Abstract
Background: COVID-19 pandemic imposes a substantial medical and socioeconomic burden on health systems. The study aimed to estimate the direct inpatient costs of COVID-19 in Iran.
Methods: This is a Cost of Illness (COI) study with the bottom-up method. Provider perspective and prevalence approach were applied for cost identification. Data included inpatient charges and clinical characteristics of all COVID-19 cases (2015 patients) admitted to a teaching hospital during a financial year (March 2020 to February 2021). We extracted data from Hospital Information System (HIS) and applied the quantile regression to estimate determinant factors of COVID-19 inpatient cost using STATA software.
Results: 1026 (50.92%) of admitted COVID-19 patients were female, and 42.3% were older than 65 years. More than 82% of discharged COVID-19 patients in this study recovered. 189 (9.38%) patients admitted to ICUs. Length of Stay (LOS) for about 70% of admitted COVID-19 cases was 7 days or less. The Total Inpatient Charges (TIC) was 155,372,056,826 Rials (5,041,836 PPP USD). The median charge was 42,410,477 Rials, and Average Inpatient Charges (AIC) was 77,107,720±110,051,702 (2,461 PPP USD) per person. Drugs and supplies accounted for 37% of total inpatient charges. Basic insurance companies would pay more than 79% of total claims and the share of Out-of-Pocket Payments (OOP) was 7%. ICUs admission and LOS of more than 3 days are associated with higher costs across all percentiles of the cost distribution (p<0.001).
Conclusion: This study call attention to the substantial economic burden based on real-world data. According to the broad socio-economic impacts of COVID-19 and also multiple components of COI study designs, conducting meta-analysis approaches is needed to combine results from independent studies.
Keywords: Hospital Economics, Hospital Costs, Cost of illnesses
Introduction
↑What is “already known” in this topic:
• COVID-19 as a recent global health threatening condition imposes socioeconomic burden to health systems.
→What this article adds:
• This study call attention to substantial economic burden of COVID-19 based on the real-world data.
• The study findings would inform policy makers for appropriate resources allocation to provide accessible and affordable health services.
COVID-19 pandemic, a global thread for human life, afflicted millions of people one year after its abrupt beginning around the world (1,2). The first confirmed case of COVID-19 in Iran was reported in Feb 2020 (3) and after that, the Iranian health system applied national and local quarantine, mass media education, rapid screening and diagnostic tests and equipped hospital settings for prevention and treatment of confirmed cases. These broad strategies are required to mobilize human resources, reallocate financial resources and fund healthcare facilities against COVID-19 limitations. Analysis of real-world data about the impact of the COVID-19 pandemic on the health system’s functions and goals will help to inform policymakers for better management of resources.
The assessment of direct and indirect costs attributed to an illness would help health systems to determine economic burden, estimate budgets, conduct cost-effectiveness analysis and design financing and payment mechanisms such as Diagnosis Related Group (DRG) (4-7).
COI studies identify, measure, and value the direct, indirect and intangible cost of a disease or public health problem (7,9). The direct cost of a disease includes resources consumed for hospital inpatient and outpatient care, nursing home care, hospice care, rehabilitation care, specialists’ and other health professionals’ care, diagnostic tests, prescription drugs, and medical supplies (8,10). Inpatient cost gets a high share of health care expenditure for noncommunicable (11) and infectious conditions (12).
Study perspective in COI is vital and implies from whose lens we are looking at the cost of a condition. It determines the data that will be collected. Common perspectives for COI studies are government, insurer, provider, patients and societal perspectives. The societal perspective is comprehensive and includes all opportunity costs that an illness imposes on society (10).
COI studies for various respiratory diseases expanded over time. Trucchi et al. (13) in a retrospective study, tried to estimate the economic burden and hospital cost of influenza-like illness and lower respiratory tract infection in adults 50 or more years old in Italy over the six influenza epidemic seasons. They reported the mean cost of emergency hospitalization for Influenza-like illnesses and lower respiratory tract infections as €3353. Ghaffari Darab et al. (14) estimated both direct medical and indirect costs of treating COVID-19 from a societal perspective in Iran. Based on their results, COVID-19 cost about 28,240,025,968 Rials in a referral hospital from March to July 2020. Cleary et al., (15) assessed the cost-effectiveness of intensive care management for COVID-19 patients in South Africa.
