectors 2019;12(1):384; doi: 10.1186/s13071-019-3643-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers VB, Huang YS, Kohl A, et al. Comparison of immunogenicity between a candidate live attenuated vaccine and an inactivated vaccine for cache valley virus. Viral Immunology 2022. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridgen A, Weber F, Fazakerley JK, et al. Bunyamwera bunyavirus nonstructural protein NSs is a nonessential gene product that contributes to viral pathogenesis. Proc Natl Acad Sci U S A 2001;98(2):664–669; doi: 10.1073/pnas.98.2.664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calisher CH, Francy DB, Smith GC, et al. Distribution of Bunyamwera serogroup viruses in North America, 1956–1984. Am J Trop Med Hyg 1986;35(2):429–443. [DOI] [PubMed] [Google Scholar]
- Campbell CL, Snell TK, Bennett S, et al. Safety study of Rift Valley Fever human vaccine candidate (DDVax) in mosquitoes. Transbound Emerg Dis 2022;69(5):2621–2633; doi: 10.1111/tbed.14415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell GL, Mataczynski JD, Reisdorf ES, et al. Second human case of Cache Valley virus disease. Emerg Infect Dis 2006;12(5):854–856; doi: 10.3201/eid1205.051625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen BQ, Beaty BJ. Japanese encephalitis vaccine (2–8 strain) and parent (SA 14 strain) viruses in Culex tritaeniorhynchus mosquitoes. Am J Trop Med Hyg 1982;31(2):403–407; doi: 10.4269/ajtmh.1982.31.403 [DOI] [PubMed] [Google Scholar]
- Collins ND, Barrett AD. Live attenuated yellow fever 17D vaccine: A legacy vaccine still controlling outbreaks in modern day. Curr Infect Dis Rep 2017;19(3):14; doi: 10.1007/s11908-017-0566-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danet L, Beauclair G, Berthet M, et al. Midgut barriers prevent the replication and dissemination of the yellow fever vaccine in Aedes aegypti. PLoS Negl Trop Dis 2019;13(8):e0007299; doi: 10.1371/journal.pntd.0007299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis EH, Beck AS, Strother AE, et al. Attenuation of live-attenuated yellow fever 17D vaccine virus is localized to a high-fidelity replication complex. mBio 2019;10(5):e02294; doi: 10.1128/mBio.02294-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis EH, Wang B, White M, et al. Impact of yellow fever virus envelope protein on wild-type and vaccine epitopes and tissue tropism. NPJ Vaccines 2022;7(1):39; doi: 10.1038/s41541-022-00460-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dieme C, Maffei JG, Diarra M, et al. Aedes albopictus and Cache Valley virus: A new threat for virus transmission in New York State. Emerg Microbes Infect 2022;11(1):741–748; doi: 10.1080/22221751.2022.2044733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop JI, Szemiel AM, Navarro A, et al. Development of reverse genetics systems and investigation of host response antagonism and reassortment potential for Cache Valley and Kairi viruses, two emerging orthobunyaviruses of the Americas. PLoS Negl Trop Dis 2018;12(10):e0006884; doi: 10.1371/journal.pntd.0006884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott RM. Orthobunyaviruses: Recent genetic and structural insights. Nat Rev Microbiol 2014;12(10):673–685; doi: 10.1038/nrmicro3332 [DOI] [PubMed] [Google Scholar]
- Gorchakov R, Wang E, Leal G, et al. Attenuation of Chikungunya virus vaccine strain 181/clone 25 is determined by two amino acid substitutions in the E2 envelope glycoprotein. J Virol 2012;86(11):6084–6096; doi: 10.1128/JVI.06449-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groseth A, Vine V, Weisend C, et al. Maguari virus associated with human disease. Emerg Infect Dis 2017;23(8):1325–1331; doi: 10.3201/eid2308.161254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgs S, Vanlandingham DL, Klingler KA, et al. Growth characteristics of ChimeriVax-Den vaccine viruses in Aedes aegypti and Aedes albopictus from Thailand. Am J Trop Med Hyg 2006;75(5):986–993. [PubMed] [Google Scholar]
- Holden P, Hess AD. Cache Valley virus, a previously undescribed mosquito-borne agent. Science 1959;130(3383):1187–1188. [DOI] [PubMed] [Google Scholar]
- Huang YJ, Harbin JN, Hettenbach SM, et al. Susceptibility of a North American Culex quinquefasciatus to Japanese encephalitis virus. Vector Borne Zoonotic Dis 2015;15(11):709–711; doi: 10.1089/vbz.2015.1821 [DOI] [PubMed] [Google Scholar]
- Huang YS, Vanlandingham DL, Bilyeu AN, et al. SARS-CoV-2 failure to infect or replicate in mosquitoes: An extreme challenge. Sci Rep 2020;10(1):11915; doi: 10.1038/s41598-020-68882-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes HR, Adkins S, Alkhovskiy S, et al. ICTV virus taxonomy profile: Peribunyaviridae. J Gen Virol 2020;101(1):1–2; doi: 10.1099/jgv.0.001365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kading RC, Crabtree MB, Bird BH, et al. Deletion of the NSm virulence gene of Rift Valley fever virus inhibits virus replication in and dissemination from the midgut of Aedes aegypti mosquitoes. PLoS Negl Trop Dis 2014;8(2):e2670; doi: 10.1371/journal.pntd.0002670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser JA, Luo H, Widen SG, et al. Genotypic and phenotypic characterization of West Nile virus NS5 methyltransferase mutants. Vaccine 2019a;37(48):7155–7164; doi: 10.1016/j.vaccine.2019.09.