Abstract
Background
Antimicrobial resistance (AMR) is an important global health concern, projected to contribute to significant mortality, particularly in developing countries. This study aimed to determine the knowledge, perceptions of clinical health professions students towards antimicrobial resistance and rational use of medicine and confidence level to prescribe antimicrobials.
Methods
An online descriptive cross-sectional survey was conducted among clinical health professions students across 9 medical schools in Uganda. A semi-structured questionnaire using Kobo Toolbox form was shared among participants via WhatsApp Messenger (Meta, California, USA). Knowledge was categorized using modified Bloom’s cut-off. One-way ANOVA, Chi-square or Fisher’s exact test, and logistic regression were used to assess the association between dependent and independent variables. A p < 0.05 was considered statistically significant.
Results
We surveyed 681 participants, most were pursuing a Bachelor of Medicine and Surgery degree (n = 433, 63.6%), with a mean age of 24 (standard deviation: 3.6) years. Most participants (n = 596, 87.5%) had sufficient knowledge about antimicrobial resistance with a mean score of 85 ± 14.2%. There was a significant difference in mean knowledge scores of year 4 (86.6%) compared to year 3 (82.4%) (p = 0.002) and year 5 (88.0%) compared to year 3 (82.4%) (p < 0.001). Most participants (n = 456, 66.9%), were confident on making an accurate diagnosis of infection, and choosing the correct antimicrobial agent to use (n = 484, 71.1%).
Conclusion
Health profession students exhibited good knowledge on antimicrobial resistance and high self-perceived confidence that should be leveraged to foster better future antimicrobial prescription practices. However, they still agreed that a separated course unit on AMR is necessary which responsible authorities should consider to consolidate the efforts.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13756-022-01186-9.
Keywords: Antimicrobial resistance, Rational use of medicine, Health profession students, Knowledge
Background
The discovery of penicillin by Sir Alexander Fleming in 1928 is one of the greatest revolutions in therapeutics and practice of modern medicine [1]. However, the current surge in antimicrobial misuse and overuse in human, agricultural and veterinary practices have escalated world-wide spread of antimicrobial-resistant organisms which has emerged as a big threat to global health [2–4]. In 2019 alone, an estimated 1.27 million deaths were directly attributed to bacterial antimicrobial resistance (AMR), with sub-Saharan Africa having the greatest burden [5]. It is projected that by 2050, AMR will cause up to 10 million deaths, especially in low- and middle-income Countries like Uganda which carry the greatest burden of severe and life-threatening infections [6, 7] and approximately USD 100 trillion of the world’s fiscal outputs will be splurged if definitive measures to contain the burden are not implemented [8]. Although AMR develops naturally, factors like poor prescription practices, improper medication use by patients, and in some instances, inadequate health workers’ knowledge on AMR accelerate its development [9, 10].
The World Health Organization (WHO) defines parameters for good prescription practice [11], and in collaboration with International Network of Rational Use of Drugs (INRUD), developed indicators to measure performance of rational antimicrobial prescription [12]. Prescriptions are largely done by qualified health professionals like doctors, whose shortage especially in low- and middle-income countries exacerbate irrational medicine usage [4, 13, 14]. Medical students are expected to prescribe drugs under supervision of clinical instructors as its imperative that the next generation is better prepared to use antimicrobials more sparingly and appropriately. The WHO emphasizes that healthcare workers and medical students should be trained on rational antimicrobial prescribing or antimicrobial stewardship as an integral part of efforts to curb antimicrobial resistance [3, 15]. Uganda in 2018 developed a national action plan against antimicrobial resistance entailing integration of antimicrobial stewardship courses into training curriculum for undergraduate courses though its implementation is still unsatisfactory [16].
The medical school curriculum generally provides students with theoretical knowledge of biomedical sciences, diagnosis, treatment, and prevention of diseases but does not set up antimicrobials and their practical rational prescription as a separate entity. Indeed, from a study by Huang et al. in 2013, clinical students exhibited good knowledge about antimicrobials however their usage and prescription were excessive and majority believed that it’s important to establish a separate course unit on rational use of antimicrobials [14]. Several other studies have also reported similar findings where medical students lacked self-confidence on antimicrobial prescription, believed inadequate time is spent on clinical pharmacology and would recommend more training on rational prescription [17–21].
Health professions students constitute the next-generation medical personnel whose knowledge, attitude and practice in relation to antimicrobial use can greatly impact in the future of antimicrobial resistance [14]. In Uganda, during the 5-year medical undergraduate study, students in the clinical years are expected to prescribe and manage patients under supervision. However, there is inadequate understanding of medical students’ knowledge and perceptions on antimicrobial resistance, confidence level of prescription and whether they receive adequate education on appropriate antimicrobial use. This study aimed to explore important concepts on rational medicine use among clinical health professions students in Uganda.
Methods
Study design
We conducted a descriptive cross-sectional, multicenter, online survey for 2 weeks within the month of October 2021 using a quantitative approach.
Study setting
The study involved 9 Universities in Uganda offering undergraduate health science courses namely Makerere University (MAK), Mbarara University of Science and Technology (MUST), Gulu University (GU), Kampala International University (KIU), Kabale University (KU), Busitema University (BU), Islamic University in Uganda (IUIU), Lira University (LU), and Bishop Stuart University (BSU). MAK, GU, MUST, BU, LU and KU are public universities, and the remaining universities are private.