Conducting COI studies for COVID-19 will provide findings for evidence-based resource allocation and compare components of health care cost. So, this study aimed to estimate the direct inpatient cost of COVID-19 in Iran.
Methods
Cost, Charges, and Payment in Hospital Costing
The concepts of cost, charge and payment are different but they may use wrongly as an alternative in hospital costing. Cost includes the value of resources a hospital consumes to provide a service. Charges are billed tariffs assigned by a hospital during service procedures. Payment is the money amounts that are paid by purchasers to the hospital (16). So, cost data indicate the provider’s perspective. Charge data are simply more accessible than cost data, and if tariffs are determined really (based on true cost), the charge would be a proxy for cost data in hospital financial administration. On the other side, payment data estimate the COI from the purchaser's perspective. Comparison of the magnitude of cost, charge and payment reported in some indicators such as cost-to-charge ratios and payment-to-charge ratios (16,17). We used charges data to estimate the direct inpatient cost of COVID-19 from the provider’s perspective in a teaching hospital.
Study setting and design
The total number of hospitals in Iran in 2019 was 1020, including 146,217 hospital beds. Based on annals of hospital information and statistics from the ministry of health and medical education, teaching hospitals accounted for 25% of Iranian hospitals and 45% of Iranian hospital beds (18). This is a Cost of Illness (COI) study with a bottom-up method conducted at Bohlool Hospital affiliated with Gonabad University Medical Sciences, east Iran. This teaching hospital has 256 active inpatient beds and departments for emergency care, surgery, internal medicine, intensive care, gynecology, midwifery and obstetrics care, ENT, pediatrics, orthopedics, urology, neurosurgery, operation room, hemodialysis, radiology, para-clinic examination, and outpatient clinics. This hospital serves as a referral treatment center and teaching field for medicine students. From the beginning of the COVID-19 epidemic in Iran in Feb 2020, this center provided national treatment protocol to admitted COVID-19 patients. To estimate resources allocated to the treatment management of COVID-19 in the teaching hospital, we designed a COI study with a prevalence-based approach.
Sampling and data collection
All 2015 clinical confirmed COVID-19 cases that were admitted to the Bohlool hospital in one financial year from March 2020 to February 2021 were entered into the study. Data were collected in a retrospective design from hospital medical records through HIS. The data included cost and financial information, demographic characteristic, medical services and curative procedures for admitted COVID-19 cases. We applied the provider’s perspective, so charge data were extracted from HIS over the first year after the COVID-19 pandemic.
Data management and analysis
Data were extracted from HIS, and primarily data management process and descriptive statistics analysis were done in Excel. Total Inpatient Cost (TIC) was calculated for each admitted COVID-19 case by summing up hoteling, nursing services, visit and consultation, drugs, laboratory test, x-ray, operation room and medical supplies and other items.
Average Inpatient Charges (AIC) estimated by:
We applied quantile regression analysis using Stata 13.0 (Stata Corporation, Texas, USA) to estimate the effects of determinant factors on COVID-19 inpatient expenditure across the multiple quantiles of the expenditure distribution. The quantile regression is less sensitive to outliers and suitable for work on the highly skewed distribution of the dependent variable. So, it is a good alternative when the main assumptions of linear regression are not satisfied (19,20). We used the case fatality rate to estimate the total admitted cases of COVID-19 in Iran. By multiplying the number of hospitalized cases by AIC, we estimated a national burden for total direct inpatient costs in Iran. For international comparisons, all estimated costs were adjusted to current international dollars based on the World Bank’s purchasing power parity (PPP) conversion factors (1 PPP$ = 31328.95 Rials) (21).
Results
Demographic and Hospitalization Characteristics Profile Of the 2015 patients studied, 1026 (50.92%) were female, and 42.3% of them were aged greater than 65 years. More than 82% of cases were discharged as healed. 189 (9.38) patients admitted to ICUs. LOS for About 78% of admitted COVID-19 cases was less than 8 days. Table 1 shows demographic chrematistics of 2015 COVID-19 cases admitted to the teaching hospital during a year and the distribution of inpatient charges for each factor variable.
