Abstract
Background: A review on the health information systems (HISs) of each country should not be limited only to data collected and reported normally by the service providers. In this regard, the first step for the development in any national project is exploring the experiences of other countries worldwide, especially those with economic, political, cultural, and regional partnerships, and then using their resources and documents to have a broader attitude and a better profitability in planning the development strategy. This study was conducted to review the studies conducted on the causes of HIS success and failure, and the challenges faced by developing countries in using these systems.
Methods: The present study was a narrative review to meet the aim of the study, and those studies published in English language in PubMed, Web of science, and Science Direct databases and Scopus between 2000 and 2020 were investigated. Primary keywords used to extract content in these databases were as follows: "health information system", "challenges", "success", "failure", "developing country", and "low and middle income country".
Results: After searching the above-mentioned databases, 455 studies were retrieved. Finally, 24 articles were used. The causes of success and failure of HISs were finally divided into 4 categories: human, organizational, financial and technical factors. A total of 30 subfactors were extracted for different factors. Moreover, the findings indicated that many of the challenges that developing countries face in using HISs are influenced by the social, cultural, economic, geographical, and political conditions of these countries. The results represented that organizational and human elements play a critical role in the advancement or falling of the health HIS in growing countries.
Conclusion: There is a demand to come up with flexible standards for designing and deploying HISs to address these complexities. Several solutions can be found to address the obstacles and problems facing HISs in developing countries, including formulating strategic plans and policies necessary for the development of national HISs.
Keywords: Information System, Health Information Systems, Developing Countries, Low and Middle Income Countries, Challenge, Success, Failure
Introduction
↑What is “already known” in this topic:
A review on the HISs of each country should not be limited only to data reported normally by the service providers. To achieve this goal, all components of the HIS, the causes of success and failure, and challenges of these systems, programs, and strategies should be noted.
→What this article adds:
There reasons for the failure of information systems, including a lack of specialized experienced human, financial resources and the lack of infrastructure. Solutions including formulating strategic developing laws on reporting diseases, collecting data from public-private sectors, determining information privacy and disclosure policies, and formulating maintenance and retention policies can used.
Since past years, the World Health Organization (WHO) has declared the health inform ation system (HIS) as a key pillar in achieving the goal of “health for all." The WHO report in 2010 had identified the improvement of management to be related to the improved information system (1,2). In addition, from the technical point of view, a system can be defined as a set of components associating with the collection, maintenance, and processing of the obtained data and published information to assist in the decision-making process and monitoring the organization. moreover, providing support on decision-making, coordination and monitoring can help managers and employees in analyzing issues, uncovering complicated matters, and creating new products (3).
In the health care system, HISs can be defined as the collected components and structured processes for producing information that would improve the decision-making process at all levels of the health system’s management. The ultimate goal of HIS is not only to obtain information, but also to improve health system performance (4,5). Accordingly, in the last decade, there have been extensive activities and innovations for the development of HISs due to the development of new technologies. Many organizations in both private and governmental sectors in developing and developed countries have resorted to HIMs to meet the increasing trend of demands on improving the efficiency and effectiveness of health services (6).
Most of the health service providers in developing countries provide their information systems with registration forms that include the patients’ name and address and the information related to their disease, which are completed weekly or monthly and then delivered without adequate feedback (7). In addition, the received data are not often useful for making decision on the management issue because they are incomplete, inaccurate, useless, and irrelevant to the priorities of the functions and the task lists of health staffs. In other words, information systems in these countries are data-based, rather than performance-based. Therefore, providing HISs in these countries is considered a barrier in management, instead of being a tool (8).
A review on the HISs of each country should not be limited only to data collected and reported normally by the service providers. On the other hand, the performance of the HIS should be considered in the quality dimensions of the produced data, and also the data should be used to improve the performance and the status of the health system. To achieve this goal, all components of the HIS;, the causes of success and failure, and challenges of these systems, programs, and strategies should be noted (9). In this regard, the first step for the development in any national project is exploring the experiences of other countries worldwide, especially those with economic, political, cultural, and regional partnerships, and then using their resources and documents to have a broader attitude and a better profitability in planning the development strategy. Therefore, the aim of this study is to explore the experiences of growing countries regarding the causes of success and failure of HISs, and the challenges faced by them in the use of HISs.
Methods
The present study was a narrative review. This research was performed in terms of the PRISMA (10) (Preferred Reporting Items for Systematic reviews and Meta-Analyses).
Search Strategy
To investigate problems and challenges of developing countries on the use of HISs and the causes of their success and failure in these countries, the related studies published in PubMed, Web of science, and Science Direct, and Scopus databases were investigated. Primary keywords used to extract content in these databases were as follows: "health information system", "challenges", "success", "failure", "developing country", and "low and middle income country". After extracting the primary keywords, the following synonyms terms were extracted (Table 1). Moreover, the following step was performed to combine these words and obtain the main keywords for searching the related material to HISs in developing countries. In addition, we have utilized Mesh terms as well as truncation, wildcard, and closeness operators to fortify the search.
