Abstract
Background
While morphological changes to the cervical spine have been observed for over 40 years in response to contact sport participation, little is known about the secondary effects of the cervical impairment on future musculoskeletal injury and disability.
Objectives and design
A scoping review was performed to discuss the relationship between contact sport participation and morphological changes to the cervical spine. Moreover, the correlation between morphological changes in the musculoskeletal structures of the cervical spine and resultant deficits in cervical sensorimotor and neuromotor function are discussed. Lastly, how alterations in cervical sensorimotor function may affect overall risk of musculoskeletal injury is discussed.
Methods
The scientific literature was searched in PubMed, Sport Discus, and Web of Science pertaining to contact-sport athletes and/or cervical pathology and the cervicocephalic network. The Asksey and O’Malley’s framework and PRISMA for Scoping Reviews were used to conduct and report the following review. Included articles were grouped into three categories: (1) Morphological changes to the cervical spine in contact sport athletes. (2) The role of the neuromotor pathways of the cervical spine in maintenance of postural tone and coordination of the extremities. (3) The correlation between altered cervical sensorimotor function and a resultant increase in musculoskeletal injury risk.
Results
Our search identified 566 documents, of which 405 underwent full-text screening, resulting in 54 eligible studies for the review. Widespread cervical sensorimotor dysfunction was observed in contact sport athletes. Independently, cervical sensorimotor function was demonstrated to play a critical role in postural control and limb coordination. However, limited research exists exploring the interaction between contact sport participation and altered cervical sensorimotor function, as well as an associated increase in musculoskeletal injury risk.
Conclusions
Limited evidence exists linking cervical injury and/or observed deficits in cervical sensorimotor and neuromotor function to musculoskeletal injury risk. Longitudinal studies combining imaging measures (e.g., MRI, DEXA), cervical functional test, and prospective injury risk are needed to further explore the correlation between resultant cervical sensorimotor deficits following contact sport impacts and future musculoskeletal injury risk.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12998-022-00458-w.
Keywords: Contact sport, Cervical spine, Musculoskeletal injury
Background
For over 40 years, morphological changes to the musculoskeletal structures of cervical spine have been observed in contact sport athletes [1–4]. These changes are thought to be a result of mechanical loads to the musculoskeletal structures of the cervical spine, which modulate up to 80% of the mechanical forces applied to the body following sports-related repetitive head impacts (RHI) [5]. RHI are thought to play a catalytic role in early degeneration of the cervical spine, including cervical stenosis, degenerative disk disease, osteoarthritis, and spondylosis/spondylolisthesis [3, 6–9]. Moreover, acute musculoskeletal injuries to the cervical spine, such as cervical strains, fractures, and sprains, frequently develop into more chronic disability lasting up to 24 months and beyond [10, 11]. Understanding the relationship between RHI and degeneration of the musculoskeletal components of the cervical spine is critical to weigh the risks and benefits of contact sport participation [12].
In addition to the morphological changes to the musculoskeletal structures of the cervical spine, alterations in the neuromotor and sensory pathways of the cervical spine have been identified in contact sport athletes. For example, alterations in cervical joint position error, cervical strength, and cervical range of motion have been observed in individuals with a history of contact sport participation as well as following exposure to instrumented RHI [13–16]. Preliminary studies have subsequently linked decreased cervical joint position error, cervical weakness, decreased static posture, and inhibited trunk activation to an increased risk of suffering future injury (e.g., lateral ankle sprain, anterior cruciate ligament tear, concussion) [17–19]. These studies highlight preliminary evidence of a relationship between RHI and future injury through alterations in the neuromotor pathways and decreased functional capacities of the cervical spine. The neuromuscular and sensory pathways of the cervical spine and brain form the cervicocephalic connection, which serves as a vital component of postural tone and neuromuscular coordination [20–23]. Cervical afferent signals work synergistically with efferent motor signals to coordinate the position of limbs throughout sports-related task [20–22, 24].
Despite frequent observations of cervical deficits in contact sport athletes, little research has focused on how those morphological changes impact the complex neurological connections between the brain and the cervical spine, which form the cervicocephalic connection. Moreover, limited research has investigated the connection between cervical deficits and prospective musculoskeletal injury risk, despite the strong documented relationships between the cervicocephalic pathways and neuromotor coordination of the limbs [20, 21, 25].
Due to the paucity of research in understanding the direct causal relationship between RHI and subsequent increased cervical dyskinesia, we established the following purposes for this scoping review: (1) Summarize evidence detailing acute and chronic morphological changes to the cervical spine in response to exposure to contact sport participation. (2) Briefly describe the cervicocephalic network and its role in proper maintenance of head position, postural tone, and coordination of the extremities. (3) Summarize existing research pertaining to a theoretical likelihood of an increase in injury risk due to altered cervical sensorimotor function in a useful way for practitioners and other relevant stakeholders. (4) Identify gaps in existing literature detailing the connection between contact sport participation, cervical disability, decreased cervical sensorimotor function, and consequential resultant changes in musculoskeletal injury risk.
Methods
We conducted a scoping review, as this approach is superior in addressing an exploratory research question [26–28]. Working within the preferred reporting items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR), we followed the framework of Arksey and O’malley [26], incorporating adaptations from Levac et al. and Joanna Briggs Institute [28, 29]. At the initiation of this review, there were no databases for registering a priori scoping review strategies.
Stage 1: Identify the research question(s)
Research Questions:
What is known about damage to the cervical spine and neuropathways in response to contact sport participation?
What is the role of cervical sensorimotor function in posture maintenance and neuromuscular control of the extremities?
What is the relationship between changes in cervical sensorimotor, neuromuscular control deficits, and increased risk of injury?
Stage 2: Identify relevant studies
Inclusion Criteria
Articles of any study design or source (peer-reviewed, grey literature, reviews)
All age groups and sexes
Contact sport athletes (e.g., hockey, lacrosse, American football, soccer, rugby, Australian football, wrestling)
Musculoskeletal injury, head impacts, and or degenerative condition affecting the cervical spine
Exclusion Criteria
Abstracts where no full-text was available
Case reports
Not published in the English language
Step 1 Initial limited search
An initial limited search (May 2021) was conducted. The search terms used were “contact sport” AND “cervical spine”. A total of 122 articles were reviewed. Twenty-two studies were included, with the references from those studies being reviewed for further relevant papers. The entire search strategy is detailed in Additional file 1: Appendix A.
Step 2 Identify key words and index terms
The title, abstract, and index terms used to describe the articles identified in step 1 were analyzed. The first search focused on prevalence of cervical pathology in contact sport athletes. Separately, articles that demonstrated the connections between cervical kinesthesia and postural control unrelated to contact sport participation were searched. Lastly, a search for studies that combined these two concepts was performed.
For the preliminary search ‘Cervical Spine’ and ‘Sport’ were set as the primary research terms. Secondary search terms (Additional file 1: Appendix A) were then added along with Boolean terms AND and OR. This process was then repeated with search terms ‘cervical kinesthesia’ and ‘posture’ to stratify evidence related to cervicocephalic connection. Lastly, ProQuest database as well as google scholar were searched to explore potential grey literature.
Step 3 Further Searching of references and citations
A final search of the reference list of identified articles was performed. A completed final search strategy is shown in Additional file 1: Appendix A.
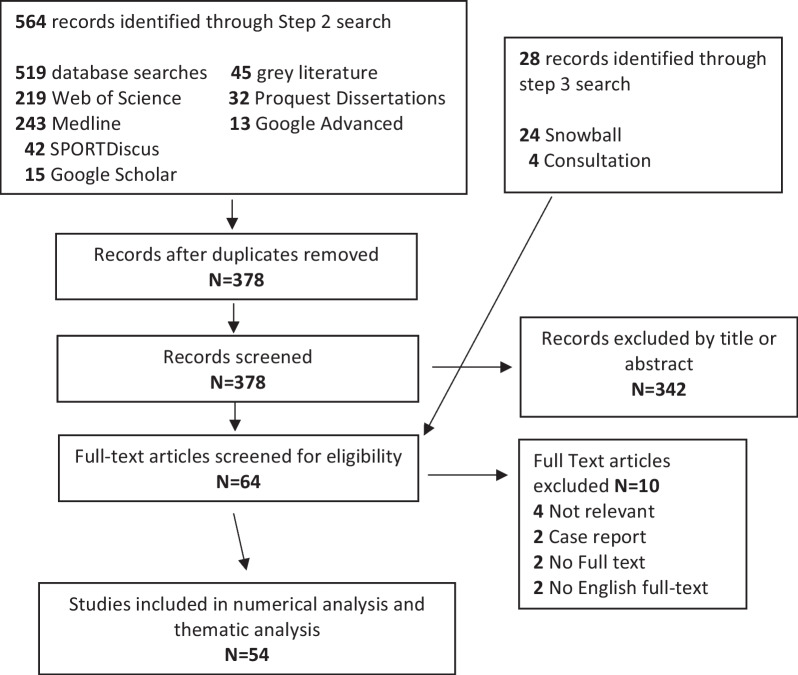
Stage 3: Study selection
Titles and abstracts were evaluated by two reviewers (KC and KK). A third reviewer (JK) completed a random sample of 20% of the titles and abstracts as a quality check and achieved concordance > 97% regarding the decision of each article [28–30]. Additional file 1: Appendix B details the selection and screening criteria. All titles and abstracts were reviewed independently, and any disagreement was discussed and the full-text was reviewed. A Prisma flow diagram (Fig. 1) details articles excluded at each step.