Table 1. Distribution of COVID-19 inpatient costs for each factor variable (numbers in ten million Rials) .
| Variable | N (%) | COVID-19 inpatient costs | ||||
| Minimum | Median | Mean | Maximum | |||
| Age | 0-15 | 145 (7.20) | 0.753 | 1.948 | 3.776 | 52.752 |
| 15-45 | 468 (23.23) | 0.802 | 3.540 | 6.831 | 135.115 | |
| 45-65 | 548 (27.20) | 0.574 | 4.569 | 8.111 | 119.273 | |
| >65 | 854 (42.38) | 0.530 | 5.038 | 8.603 | 80.148 | |
| Gender | Male | 989 (49.08) | 0.530 | 4.361 | 7.925 | 135.115 |
| Female | 1026 (50.92) | 0.574 | 4.073 | 7.503 | 119.273 | |
| Discharge Types | Recovered | 1656 (82.35) | .574 | 3.847 | 5.966 | 135.115 |
| Transferred | 17 (0.85) | 1.557 | 5.263 | 7.788 | 27.801 | |
| DAMA | 85 (4.23) | .840 | 3.659 | 6.183 | 37.289 | |
| Death | 253 (12.58) | .530 | 12.682 | 19.731 | 119.273 | |
| ICU Services | Admitted | 189 (9.38) | .530 | 18.358 | 23.564 | 135.115 |
| Not Admitted | 1826 (90.62) | .574 | 3.891 | 6.069 | 124.831 | |
| LOS (Day) | 1 | 108 (5.36) | .574 | 1.556 | 1.883 | 9.872 |
| 2 | 227 (11.27) | .530 | 1.734 | 2.125 | 11.521 | |
| 3 | 266 (13.20) | 1.195 | 2.225 | 2.704 | 18.519 | |
| 4 | 246 (12.21) | .989 | 2.839 | 3.727 | 16.658 | |
| 5 | 224 (11.12) | 1.857 | 3.677 | 5.011 | 25.238 | |
| 6 | 196 (9.73) | 2.558 | 4.357 | 5.460 | 16.801 | |
| 7 | 148 (7.34) | 2.851 | 5.670 | 6.650 | 29.177 | |
| 8-14 | 440 (21.84) | 3.662 | 9.018 | 10.662 | 48.662 | |
| ≥15 | 160 (7.94) | 1.602 | 29.585 | 33.415 | 135.115 | |
| Total | 2015 (100) | .530 | 4.241 | 7.710 | 135.115 | |
aLOS: Length of Stay. bDAMA: Discharge Against Medical Advice
Direct Inpatient Cost
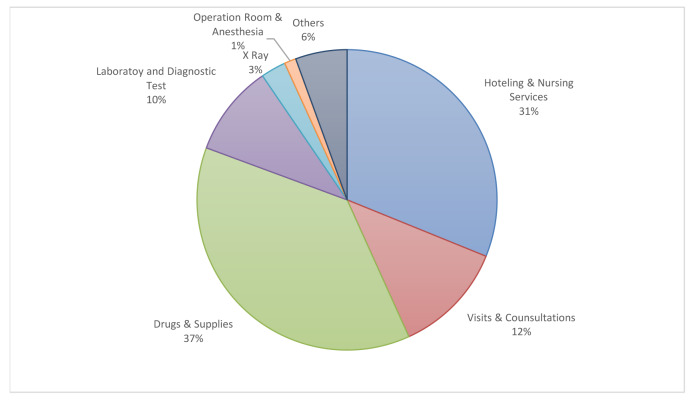
The TIC for 2015 admitted COVID-19 case was 155,372,056,826 Rials (4,959,376 PPP USD). The median cost was 42,410,477 Rials (1,354 PPP USD), and the mean (or AIC) was 77,107,720 (SD: 110,051,702) (2,461 PPP USD) per person. Drugs and supplies accounted for 37% of total inpatient charges. Figure 1 shows the proportion of each hospital cost items.
Fig. 1.
The proportion of inpatient cost items for COVID-19 in the teaching hospital
Financing Agents
The amount of money in hospital claims for the financing agent was 157,955,442,524 Rials (5,041,836 PPP USD). Major financing agent was basic insurance companies that would pay more than 79% of total claims. The share of OOP in the financing of COVID-19 inpatient charges was 7%. (Table 2).