Study population
The study involved health professions students specifically in their clinical years pursuing any of the following courses: Bachelor of Medicine and Bachelor of Surgery (MBChB), Bachelor of Dental Surgery (BDS), Bachelor of Science in Nursing (BNS), Bachelor of Pharmacy (BPharm) and Bachelors of Anesthesia (BNA). In Uganda the different Universities run different 5-year curriculums of MBChB and BDS, 4 years for BNS, BNA, and BPHARM where some students start clinical studies in the third year while others in the fourth year. Therefore, the study targeted students from year three to five in the different universities considering that they were in their clinical phase of study.
Inclusion and exclusion criteria
Students in the above-mentioned Universities pursuing MBChB, BDS, BNS, BNA, BPharm courses in their clinical years who had consented to participate were included in the study while those who didn’t consent to participate were excluded.
Data collection and sampling procedure
This study was conducted at a time that Uganda was still in a partial lockdown. We therefore opted to use WhatsApp Messenger (Meta, California, USA) for enrolling potential participants. We employed convenience sampling where we identified all the existing WhatsApp groups of health professions students in the nine universities through a coordinator for each specific group. The Kobo Toolbox link to the questionnaire was then sent to the potential participants via the identified WhatsApp groups.
Data collection tool
The data collection tool was developed from validated questionnaires of similar studies [3, 4, 22, 23] and modified to suit our study objectives and locality (Additional file 1: Questionnaire.docx). It was aggregated in four parts the first one collecting participants’ demographic information. Knowledge about antimicrobial resistance was assessed using 5 questions 3 on general aspects and 2 on national AMR patterns. Each question had a value of ‘1’ for correct response or ‘0’ for wrong or don’t know response. Then it was categorized using modified Bloom’s cut-off point, as sufficient if the score was above 80%. The knowledge on rational use of medicine was assessed with 5 questions assessing awareness of different aspects with a ‘yes’ or ‘no’ response. Third part consisted of perceptions of students about antimicrobial resistance with 6 statements answered on a 5-point Likert scale from strongly agree to strongly disagree and 5 statements about perceptions on quality of the training on antibiotic resistance and rational use of medicine answered by 3-Likert scale of “yes”, “no”, or “unsure”. The last assessed Confidence level of prescription among medical Students answered on a 5-point Likert scale from Very confident to Very unconfident assigned a score of 5 through 1.
Study variables
Independent variables were the demographic details which included sex, age, religion, residence, and University and dependent variables were knowledge, attitude, perceptions on antimicrobial resistance and rational use of medicine, perception on training and level of prescription confidence.
Data management analysis
Fully completed questionnaires were extracted from Kobo Toolbox and exported to Microsoft Excel 2016 (Microsoft Corporation) for cleaning and coding. The cleaned data was exported to Stata (StataCorp) version 16 for analyses. Numerical data was summarized as means and standard deviations. Categorical data was summarized as frequencies and proportions. Associations between independent variables and dependent variables were assessed using one way ANOVA, Chi-square test or Fischer’s exact test and multivariate logistic regression analysis. A P < 0.05 is considered statistically significant.
Results