Fig. 1.
Scoping review flow chart
Stage 4: Charting the data
KC and KK independently trialed the data extraction form which included: author(s), year of publication, aims/purpose, participants, methodology, outcomes, intervention type, and key findings on 10 selected studies. Following this step, KC extracted data from 90% of included studies, and KK extracted data from 10% of the studies. Following data extraction, KC reviewed those studies extracted by KK while KK reviewed 10% of the studies that KC extracted. Ninety-five percent overall concordance was established, in agreement with previously published scoping reviews thus, no further cross-checking was performed [28, 29]. Table 1 presents a summary of each article identified in the scoping review.
Table 1.
Details of identified studies
| Author | Participants | Study design | Year | Intervention | Outcomes | Key findings |
|---|---|---|---|---|---|---|
|
Theme 1. Cervical spine and contact sport participation 1.1 Epidemiology of cervical injuries | ||||||
| Mueller [33] | N/A | Literature review | 1998 | N/A | N/A |
Dramatic reduction in fatalities 1975 through 1994 1976 rule change that prohibited initial contact with the head and face when blocking and tackling |
| Cantu [31] |
183 High School 29 Collegiate 7 Professional |
Retrospective review of injury records | 2003 | N/A | Catastrophic spine injuries in football |
Incidence rate of 0.52 in high school, 1.55 in college, and 14 in professional football for every 100,000 participants A 270% reduction in catastrophic injuries was observed following 1976 rule change |
| Fuller [39] | Professional Soccer athletes | Case control | 2005 | N/A | Cervical Injury rates |
Most frequent injuries were contusions (53%), lacerations (20%), and concussions (11%) The incidence of all head and neck injuries was 12.5/1000 player hours (men 12.8, women 11.5) and 3.7 for lost-time injuries (men 3.5, women 4.1) Frequent mechanisms of injury involved aerial challenges (55%) and use of the upper extremity (33%) or head (30%) |
| Nilsson [40] | 26 European soccer teams between 2001/2002 -2009/2010 | Prospective cohort study | 2013 | Professional Soccer participation |
Injury rate (number of time loss injuries per 1000 h) |
136 head and neck injuries were recorded (2.2% of all injuries) Injury rate was 0.17 (0.06 concussions) per 1000 h 20-fold higher rate of head and neck injury during match play compared with training (rate ratio[RR], 20.2; 95% [CI] 13.3–30.6) and a 78-fold higher rate of concussions (RR, 78.5; 95% CI 24.4–252.5) |
| Hutton [32] | N/A | Systematic review | 2016 | N/A | Incidence catastrophic cervical injuries |
Among Rugby Union players, incidence of catastrophic cervical spine injury (CCSI) was 4.1 per 100,000 player-hours Among NFL players, the CCSI rate was 0.6 while collegiate rate ranged from 1.1 to 4.7 per 100,000 player-years CCSI rate of 1.4–7.2 per 100,000 player-years |
| Meron [36] | National High School Sports-related Injury Surveillance system | Retrospective review of records | 2017 | N/A | Cervical spine injury rates |
1080 cervical spine injuries were reported during 35,581,036 athletic exposure (AE), resulting in an injury rate of 3.04 per 100,000 AE Cervical spine injuries were highest in football (10.10), wrestling (7.42) and gymnastics (4.95) Muscle injuries were the most common (63.1%), followed by nerve injuries (20.5%) The most common mechanisms of injury were contact with another player (70.7%) and contact with playing surface (16.1%) |
| Simmons [37] | Ice hockey NCAA Injury Surveillance Program 2009–2014 | Descriptive epidemiology study | 2017 | N/A | Head and neck Injury rates per 1000 AE |
Injury rate was higher in men than in women (1.75 vs. 1.16/1000 AE; CI = 1.25, 1.84) The most common head and neck injury was concussion; most concussions occurred in men's competitions from player contact while checking (25.9%) |
| Williams [38] | 3 NCAA Division I universities from 2007 to 2012 | Descriptive study | 2017 | Head and neck injury rates per 10,000 AE |
Overall injury rate was 35.2 per 10,000 athletic exposure (AE)s Rates for initial and subsequent injuries were 31.7 and 45.3 per 10,000 AEs, respectively, with a rate ratio (RR) of 1.4 for rate of subsequent injury vs rate of initial injury (95% CI 1.1–1.9) Subsequent injuries to the head, neck, and face were nearly double the rate of initial injury to same site (10.9 per 10,000 AEs, RR = 2.0; 95% CI 1.1–3.5) |
|
| Chung [34] | Collegiate football players in the NCAA database | Descriptive study | 2019 | N/A | Cervical spine injury rates |
300 cervical Injuries were identified in the data representing an estimated 7496 total cervical spine injuries extrapolated from the observed population to entire NCAA Injury rate of 2.91 per 10,000 AEs Most common was stinger with 1.8/10000 AEs and cervical strains with 0.8/10000 AEs Injuries were highest among defensive players |
| Lee [35] | High school and collegiate athletes from national sport injury surveillance databases | Retrospective record review | 2019 | N/A | Cervical injury counts and rates/10,000 AE |
The NCAA database reported 49 cervical muscle strains (rate = 0.96/10000 AEs), (57.1%) were time loss injuries (rate = 0.55/10, 000 AEs) High School databases reported 184 cervical muscle strains (rate = 1.66/10, 000 AEs), of which 33 (17.9%) were time-loss injuries (rate = 0.30/10,000 AEs) -The overall injury rate was lower among collegiate athletes than high school (injury rate ratio = 0.58; 95% CI = 0.42, 0.79) |
|
Theme 1. Cervical spine and contact sport participation 1.2 Morphological changes to the cervical spine in contact sport athletes | ||||||
| Sortland [3] |
43 national soccer players from Norway 43 matched control |
Cross-sectional | 1982 | Exposure to professional soccer | Spinal axis, healed fractures, cervical degenerative changes |
Compared with men of the same age group the onset of degeneration was 10–20 years earlier and the frequency of degeneration was significantly higher in retired professional soccer players Degenerative changes were not especially high in among individuals who reported higher heading frequency but this group had a higher frequency of subjective complaints and clinical findings such as reduced cervical movements |
| Kuman [43] | 30 Athletes | Cross-sectional observational | 1986 | Treatment of rest and traction versus referral for surgery |
Time to recovery radicular symptoms vs no radicular symptoms |
60% of radicular signs and symptoms were from the 4th and 5th cervical intervertebral space Roentgenographic changes were most common at the 4th and 5th cervical root Most cases responded favorably to conservative treatment of traction and rest Patients who presented with radicular signs and symptoms required up to 5 months to return while athletes with no radicular signs returned in less than 3 weeks |
| Tysvaer [47] | 69 active soccer players and 37 retired Norwegian national team members | Cross sectional | 1992 | Exposure to professional soccer | Computerized tomography electroencephalogram (EEG) |
Head injuries account for between 4 and 22% of soccer injuries There were fewer abnormal EEG changes among typical 'headers'(10%) than among 'nonheaders' (27%) One-third of the players were found to have central cerebral atrophy and 81% to have from mild to severe neuropsychological impairment The radiological examination of the cervical spine revealed a significantly higher incidence and degree of degenerative changes than in a matched control group |
| Torg [46] | 5 groups of individuals based on graded amount of years of exposure to football | Descriptive study | 1996 | Exposure to football | Torg ratio |
A torg ratio (Diameter of spinal canal/diameter of the vertebral body) of 0.80 or less had a high sensitivity (93%) for transient neurapraxia Developmental narrowing of the cervical canal in a stable spine does not appear to predispose an individual to permanent catastrophic neurological injury and therefore should not preclude an athlete from participation in contact sports |
| Quarrie [45] | N/A | Review article | 2002 | N/A | N/A |
Majority of injuries occur early in the season, when players are lacking both practice and physical conditioning for the physical contact phases of the sport Hookers and props have been at disproportionate risk of cervical spine injury, predominantly because the scrum was the phase of play most commonly associated with spinal injuries |
| Kartal [8] | 15 veteran, 15 current, 28 age matched controls soccer players | Cross-sectional descriptive study | 2004 | Exposure to soccer |
Cervical strength Cervical RoM Cervical X-ray Spinal cord compression |
Degenerative changes were prominent in veteran players, and the sagittal diameter spinal canal at C5 to C7 was lower when compared to active players and controls Magnetic resonance findings of degeneration were more prominent in soccer players when compared to their age-matched controls A tendency towards early degenerative changes exists in soccer players |
| Bailes [45] | Ten contact sport athletes | Cross-sectional Observation | 2005 | N/A | X-ray and CT with dynamic studies |
The occurrence of TSCI is not uncommon in athletes involved in contact sports Transient spinal cord injuries appear among those in yet whom radiographic studies are normal, and those with cervical stenosis, the later is the most difficult management group |
| Mehnert [9] | N/A | Review | 2005 | N/A | N/A |
Existing studies of long-term effects suggest a predisposition to degenerative changes of the cervical spine Further research in this area is needed with studies that assess biomechanical forces under simulated play conditions and control for impacts and stresses to the neck and spine that occur from non-heading activity |