Table 2. The effects (coefficient and 95% confidence interval) of determinants factors on COVID-19 inpatient expenditures across the 10th, 25th, 50th, 75th, and 90th quantile of the expenditure distribution. Effects are measured in ten million Rials .
| Variable | 10th, quantile | 25th, quantile | 50th, quantile | 75th, quantile | 90th, quantile |
| Intercept | 0.47 (0.05, 0.99) | 0.49 (-0.12, 1.11) | 0.96 (0.16, 1.75) * | 1.49 (-0.01, 2.99) | 2.26 (-0.03, 4.48) |
| Age (ref=16-45) | |||||
| 1-15 | -0.21 (-0.66, 0.23) | -0.23 (-0.76, 0.29) | -0.29 (-0.98, 0.38) | -0.62 (-1.91, 0.65) | -1.11 (-3.01,0.78) |
| 45-65 | 0.04 (-0.25, 0.33) | 0.04 (-0.31, 0.39) | 0.06 (-0.38, 0.52) | 0.12 (-0.72,0.98) | 0.02 (-1.29, 1.23) |
| >65 | 0.14 (-0.13, 0.42) | 0.10 (-0.22, 0.43) | 0.02 (-0.40, 0.45) | -0.24 (-1.05, 0.55) | -0.47(-1.66, 0.72) |
| Gender (ref=Male) | |||||
| Female | -0.004 (-0.20, 0.21) | -0.05 (-0.30, 0.18) | -0.14 (-0.46, 0.17) | -0.14(-0.74, 0.45) | -0.11 (-0.99, 0.76) |
| Discharge Type (ref=Recovered) | |||||
| Death | 0.93 (0.47, 1.36) ** | 1.22 (0.67, 1.76) ** | 1.16 (0.46, 1.85) ** | 1.28 (-0.02, 2.59) | 1.56 (-0.37, 3.50) |
| Transfer | 0.6 (-0.52, 1.77) | 0.69 (-0.66, 2.05) | 0.65 (-1.09, 2.41) | 1.03 (-2.26, 4.33) | 0.44(-4.44, 5.32) |
| DAMAb | 0.36 (-0.15, 0.89) | 0.54 (-.07, 1.16) | 0.41 (-0.38, 1.21) | 0.26 (-1.24, 1.76) | 0.65(-1.57, 2.88) |
| ICUs Admission (ref= Not admitted in ICUs) | |||||
| ICUs admitted | 1.40(0.90, 1.89) ** | 3.37 (2.78, 3.95) ** | 5.58 (4.83, 6.34) ** | 7.97 (6.55, 9.39) ** | 12.08 (9.98,14.17) ** |
| Co-Diagnosis (ref= Single Diagnosis-COVID-19) | |||||
| COVID-19 plus other diagnosis | 0.34 (-0.37, 0.72) | 0.76 (0.31, 1.21) * | 1.39 (0.80, 1.97) ** | 2.11(1.01, 3.21) ** | 4.02(2.39, 5.65) ** |
| LOS (ref= 1 day) | |||||
| 2 | 0.67(0.11,1.22) * | 0.83(0.17, 1.49) * | 0.67(-0.16, 1.52) | 0.64 (-0.95, 2.23) | 0.66 (-1.69, 3.02) |
| 3 | 1.16 (0.61, 1.71) ** | 1.38 (0.73, 2.02) ** | 1.24 (0.41, 2.08) * | 1.27 (-0.29, 2.84) | 1.61 (-0.71, 3.94) |
| 4 | 1.68 (1.13, 2.24) ** | 1.92 (1.27, 2.58) ** | 1.84 (1.00, 2.69) ** | 2.44 (0.84, 4.03) * | 4.36 (1.98, 6.74) ** |
| 5 | 2.14 (1.58, 2.71) ** | 2.56 (1.89, 3.23) ** | 2.63 (1.77, 3.49) ** | 5.29 (3.67, 6.90) ** | 5.80 (3.41, 8.20) ** |
| 6 | 2.67 (2.09, 3.24) ** | 3.05 (2.37, 3.73) ** | 3.31 (2.44, 4.19) ** | 4.71 (3.06, 6.36) ** | 6.14 (3.69, 8.59) ** |
| 7 | 3.02 (2.41, 3.62) ** | 3.70 (2.98, 4.41) ** | 4.48 (3.56, 5.40) ** | 6.56 (4.83, 8.30) ** | 7.69 (5.12, 10.26) ** |
| 8-14 | 4.42 (3.90, 4.93) ** | 5.37 (4.76, 5.98) ** | 7.73 (6.94, 8.52) ** | 9.89 (8.41, 11.37) ** | 12.71 (10.52, 14.90) ** |
| ≥15 | 11.10 (10.50, 11.70) ** | 16.48 (15.77, 17.19) ** | 24.15 (23.23, 25.06) ** | 34.45 (32.73, 36.17) ** | 46.30 (43.75, 48.84) ** |
aLOS: length of Stay. bDAMA: Discharge Against Medial Advice. *P-value < 0.05. **P-value < 0.001
Table 3 summarizes the coefficient estimates and 95% confidence intervals for each of the five determinant factors. Among five determinant factors, ICU admission and LOS of more than 3 days are associated with higher costs across all percentiles of the cost distribution. Co-diagnosis were linked to higher costs among high-cost patients and death outcome were linked to higher costs among low-cost patients.