Sociodemographic characteristics of participants
A total of 681 participants (55% response rate), with a mean age of 24 ± 3.6 years were enrolled. Of this, most were male (n = 381, 55.9%), in their third year of study (n = 314, 46.1%), and pursuing MBChB (n = 433, 63.6%), Table 1.
Table 1.
Sociodemographic characteristics and knowledge scores of participants on antimicrobial resistance (N = 681)
| Variable | Frequency (%) | Knowledge (% Score) Mean ± SD | Sufficient knowledge | p value | |
|---|---|---|---|---|---|
| Yes (%) | No (%) | ||||
| Overall | 85 ± 14.2 | 596 (87.5) | 85 (12.5) | ||
| Age (Mean ± SD) | 24 ± 3.6 years | ||||
| Sex | |||||
| Male | 381 (55.9) | 85.4 ± 15 | 325 (54.5) | 56 (65.9) | 0.049* |
| Female | 300 (44.1) | 84.4 ± 13.2 | 271 (45.5) | 29 (34.1) | |
| Year of study | |||||
| Year 3 | 314 (46.1) | 82.4 ± 13.2 | 272 (45.6) | 42 (49.4) | 0.806 |
| Year 4 | 220 (32.3) | 86.6 ± 14.4 | 194 (32.6) | 26 (30.6) | |
| Year 5 | 147 (21.6) | 88.0 ± 15.3 | 130 21.8) | 17 (20.0) | |
| Course | |||||
| Medicine & surgery | 433 (63.6) | 86.1 ± 15.6 | 365 (61.2) | 68 (80.0) | 0.016* |
| Nursing | 206 (30.3) | 82.3 ± 10.7 | 191 (32.0) | 15 (17.6) | |
| Pharmacy | 25 (3.6) | 86.4 ± 11.1 | 24 (4.0) | 1 (1.2) | |
| Dental surgery | 9 (1.3) | 91.1 ± 10.5 | 9 (1.5) | 0 (0) | |
| Anesthesia | 8 (1.1) | 77.5 ± 16.7 | 7 (1.2) | 1 (1.2) | |
| University | |||||
| Lira university | 150 (22.0) | 81.6 ± 8.8 | 143 (24.0) | 7 (8.2) | 0.014* |
| Busitema university | 114 (16.7) | 87.5 ± 15.4 | 100 (16.8) | 14 (16.5) | |
| Kampala international | 113 (16.6) | 83 ± 15.9 | 92 (15.4) | 21 (24.7) | |
| Mbarara university | 76 (11.2) | 85.3 ± 14.4 | 68 (11.4) | 8 (9.4) | |
| Gulu university | 69 (10.1) | 84.6 ± 16.9 | 55 (9.2) | 14 (16.5) | |
| Kabale university | 63 (9.3) | 86.7 ± 14.8 | 53 (8.9) | 10 (11.8) | |
| Makerere university | 50 (7.3) | 89.2 ± 14.1 | 46 (7.7) | 4 (4.7) | |
| Bishop Stuart university | 26 (3.8) | 83.1 ± 14.6 | 21 (3.5) | 5 (5.9) | |
| Islamic university in Uganda | 20 (2.9) | 90 ± 13.8 | 18 (3.0) | 2 (2.4) | |
| Prior antimicrobial resistance training | |||||
| Yes | 481 (70.6) | 85.3 ± 13.5 | 430 (72.1) | 51 (60.0) | 0.021* |
| No | 200 (29.3) | 84.2 ± 15.9 | 166 (27.9) | 34 (40.0) | |
*Statistically significant at P < 0.05
Knowledge of participants on antimicrobial resistance and rational use of medicine
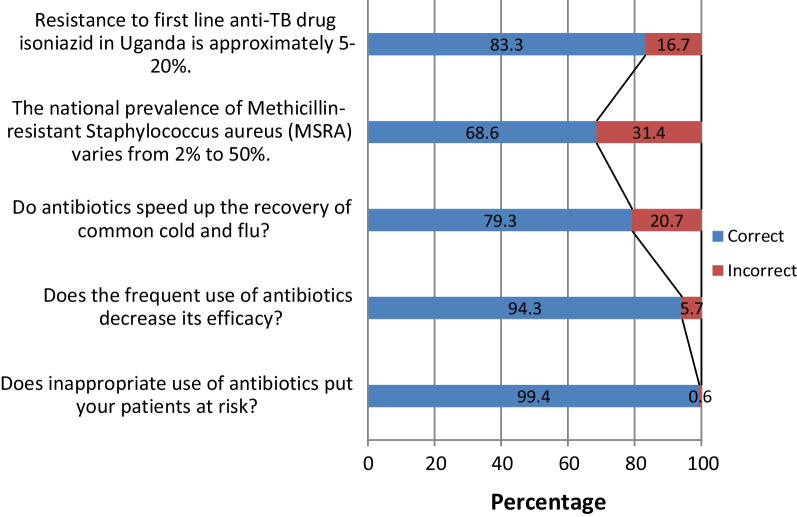
Most participants (n = 596, 87.5%) had sufficient knowledge about AMR with a mean score of 85 ± 14.2%. A higher proportion of female than males participants (54.5% vs. 45.5%, p = 0.049) and those who had received a prior training on AMR than not (72.1% vs. 27.9%, p = 0.021) had sufficient knowledge (Table 1). Majority of students knew the fact that antibiotics don’t speed up recovery of common cold (n = 540, 79.3%), Fig. 1. On bivariate analysis, sex (p = 0.049), course (p = 0.016), university (p = 0.014) and prior training on AMR (p = 0.021) were significantly associated with knowledge on AMR, Table 1. However, they all lost significance at multivariate logistic regression analysis.
Fig. 1.
Responses participants to knowledge questions on antimicrobial resistance
There was a statistically significant difference in level of knowledge on AMR across year of study (p < 0.001) and course (p = 0.006). Mean knowledge scores of fourth year students were significantly higher than those of third year (86.6% vs. 82.4%, p = 0.002), and fifth-year students higher than those of third year students (88.0% vs. 82.4%, p < 0.001). There was no significant difference between those of 4th and 5th year students (p = 0.622). Also, the mean score of students pursuing MBChB (86.1%) was higher than those doing Nursing (82.3%) (p = 0.006), Table 2.
Table 2.