| Ivancic [48] | 10 cadavers | Pre-post Experimental | 2013 | Crash simulation | Intact and postimpact flexibility test, axial torque and lateral bending |
Multidirectional instability of the upper cervical spine caused by atlas and dens fractures was evidenced by increases up to 53% in cervical flexion and extension due to impacts Increases in extension range of motion were 14.9 degrees in the upper cervical spine and 24.9 degrees (p < 0.05) at the middle cervical spine and in flexion at C7/T1 were 25.6 degrees |
| Brauge [42] |
101 former rugby players (mean age 40.4) 85 aged matched controls |
Cross-sectional | 2015 | Participation as a professional rugby athlete |
Japanese orthopaedic questionnaire Neck disability MRI |
Rugby players complained of chronic neck and decreased mobility pain more frequently (51 of 101 vs. 27 of 85, p = 0.01) Rugby players had a narrower vertebral canal(0.88 ± 0.167 cm vs. 0.99 ± 0.130 cm, p = 0.007) and more foraminal stenosis (p = 0.01) Rugby players had more often undergone surgery for a degenerative condition than controls (10 cases vs. 0, p = 0.0021) |
| Trewartha [49] | N/A | Literature Review | 2015 | N/A | N/A |
Scrummaging leads to premature chronic degeneration of the cervical spine Biomechanical studies of rugby scrummaging confirm that scrum engagement forces are high and multiplanar, but can be altered through modifications to the scrum engagement process to control engagement velocity The incidence of acute injury associated with scrummaging is moderate but the risk per event is high |
| Ndubuisi | 204 symptom free adults, 21–50 years of age | Cross-sectional | 2017 | Exposure to active leisure contact sports | Space available for the Cord (SAC) |
SAC at C3-4 was 4.39 ± 0.28 mm contact sport group and 4.90 ± 0.30 mm in controls (p = 0.036) and at C4-5 was 4.16 ± 0.27 mm contact sport group and 4.56 ± 0.35 mm (group B) Significant effect of contact sports (p = 0.005), sex (p = 0.001), and age (p = 0.0001) were observed in relation to SAC |
|
Theme 1. Cervical spine and contact sport participation 1.3 Return to play considerations | ||||||
| Cantu [51] | N/A | Informational | 1998 | N/A | Clinical criteria for diagnosis of cervical stenosis |
Spinal stenosis can't be defined by bone measurement alone as this fails to control for dural compression Patients with functional spinal stenosis recovery far less frequently than those who have structural narrowing of the spine as measured by radiography Radiography is critical for initial work up to clear subluxation or fracture when symptoms are present |
| Okonkwo [58] | N/a | Review | 2003 | N/A | N/A |
Two million persons suffer a head injury each year in the United States; of these, approximately 350,000 are sports- and recreation-related head injuries Between 12,000 and 15,000 cases of spinal cord injury occur each year in the United States, of which 10–15% are sports-related Traumatic brain injury is the most common cause of death in persons under 45 in the western world |
| Torg [59] | N/A | Systematic review | 2009 | N/A | N/A |
The overriding principle regarding the return to football or any collision activity should be that the individual is asymptomatic, pain-free, and neurologically intact and have full cervical strength and range of cervical motion Any injury to C1-C2 is an immediate contraindication to contact sport participation |
| Chao [52] | N/A | Review article | 2010 | N/A | N/A |
Catastrophic cervical injuries at are rare and account for less than 3% of cervical spine injuries Transient neurological episodes are estimated at 7/10,000 and typically resolve in 10–15 min but may last up to days Most frequent mechanism of brachial plexus injury is traction and are associated with athletes with a higher rate of cervical stenosis, disk disease and other degenerative conditions |
| Dailey [53] | N/A | Clinically based systematic review | 2010 | N/A | N/A |
Weak recommendation that patients with transient neuropraxia and radiographic evidence of cervical canal compromise should be withheld from participation in contact sports Strong recommendation that patients with transient neuropraxia without radiographic evidence of cervical stenosis can return to full sports activities |
| Kepler [55] | N/A | Expert opinion | 2012 | N/A | N/A |
Benign injury types such as isolated spinous process fractures or compression fractures can be treated with immobilization and typically do not preclude return to play once healed Complex injuries must be evaluated based on spinal stability, need for fusion, and the number of levels fused if necessary; fusion of 3 or more cervical levels is a contraindication to return to play Players with a third stinger in a single season or a recurrent transient quadriparesis must undergo imaging to rule out stenosis and parenchymal injury; return to play is dependent on resolution of symptoms and severity of episode |
| Mcana [57] | N/A | Commentary | 2014 | N/A | N/A |
Cervical spondylolysis, unlike lumbar spondylolysis, is an exceedingly rare only 150 have been reported Limited knowledge is known about RTP guidelines following cervical spondylolysis |
| Joaquim [54] | N/A | Systematic Review | 2016 | N/A | Relief of symptoms, RTP, career length after surgery, and permanent neurological deficits |
Return to play is safe for athletes who are asymptomatic after disk fusion for cervical radiculopathy due to disc herniation Surgical treatment may provide a higher rate of return to play for these athletes than nonsurgical treatment Cervical cord signal changes may not be an absolute contraindication for return to play in neurologically intact patients Cervical contusions secondary to cervical stenosis may be associated with a worse outcome and a higher recurrence rate than those secondary to disc herniation |
|
Theme 2: Cervical afferents and postural control 2.1 Artificially induced afferent cervical dysfunction alters neuromotor control and posture maintenance | ||||||
| McLain [23] | 21 cervical facet capsules, taken from three normal human subjects | Cross-sectional | 1994 | N/A |
Mechanorece-ptor count Nociceptive nerve ending count |
The presence of mechanoreceptive and nociceptive nerve endings in cervical facet capsules proves that these tissues are monitored by the central nervous system Protective muscular reflexes modulated by these types of mechanoreceptors are important in preventing joint instability and degeneration |
| Allum [20] |
4–10 controls 3–7 bilateral labyrinthine deficient patients (depending on experiment) |
Cross-sectional | 1997 | Labyrinthine deficient vs normal control |
EMG Head acceleration |
Head velocities observed during balance corrections depend to a large extent on the movements of the head-neck mass-viscoelastic system whose properties could be altered by co-contracting the neck muscles For experiments involving stance perturbations, much of the corrective response in neck muscles appeared to be triggered by trunk and leg proprioceptive signals Cervical reflexes modulate the amplitude of functionally stabilizing responses and dampen mechanically induced instability of the head and neck |
| MalmstrÃm [64] | 16 healthy subjects | Cross-sectional experimental | 2017 | Disturbance of cervical proprioception by vibration | Spatial body position |
Significant differences were seen in posturography between no vibration (628 mm or 25.1 mm/s) relative to each vibration condition When vibration was applied on the left-sided muscles, rotation to the right was induced (p = 0.005) Cervical proprioception is a critical component of internal spatial orientation and postural control |
|
Theme 2: Cervical afferents and postural control 2.2 Cervical pathology is linked to altered neuromotor control and poor posture maintenance | ||||||
| Karlberg [63] |
17 with cervicogenic dizziness 17 healthy controls |
Randomized controlled trial | 1996 | Physical therapy to reduce symptoms | Vibration-induced body sway, intensity and frequency of neck pain |
Neck pain patients manifested significantly poorer postural performance than did healthy subjects (0.05 > p > 0.0001) Physiotherapy significantly reduced neck pain and intensity and the frequency of dizziness (p < 0.01), and significantly improved postural performance (0.05 > p > 0.0007) |
| Sjostrom [66] |
25 whiplash participant 170 healthy age-matched control participants |
Cross-sectional | 2003 | Whiplash vs healthy | Trunk sway | Greater trunk sway for stance tasks and for complex gait tasks that required task-specific gaze control such as walking up and down stairs or walking while turning the head |
| Treleaven [68] |
100 whiplash participants (50 dizziness/50 no dizziness) 50 healthy controls |
Prospective observational design | 2005 | Whiplash with and without dizziness vs healthy control | Clinical test for sensory Interaction in balance |
Energy of the sway signal for comfortable stance tests was significantly greater in the group with dizziness compared with the group without dizziness Subjects with dizziness were significantly less able to complete the test than subjects without dizziness and controls after controlling for medications, compensation, anxiety or age and are likely to be due to disturbances to the postural control system possibly originating from abnormal cervical afferent input |
| Theme 3: Damage to cervical afferents and increased risk of injury | ||||||
| Treleaven [67] | N/A | Masterclass | 2008 | N/A | N/A |