Table 3. The share of financing agents for COVID-19 payment .
| Financing Agent | Payment (Rials) | Percent |
| Basic Insurance | 124,390,031,567 | 79 |
| Government Subsidy and Discount | 15,795,112,851 | 10 |
| Supplementary Insurance | 5,782,059,178 | 4 |
| Out of Pocket Payment | 11,988,238,928 | 7 |
| Total | 157,955,442,524 | 100 |
Discussion
The aim of the study was to determine the direct inpatient cost of COVID-19 in a teaching hospital and estimate a national burden for the Iranian health system. Based on demographic and hospitalization characteristics, 42.38% of the study population was aged above 65 years. 82.35% of COVID-19 cases admitted to the teaching hospital recovered and the case fatality rate was 12.58% (it means that from every 100 admitted cases, 12.58 people died). Baigi et al (22) explored the epidemiological characteristics of COVID-19 in a major hospital in Tehran, Iran. They estimated the case fatality rate as 12.5% and 9.8% for men and women respectively. A similar study of the United States in-hospital mortality reported 13.6% (23). These differences might be associated with different impacts of sequential waves of COVID-19 because there is a difference in the length of the study period between these studies. Conducting meta-analysis approaches is needed to combine results from independent studies.
In this study, about 30% of patients had LOS for more than 7 days. A review of past studies showed LOS for COVID-19 was associated with demographic and clinical factors and varied substantially between health settings and countries (24). Of 2015 hospital admitted cases, 9.38% were admitted to an ICU. Regarding the pressing demand for ICU services during the COVID-19 pandemic, effective management of ICU procedures from admission to discharge is essential. Sadeghi et al (25) reported that 25.7% of COVID-19 patients were admitted to ICU in a teaching hospital in Tehran. In the study of the economic burden of hospitalized COVID-19 patients in the United States (23), Di Fuscoa et al. reported that 21.9% of hospitalized cases were admitted to the ICU. In the comparison of COI studies conducted for COVID-19, we faced different study periods while treatment protocols have been varying over time, so different health service utilization indicators are possible.
The total TIC for 2015 hospital admitted COVID-19 case was 155,372,056,826 Rials (4,959,376 PPP USD). The median was 42,410,477 Rials (1,354PPP USD), and the mean (or AIC) was 77,107,720 (2,461 PPP USD). In a similar study in Iran (14), Ghafari Darab et al reported 59,203,409 Rials as the mean cost per person. Nakhaei et al (26) estimated the total direct and indirect cost for 745 hospitalized patients with COVID-19 in Vali-e-Asr Hospital affiliated with Birjand University of Medical Sciences, Iran from March 2020 to July 2020. They reported the mean of total direct cost (including hospitalization cost, outpatients cost and direct nonmedical cost) as 3362.49 PPP$. In the United States, median hospital charges and median hospital costs for hospitalized COVID-19 patients were reported at 43,986 and 12,046 respectively (23). Achonu et al. (27) reported the cost for controlling a SARS outbreak in a teaching hospital over an 8-week period as 12 million dollars in Canada. The study by A. Khan et al., (28) in Saudi Arabia estimated direct medical costs of hospitalized COVID-19 patients at 42,704.49 SAR in general wards and 79,418.30 for ICU admitted cases. They concluded the mean direct medical cost per COVID-19 patient was not significantly different from a MERS-CoV case but a high number of COVID-19 infections led to a larger amount of total direct medical cost of COVID-19. The comparison between costing results should be based on several components of COI design such as different perspectives, costing methods, cost types, etc.