Post Hoc Tukey HSD results for comparison groups according to year of study and course
| comparison group | Mean 1 | Mean 2 | Mean difference | 95% CI of difference | p value |
|---|---|---|---|---|---|
| According to year of study | |||||
| Year 5 Vs. Year 4 | 88.03 | 86.64 | 1.391 | − 2.125 to 4.907 | 0.622 |
| Year 5 Vs. Year 3 | 88.03 | 82.36 | 5.679 | 2.372 to 8.969 | < 0.001* |
| Year 4 Vs. Year 3 | 86.64 | 82.36 | 4.280 | 1.378 to 7.182 | 0.002* |
| According to course of study | |||||
| Medicine and Surgery vs. Nursing | 86.14 | 82.33 | 3.813 | 0.8254 to 6.801 | 0.006* |
| Medicine and Surgery vs. Pharmacy | 86.14 | 86.40 | − 0.2568 | − 7.518 to 7.004 | > 0.999 |
| Medicine and Surgery vs. Dental Surgery | 86.14 | 91.11 | − 4.968 | − 16.86 to 6.920 | 0.754 |
| Medicine and Surgery vs. Anesthesia | 86.14 | 77.50 | 8.643 | − 3.952 to 21.24 | 0.304 |
*Statistically significant at P < 0.05
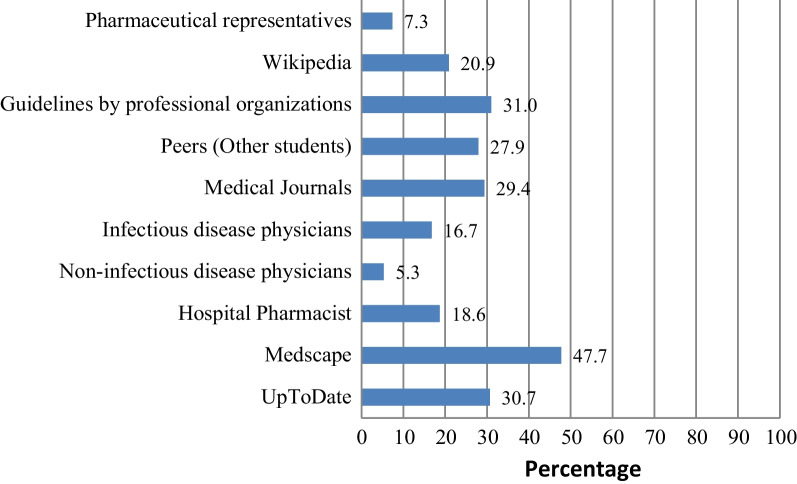
On rational use of medicine, most participants reported awareness of the terms rational use of medicine (n = 631, 92.7%), essential medicine list (n = 586, 86.1%) and could name parts of a prescription (n = 600, 88.1%), Table 3. Most participants used Medscape (47.7%) as the major source of information on AMR and rational use of medicine, Fig. 2.
Table 3.
Responses of participants on knowledge questions on rational use of medicine
| Question | Yes frequency (%) | No frequency (%) |
|---|---|---|
| Are you aware of the term Rational use of medicine? | 631 (92.7) | 50 (7.3) |
| Are you aware of the term essential medicines Lists (EML)? | 586 (86.1) | 95 (13.9) |
| Are you aware of the term P-drugs? | 505 (74.1) | 176 (25.8) |
| Can you name the parts of a prescription? | 600 (88.1) | 81 (11.9) |
| Are you aware of STEP (Safety, tolerability, efficacy, price) criteria for selection of P-drug? | 459 (67.4) | 222 (32.6) |
Fig. 2.
Sources of Information on antimicrobial resistance and rational drug
Perceptions of participants towards and on their quality of training on antimicrobial resistance
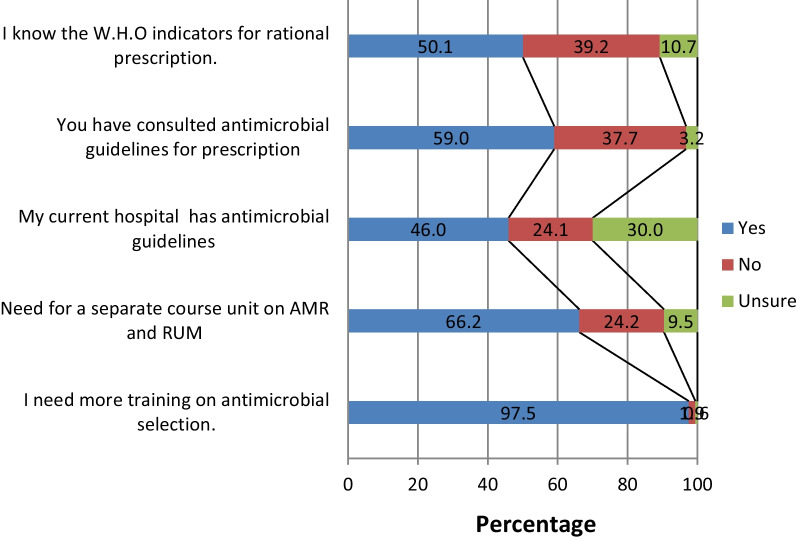
Over half of the participants (n = 371, 54.5%) agreed that antimicrobials were overused at their university teaching hospitals and that poor infection control practices by healthcare professionals causes spread of antimicrobial resistance (n = 318, 46.7%). About a third of the students (n = 277, 40.7%) thought that new antimicrobials will be developed in the future to keep up with the escalating problem of antimicrobial resistance (Table 4). Most participants (97.5%) agreed that they need more training on antimicrobial selection and a separate course unit on AMR and rational use of medicine (66.2%), (Fig. 3).
Table 4.
Perceptions of participants towards antimicrobial resistance
| Statement | SA (n, %) | A (n, %) | N (n, %) | D (n, %) | SD (n, %) |
|---|---|---|---|---|---|
| Prescribing broad-spectrum antimicrobials when equally effective narrower spectrum antimicrobials are available increases antimicrobial resistance | 480 (70.5) | 163(23.9) | 16 (2.4) | 14 (2.1) | 8 (1.2) |
| Strong knowledge of antimicrobials is important in my medical career | 520 (76.4) | 155 (22.8) | 6 (0.8) | 0 (0) | 0 (0) |
| Poor infection control practices by healthcare professionals cause spread of antimicrobial resistance | 318 (46.7) | 303 (44.5) | 32 (4.7) | 21 (3.1) | 7 (1.0) |
| Excessive use of antimicrobials in livestock causes antimicrobial resistance | 301 (44.2) | 277 (40.7) | 71 (10.4) | 30 (4.4) | 2 (0.3) |
| New antimicrobials will be developed in the future that will keep up with the problem of resistance | 110 (16.2) | 277 (40.7) | 170 (24.9) | 99 (14.5) | 25 (3.7) |
| Antimicrobials are overused at the hospitals where I have rotated | 196 (28.8) | 371 (54.5) | 91 (13.4) | 22 (3.2) | 1 (0.2) |
SA strongly agree, A agree, N neutral, D disagree, SD strongly disagree
Fig. 3.