The importance of the cervical reflex connections on postural control can be understood by observing changes in postural sway in response to artificial disturbances to the cervical afferents in asymptomatic individuals Dysfunction of the cervical receptors following injury to the cervical spine can alter afferent input subsequently changing the integration, timing and tuning of sensorimotor control of the extremities Afferent information from the cervical receptors can be altered via a number of mechanisms such as trauma and or functional impairment of the receptors, changes in muscle spindle sensitivity and the vast effects of pain at many levels of the nervous system |
| Freppel [62] |
17 patients with degenerative cervical spine disease 31 healthy controls |
Pre-test, post-test | 2013 | Surgery to correct either herniated disk or cervical degenerative disease |
Displacement in center of foot pressure Static posture tests |
C ontribution of visual input to postural control is reduced in a dynamic visual environment where cervical spine diseases is present The relative importance of visual and proprioceptive inputs to postural control varies according to the type of pathology and surgery tends to reduce visual contribution mostly in the spondylosis group |
| Treleaven | 140 whiplash patient | Randomized controlled trial | 2016 | whiplash vs healthy control | Static and dynamic clinical balance tests and cervical joint position error | Between and within group comparisons suggest that physiotherapist led neck exercise groups had advantages in improving measures of dizziness compared with the general physical activity group, although many still complained of dizziness and balance impairment |
| Wannaprom [69] |
30 adults withchronic neck pain 30 healthy control |
Cross-sectional | 2018 |
neck pain vs healthy control Vibration of suboccipital muscles |
Balance in a comfortable stance and timed gait test using a 10 m walk test |
At baseline, neck pain participants had greater postural sway, and slower gait speed than healthy controls (p < 0.001) Immediately after vibration, neck pain participants displayed decreased postural sway, and increased gait speed (p < 0.001) Neck muscle vibration improved standing balance and gait speed in participants with neck pain but reduced performance in healthy controls |
| Reddy [65] | 132 subjects with cervical spondylosis (CS) and 132 healthy age-matched control | Cross sectional | 2019 | Cervical JPE testing, neck pain assessment, |
Cervical spine injury subjects (CS) showed significantly larger cervical joint position sense error than healthy control subjects in all the directions tested(flexion, extension, right and left rotation) with a p value (< 0.001) Comparing all the movement directions in the CS and healthy control groups, the cervical joint position sense were largest in cervical extension (CS groups = 8.28° ± 1.80°; healthy group = 4.48° ± 1.26°) with standard error of measurements of 0.21° and minimal detectable change of 0.48° |
|
| Carrick [61] |
575 concussion patients 60 healthy controls |
Repeated measures experimental | 2020 |
Concussed vs healthy Changes in head position during static posture assessment |
Computerized dynamic posturographic measurement |
Postural stability scores are correlated with changes in head position in subjects following a concussion The position of the head and neck induced by statically maintained head turns is associated with significantly lower stability scores than the standardized head neutral position in Post-concussion Syndrome subjects but not in normal healthy controls Head positions on the neutral plane provide novel biomarkers that identify and differentiate subjects suffering from persistent post-concussion symptoms from healthy normal subjects |
| Hammerle | 48 post-concussion patients with dizziness | Retrospective record review | 2019 | Vestibular vs. cervical therapy | Improvement in dizziness | Patients who received cervical specific therapy were 30 times more likely to report improvement in dizziness symptoms compared with those who received vestibular therapy alone (adjusted odds ratio: 30.12; 95% confidence interval 4.44–204.26, p < 0.001) when cervical spine symptoms were present |
| Hides [72] |
190 Male rugby players 47 reported history of concussion |
Prospective cohort study | 2017 | History of reported concussion |
Balance Vestibular function Cervical Joint position error Trunk muscle function |
A history of concussion was related to changes in size and contraction of trunk muscles 22 (11.6%) players sustained a head/neck injury during the playing season of which 14 (63.6%) players had a previous history of SRC Five risk factors in total were identified (cervical joint position error, history of concussion, and 3 measures of trunk muscle function) athletes with 3 or more were 14 times more likely to suffer a neck/head injury (sensitivity 75% and specificity 82) then players with 2 or fewer risk factors |
| Hides [19] |
54 Professional rugby league players 14 suffered concussion |
Prospective cohort study | 2017 | Pre/Post Concussion |
Trunk muscle imaging Cervical joint position error Balance assessment |
Significant decreases in sway velocity and increased size/contraction of trunk muscles, were identified following concussion Whilst not significant overall, large inter-individual variation of test results for cervical proprioception and the vestibular system was observed Preliminary findings Post-concussion suggest an altered balance strategy and trunk muscle control with splinting/over-holding requiring consideration as part of the development of appropriate physiotherapy management strategies |
| Howell [27] | N/A | Scoping review | 2018 | N/A | N/A |
Based on existing literature, athletes appear more likely to sustain a musculoskeletal injury in the year after sustaining a concussion There are no known mechanisms for the increase in lower extremity injury following concussion, but one contributing factor may be that continued neuromuscular control deficits exist for a longer period than standard clinical tests are equipped to identify |
| Abdelkader [71] | 45 (18–40 years old) | Repeated measures | 2020 | Fatigue |
Neck Reposition Error Postural control (biodex balance system multidirectional reach test) |
Declines in postural stability were correlated with increased cervical joint position error Subjects suffering from cervical muscles fatigue are vulnerable to neck proprioception deficits and postural instability Clinicians and patients should avoid overload fatigue of the cervical muscles because it affects overall postural balance, neck proprioception & righting reaction |
| Cheever [13] | 40 female colligate club soccer athletes | Repeated measures pre-test post-test design with 4 groups | 2020 |
Instrumented head impacts Fatigue workout |
Cervical joint position error test, Neck Disability Index |
A 65%,54%,and49% increases in cervical joint position error were observed following soccer heading, fatigue only, and soccer heading + fatigue interventions, respectively. Meanwhile, the controls who did not head soccer balls or complete the fatigue protocol saw a 6% decrease in neck position error No difference between fatigue group and head impact group |
| Cheever [14] |
27 contact sport athletes 20 controls |
Cross-sectional | 2021 | History of contact sport participation |
Cervical strength Cervical joint reposition error Neck Disability Index |
Amateur sport athletes with a history of contact sport exposure exhibited 25.2% more total neck reposition error and 24.6% more maximum neck reposition error than athletes with no history of contact sport participation S/S number (r2 = 0.12, F(2,44 = 6.2, p = 0.017) and S/S severity (r2 = 0.14, F(2,44) = 5.6, p = 0.02) were significantly correlated with total neck reposition error |
| Peng | N/A | Narrative Review | 2021 | N/A | N/A |
Main problem in patients with neck pain is the impairment of cervical proprioception, which subsequently leads to cervical sensorimotor control disturbances Experimental neck muscle pain induced by injection of hypertonic saline results in significant inhibition of the activation of painful muscles suggesting chronic neck pain may cause structural and functional impairment of cervical muscles leading to excessive activation of mechanoreceptors in degenerative cervical discs and facet joints producing a large number of erroneous sensory signals |
NCAA National Collegiate Athletic Association
Stage 5: Collating, summarizing, and reporting the results
The methods employed throughout this protocol enabled us to collate existing knowledge and summarize the data in the following ways
A numerical and descriptive analysis, mapping of data within a scoping review flow chart.
An inductive thematic summary and analysis describing to the research questions and aims, based on the analysis on Braum and Clarke’s six-phase framework.
Results
Descriptive analysis
Our initial search identified 564 documents. Of these, 519 were within databases/search platforms and 45 from grey literature (Fig. 1). After duplicates were excluded, 378 records remained. An additional 28 potential studies were identified during step 3. In total, 406 articles underwent screening, and 315 records were excluded following abstract screening. An additional 37 were removed after reading full text. As a result, the scoping review identified 54 eligible studies (Fig. 1).
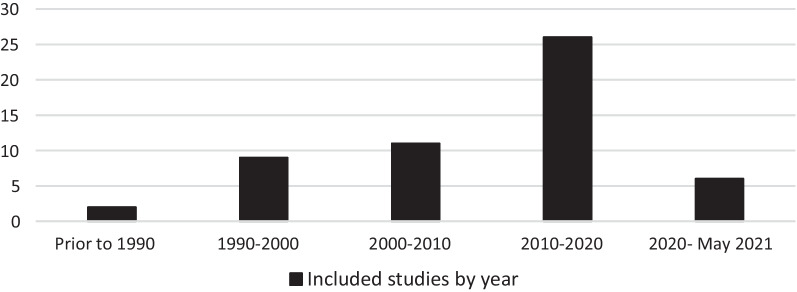
Included studies by year of publication
As consistent across the wider bibliometric trends, a substantial chronological increase in the number of relevant papers was identified over the previous 50 years (Fig. 2).
Fig. 2.