Table 1. The main keywords and their subsets .
| Keywords | Synonyms |
| Health Information Systems | • Health Information System • Information System, Health • Information Systems, Health • System, Health Information • Systems, Health Information • Health Information System • Healthcare Information System • Health Information Systems • Healthcare Information Systems • Medical information system • Laboratory information system • Clinical information system • Pharmacy information system • Nursery information system • Electronic Health Record • Electronic Medical Record |
| Challenge | • Problem • Dispute • Obstacles |
| Failure | • Defeat • Setback • losing |
| Success | • Achievement • Prosperity • hit |
| Developing Countries | • Least Developed Countries • Less Developed Countries • Under Developed Nations • Third-World Countries • Third-World Nations • Under Developed Countries • Developing Nations • Less Developed Nations • Low and Middle income Countries |
Inclusion Criteria
The inclusion criteria were the articles published in English language from January 1, 2000 to June 1, 2020 that reported a problem or a challenge of HISs in developing countries as well as the causes of success and failure of HISs.
Exclusion Criteria
Studies without available full text were excluded from this study.
Study Selection
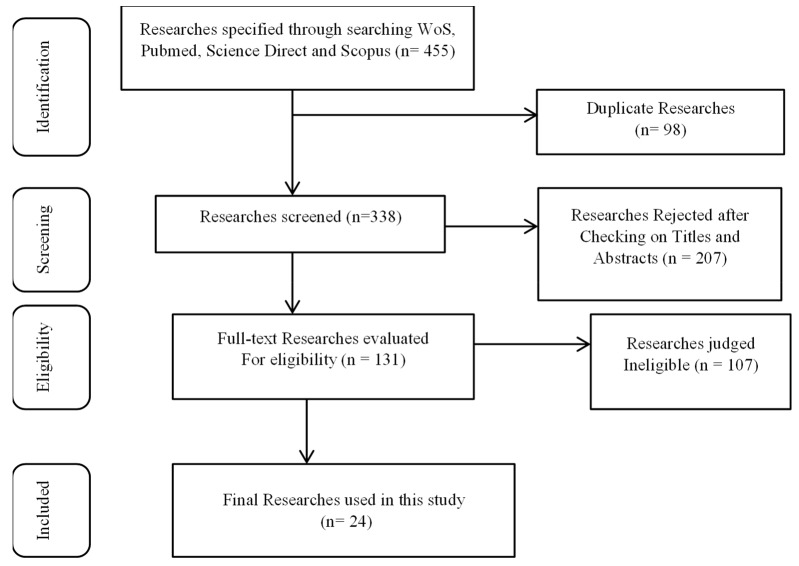
After removing duplicates, the researchers screened the titles and abstracts of the studies according to the inclusion/ exclusion criteria. The same researchers has then evaluated the full texts of potential related articles (Fig. 1).
Fig. 1.
Flowchart of studies selection
Results
After searching the above-mentioned databases, 455 studies were retrieved. Afterward, the duplicates were deleted and 338 articles remained. Based on their titles and abstracts, 131 articles were included, and after reading their full text, 24 studies were approved (Fig. 1). Of these, 5 studies (21%) have been conducted in 2015. Also, 12 studies (50%) were conducted in Asian countries and 6 studies (25%) in African countries. Notably, 6 studies (25%) were review articles, and 7 studies (29%) have focused on the HIS (Table 2).
Table 2. HISs challenge and causes of failure and success extracted from selected studies .