Perception of participants on their training on antimicrobial resistance and rational use of medicine
Confidence level of participants on prescribing antimicrobials
Two thirds of the participants (n = 456, 66.9%), were confident on making an accurate diagnosis of infection/sepsis, choosing the correct antimicrobial to use (n = 484, 71.1%) and using a combination therapy if appropriate (n = 443, 65.1%), (Table 5). There was a statistically significant difference in confidence level scores among classes with highest scores among year 5 on making an accurate diagnosis of infection/sepsis (p < 0.001), choosing the correct antimicrobial to use (p = 0.019), choosing the correct dose and interval of administration (p = 0.019) among others.
Table 5.
Confidence level of clinical year medical students to prescribe antimicrobials
| Statement | VC (n, %) | C (n, %) | U (n, %) | UC (n, %) | VUC (n, %) |
|---|---|---|---|---|---|
| Making an accurate diagnosis of infection/sepsis | 121(17.8) | 456 (66.9) | 24 (3.5) | 54 (7.9) | 26 (3.8) |
| Choosing the correct antimicrobial to use | 72 (10.6) | 484 (71.1) | 24 (3.5) | 82 (12.0) | 19 (2.8) |
| Choosing the correct dose and interval of administration | 86 (12.6) | 439 (64.5) | 26 (3.8) | 108 (15.9) | 22 (3.2) |
| Using a combination therapy if appropriate | 67 (9.8) | 443 (65.1) | 31 (4.6) | 115 (16.9) | 25 (3.7) |
| Choosing between intravenous and oral administration | 115 (16.9) | 458 (67.2) | 22 (3.2) | 63 (9.3) | 23 (3.4) |
| Planning to streamline/stop the antimicrobial treatment, according to clinical evaluation and investigations | 66 (9.7) | 425 (62.4) | 63 (9.3) | 106 (15.6) | 21 (3.1) |
VC very confident, C confident, U uncertain, UC unconfident, VUC very unconfident
Discussion
The greatest increase in AMR and related deaths are estimated to occur in sub-Saharan Africa if nothing is done to avert the current trends [24]. This study explored the knowledge, confidence level of prescription, perceptions on antimicrobial resistance and training on antimicrobial use of health professions students in Uganda.
Our findings suggest that almost 9 in 10 participants had sufficient knowledge about AMR, especially the male students and those that had received prior additional training on AMR. This finding is in agreement with earlier findings around medical students in, Nigeria [25], Egypt [26], South Africa [27] and China [14, 28] which showed that medical students generally were more knowledgeable about antibiotics use. Contrary to this, previous findings among final year medical students in Uganda and Kenya report otherwise; only 36.6% (120/328) of students had good overall total knowledge [29]. The variations in the findings of these studies could be attributed to the fact that our study had a larger sample size i.e., 681 participants from 9 medical schools versus 328 participants in a study by Lubwama et al., 2021 from 3 medical Schools [29]. Furthermore, our study included students pursuing other medical courses i.e., Bachelor of Dental Surgery (BDS), Bachelor of Science in Nursing (BNS), and Bachelors of Anesthesia (BNA) which is not the case with the other study. Our findings are also contrary to previous studies in other parts of the world that reported limited knowledge amongst final year medical students; in Thailand [30] and Australian [31]. Such discrepancies could probably be due to the geographical reasons where diseases targeted by antibiotics may not be equally prevalent in the respectively settings. Also, the differences in medical curricula used, could also have an impact on the overall students’ knowledge regarding antibiotic use and antimicrobial resistance.
The knowledge scores of students on AMR increased up the years peaking at fifth year and a significant knowledge difference was observed among third years against fourth and fifth years. Also, the medicine students scored significantly higher than nursing students on AMR knowledge. Similar findings are drawn from other studies in Malaysia and China [2, 14]. As students’ progress in their respective academic programs, they get more encounters with antimicrobials, start prescribing and administering them under supervision thus garner more knowledge. Despite our study not showing a strong evidence on the effect of sex on AMR, males have been found to have poorer levels of knowledge compared to females [26].
Students in our study mainly used Medscape (47.7%), guidelines from professional bodies (31.0%), and UpToDate (30%) and as their sources of information on AMR. This is however in disagreement, with an earlier study among Chinese medical students which found textbooks or study guides, peers, and Wikipedia to be the topmost used resources of information [28]. There is need to ensure that medical students use the right information sources to help them acquire quality and updated good AMR knowledge. Over the past decades, there has been a significant increase in the number of educational websites and smartphone applications with information on drug prescriptions. Some of these include in addition to UpToDate, drugs.com, Medline, WebMD, Mayo Clinic, rxlist.com, goodrx.com, etc. Health professional students can utilize these readily available sources to improve their prescription practices.