In this study, drugs and supplies accounted for the biggest share (37%) of the total inpatient charge of COVID-19 in a teaching hospital. In the study conducted in Shiraz province (14), drugs included 28% of the direct medical cost for hospitalized COVID-19 cases. Cost-effective drug protocols will play a significant role in controlling health spending through treatment management of COVID-19 and other infectious diseases.
Universal Health Coverage (UHC) and other social protection plans emphasize low OOP for ensuring equitable access to medical care for all population groups (29,30). Also, the Price-demand elasticity in an emergency condition for medical care is low (31), so financial protection of patients against COVID-19 is a high priority (32). Furthermore, El-Khatib et al., (33) reported a positive association between high OOP and COVID-19 mortality. Our findings showed basic social insurance packages covered about 80% of the total payment for inpatient care for COVID-19 and the share of OOP was just 7% during the first year after the epidemic.
The quantile regression model indicated that ICUs admission and LOS of more than 3 days are associated with higher costs across all percentiles of the cost distribution. In a similar study in Iran (14), inpatient cost for COVID-19 cases in ICUs was four times greater than in other units. In a recent study in South Africa, Cleary et al. (15) conducted a cost‐effectiveness analysis of intensive care for hospitalized COVID-19 patients. In this study cost per admission of severe and critical COVID-19 patients in general wards was 75,127 ZAR and increased to 103,030 ZAR for patients who used ICUs. Taheri et al. (34) reviewed the cost-accounting records of all surviving patients discharged with LOS of 4 days or more from a university hospital in the United States. They concluded LOS has minimal impact on the cost of hospital admission.
This study encountered some limitations. We used charge data as a proxy for COVID-19 inpatient costs in a teaching hospital. Charges are formal tariffs assigned by a hospital to patients’ records. These tariffs may not depict the true cost incurred over the COVID-19 treatment. Also, some cost items such as cost for overhead departments and personnel protection equipment ignored in this study. Our study setting was one referral teaching hospital, for addressing this limitation, we chose a longer study time frame than other similar studies to capture diverse cases of several waves of COVID-19.
National burden of COVID-19 direct inpatient cost
We used the case fatality rate to estimate the total admitted cases of COVID-19 in Iran. The total number of COVID-19 death divided by the hospital case fatality rate. So, 595,840 hospitalized cases were estimated for 12 months in Iran (Table 4). After that, by multiplying the number of hospitalized cases by AIC, we estimated the total direct inpatient cost in Iran for 12 months would be about 1,466,498.682 PPP USD (equals 0.138 % of Iranian GDP).
Table 4. The burden of COVID-19 direct inpatient costs in Iran- 2020 .
| Indicators | |
| Total Population | 83,992,953* |
| Gross domestic product (PPP $)-constant 2017 | 1.062 (Tn)* |
| GDP per capita, PPP (constant 2017 international $) | 16,177* |
| Domestic general government health expenditure per capita, PPP (current international $) | 776.78 (2018) * |
| Current health expenditure per capita, PPP (current international $) | 1691(2018) * |
| Estimated number of COVID-19 hospitalized cases (12 months) | 595,840 |
| Estimated Direct Inpatients Cost of COVID-19 (PPP $)- Annual | 1,466,498,682 |
| Estimated Direct Inpatients Cost of COVID-19 (as % of GDP) | 0.138% |
*Resource: World bank, https://data.worldbank.org/country/iran-islamic-rep (Available: 23 Jan 2022) (34)
Conclusion
This study call attention to the recent global health-threatening condition in term of socioeconomic burden. The results indicated a substantial economic burden for COVID-19 based on real-world data. These findings would inform policymakers for appropriate resource allocation to provide accessible and affordable health services. According to the broad socio-economic impacts of COVID-19 and also multiple components of COI study designs, conducting meta-analysis approaches is needed to combine results from independent studies.
Abbreviation
COI: Cost of Illness; HIS: Hospital Information System; DAMA: Discharge Against Medial; Advice LOS: Length of Stay; TIC: Total Inpatient Charges; AIC: Average Inpatient Charges; OOP: Out-of-Pocket Payments; DRG: Diagnosis Related Group.
Ethics approval
We gained approval from the ethics committee of Gonabad University of Medical Science (ethical code: IR.GMU.REC.1398.186).