| Author | Year | Place | Type of research | Type of information system | Challenge and Causes of Failure | Causes of success |
| Sahay (11) | 2001 | Developing Countries | Narrative Review | Information and Communication technologies in healthcare | Insignificant use of data Low quality of data Function of health information systems in parallel Lack of prompt reporting and effective and timely reviews Unrelated information collected to fulfill the intended purposes |
|
| Oak (12) | 2007 | Developing Countries | Narrative Review | Geographic InformationSystem | financial restrictions - Disparities in wages - pricypayments of usage bills and telephone time -primitive health information system payments- Inadequate resources- politics Conflicts of interest with medical profession Culture and socio-ecological factors Population inflation and social crises Enforcing the legislation convincing individuals to new technologies Availability and visibility of health research Lack of infrastructures, untrained personnel data management |
|
| Asangansi (13) | 2012 | Africa | case study | Health Management Information System | Inadequate logic of institutions that consider the system implementation process - Numerous errors in system implementation | Improving the performance of a health information management system - a strategy based on logic |
| Al-Yaseen (14) | 2012 | Asia | case study | health information systems in private hospitals |
practitioners are not appreciating the full gains of HIS and need to be aware of such gainsabsense of acknowledgementis evidently behind the apparent deficitof developmentof HIS, |
|
| Cline and Luiz (15) | 2013 | Africa | case study | Hospital Information System | Computer time consuming - systems are not automated | Increase employee satisfaction, improve resource management, reduce transaction costs, Better security and privacy |
| Forazin and Joia (16) | 2013 | south America | case study with a review | Health Information System | No system updates, General error, Tolerance error, duplication error, repetition error |
Ability to interact with other systems - use the experiences of developed countries |
| Khalifa (17) |
2013 | Asia | Explorative method used a questionnaire | Electronic Medical Records | Lack of experience of people - technical, Financial, organizational, legal, professional and human obstacles |
|
| Sadoughi et al (18) | 2013 | Developing Countries | systematic review | Hospital Information System | User unsatisfaction Improper usability |
Improvements of Financial, organizational, behavioral and managerial Technical |
| Aziz and Mohamadali (19) | 2015 | Asia | Review article | Hospital Information System | Provides continuing education Use of management rules |
shortage of manpower Non-sharing of information |
| Ishijima et al (20) |
2015 | Africa | case study | Human Resource for Health Information System (HRHIS) and the Training Institution Information System(TIS) | Large amount of information | Improvement of system management performance – use of experts |
| Othman and Hayajneh (21) |
2015 | Asia | Descriptive-cross sectional | Electronic Medical Record | Employee learning and growth, promotion Financial, customer satisfaction, quality of health information, system, internal process |
|
| Tilahun and Fritz (22) |
2015 | Africa | quantitative cross sectional study | Electronic Medical Record | Insufficient resources, problems in the quality of services and information and user satisfaction | Increase user satisfaction, quality of services, quality of information |
| Verbeke et al (23) | 2015 | Africa | Review article | Hospital Information System | clear communication, real-time scheduling Manage ongoing changes |
Unclear goals, poor management, insufficient skills, inadequate training |
| Sidek and Martins (24) | 2017 | Asia | Grounded Theory | electronic health record system | software practices overall management culture; technical glitches, consistency in data records and episodes of data miss |
usability, requirements analysis, training, change management, project organization; |
| Alipour et al (25) | 2017 | Asia | cross-sectional descriptive and analytic | hospital information system | educational factors organizational factor |
behavioral factor |
| Mohamadali and Azizah (26) |
2017 | Asia | Review article | hospital information system in hospitals | technological barriers ineffective design, data loss usefulness of the IT inadequate equipment, lack of internet access compatibility, readiness, availability and network stability, Content complexity in the design Data quality and data authenticity, Lack of system integration, Poor interface and less user- friendly, Time consuming Poor usability, functionality and performance Inconvenience practice |
|
| deRiel et al (27) | 2018 | south America | case study | electronic medical records (EMRs) | ethical, financial, functionality, organizational, political, technical and training balancing expensesin hardware and software infrastructure upkeep, user capacity and data quality control; implementinga system within the context of the larger eHealth ecosystem with a strategy for interoperability and data exchange; providing system governance and strong coaching to support local system ownership and planning for system financing to ensure sustainability |
|
| ChePa et al (28) | 2018 | Asia | Interventional | Information System (IS) in government hospitals |
Resistance to change conflict between users human problems (workload, readiness, priority, skill, mentality, desire, outlook, feeling, initiative, perception, commitment, awareness, personal interest, and user dependence). Support and technology Software limitation issues. |
|
| Kpobi et al (29) | 2018 | Asia | Individual semi-structured interviews |
mental health information system |
Expanded work load, low staff involvement and training, and lack of logistic support to maintain the system working. limited number of computers available at the hospital, absense of enthusiasm in the optimal use of the MHIS, does not meet the needs of all the different categories of users |
|
| Sahay et al (30) | 2018 | Asia | case studies | Universal Health Coverage (UHC) robust Civil Registra- tion and Vital Statistics (CRVS) |
low and incomplete infrastructure, insufficient and unevenly distributed resources, absense of acceptable capacity to deal with the complexity they entail | |
| Ebnehoseini et al (31) | 2019 | Asia | Survey | Healthcare Information Systems | usability, information security, completeness and job relevancy operational reliability, response time, log in and support |
|
| Afrizal et al (32) |
2019 | Asia | qualitative study done by conducting in-depth interviews |