Included studies by year of publication
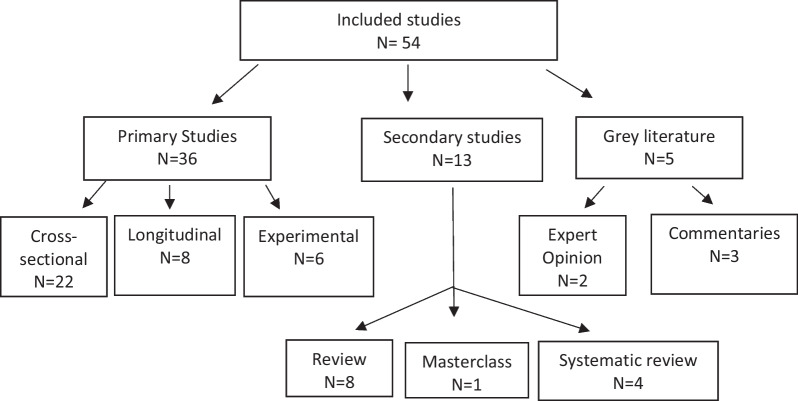
Type of study
Study design
The studies varied in terms of study design and primary focus. No formal quality assessment of included studies was performed, as scoping reviews are intended to provide a map of what evidence has been produced as opposed to seeking only the best available evidence to create policy or answer evidence-based practice questions [26, 30]. A taxonomy of research designs included in this scoping review is shown in Fig. 3.
Fig. 3.
Taxonomy of research designs for included literature
Theme of the study
Each included study fit into one of 3 themes which were further divided up into subthemes to accomplish the 4 purposes outlined in the introduction.
Theme 1: Cervical spine and contact sport participation
Thirty-three articles detailed the relationship between contact sport participation and the cervical spine. These articles present the evidence relating to the effects of contact sport participation on the cervical spine congruent with our first purpose. These studies provided consistent evidence of damage to the structures of the cervical spine responsible for maintaining the cervicocepahlic connection. Three secondary themes, including: (1) epidemiology of cervical injuries; (2) morphological changes to the cervical spine; and (3) return to play considerations emerged.
Epidemiology of cervical injuries in contact sport athletes
Three studies identified 223 catastrophic cervical injuries [31–33]. Representing an incidence rate of 0.52 in high school, 1.55 in college, and 14.00 in professional football for every 100,000 participants [31, 33]. Five epidemiological studies explored the prevalence of acute head and neck injuries in contact sport athletes [34–38]. Among the collegiate population, an estimated 7496 total cervical spine injuries between 2009–2010 to 2013–2014 were extrapolated from a smaller observed population, creating an estimated injury rate of 2.91 per 10,000 athlete exposure (AE) [34]. Stinger was the most common cervical injury (1.8/10,000 AE), followed by cervical strains (0.8/10,000 AEs) [34]. Among high school students, time loss cervical spine injuries were estimated at 3.04 per 100,000 AEs [36]. The most frequent mechanism of a cervical injury was contact with another player (70–85%) followed by contact with the ground (15–20%) [35, 36].
Two prospective studies explored head and neck injuries in professional soccer athletes [39, 40]. The incidence rate was 0.17–12.5/1000 player hours (men 12.8, women 11.5) and 3.7/1000 player hours for lost-time injuries (men 3.5, women 4.1) [39]. Mechanisms of injury involved aerial challenges (55%) and the use of the upper extremity (33%) or head (30%). [39]
Morphological changes to the cervical spine
Ten studies identified degenerative changes such as cervical spinal stenosis, degenerative disk disease, temporary paralysis, spondylolisthesis, and neck pain 10–20 years prior to aged-matched controls among contact sport athletes [3, 8, 41–47]. Lastly, three studies reviewed the experimental biomechanical stresses placed on the cervical spine in response to mechanical head loads during contact sport participation [9, 48, 49]. In these studies, multidirectional instability in the upper cervical spine was observed following simulated head impacts.
Return to play considerations
Ten studies explained principles guiding returning to play which included: asymptomatic, pain-free, neurologically intact, full strength and full cervical range of motion [50–59]. The primary concerns included reticulating pain, damage to C1 or C2, and instability [59, 60]. However, observations of increased risk of musculoskeletal injury following a concussion, portend the importance of caring for surrounding structures [19, 27].
The two most frequent concerns for disqualification were spinal stenosis and brachial plexus injury. Brachial plexus injury has an estimated 87% reoccurrence rate and caution should be taken to return those athletes with reoccurring radicular pain [53].
Theme 2: Cervical afferents and postural control
A total of twelve studies demonstrated the role cervical afferents play in upright posture and control of locomotion [11, 20, 23, 61–69]. These articles describe the cervicocephalic network and the role it plays in proper maintenance of head position, postural tone and coordination of the extremities congruent with the 2nd purpose of this review. Cervical afferents such as mechanoreceptors and nociceptive nerve endings are prevalent in cervical facet capsular tissue [23]. High densities up to 200 muscle spindles per gram compared to the first lumbrical in the thumb which has a mere 16 muscle spindles per gram [67].
Artificially induced afferent cervical dysfunction alters neuromotor control and posture maintenance
Three studies demonstrated how vibration and/or using anesthetic injections to simulate cervical dysfunction could cause severe ataxia and disequilibrium [64, 67, 69]. Malmstrom et al. [64] demonstrated significant increases in error during walking task. Moreover, Wannaprom et al. [69] reported increased postural sway and slower gait speeds under a vibration condition. Allum et al. [20] compared healthy controls to individuals with labyrinthine deficiency to isolate the contributions of the vestibular and cervical afferents in head control revealing head velocities during balance corrections were highly dependent on the movements of the head-neck mass-viscoelastic system. The cervico-collic reflex was also found to modulate the amplitude of functionally stabilizing responses and dampen mechanically induced instability of the head and neck.
Cervical pathology is linked to altered neuromotor control and poor posture maintenance
In addition to experiments in healthy controls, alterations in postural maintenance and locomotion, as well as cervical afferent processing following cervical pathology have been observed [11, 61–68, 70]. Patients with neck pain and dizziness demonstrate decreased postural stability [11, 63], as well as decreases in cervical sensorimotor function [62]. Specifically, cervical joint position error was significantly correlated with greater levels of neck pain and extent of cervical degeneration [62]. These findings have been replicated several times [11, 62, 65]. Separately, changes in cervical joint position error have also been correlated with altered postural stability [71].
Theme 3: Damage to cervical afferents and increased risk of injury
In considering the 3rd aim of the present review 4 studies demonstrate preliminary evidence of a connection between head impacts and altered cervical sensorimotor function [13, 14, 16, 72]. Cheever et al. [14] reported amateur sport athletes with a history of contact sport exposure exhibit 25% more total neck reposition error than controls. A follow up study utilized an acute bout of instrumented head impacts and observed a 65% acute increase in cervical joint position error following soccer heading compared to a 6% decrease among controls who did not complete the heading [13]. A decrease in trunk and head positioning following head impacts has also been observed, suggesting altered balance strategies and trunk muscle activation as regulated by the cervicocephalic network may also manifest following RHI. [72]
Further exploring the 3rd aim two preliminary prospective studies explored the correlation between decreased cervical sensorimotor function and a corresponding increase in musculoskeletal injury risk [13, 19]. In a prospective cohort study performed by Hides et al. [19], five risk factors were identified (cervical joint position error, history of concussion, and 3 measures of trunk muscle function). Athletes with 3 or more risk factors were 14 times more likely to suffer a neck/head injury (sensitivity 75% and specificity 82%) than players with 2 or fewer risk factors. Significantly decreased sway velocity and increased size/contraction of trunk muscles were also correlated with head position sense [19]. A similar study by Cheever et al. [13] found that a combination of sign and symptom severity scores and neck reposition error had robust predictive capability of individual’s future musculoskeletal injury status (AUC = 0.80, p = 0.003).
Discussion
The objective of this scoping review was to present the available evidence of morphological changes to the cervical spine following contact sport participation and to describe a theorized increased risk of musculoskeletal injury due to alterations in cervical sensorimotor function resulting from those morphological changes. Morphological changes to the cervical spine were observed throughout the literature, and associated decreased cervical sensorimotor function were observed in a few instances [13, 14]. Furthermore, preliminary evidence of a correlation between cervical sensorimotor function and secondary musculoskeletal injury was observed. [13, 19]
Decreased cervical sensorimotor function following morphological changes to the cervical spine and exposure to RHI
A preponderance of studies have demonstrated a relationship contact sport athletes who have a history of scrumming, tackling, and/or head contact with a ball and early development of chronic degeneration of the cervical spine [3, 6, 9, 73]. Separately, acute bouts of soccer heading and a history of contact sport history have been correlated with decreased cervical sensorimotor function [13, 14, 16]. However, while observations of accelerated degeneration and acute damage to the cervical spine have been corroborated in different sports (e.g., soccer, rugby, American football), all studies employed a cross-sectional design, failing to demonstrate a longitudinal correlation [7, 44, 46].
Preliminary findings from a series of instrumented heading studies serve as a potential foundation of a direct link between exposure to RHI and decreased cervical sensorimotor function and posture [13, 74]. Cheever et al. demonstrated a 65% increase in cervical joint reposition error in response to controlled soccer headers [13]. Similarly, decreased balance following instrumented soccer headers has been observed [74]. Both cervical sensorimotor function and balance deficits have been identified independently in patients suffering from chronic cervical pathology and athletes following an acute bout of soccer headers [75–77].