It is encouraging to realize that most students in our study (over 80%) were aware about the essential medicines, and rational use of medicine, and could name prescription parts. This is a good indicator on their pharmacological training that could translate into better practices towards use of antimicrobials. The majority also appreciated the fact that antibiotics don’t speed up recovery of common cold because this is a great contributor to misuse of antibiotics. Over half of the students (54.5%) reported that antimicrobials were overused at their university teaching hospitals. This is consistent with several other Global Point Prevalence surveys done in hospitals in Uganda, Tanzania, Ghana, and other international reviews [32–34]. This shines a light on the pressing drivers of resistance that should be addressed within our hospitals by establishment of medicines and therapeutic committees, and/or infection prevention committees in which students’ representatives can be invited to become members.
About two-thirds of participants in our study believed that strong knowledge of antimicrobials is important in for their medical career. This result has also been previously documented among Chinese medical student by Yang et al.,2016[15]. The role of having strong antimicrobial knowledge can’t be overemphasized in antimicrobial stewardship, because it’s what drives antibiotics prescribing behaviors of health care workers [28]. There is need for more efforts to be directed towards improvement of medical students’ knowledge of antibiotics and their rational use of medicines, among especially those medical students with poor knowledge, attitudes and perception regarding AMR for example among Japanese medical students, of whom only 43 (6.5%) had ever heard about the AMR [35].
Unlike several systematic reviews that have consistently reported unpreparedness and low self-reported confidence of medical students to prescribe antimicrobials [21, 36, 37], majority of our respondents were confident on choosing the correct antimicrobial to use (71.1%) and using a combination therapy if appropriate (65.1%). This could be due to for instance having 430 (89.4%) of students in our sample having had prior AMR training. Furthermore, the level of confidence was significantly highest among fifth year students possibly because they are the most senior and have encountered patients and prescriptions often. But this is also an encouraging finding as these confident students are soon entering into the health system. Thus, the confidence exhibited should be built on to create strong stewardship towards AMR.
Although students exhibited high confidence and good knowledge, almost all of them (97.5%) believed they need more training on antimicrobial selection and a separate course unit on AMR and rational use of medicine. This is in consonance with various other KAP studies on AMR among students [14, 19, 38] which underscores the need to rethink the medical curriculum in line with delivery of pharmacology course to put emphasis on antimicrobial prescription and resistance. The largest proportion of students knew about their teaching hospital antimicrobial guidelines and had consulted them.
Limitations and strengths
This is a cross-sectional study that only provides a snippet of the prevailing situation at the time. The convenience sampling method used could have created bias in the different categories with few numbers represented in some however we tried to control for this by consistently sharing the tool across all groups. The use of WhatsApp as a data collection platform presents challenges of who accesses the data collection tool link that we could not completely control however we tried correcting for this by having focal persons per participating site to only share in specified groups with the targeted population. However, our study involved many health professions students across different universities and courses therefore the findings can be generalized with much confidence.
Conclusion
This survey indicates that there is good knowledge among health profession students on antimicrobial resistance and rational use of medicine however they still demanded that a separated course on this is necessary. Responsible authorities should consider introducing this course unit in the curriculum of medical schools to consolidate this knowledge that can translate into good practices of antimicrobial use. The high self-perceived confidence level of students on prescription of antimicrobials should be leveraged to encourage to translate the exhibited good knowledge into better practice later when they start prescribing antimicrobials without supervision (Additional file 1).
Supplementary Information
Acknowledgements
The authors would like to acknowledge all the medical students who spared their time to make this study possible are highly appreciated.
Abbreviations
- AMR
Antimicrobial resistance
- WHO
World Health Organization
- INRUD
International Network of Rational Use of Drugs
- MBChB
Bachelor of Medicine and Bachelor of Surgery
- BDS
Bachelor of Dental Surgery
- BNS
Bachelor of Science in Nursing
- BPharm
Bachelor of Pharmacy
- BNA
Bachelors of Anesthesia
Author contributions
AMK, KK, and OS conceptualized and designed the study protocol. OR, JK, DO, DRN, JFA, LA, KA, DA, NKW, RB, GN, RK, RL, WO, DM and PM participated in data collection. AMK, RO and FB analyzed the data. AMK, JK, RO, and OS drafted the original manuscript. All authors reviewed and approved the final manuscript.
Funding
This study was not funded by any organization.
Availability of data materials
The data collection tool used for this study is attached. All data generated or analyzed during the current study is not publicly available due to some individualized information it contains but are available from the corresponding author on reasonable request.
Declarations
Ethical Approval and consent to participate
The study was conducted according to the Declaration of Helsinki and in line with the principles of Good Clinical Practice and Human Subject Protection. Prior to collecting data, we sought ethical clearance from the Research Ethics Committee of Cure Children’s Hospital of Uganda (CCHU-REC) approval number CCHU-REC/04/021. The students were informed that participation in the study was voluntary, and an electronic informed consent was sought on the initial page of the questionnaire. Participant’s personal identifiers like email, home address, identification numbers or mobile numbers were not collected to ensure privacy and confidentiality.
Consent for publication
Not applicable.