Primary health care information system | lack of commitment, lack of care difficult to use electronic documentation for outside activities Limited electricity the policy for the developing of information systems in the PHC is still not yet available. |
Access to internet-Computer availability- Availability of IT team/unit- Electricity power- Occasional IT use-users computer skills-Workload-Employee Turnover-Lack of training in IT Resistance of change-Budget Constraints-Security Absence of planning, project administration -Lack of financial incentives-Lack of technology support-Loss of fertility Absense of functions, not meet the practice needs-Absense of System maintenance |
| Abbas and Singh (33) |
2019 | Africa | qualitative -semi structured interviews | Picture Archiving and Communication Systems (PACS) | Space and inappropriate furniture, Insufficient infrastructure, Protection of equipment, Hospital financial constraints, Lack of IT knowledge, Resistance to change, Image storage capacity, System maturity, Software and hardware encounters, Maintaining the radiology workflow, Vendor related concerns | |
| Mayston et al (34) |
2020 | low and middle-income countries chronic |
Review article | mental healthcare | behavioral, technical and organizational determinants resource allocation poor quality unreliable of data incomplete management and administrative capacity to use data effectively to support decision-making lack of healthcare personnel with health informatics training deficits in IT infrastructure, absence of computers, networking equipment, internet connectivity interoperability between different EHR systems is poor challenge of mixture of the new data collection with current information systems, insufficient decentralization |
data collection is planned in association with local stakeholders, there is some sign of success completion and accuracy of data forms |
Challenges and Causes of Success and Failure of HISs in Developing Countries
Various studies have presented numerous challenges and different causes for the success and failure of HIS in developing countries.15-38 In this regard, Sidek and Martinez (24). in their study have identified the lack of confidence of clinical professionals in the new system as the main challenge to have a successful implementation of the electronic health record at a dental center. Paying attention to the principles of change management and the commitment of the center's senior managers in adhering to making changes is considered as the key factor in the success of this system. Moreover, in a study by Maystson et al, (34), the challenges and opportunities for a successful implementation of an information system for chronic mental health care were divided into 3 categories as follows: behavioral, organizational, and technical factors. In addition, Poor data quality in decision-making was one of the main causes for the failure of the system. Accordingly, they have also cited the high adaptation of the data collected to the needs of stakeholders as another important cause in the success of a the HIS. Ebne Hosseini et al (31) in their study mentioned 3 factors of usefulness, system quality, and net profit as essential for the success of the hospital information system. In a systematic review on the success factors of HISs, deRiel et al (27) identified 5 following categories of success factors: functional, organizational, political, technical, and educational. Moreover, they emphasized that these important factors for the long term success in developing complex HISs are as follows: adjustinginvestment in hardware and software, user infrastructure, and data quality control.
In another study by ChePa et al (28) a total of 36 challenges were identified in implementing hospital information systems projects, which fall into 4 fundemental categories, including human, technology and infrastructure, software constraints, and support. Moreover, 14 challenges were also found to be related to human problems, such as workload, readiness, priority, skill, mentality, desire, outlook, feeling, initiative, perception, commitment, awareness, personal interest, and user dependence. Also, there were 6 challenges for support and technology, as well as 12 challenges for software constraint problems. In a study by Alipour et al (25) functional, ethical, and cultural factors were identified as success factors, and behavioral, organizational, and educational factors were recognized as weaknesses of the system. In their study, Afrizal et al (32) have reported human factors, infrastructure, organizational support, and process as effective factors on adopting the primary health care information system. Furthermore, in a study conducted by Kpobi et al (29) the increase in staff workload and rework in data recording were noted as the causes of the failure of the mental health information system and the lack of infrastructure was found as the challenge in implementing
System. In a review article, Mohamadali and Aziz (26) have also stated the lack of system integration as the main obstacle for the implementation of hospital information system in hospitals. In this regard, the quality of information and system quality were introduced as the other factors affecting the success of the system. In another study, Abbas and Singh (33) considered the lack of financial support as the most important obstacle for the successful implementation of information technology in health care from the perspectives of customers and sellers. The lack of general knowledge on information technology is another challenge that can disrupt the implementation of PACS systems as well, along with the lack of management and change in management that create challenges during the implementation and training of the project. Additionally, in a study performed on the Health Management Information System, Asangansi (13) cited the lack of access to quality data, ambiguous data and system ownership, and instability and lack of trust in servers as challenges in the way of implementing this system. His study has mentioned the lack of sufficient time to provide services to patients following the use of hospital information system, and high safety and information security were among the factors in the success of this system. Khalifa (17). in his study he aimed to reduce the obstacles to HISs and divided them into 6 categories as follows: human, financial, legal, organizational, technical, and professional. The high cost of setting up and maintaining the system, misconceptions and beliefs on the use of these systems, and the fear of losing information were among the important obstacles raised in this study.