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser JA, Luo H, Widen SG, et al. Japanese encephalitis vaccine-specific envelope protein E138K mutation does not attenuate virulence of West Nile virus. NPJ Vaccines 2019b;4:50; doi: 10.1038/s41541-019-0146-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamal M, Kenawy MA, Rady MH, et al. Mapping the global potential distributions of two arboviral vectors Aedes aegypti and Ae. albopictus under changing climate. PLoS One 2018;13(12):e0210122; doi: 10.1371/journal.pone.0210122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraatz F, Wernike K, Hechinger S, et al. Deletion mutants of Schmallenberg virus are avirulent and protect from virus challenge. J Virol 2015;89(3):1825–1837; doi: 10.1128/jvi.02729-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez K, Wilson SN, Coutermash-Ott S, et al. Novel murine models for studying Cache Valley virus pathogenesis and in utero transmission. Emerg Microbes Infect 2021;10(1):1649–1659; doi: 10.1080/22221751.2021.1965497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy KL, Girard YA, McGee CE, et al. Characterization of the antigen distribution and tissue tropisms of three phenotypically distinct yellow fever virus variants in orally infected Aedes aegypti mosquitoes. Vector Borne Zoonotic Dis 2008;8(5):675–687; doi: 10.1089/vbz.2007.0269 [DOI] [PubMed] [Google Scholar]
- McElroy KL, Tsetsarkin KA, Vanlandingham DL, et al. Characterization of an infectious clone of the wild-type yellow fever virus Asibi strain that is able to infect and disseminate in mosquitoes. J Gen Virol 2005;86(Pt 6):1747–1751; doi: 10.1099/vir.0.80746-0 [DOI] [PubMed] [Google Scholar]
- McElroy KL, Tsetsarkin KA, Vanlandingham DL, et al. Role of the yellow fever virus structural protein genes in viral dissemination from the Aedes aegypti mosquito midgut. J Gen Virol 2006;87(Pt 10):2993–3001; doi: 10.1099/vir.0.82023-0 [DOI] [PubMed] [Google Scholar]
- Monath TP, Kortekaas J, Watts DM, et al. Theoretical risk of genetic reassortment should not impede development of live, attenuated Rift Valley fever (RVF) vaccines commentary on the draft WHO RVF Target Product Profile. Vaccine 2020;5:100060; doi: 10.1016/j.jvacx.2020.100060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen NL, Zhao G, Hull R, et al. Cache Valley virus in a patient diagnosed with aseptic meningitis. J Clin Microbiol 2013;51(6):1966–1969; doi: 10.1128/jcm.00252-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen CE Jr., Robinson DM, Cole FE Jr. Isolation of the vaccine strain of Venezuelan equine encephalomyelitis virus from mosquitoes in Louisiana. Am J Epidemiol 1972;95(5):490–496; doi: 10.1093/oxfordjournals.aje.a121416 [DOI] [PubMed] [Google Scholar]
- Plante KS, Rossi SL, Bergren NA, et al. Extended preclinical safety, efficacy and stability testing of a live-attenuated Chikungunya vaccine candidate. PLoS Negl Trop Dis 2015;9(9):e0004007; doi: 10.1371/journal.pntd.0004007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi SL, Russell-Lodrigue KE, Plante KS, et al. Rationally attenuated vaccines for Venezuelan equine encephalitis protect against epidemic strains with a single dose. Vaccines (Basel) 2020;8(3):497; doi: 10.3390/vaccines8030497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman SJ, Gould EA. Live flavivirus vaccines: Reasons for caution. Lancet 2004;363(9426):2073–2075; doi: 10.1016/S0140-6736(04)16459-3 [DOI] [PubMed] [Google Scholar]
- Sexton DJ, Rollin PE, Breitschwerdt EB, et al. Life-threatening Cache Valley virus infection. N Engl J Med 1997;336(8):547–549; doi: 10.1056/nejm199702203360804 [DOI] [PubMed] [Google Scholar]
- Szemiel AM, Failloux AB, Elliott RM. Role of Bunyamwera Orthobunyavirus NSs protein in infection of mosquito cells. PLoS Negl Trop Dis 2012;6(9):e1823; doi: 10.1371/journal.pntd.0001823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilston-Lunel NL, Acrani GO, Randall RE, et al. Generation of recombinant Oropouche viruses lacking the nonstructural protein NSm or NSs. J Virol 2015;90(5):2616–2627; doi: 10.1128/JVI.02849-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Li SH, Zhu L, et al. Near-atomic structure of Japanese encephalitis virus reveals critical determinants of virulence and stability. Nat Commun 2017;8(1):14; doi: 10.1038/s41467-017-00024-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watret GE, Pringle CR, Elliott RM. Synthesis of bunyavirus-specific proteins in a continuous cell line (XTC-2) derived from Xenopus laevis. J Gen Virol 1985;66 (Pt 3):473–482; doi: 10.1099/0022-1317-66-3-473 [DOI] [PubMed] [Google Scholar]
- Wilson MR, Suan D, Duggins A, et al. A novel cause of chronic viral meningoencephalitis: Cache Valley virus. Ann Neurol 2017;82(1):105–114; doi: 10.1002/ana.24982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Qiu J, Snyder-Keller A, et al. Fatal Cache Valley virus meningoencephalitis associated with rituximab maintenance therapy. Am J Hematol 2018;93(4):590–594; doi: 10.1002/ajh.25024 [DOI] [PMC free article] [PubMed] [Google Scholar]