Competing Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Afzal Khan AK, Banu G, Reshma KK. Antibiotic resistance and usage-a survey on the knowledge, attitude, perceptions and practices among the medical students of a southern Indian teaching hospital. J Clin Diagn Res. 2013;7(8):1613–1616. doi: 10.7860/JCDR/2013/6290.3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kanneppady S, Oo A, Lwin O, Ahmed Al-Abed AA, Kanneppady S. Knowledge, attitude, and awareness of antibiotic resistance among medical students. Arch Med Health Sci. 2019;7(1):57. doi: 10.4103/amhs.amhs_104_18. [DOI] [Google Scholar]
- 3.Hoque R, Mostafa A, Haque M. Insight of medical students of clinical years to antimicrobials prescribing and resistance in private medical school, Chittagong, Bangladesh. J Young Pharm. 2016;8(4):447–455. doi: 10.5530/jyp.2016.4.22. [DOI] [Google Scholar]
- 4.Abbo LM, Cosgrove SE, Pottinger PS, Pereyra M, Sinkowitz-Cochran R, Srinivasan A, et al. Medical students’ perceptions and knowledge about antimicrobial stewardship: How are we educating our future prescribers? Clin Infect Dis. 2013;57(5):631–638. doi: 10.1093/cid/cit370. [DOI] [PubMed] [Google Scholar]
- 5.Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Robles Aguilar G, Gray A, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022 doi: 10.1016/S0140-6736(21)02724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kivumbi MT, Standley CJ. Efforts to identify and combat antimicrobial resistance in Uganda: a systematic review. Trop Med Infect Dis. 2021;6(2):86. doi: 10.3390/tropicalmed6020086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Obakiro SB, Kiyimba K, Paasi G, Napyo A, Anthierens S, Waako P, et al. Prevalence of antibiotic-resistant bacteria among patients in two tertiary hospitals in Eastern Uganda. J Glob Antimicrob Resist. 2021;25:82–86. doi: 10.1016/j.jgar.2021.02.021. [DOI] [PubMed] [Google Scholar]
- 8.WHO. Global Antimicrobial Resistance Surveillance System (GLASS) Report. Geneva, World Health Organization. Who. 2017. 268 p.
- 9.Ghadeer ARY, Mayadah S, Dana AD. A cross-sectional study on knowledge, attitude and behavior related to antibiotic use and resistance among medical and non-medical university students in Jordan. Afr J Pharm Pharmacol. 2012;6(10):763–770. [Google Scholar]
- 10.Hay SI, Rao PC, Dolecek C, Day NPJ, Stergachis A, Lopez AD, et al. Measuring and mapping the global burden of antimicrobial resistance. BMC Med. 2018;16(1):1–3. doi: 10.1186/s12916-018-1073-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guzmán-Álvarez R, Medeiros M, Reyes Lagunes LI, Campos-Sepúlveda AE. Knowledge of drug prescription in dentistry students. Drug Healthc Patient Saf. 2012;4(1):55–59. doi: 10.2147/DHPS.S30984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amaha ND, Weldemariam DG, Abdu N, Tesfamariam EH. Prescribing practices using WHO prescribing indicators and factors associated with antibiotic prescribing in six community pharmacies in Asmara, Eritrea: a cross-sectional study. Antimicrob Resist Infect Control. 2019;8(1):1–7. doi: 10.1186/s13756-019-0620-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shahroom NSB, Lakshmi T, Roy A. Knowledge of drug prescription among dental and medical student in India–an online survey. J Adv Pharm Educ Res. 2017;7(2):76–81. [Google Scholar]
- 14.Huang Y, Jiarui Gu, Zhang M, Ren Z, Yang W, Chen Y, Yingmei Fu, Chen X, Cals JWL, Zhang F. Knowledge, attitude and practice of antibiotics: a questionnaire study among 2500 Chinese students. BMC Med Educ. 2013 doi: 10.1186/1472-6920-13-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang K, Wu D, Tan F, Shi S, Guo X, Min Q, et al. Attitudes and perceptions regarding antimicrobial use and resistance among medical students in Central China. Springerplus. 2016;5(1):1779. doi: 10.1186/s40064-016-3454-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ministry of National Health Services Regulations & Coordination Government of Uganda. Antimicrobial Resistance National Action Plan. Uganda Government. 2017;6(May):1–174.
- 17.Ibia E, Sheridan M, Schwartz R. Knowledge of the principles of judicious antibiotic use for upper respiratory infections: a survey of senior medical students. South Med J. 2005;98(9):888–894. doi: 10.1097/01.smj.0000177439.89762.ee. [DOI] [PubMed] [Google Scholar]
- 18.Eyal L, Cohen R. Preparation for clinical practice: a survey of medical students’ and graduates’ perceptions of the effectiveness of their medical school curriculum. Med Teach. 2006;28(6):e162–e170. doi: 10.1080/01421590600776578. [DOI] [PubMed] [Google Scholar]
- 19.Minen MT, Duquaine D, Marx MA, Weiss D. A survey of knowledge, attitudes, and beliefs of medical students concerning antimicrobial use and resistance. Microb Drug Resist. 2010;16(4):285–289. doi: 10.1089/mdr.2010.0009. [DOI] [PubMed] [Google Scholar]
- 20.Haque M, Rahman NIA, Zulkifli Z, Ismail S. Antibiotic prescribing and resistance: Knowledge level of medical students of clinical years of university Sultan Zainal Abidin, Malaysia. Ther Clin Risk Manag. 2016;12:413–426. doi: 10.2147/TCRM.S102013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brinkman DJ, Tichelaar J, Graaf S, Otten RHJ, Richir MC, van Agtmael MA. Do final-year medical students have sufficient prescribing competencies? A systematic literature review. Br J Clin Pharmacol. 2018;84(4):615–635. doi: 10.1111/bcp.13491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hooli TV, Srikanth SS, Suraj B. Knowledge, attitude, practice of rational use of medicines among junior residents in a tertiary care hospital. Int J Basic Clin Pharmacol. 2017;6(8):2001. doi: 10.18203/2319-2003.ijbcp20173286. [DOI] [Google Scholar]
- 23.Seid MA, Hussen MS. Knowledge and attitude towards antimicrobial resistance among final year undergraduate paramedical students at University of Gondar, Ethiopia. BMC Infect Dis. 2018;18(1):1–8. doi: 10.1186/s12879-018-3199-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.IACG. No time to wait: securing the future from drug-resistant infections. Report to the Secretary-General of the United Nations. 2019.