In a review study on the elements influencing the advancement and falling of hospital information systems, Sadoughi et al (18) identified several factors in developing and developed countries. Correspondingly, these factors were then classified into 12 areas named as functional, organizational, behavioral, cultural, managerial, technical, strategic, economic, educational, legal, ethical, and political factors. In their study, Aziz et al (19) examined the role of human factors or the role of users of the hospital information system in the success or failure of these systems. The results have shown that physicians play the most important role in the acceptance of hospital information systems in hospitals. Also, Verbeke et al (23) in their study listed 14 failure factors as well as 15 success factors for hospital information systems in sub-Saharan Africa. Some of these failure factors were as follows: unclear goals, poor management, inadequate skills, and inadequate training. Also, some of the success factors were transparent communication, real timing, and managing progressive changes.
Solutions to the Barriers and Challenges of HISs in Developing Countries
Seven studies (14,24,26-30) have provided some solutions to address the challenges raised in the previous sections, which are presented in Table 3.
Table 3. Solutions extracted from selected studies to overcome HISs challenges .
| Solutions | |
| Continuous and appropriate training of health personnel Development of local and national technologies Establishment and operation of an organization coordinating activities related to the health information system at the national level Use of standards Process reengineering Develop vision and action plan Strengthen organizations and human resources in terms of awareness, skills and leadership Strengthen information and communication technology Apply data-related rules and standards Private sector financing and cooperation with the public sector (14) |
|
| Expanded communication and horizontal collaboration amongst stakeholders; elemental conversion from being focused on pushing healthcare technology to using EHR for developing the working practice of clinical staff; manage the alteringprocess by agreeing system aimsand functionalities through wider consensual debate, and participated helping strategies realized through common commitment28 | |
| Improve computer self-efficacy, Monitor adverse effects on patient safety, Improve system design to be more user friendly, Improve system response time, System need to be flexible to alter and, integrate with current systems, Require adequate and effective IT strategies, Look for new methods to enhanceworkload, and enhance information quality, System can create a complete record, report and support related activities Make a secure intranet for information exchanging30 | |
| Continuing involvement of policymakers, medical staff, technicians and managersin the developingprocess. Involving all stakeholders to ensure better compliance33 | |
| Adopting hybrid rather than fully Internet; dependent systems Renewing what already exists – integration and rationalization34 | |
| Proper situational and needs assessment, Government and private sector support, Training, Proper change management processes, Adequate needs assessment, Regular maintenance and evaluation37 | |
| building strong multispectral partnerships, Locally meaningful mental health indicators, aligned to service; Technology used for data collection and management should be appropriate38 |
Classification of HISs Causes of Success and Failure
After reviewing the success and failure factors that were raised in various studies, researchers compared the different divisions related to these factors, and then the differences and similarities of these classifications were extracted. Finally, success and failure causes were divided into 4 categories, which are human, organizational, financial, and technical factors. Human factors were divided into 6, organizational factors into 13, financial factors into 5, and technical factors into 6 subfactors (Table 4). If the factors listed in Table 4 are taken into account, the information system will be successful. And if ignored, they cause the HIS to fail.
Table 4. Classification of HISs success and failure factors .
| Human factors | Organizational factors | Financial factors | Technical factors |
| 1. Use of devices and tools (13,15,25) 2. Knowledge of users (13,170-19,21,23,27,33-34 3. Acceptance and readiness of users (15,17,19,21,28) 4. User satisfaction (22,23,29) 5. Lack of appreciation (14) 6. Poor staff involvement (29,32) |
1. Staff monitoring (17) 2. Staff training (12,17,19,21,23,25,32) 3. Organizational policies (16-17,19,20,25) 4. Employee interactions (13,18) 5. Quality of staff service (15,16) 6. Ethical considerations (16,18) 7. Insignificant use of information (1) 8. Function in parallel (11) 9. Change management (24,27,32-33) 10. Project organization (24) 11. Strong leadership (27) 12. Conflict between users (12,27) 13. Increased workload (27,33) |
1. Rudimentary health information system costs (12,15,17-18,21) 2. Profit (12,17-18,22) 3. Budget (13,18,20) 4. Inadequate resources (12,26,30,33) 5. Investments in hardware and software (27,32) |
1. Infrastructure (12-13,15,17,22-23,26-27,30,32-34) 2. Data quality and integrity (11-13,17-18,20,21-22,24,26-28,34) 3. Usability (18,21,24,26,27,31) 4. Safety and security (13,15,18-31) 5. Requirements analysis (24) 6. Ineffective design (26) |
Discussion
This study attempted to answer these questions: What are the challenges and barriers to health information systems in developing countries? And What factors contribute to the success and failure of these systems in these countries? In this regard, the findings indicated that many of the challenges that developing countries face in using HISs are influenced by the social, cultural, economic, geographical, and political conditions of these countries. High population and low level of literacy and inequality in the access to and use of information technology services and low level of information technology literacy in many developing countries are key factors in affecting the use of information technology and information systems in the health care systems of these countries (35). Some of the challenges are more specific to developing countries and developed countries have been less involved in applying HISs; some of these challenges are socioeconomic constraints (1,15,20-24,23,29,32); topics related to technical and operational infrastructure (17,22,23,27,30,32-36); incomplete business and lack of adequate business space; lack of private sector participation in health information; non-standard equipment and facilities used in this area; lack of a clear vision in this area (22,23,27,30,37-40); and poor integrity between the same HISs at health facility and health management level section (11-12,18,20,21-22,24,39) In addition to these factors, the increase in workload due to the change of HISs from manual to electronic systems has also caused users to resist using these systems (40). Considering the experiences of developed countries, it seems that one of the root causes in the failure HISs is the existence of cultural factors and the lack of cultural capabilities required to accept and use this system. The other main factor that the researcher emphasizes is the lack of information and communication technology (ICT) infrastructures in these countries. ICT plays a significant role in developing information systems in organizations. On the other hand, one of the major challenges of using these systems in these countries is organizational complexity in the health sector, which is a major challenge to the governmental and private sectors in implementing development strategy. There is a need to deal with these complications by applying flexible standards regarding the design and deployment of HISs (41).