Acknowledgment
The social development and health promotion research center supported the study. The authors would like to acknowledge and thank the Clinical Research Development Unit of Bohlool hospital in Gonabad University of Medical Sciences for their contribution to this research. Special thanks to Azam Zanganeh at the information technology department of the hospital.
Conflict of Interests
The authors declare that they have no competing interests.
Cite this article as: Khandehroo M, Dorri M, Paykani T, Khajavi A, Joshani-Kheibari M, Esmaeili R. Direct Inpatient Cost and Payments of COVID-19 in Iran: Quantile Regression Analysis. Med J Islam Repub Iran. 2022 (3 Sep);36:101. https://doi.org/10.47176/mjiri.36.101
References
- 1.Nicole M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Losifidis C, et al. The socio-economic implications of the coronavirus and covid-19 pandemic: A review. Int J Surg. 2020;78:185–93. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Word Health Organization (WHO). Coronavirus disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update, 2021. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 3.Pourmalek F, Hemami MR, Janani L, Moradi-Lakeh M. Rapid review of COVID-19 epidemic estimation studies for Iran. BMC Public Health. 2021;21(1):1–30. doi: 10.1186/s12889-021-10183-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Durand-Zaleski I. Why cost-of-illness studies are important and inform policy. Vasc Med. 2008;13(3):251–3. doi: 10.1177/1358863X08091738. [DOI] [PubMed] [Google Scholar]
- 5.Ernst R. Indirect costs and cost-effectiveness analysis. Value Health. 2006;9(4):253–61. doi: 10.1111/j.1524-4733.2006.00114.x. [DOI] [PubMed] [Google Scholar]
- 6.Miners A. Estimating ‘costs’ for cost-effectiveness analysis. Pharmacoeconomics. 2008;26(9):745–51. doi: 10.2165/00019053-200826090-00005. [DOI] [PubMed] [Google Scholar]
- 7. Busse R, Geissler A, Aaviksoo A, Cots F, Häkkinen U, Kobel C, et al. Diagnosis related groups in Europe: moving towards transparency, efficiency, and quality in hospitals? BMJ 2013;346. [DOI] [PubMed]
- 8.Jo C. Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol. 2014;20(4):327. doi: 10.3350/cmh.2014.20.4.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Larg A, Moss JR. Cost-of-illness studies. Pharmacoeconomics. 2011;29(8):653–71. doi: 10.2165/11588380-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 10.Segel JE. Cost-of-illness studies—a primer. RTI-UNC center of excellence in health promotion economics. 2006;1:39. [Google Scholar]
- 11. Yin X, Xu Y, Man X, Liu L, Jiang Y, Zhao L, et al. Direct costs of both inpatient and outpatient care for all type cancers: the evidence from Beijing, China. Cancer Med. 2019 Jun;8(6):3250-60. [DOI] [PMC free article] [PubMed]
- 12.Arora V, Moriates C, Shah N. The challenge of understanding health care costs and charges. AMA J Ethics. 2015;17(11):1046–52. doi: 10.1001/journalofethics.2015.17.11.stas1-1511. [DOI] [PubMed] [Google Scholar]
- 13. Trucchi C, Paganino C, Orsi A, Amicizia D, Tisa V, Piazza MF, et al. Hospital and economic burden of influenza-like illness and lower respiratory tract infection in adults≥ 50 years-old. BMC Health Serv Res. 2019 Dec;19(1):1-1. [DOI] [PMC free article] [PubMed]
- 14.Darab MG, Keshavarz K, Sadeghi E, Shahmohamadi J, Kavosi Z. The economic burden of coronavirus disease 2019 (COVID-19): evidence from Iran. BMC Health Serv Res. 2021;21(1):1–7. doi: 10.1186/s12913-021-06126-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cleary SM, Wilkinson T, Tchuem CT, Docrat S, Solanki GC. Cost‐effectiveness of intensive care for hospitalized COVID-19 patients: experience from South Africa. BMC Health Serv Res. 2021 Dec;21(1):1-0. [DOI] [PMC free article] [PubMed]
- 16. Smith MW, Friedman B, Karaca Z, Wong HS. Predicting inpatient hospital payments in the United States: a retrospective analysis. BMC Health Serv Res. 2015 Jun;15(1):1-2. [DOI] [PMC free article] [PubMed]
- 17.Poorman GW, Horn SR, Bronson WH, Hasan S, Moon JY, Diebo BG, et al. Determinants of Cost-to-Charge Ratio Variation among US Hospitals. Spine J. 2017;17(10):S87. [Google Scholar]
- 18. Iranian ministery of Health and Medical Education, Annals of Hospital Information and Statistics. Tehran, 2019.