- 25.Alex IO. Knowledge of antibiotic use and resistance among students of a medical school in Nigeria. Malawi Med J. 2019;31(2):133. doi: 10.4314/mmj.v31i2.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Assar A, Abdelraoof MI, Abdel-Maboud M, Shaker KH, Menshawy A, Swelam AH, et al. Knowledge, attitudes, and practices of Egypt’s future physicians towards antimicrobial resistance (KAP-AMR study): a multicenter cross-sectional study. Environ Sci Pollut Res. 2020;27(17):21292–21298. doi: 10.1007/s11356-020-08534-5. [DOI] [PubMed] [Google Scholar]
- 27.Wasserman S, Potgieter S, Shoul E, Constant D, Stewart A, Mendelson M, et al. South African medical students’ perceptions and knowledge about antibiotic resistance and appropriate prescribing: Are we providing adequate training to future prescribers? S Afr Med J. 2017;107(5):405. doi: 10.7196/SAMJ.2017.v107i5.12370. [DOI] [PubMed] [Google Scholar]
- 28.Hu Y, Wang X, Tucker J, Little P, Moore M, Fukuda K, et al. Knowledge, attitude, and practice with respect to antibiotic use among Chinese medical students: a multicentre cross-sectional study. Int J Environ Res Public Health. 2018;15(6):1165. doi: 10.3390/ijerph15061165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lubwama M, Onyuka J, Ayazika KT, Ssetaba LJ, Siboko J, Daniel O, et al. Knowledge, attitudes, and perceptions about antibiotic use and antimicrobial resistance among final year undergraduate medical and pharmacy students at three universities in East Africa. PLoS ONE. 2021;16(5):e0251301. doi: 10.1371/journal.pone.0251301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chuenchom N, Thamlikitkul V, Chaiwarith R, Deoisares R, Rattanaumpawan P. Perception, attitude, and knowledge regarding antimicrobial resistance, appropriate antimicrobial use, and infection control among future medical practitioners: a multicenter study. Infect Control Hosp Epidemiol. 2016;37(5):603–605. doi: 10.1017/ice.2016.8. [DOI] [PubMed] [Google Scholar]
- 31.Weier N, Thursky K, Zaidi STR. Antimicrobial knowledge and confidence amongst final year medical students in Australia. PLoS ONE. 2017;12(8):e0182460. doi: 10.1371/journal.pone.0182460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.D’Arcy N, Ashiru-Oredope D, Olaoye O, Afriyie D, Akello Z, Ankrah D, et al. Antibiotic prescribing patterns in Ghana, Uganda, Zambia and Tanzania hospitals: results from the global point prevalence survey (G-PPS) on antimicrobial use and stewardship interventions implemented. Antibiotics. 2021;10(9):1122. doi: 10.3390/antibiotics10091122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Versporten A, Zarb P, Caniaux I, Gros MF, Drapier N, Miller M, et al. Antimicrobial consumption and resistance in adult hospital inpatients in 53 countries: results of an internet-based global point prevalence survey. Lancet Glob Health. 2018;6(6):e619–e629. doi: 10.1016/S2214-109X(18)30186-4. [DOI] [PubMed] [Google Scholar]
- 34.Saleem Z, Hassali MA, Godman B, Versporten A, Hashmi FK, Saeed H, et al. Point prevalence surveys of antimicrobial use: a systematic review and the implications. Expert Rev Anti Infect Ther. 2020;18(9):897–910. doi: 10.1080/14787210.2020.1767593. [DOI] [PubMed] [Google Scholar]
- 35.Hagiya H, Ino H, Tokumasu K, Ogawa H, Miyoshi T, Ochi K, et al. Antibiotic literacy among Japanese medical students. J Infect Chemother. 2020;26(10):1107–1109. doi: 10.1016/j.jiac.2020.06.021. [DOI] [PubMed] [Google Scholar]
- 36.Monrouxe LV, Grundy L, Mann M, John Z, Panagoulas E, Bullock A, et al. How prepared are UK medical graduates for practice? A rapid review of the literature 2009–2014. BMJ Open. 2017;7(1):e013656. doi: 10.1136/bmjopen-2016-013656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cameron A, Millar J, Szmidt N, Hanlon K, Cleland J. Can new doctors be prepared for practice? A review. Clin Teach. 2014;11(3):188–192. doi: 10.1111/tct.12127. [DOI] [PubMed] [Google Scholar]
- 38.Dyar OJ, Nathwani D, Monnet DL, Gyssens IC, Stålsby Lundborg C, Pulcini C, et al. Do medical students feel prepared to prescribe antibiotics responsibly? Results from a cross-sectional survey in 29 European countries. J Antimicrob Chemother. 2018;73(8):2236–2242. doi: 10.1093/jac/dky150. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data collection tool used for this study is attached. All data generated or analyzed during the current study is not publicly available due to some individualized information it contains but are available from the corresponding author on reasonable request.