According to the research findings, one of the most critical elements influencing the advance or falling of the HIS in developing countries was the poor data quality and integrity. There are many reasons why data quality is low in different sources. In many developing countries, technical and professional skills needed to communicate with information among experts are few. Another reason is the lack of motivation among health workers. Also, the lack of feedback mechanisms is another reason for poor quality of data (42-43). One of the reasons for the failure of information systems in developing countries was the irrelevance of the data collected to cover professional activities. Most of the data recorded and reported by the health sector employees of these countries have no practical application to help managers make decisions and control the delivery processes. On the other hand, useful data collected often support the goals related to control of diseases and rarely support managerial goals. One of the reasons for weaknesses in these countries is poor consensus about information needs between providers and users in different level of heal thcare (44).
There can be different solutions to overcome obstacles and problems on the way to HISs in developing countries, including the formulation of strategic plans and policies required for the development of information systems in the national and private sectors, formulation of laws for reporting communicable diseases from governmental and private sectors, formulation of confidentiality and retrieval policies, developing knowledge management capacity and using health information capacity by users and service providers, creating networks for knowledge sharing, establishing coordination and integration between information gathering systems, strengthening the disease surveillance and reporting systems, the periodic reporting of information needs and protection of health information system components, enhancing the use of information technology and communication technologies, enhancing the use of information technology in the field of transmission and access and sharing health information. (14,26,29-30,33-34,45) Many of the solutions proposed to remove barriers to the success of HISs in developing countries have focused on strengthening policy in this area. One of the most important limitations of the researchers in conducting this study was the scattering of success and failure factors of HISs in different studies, so that in some cases only one challenge or success and failure factor was presented. Researchers tried to select studies that presented a set of factors by expanding the range of keywords to increase the comprehensiveness of the search process.
Conclusion
Various sources have cited several reasons for the failure of information systems, including a lack of specialized and experienced human and financial resources and cultural factors and the lack of infrastructure. There is a need to create flexible standards for designing and deploying HISs to address these complexities. Finally, there are several solutions to address the obstacles and problems facing health information systems in developing countries, including formulating strategic plans and policies necessary for the development of national HISs, developing laws on reporting diseases and collecting data from public and private sectors, determining information privacy and disclosure policies, formulating maintenance and retention policies, Enhancing the capacity of knowledge management and health information capacity utilization by users and providers of health services, Creating a network for knowledge exchange, creating harmony and integration between information collection systems, strengthening disease surveillance and reporting systems, conducting periodic information needs assessment and support in health information system components, strengthening the use of information and communication in the health sector, using appropriate ICT technologies and strengthening the use of information technology in the transmission and sharing of HISs.
Acknowledgment
The authors thank the Health Information Technology Research Center in Isfahan University of Medical Sciences.
Conflict of Interests
The authors declare that they have no competing interests.
Cite this article as: Bagherian H, Sattari M. Health Information System in Developing Countries: A Review on the Challenges and Causes of Success and Failure. Med J Islam Repub Iran. 2022 (26 Sep);36:111. https://doi.org/10.47176/mjiri.36.111
References
- 1.AbouZahr C, Boerma T. Health information systems: the foundations of public health. Bull World Health Organ. 2005;83:578–83. [PMC free article] [PubMed] [Google Scholar]
- 2.Braa J, Monteiro E, Sahay S. Networks of action: sustainable health information systems across developing countries. MIS Q. 2004;28:337–62. [Google Scholar]
- 3. Braun E. Technology in context: Technology assessment for managers 1st Edition. London, UK: Rutledge, eBook Published 2005.