- 19. Madadizadeh F, Asar ME, Bahrampour A. Quantile regression and its key role in promoting medical research. Iran J Public Health. 2016 Jan;45(1):116. [PMC free article] [PubMed]
- 20. Howard, M. Comparison of the Performance of Simple Linear Regression and Quantile Regression with Non-Normal Data: A Simulation Study. (Doctoral dissertation) 2018. Retrieved from https://scholarcommons.sc.edu/etd/4517.
- 21. World bank. PPP conversion factor, GDP (LCU per international $) - Iran, Islamic Republic rates 2020. Available from: https://data.worldbank.org/indicator/PA.NUS.PPP?locations=IR. (23 Jan 2022).
- 22.Baigi V, Nedjat S, Yunesian M, Sari AA, Mirzaee M, Allameh SF. Clinical and Epidemiological Features of Hospitalized Patients with COVID-19 in Hospitals of Tehran University of Medical Sciences. Front Emerg Med. 2021;5(2):e20–e. [Google Scholar]
- 23.Di Fusco M, Shea KM, Lin J, Nguyen JL, Angulo FJ, Benigno M, et al. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J Med Eco. 2021;24(1):308–17. doi: 10.1080/13696998.2021.1886109. [DOI] [PubMed] [Google Scholar]
- 24.Rees EM, Nightingale ES, Jafari Y, Waterlow NR, Clifford S, Pearson CA, et al. COVID-19 length of hospital stay: a systematic review and data synthesis. BMC Med. 2020;18(1):1–22. doi: 10.1186/s12916-020-01726-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sadeghi A, Eslami P, Moghadam AD, Pirsalehi A, Shojaee S, Vahidi M, et al. COVID-19 and ICU admission associated predictive factors in Iranian patients. Caspian J Intern Med. 2020;11(Suppl 1):512. doi: 10.22088/cjim.11.0.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nakhaei K, Jalilian H, Arab-Zozani M, Heydari S, Torkzadeh L, Taji M. Direct and indirect cost of COVID-19 patients in Iran. Health Policy Technol. 2021 Dec 1;10(4):100572. doi: 10.1016/j.hlpt.2021.100572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Achonu C, Laporte A, Gardam MA. The financial impact of controlling a respiratory virus outbreak in a teaching hospital. Can J Public Health. 2005;96(1):52–4. doi: 10.1007/BF03404018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khan AA, AlRuthia Y, Balkhi B, Alghadeer SM, Temsah M-H, Althunayyan SM, et al. Survival and estimation of direct medical costs of hospitalized COVID-19 patients in the Kingdom of Saudi Arabia. Int J Environ Res Public Health. 2020;17(20):7458. doi: 10.3390/ijerph17207458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rim, J. and C. Tassot, "Towards universal social protection: Lessons from the universal health coverage initiative", OECD Development Policy Papers, No. 20, OECD Publishing, Paris, 2019.
- 30.Tediosi F, Lönnroth K, Pablos-Méndez A, Raviglione M. Build back stronger universal health coverage systems after the COVID-19 pandemic: the need for better governance and linkage with universal social protection. BMJ Glob Health. 2020;5(10):e004020. doi: 10.1136/bmjgh-2020-004020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ellis RP, Martins B, Zhu W. Health care demand elasticities by type of service. J Health Econ. 2017 Sep 1;55:232–43. doi: 10.1016/j.jhealeco.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang Z, Tang K. Combating COVID-19: health equity matters. Nat Med. 2020;26(4):458. doi: 10.1038/s41591-020-0823-6. [DOI] [PubMed] [Google Scholar]
- 33.El-Khatib Z, Otu A, Neogi U, Yaya S. The association between out-of-pocket expenditure and COVID-19 mortality Globally. J Epidemiol Glob Health. 2020;10(3):192. doi: 10.2991/jegh.k.200725.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Taheri PA, Butz DA, Greenfield LJ. Length of stay has minimal impact on the cost of hospital admission. J Am Coll Surg. 2000 Aug 1;191(2):123–30. doi: 10.1016/s1072-7515(00)00352-5. [DOI] [PubMed] [Google Scholar]