Cervical sensorimotor dysfunction and increased musculoskeletal injury risk
Previous research studies have demonstrated correlations between decreases in cervical joint position and postural control deficits Independent of contact sport exposure [70–79]. Both patients suffering from persistent cervical symptoms and persistent post-concussive symptoms have demonstrated altered postural control, as well as decreased cervical sensorimotor function [61, 66, 68, 70].
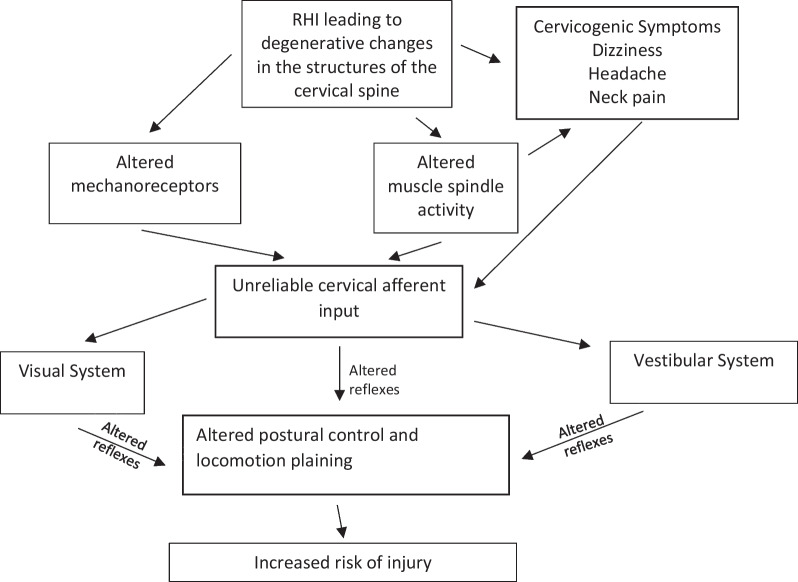
A large body of existing literature demonstrates an observed increase in musculoskeletal injury risk in the year after sustaining a concussion [80]. The mechanism for this relationship remains highly contested [27]. However, one leading hypothesis points to observations of lingering neuromuscular control deficits [79]. While not fully explored, altered cervical afferent processing may play a role in this heightened risk. Sensorimotor control of both stable upright position and locomotion relies heavily on cervical afferent information that play a critical role in three reflexes that influence head, eye and postural stability: the cervico-collic reflex, the cervico-ocular reflex, and the tonic neck reflex [67]. These reflexes work alongside the vestibular and visual systems throughout the central nervous system to maintain proper postural control [80]. These connections have been further mapped in Fig. 4 to visually demonstrate the potential connection of morphological and neurological changes to the cervical spine and increased risk of secondary injury.
Fig. 4.
Mapping of potential implications for altered cervical afferent input
While findings of impaired sensorimotor function and balance in contact sport athletes are an important step, these movements were all performed at slow speeds, which don’t mirror the pace of sports-related task. Previous experiments exploring the integration of deficient cervical afferent information into the cerviocephalic network were performed in either a static position or walking at a relatively slow steady state (< 2–3 mph) [64, 69]. Athletes frequently travel in excess of 15–20 mph during sprints with individual spikes in limb movement exceeding 8000 degrees/s [81]. No research has been performed in a high velocity movement state to test how variations in postural control and cervical sensorimotor function may be magnified by the high velocity demands of contact sport movement patterns (e.g., dodging a potential tackler, sprinting after an advancing player, or adjusting to a rapid change of direction).
Knowledge gaps and future research
In line with the 4th aim of the present scoping review several gaps in the available literature were identified (Box 1). Future research should explore the dose dependent effect of RHI on structures of the cervical spine and the causative affect those changes have on musculoskeletal injury risk. Moreover, it would be important to explore potential interventional therapies to reduce the increased risk of injury.
Box 1.
Relevant research priorities identified
| The dose–response effect of RHI and degeneration of cervical spine across different competition levels (youth, high school, college, amateur, professional) and time periods (single exposure, season, career) |
| Larger prospective cohort studies that utilize measures of cervical sensorimotor function to predict increased injury risk |
| Large retrospective epidemiological studies utilizing injury sport databases to see if individuals who suffered a neck injury were subsequently more likely to suffer a subsequent secondary injury |
| The role altered cervical sensorimotor function plays in postural control and coordination of the limbs at speeds more similar to those experienced during sport participation |
Limitations
While scoping reviews are comprehensive, they fall short of exhaustively identifying all relevant literature by balancing the breadth and depth of the desired analysis. Our search was subject to a limited number of contact sports rather than all physical activity involving RHI. Contact sport athletes are different from controls for many reasons such as exercise history, exposure to other impacts to the head or body, making it difficult to have true controls matched across all demographical and extraneous factors. Scoping reviews are broad in nature and allow for the development of theoretically connections regardless of quality, which allows for a broader and more contextual overview than a systematic review but may be more subject to individual bias. Rigorous and reproducible methods were employed to demonstrate the authors commitment to publish all findings whether findings were positive, negative or not significant to the theoretical argument presented in the introduction.
Conclusions
While preliminary work exploring the role the cervicocepahlic network plays in control of both static posture and locomotion demonstrates clear connections between deficit cervical afferent input and erroneous motor output. Moreover, morphological changes to the cervical spine and associated sensorimotor deficits were observed throughout the literature in response to contact sport participation. However, while both deficit cervical afferent and erroneous motor output have been observed in response to contact sport participation little research has explored a potential causal relationship between those deficits and future musculoskeletal injury risk. Further research is necessary to elucidate the relationship between cervical pathology and alterations in cervical sensorimotor function in recreational and amateur athletes.
Supplementary Information
Acknowledgements
We would like to acknowledge Leslie Rosas, Clarissa Garcia, and Ivanna Peralta who all work as undergraduate research assistants for Dr. Cheever and May Hayward who is a research librarian who all provided valuable assistance in helping to identify and categorize the articles for this scoping review.
Author contributions
KC was primarily responsible for the conception and framework of the scoping review. Additionally, Dr. KC lead the scoping review process. JK assisted in the development and critically reviewed the manuscript while adding much needed content expertise as skilled clinician in the diagnosis and treatment of cervical spine pathology. KK assisted in the process of the scoping review while also providing meaningful structure development and writing expertise. All authors read and approved the final manuscript.
Funding
The authors report no funding associated with the scoping review.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors report no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bailes JE. Management of cervical spine sports injuries. Athl Train. 1990;25(2):156–159. [PMC free article] [PubMed] [Google Scholar]
- 2.Legault EP, Descarreaux M, Cantin V. Musculoskeletal symptoms in an adolescent athlete population: a comparative study. BMC Musculoskelet Disord. 2015;16(210):1–9. doi: 10.1186/s12891-015-0681-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sortland O, Tysvaer AT, Storli OV. Changes in the cervical spine in association football players. Br J Sports Med. 1982;16(2):80–84. doi: 10.1136/bjsm.16.2.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Torg JS, Ramsey-Emrhein JA. Suggested management guidelines for participation in collision activities with congenital, developmental, or postinjury lesions involving the cervical spine. Med Sci Sports Exer. 1997;29(7 Suppl):S256–s272. doi: 10.1097/00005768-199707001-00008. [DOI] [PubMed] [Google Scholar]
- 5.Panjabi MM, Cholewicki J, Nibu K, Grauer J, Babat LB, Dvorak J. Critical load of the human cervical spine: an in vitro experimental study. Clin Biomech. 1998;13(1):11–17. doi: 10.1016/S0268-0033(97)00057-0. [DOI] [PubMed] [Google Scholar]
- 6.Berge JRM, Marque B, Vital JM, Sénégas J, Caillã JM. Age-related changes in the cervical spines of front-line rugby players. Am J Sports Med. 1999;27(4):422–429. doi: 10.1177/03635465990270040401. [DOI] [PubMed] [Google Scholar]
- 7.Castinel BH, Adam P, Milburn PD, Castinel A, Quarrie KL, Peyrin JC, Yeo JD. Epidemiology of cervical spine abnormalities in asymptomatic adult professional rugby union players using static and dynamic MRI protocols: 2002 to 2006. Br J Sports Med. 2010;44(3):194–199. doi: 10.1136/bjsm.2007.045815. [DOI] [PubMed] [Google Scholar]
- 8.Kartal A, ıldıran I, Şenköylü A, Korkusuz F. Soccer causes degenerative changes in the cervical spine. Euro Spine J. 2004;13(1):76–82. [DOI] [PMC free article] [PubMed]
- 9.Mehnert MJ, Agesen T, Malanga GA. "Heading" and neck injuries in soccer: a review of biomechanics and potential long-term effects. Pain Phys. 2005;8(4):391–397. doi: 10.36076/ppj.2005/8/391. [DOI] [PubMed] [Google Scholar]
- 10.Service NH. Whiplash/symptoms of whiplash 2015. 2015. http://www.nhsinform.com/health-library/articles/w/whiplash/symptoms.