- 4. Beaver K. Healthcare information systems 2nd Edition. New York, USA: Auerbach Publications, 2002.
- 5. Consulting VW. Health information systems in developing countries; a landscape analysis. United States of America: Vital Wave Consulting United States of America. 2009.
- 6.Karuri J, Waiganjo P, Orwa D, DHIS MA. The Tool to Improve Health Data Demand and Use in Kenya. J Health Inform Dev Ctries. 2014;8:38–60. [Google Scholar]
- 7. Ono R. Critical Obstacles to Telecommunication Development in Developing Countries. Proceedings of the 18th Annual Pacific Telecommunications Conference, 2007,1:280- 289.
- 8. Sood SP, Nwabueze SN, Mbarika VW, Prakash N, Chatterjee S, Ray P, Mishra S. Electronic medical records: A review comparing the challenges in developed and developing countries. In: Proceedings of the 41st Annual Hawaii International Conference on System Sciences (HICSS 2008) 2008 Jan 7 (pp. 248-248).
- 9.Krickeberg K. Principles of health information systems in developing countries. Health Inf Manag. 2007;36:8–20. doi: 10.1177/183335830703600303. [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 11. Sahay S. Special issue on “IT and health care in developing countries”. Electron J Inf Syst Dev Ctries. 2001 May;5(1):1-6.
- 12. Oak M. A review on barriers to implementing health informatics in developing countries. J Health Inf Dev Ctries. 2007 Dec 18;1(1).
- 13. Asangansi I. Understanding HMIS implementation in a developing country Ministry of Health context-An institutional logics perspective. Online J Public Health Inform 2012;4(3). [DOI] [PMC free article] [PubMed]
- 14. Al-Yaseen HM. Challenges of Implementing Health Care Information Systems in Developing Countries: Using a Mixed Method Research. J emerg trends comput Inform Sci. 2012 Nov; 3(11):1521-5.
- 15.Cline GB, Luiz JM. Information technology systems in public sector health facilities in developing countries: the case of South Africa. BMC Med Inform Decis Mak. 2013 Dec 1;13(1):13. doi: 10.1186/1472-6947-13-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Forazin M, Joia LA. Dimensions of Analysis for Health Informatics in Brazil. Proced Technol. 2013 Jan 1;9:1344–50. [Google Scholar]
- 17.Khalifa M. Khalifa MBarriers to health information systems and electronic medical records implementationA field study of Saudi Arabian hospitalsProced Comput Sci. 2013 Jan. 1;21:335–42. [Google Scholar]
- 18. Sadoughi F, Kimiafar K, Ahmadi M, Shakeri MT. Determining of factors influencing the success and failure of hospital information system and their evaluation Methods: a systematic review. Iran Red Crescent Med J. 2013 Dec;15(12). [DOI] [PMC free article] [PubMed]
- 19.Ab Aziz NF, Mohamadali NA. The challenges of human factors for implementation of information systems in the healthcare. ARPN J Eng Appl Sci. 2015;10(23):17914–22. [Google Scholar]
- 20. 20 Ishijima H, Mapunda M, Mndeme M, Sukums F, Mlay VS. Challenges and opportunities for effective adoption of HRH information systems in developing countries: national rollout of HRHIS and TIIS in Tanzania. Human Resour Health. 2015 Dec;13(1):1-4. [DOI] [PMC free article] [PubMed]
- 21.Othman M, Hayajneh JA. An integrated success model for an electronic health record: a case study of Hakeem Jordan. Procedia Econom Fin. 2015 Jan 1;23:95–103. [Google Scholar]
- 22.Tilahun B, Fritz F. Modeling antecedents of electronic medical record system implementation success in low-resource setting hospitals. BMC Med Inform Decis Mak. 2015 Dec 1;15(1):61. doi: 10.1186/s12911-015-0192-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Verbeke F, Karara G, Nyssen M. Human Factors Predicting Failure and Success in Hospital Information System Implementations in Sub-Saharan Africa. Stud Health Technol Inform 2015;482-486). [PubMed]
- 24.Sidek YH, Martins JT. Perceived critical success factors of electronic health record system implementation in a dental clinic context: an organisational management perspective. Int J Med Inform. 2017 Nov 1;107:88–100. doi: 10.1016/j.ijmedinf.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 25.Alipour J, Karimi A, Ebrahimi S, Ansari F, Mehdipour Y. Success or failure of hospital information systems of public hospitals affiliated with Zahedan University of Medical Sciences: A cross sectional study in the Southeast of Iran. Int J Med Inform. 2017 Dec 1;108:49–54. doi: 10.1016/j.ijmedinf.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 26.Mohamadali NA, Ab Aziz NF. the technology factors as barriers for sustainable health information systems (his)–a review. Procedia Comput Sci. 2017 Jan 1;124:370–8. [Google Scholar]