- 11.Treleaven J, Peterson G, Ludvigsson ML, Kammerlind AS, Peolsson A. Balance, dizziness and proprioception in patients with chronic whiplash associated disorders complaining of dizziness: a prospective randomized study comparing three exercise programs. Man Ther. 2016;22:122–130. doi: 10.1016/j.math.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 12.Cantu RC. Cervical spinal stenosis. Challenging an established detection method. Phys Sportsmed. 1993;21(9):57–58;62–63. [DOI] [PubMed]
- 13.Cheever KM, Howard JT, Kawata K. Clinical changes in cervical neuromuscular control following subconcussive impacts. J Sport Rehabil. 2021;30(3):467–474. doi: 10.1123/jsr.2020-0228. [DOI] [PubMed] [Google Scholar]
- 14.Cheever K, Mcdevit J, Wright WG, Tierney R. Differences in cervical kinesthesia between amateur athletes with and without a history of contact sport participation. Brain Inj. 2021;35(4):404–410. doi: 10.1080/02699052.2021.1878551. [DOI] [PubMed] [Google Scholar]
- 15.Lark SD, Mccarthy P. The effects of a rugby playing season on cervical range of motion. J Sports Sci. 2010;28(6):649–655. doi: 10.1080/02640411003631968. [DOI] [PubMed] [Google Scholar]
- 16.Lark SD, Mccarthy PW. Cervical range of motion and proprioception in rugby players versus non-rugby players. J Sports Sci. 2007;25(8):887–894. doi: 10.1080/02640410600944543. [DOI] [PubMed] [Google Scholar]
- 17.Cheever K. Exploring the relationship between musculoskeletal injury and clinical outcome measures of cervical sensorimotor function. Int J Athl Ther Train. 2021;26:262–268. doi: 10.1123/ijatt.2020-0033. [DOI] [Google Scholar]
- 18.Collins CL, Fletcher EN, Fields SK, Kluchurosky L, Rohrkemper MK, Comstock RD, Cantu RC. Neck strength: a protective factor reducing risk for concussion in high school sports. J Prim Prevent. 2014;35(5):309–319. doi: 10.1007/s10935-014-0355-2. [DOI] [PubMed] [Google Scholar]
- 19.Hides JA, Smith MMF, Mendis MD, Treleaven J, Rotstein AH, Sexton CT, Choy NL, Mccrory P. Self-reported concussion history and sensorimotor tests predict head/neck injuries. Med Sci Sports Exer. 2017;49(12):2385–2393. doi: 10.1249/MSS.0000000000001372. [DOI] [PubMed] [Google Scholar]
- 20.Allum JH, Gresty M, Keshner E, Shupert C. The control of head movements during human balance corrections. J Vestib Res Equil Orient. 1997;7(2–3):189. doi: 10.3233/VES-1997-72-309. [DOI] [PubMed] [Google Scholar]
- 21.Boyle R. Vestibulospinal control of reflex and voluntary head movement. Ann New York Acad Sci. 2001;942(1):364–380. doi: 10.1111/j.1749-6632.2001.tb03760.x. [DOI] [PubMed] [Google Scholar]
- 22.Kulkarni V, Chandy MJ, Babu KS. Quantitative study of muscle spindles in suboccipital muscles of human foetuses. Neurol India. 2001;49(4):355–359. [PubMed] [Google Scholar]
- 23.Mclain RF. Mechanoreceptor endings in human cervical facet joints. Spine. 1994;19(5):495–501. doi: 10.1097/00007632-199403000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Marshall CM, Vernon H, Leddy JJ, Baldwin BB. The role of the cervical spine in post-concussion syndrome. Phys Sports Med Phys Sportsmed. 2015;43(3):274–284. doi: 10.1080/00913847.2015.1064301. [DOI] [PubMed] [Google Scholar]
- 25.Schneider KJ, Meeuwisse WH, Nettel-Aguirre A, Barlow K, Boyd L, Kang J, Emery CA. Cervicovestibular rehabilitation in sport-related concussion: a randomised controlled trial. Br J Sports Med. 2014;48(17):1294–U55. doi: 10.1136/bjsports-2013-093267. [DOI] [PubMed] [Google Scholar]
- 26.Arskey HL, O'Malley K. Scoping studies, towards a methodological fraemwork. Int J Soc Res Methodol. 2005;5(8):19–32. [Google Scholar]
- 27.Howell DR, Lynall RC, Buckley TA, Herman DC. Neuromuscular control deficits and the risk of subsequent injury after a concussion: a scoping review. Sports Med. 2018;48(5):097–1115. doi: 10.1007/s40279-018-0871-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murray AD, Daines L, Archibald D, Hawkes RA, Schiphorst C, Kelly P, Grant L, Mutrie N. The relationships between golf and health: a scoping review. Br J Sports Med. 2017;51(1):12. doi: 10.1136/bjsports-2016-096625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Griffin SA, Perera NKP, Murray A, Hartley C, Brooks JHM, Kemp SPT, Stokes KA. The relationships between rugby union and health: a scoping review protocol. BMJ Open Sport Exer Med. 2019;5(1):11–17. doi: 10.1136/bmjsem-2019-000593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Caron JG, Bloom GA, Falcao WR, Sweet SN. An examination of concussion education programmes: a scoping review methodology. Inj Prev. 2015;21(5):301–308. doi: 10.1136/injuryprev-2014-041479. [DOI] [PubMed] [Google Scholar]
- 31.Cantu RC, Mueller FM. Catastrophic spine injuries in American football. 1977–2001. Neurosurgery. 2003;53(2):358–362. doi: 10.1227/01.NEU.0000073422.01886.88. [DOI] [PubMed] [Google Scholar]
- 32.Hutton MJ, Mcguire RA, Dunn R, Williams R, Robertson P, Twaddle B, Kiely P, Clarke A, Mazda K, Davies P, Pagarigan KT, Dettori JR. Catastrophic cervical spine injuries in contact sports. Global Spine J. 2016;6(7):721–733. doi: 10.1055/s-0036-1586744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mueller FO. Fatalities from head and cervical spine injuries occurring in tackle football: 50 years' experience. Clin Sports Med. 1998;17(1):169–182. doi: 10.1016/S0278-5919(05)70071-5. [DOI] [PubMed] [Google Scholar]
- 34.Chung AS, Makovicka JL, Hassebrock JD, Patel KA, Tummala SV, Deckey DG, Hydrick TC, Rubel NC, Chhabra A. Epidemiology of cervical injuries in NCAA football players. Spine. 2019;44(12):848–854. doi: 10.1097/BRS.0000000000003008. [DOI] [PubMed] [Google Scholar]
- 35.Lee KM, Kay MC, Kucera KL, Prentice WE, Kerr ZY. Epidemiology of cervical muscle strains in collegiate and high school football athletes, 2011–2012 through 2013–2014 academic years. J Athl Train. 2019;54(7):780–786. doi: 10.4085/1062-6050-229-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meron A, Mcmullen C, Laker SR, Currie D, Comstock RD. Epidemiology of cervical spine injuries in high school athletes over a ten-year period. PM & R. 2018;10(4):365–372. doi: 10.1016/j.pmrj.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 37.Simmons MM, Swedler DI, Kerr ZY. Injury surveillance of head, neck, and facial injuries in collegiate ice hockey players, 2009–2010 through 2013–2014 academic years. J Athl Train. 2017;52(8):776–784. doi: 10.4085/1062-6050-52.4.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Williams JZ, Singichetti B, Li HM, Xiang H, Klingele KE, Yang JZ. Epidemiological patterns of initial and subsequent injuries in collegiate football athletes. Am J Sports Med. 2017;45(5):1171–1178. doi: 10.1177/0363546516685317. [DOI] [PubMed] [Google Scholar]
- 39.Fuller CW, Junge A, Dvorak J. A six year prospective study of the incidence and causes of head and neck injuries in international football. Br J Sports Med. 2005;39:I3–I9. doi: 10.1136/bjsm.2005.018937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nilsson M, Hagglund M, Ekstrand J, Walden M. Head and neck injuries in professional soccer. Clin J Sport Med. 2013;23(4):255–260. doi: 10.1097/JSM.0b013e31827ee6f8. [DOI] [PubMed] [Google Scholar]
- 41.Bailes JE. Experience with cervical stenosis and temporary paralysis in athletes. J Neurosurg-Spine. 2005;2(1):11–16. doi: 10.3171/spi.2005.2.1.0011. [DOI] [PubMed] [Google Scholar]
- 42.Brauge D, Delpierre C, Adam P, Sol JC, Bernard P, Roux FE. Clinical and radiological cervical spine evaluation in retired professional rugby players. J Neurosurg-Spine. 2015;23(5):551–557. doi: 10.3171/2015.1.SPINE14594. [DOI] [PubMed] [Google Scholar]
- 43.Kuman K, Umeyama T. Cervical disk injuries in athletes. Arch Orthopaed Trauma Surg. 1986;105(4):223–226. doi: 10.1007/BF00435485. [DOI] [PubMed] [Google Scholar]
- 44.Ndubuisi CA, Ohaegbulam SC, Mezue WC. Impact of active leisure (noncompetitive) contact sports activities on the space available for the cord of the subaxial cervical spine of asymptomatic adults. World Neurosurg. 2017;108:705–710. doi: 10.1016/j.wneu.2017.09.052. [DOI] [PubMed] [Google Scholar]