- 27.Deriel E, Puttkammer N, Hyppolite N, Diallo J, Wagner S, Honoré JG, Balan JG, Celestin N, Vallès JS, Duval N, Thimothé G. Success factors for implementing and sustaining a mature electronic medical record in a low-resource setting: a case study of iSanté in Haiti. Health Policy Plan. 2018 Mar 1;33(2):237–46. doi: 10.1093/heapol/czx171. [DOI] [PubMed] [Google Scholar]
- 28.ChePa N, Jasin NM, Bakar NA. Information System Implementation Failure in Malaysian Government Hospitals: How Change Management Helps? J Telecommun Electron Comput Eng. 2018 Feb 26;10(1-11):69–75. [Google Scholar]
- 29. Kpobi L, Swartz L, Ofori-Atta AL. Challenges in the use of the mental health information system in a resource-limited setting: lessons from Ghana. BMC Health Serv Res. 2018 Dec;18(1):1-8. [DOI] [PMC free article] [PubMed]
- 30.Sahay S, Nielsen P, Latifov M. Grand challenges of public health: How can health information systems support facing them? Health policy technol. 2018 Mar. 1;7(1):81–7. [Google Scholar]
- 31.Ebnehoseini Z, Tabesh H, Deldar K, Mostafavi SM, Tara M. Determining the Hospital Information System (HIS) Success Rate: Development of a New Instrument and Case Study. Open Access Maced J Med Sci. 2019 May 15;7(9):1407. doi: 10.3889/oamjms.2019.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Afrizal SH, Handayani PW, Hidayanto AN, Eryando T, Budiharsana M, Martha E. Barriers and challenges to Primary Health Care Information System (PHCIS) adoption from health management perspective: A qualitative study. Inform Med Unlocked. 2019 Jan 1;17:100198. [Google Scholar]
- 33.Abbas R, Singh Y. PACS Implementation Challenges in a Public Healthcare Institution: A South African Vendor Perspective. Healthcare Inform Res. 2019 Oct 1;25(4):324–31. doi: 10.4258/hir.2019.25.4.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mayston R, Ebhohimen K, Jacob K. Measuring what matters–information systems for management of chronic disease in primary healthcare settings in low and middle-income countries: challenges and opportunities. Epidemiol Psychiatr Sci 2020; 29. [DOI] [PMC free article] [PubMed]
- 35. Web cast ‘Health Informatics and Developing Countries’, informaticopia, Friday, January 27, 2006, Available from: http://www.rodspace.co.uk/blog/2006/01/web-cast-health-informatics-and.html.
- 36.Nkrumah GA, Ebo HR. Towards a sustainable framework for computer based health information systems (CHIS) for least developed countries (LDCs) Int J Qual Health Care. 2007;20:532–44. doi: 10.1108/09526860710819468. [DOI] [PubMed] [Google Scholar]
- 37. Edoh TO, Pawar PA, Loko LY. Challenges Facing Health Service Delivery in Developing Countries and Solution Approaches: The Case of Benin, a West-African Developing Country. In: Handbook of Research on Emerging Perspectives on Healthcare Information Systems and Informatics 2018 (pp. 515-559). IGI Global.
- 38. Heeks R. Information Systems and Developing Countries: Failure, Success, and Local Improvisations. Institute for Development Policy and Management. University of Manchester, Manchester, United Kingdom; 2002.
- 39.Miraj SS. Challenges and perspectives of health informatics and its management in developing Asian countries. Biosci Biotechnol Res Commun. 2017;10:597–600. [Google Scholar]
- 40. Mengiste SA. Globalization and Icts: Potentials and Challenges to the Public Health Sector of Developing Countries. IN: Proceedings of the Nineteenth Americas Conference on Information Systems, Chicago, Illinois, August 15-17, 2013.
- 41. UK Essay. Challenges of health information systems. www.ukEssay.co.uk, 2008.
- 42. Gahleb E, Mohamed I. Health Information System Success Framework Based On User Requirements Perspective. J Theor Appl Inf Technol 2018;96.
- 43. Hamunyela S, Jere N. An Evaluation of Health Information Systems (HIS) for Namibia. In2018 IST-Africa Week Conference (IST-Africa) 2018 May 9 (pp. Page-1). IEEE.
- 44.Ndetei DM, Jenkins R. The implementation of mental health information systems in developing countries: Challenges and opportunities. Epidemiol Psychiatr Sci. 2009;18:12–6. [PubMed] [Google Scholar]
- 45.Tessa T, Edejer E. Information in practice disseminating health information in developing countries: the role of the Internet. BMJ. 2000;321:797–800. doi: 10.1136/bmj.321.7264.797. [DOI] [PMC free article] [PubMed] [Google Scholar]