- 45.Quarrie KL, Cantu RC, Chalmers DJ. Rugby union injuries to the cervical spine and spinal cord. Sports Med. 2002;32(10):633–653. doi: 10.2165/00007256-200232100-00003. [DOI] [PubMed] [Google Scholar]
- 46.Torg JS, Naranja RJ, Pavlov H, Galinat BJ, Warren R, Stine RA. The relationship of developmental narrowing of the cervical spinal canal to reversible and irreversible injury of the cervical spinal cord in football players—an epidemiological study. J Bone Joint Surg-Am Volume. 1996;78A(9):1308–1314. doi: 10.2106/00004623-199609000-00003. [DOI] [PubMed] [Google Scholar]
- 47.Tysvaer AT. Head and neck injuries in soccer—impact of minor trauma. Sports Med. 1992;14(3):200–213. doi: 10.2165/00007256-199214030-00006. [DOI] [PubMed] [Google Scholar]
- 48.Ivancic PC. Cervical spine instability following axial compression injury: a biomechanical study. Orthopaed Traumatol Surg Res. 2014;100(1):127–133. doi: 10.1016/j.otsr.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 49.Trewartha G, Preatoni E, England ME, Stokes KA. Injury and biomechanical perspectives on the rugby scrum: a review of the literature. Br J Sports Med. 2015;49(7):425–U25. doi: 10.1136/bjsports-2013-092972. [DOI] [PubMed] [Google Scholar]
- 50.Cantu RC. Functional cervical spinal stenosis—a contraindication to participation in contact sports. Med Sci Sports Exer. 1993;25(3):316–317. doi: 10.1249/00005768-199303000-00003. [DOI] [PubMed] [Google Scholar]
- 51.Cantu RC. The cervical spinal stenosis controversy. Clin Sports Med. 1998;17(1):121–126. doi: 10.1016/S0278-5919(05)70066-1. [DOI] [PubMed] [Google Scholar]
- 52.Chao S, Pacella MJ, Torg JS. The pathomechanics, pathophysiology and prevention of cervical spinal cord and brachial plexus injuries in athletics. Sports Med. 2010;40(1):59–75. doi: 10.2165/11319650-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 53.Dailey A, Harrop JS, France JC. High-energy contact sports and cervical spine neuropraxia injuries what are the criteria for return to participation? Spine. 2010;35(21):S193–S201. doi: 10.1097/BRS.0b013e3181f32db0. [DOI] [PubMed] [Google Scholar]
- 54.Joaquim AF, Hsu WK, Patel AA. Cervical spine surgery in professional athletes: a systematic review. Neurosurg Focus. 2016;40(4):143–148. doi: 10.3171/2016.1.FOCUS15560. [DOI] [PubMed] [Google Scholar]
- 55.Kepler CK, Vaccaro AR. Injuries and abnormalities of the cervical spine and return to play criteria. Clinics Sports Med. 2012;31(3):499–508. doi: 10.1016/j.csm.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 56.Mcana S, Cho S, Qureshi S, Hecht AC. A commentary on cervical spondylolysis in the contact athlete. Spine. 2014;14(6):E7–8. [DOI] [PubMed]
- 57.Mcana S, Cho S, Qureshi S, Hecht AC. A commentary on cervical spondylolysis in the contact athlete. Spine. 2014;14(6):E7–E8. doi: 10.1016/j.spinee.2014.02.026. [DOI] [PubMed] [Google Scholar]
- 58.Okonkwo DO, Stone JR. Basic science of closed head injuries and spinal cord injuries. Clin Sports Med. 2003;22(3):467–481. doi: 10.1016/S0278-5919(02)00107-2. [DOI] [PubMed] [Google Scholar]
- 59.Torg JS. Cervical spine injuries and the return to football. Sports Health. 2009;1(5):376–83. doi: 10.1177/1941738109343161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Torg JS, Ramsey-Emrhein JA. Cervical spine and brachial plexus injuries: return-to-play recommendations. Phys Sportsmed. 1997;25(7):60–62;64;66–67;72;81–82;85–88. [DOI] [PubMed]
- 61.Carrick FR, Pagnacco G, Hunfalvay M, Azzolino S, Oggero E. Head position and posturography: a novel biomarker to identify concussion sufferers. Brain Sci. 2020;10(12):1003. doi: 10.3390/brainsci10121003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Freppel S, Bisdorff A, Colnat-Coulbois S, Ceyte H, Cian C, Gauchard G, Auque J, Perrin P. Visuo-proprioceptive interactions in degenerative cervical spine diseases requiring surgery. Neuroscience. 2013;25(5):226–232. doi: 10.1016/j.neuroscience.2013.09.060. [DOI] [PubMed] [Google Scholar]
- 63.Karlberg M, Magnusson M, Malmstrom ME, Melander A, Moritz U. Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Arch Phys Med Rehabil. 1996;77(9):874–882. doi: 10.1016/S0003-9993(96)90273-7. [DOI] [PubMed] [Google Scholar]
- 64.Malmstrom EM, Fransson PA, Bruinen TJ, Facic S, Tjernstrom F. Disturbed cervical proprioception affects perception of spatial orientation while in motion. Exp Brain Res. 2017;235(9):2755–2766. doi: 10.1007/s00221-017-4993-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Reddy RS, Tedla JS, Dixit S, Abohashrh M. Cervical proprioception and its relationship with neck pain intensity in subjects with cervical spondylosis. BMC Musculoskelet Disord. 2019;20(1):1–7. doi: 10.1186/s12891-019-2846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sjostrom H, Allum JFJ, Carpenter MG, Adkin AL, Honegger F, Ettlin T. Trunk sway measures of postural stability during clinical balance tests in patients with chronic whiplash injury symptoms. Spine. 2003;28(15):1725–1734. doi: 10.1097/01.BRS.0000083170.34304.A3. [DOI] [PubMed] [Google Scholar]
- 67.Treleaven J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control. Man Ther. 2008;13(1):2–11. doi: 10.1016/j.math.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 68.Treleaven J, Jull G, Lowchoy N. Standing balance in persistent whiplash: a comparison between subjects with and without dizziness. J Rehabil Med. 2005;37(4):224–229. doi: 10.1080/16501970510027989. [DOI] [PubMed] [Google Scholar]
- 69.Wannaprom NJ, Treleaven J, Jull G, Uthaikhup S. Neck muscle vibration produces diverse responses in balance and gait speed between individuals with and without neck pain. Musculoskelet Sci Pract. 2018;35:25–29. doi: 10.1016/j.msksp.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 70.Treleaven J, Jull G, Lowchoy N. Lowchoy N The relationship of cervical joint position error to balance and eye movement disturbances in persistent whiplash. Man Ther. 2006;11(2):99–106. doi: 10.1016/j.math.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 71.Abdelkader NA, Mahmoud AY, Fayaz NA, Mahmoud LS. Decreased neck proprioception and posturalstability after induced cervical flexor muscles fatigue. J Musculoskelet Neur Interact. 2020;20(3):421–428. [PMC free article] [PubMed] [Google Scholar]
- 72.Hides JA, Smith MMF, Mendis MD, Smith NA, Cooper AJ, Treleaven J, Leung F, Gardner AJ, Mccrory P, Choy NL. A prospective investigation of changes in the sensorimotor system following sports concussion. An exploratory study. Musculoskelet Sci Pract. 2017;29:7–19. doi: 10.1016/j.msksp.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 73.Svaldi DO, Joshi C, Mccuen EC, Music JP, Hannemann R, Leverenz LJ, Nauman EA, Talavage TM. Accumulation of high magnitude acceleration events predicts cerebrovascular reactivity changes in female high school soccer athletes. Brain Imag Behavior. 2020;14(1):164–174. doi: 10.1007/s11682-018-9983-0. [DOI] [PubMed] [Google Scholar]
- 74.Haran FJ, Tierney R, Wright WG, Keshner E, Silter M. Acute changes in postural control after soccer heading. Int J Sports Med. 2013;34(4):350–354. doi: 10.1055/s-0032-1304647. [DOI] [PubMed] [Google Scholar]
- 75.Hwang S, Ma L, Kawata K, Tierney R, Jeka JJ. Vestibular dysfunction after subconcussive head impact. J Neurotrauma. 2017;34(1):8–15. doi: 10.1089/neu.2015.4238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mcpartland JM, Brodeur RR, Hallgren RC. Chronic neck pain, standing balance, and suboccipital muscle atrophy—a pilot study. J Manipul Physiol Therapeut. 1997;20(1):24–29. [PubMed] [Google Scholar]
- 77.Rix GD, Bagust J. Cervicocephalic kinesthetic sensibility in patients with chronic, nontraumatic cervical spine pain. Arch Phys Med Rehabil. 2001;82(7):911–919. doi: 10.1053/apmr.2001.23300. [DOI] [PubMed] [Google Scholar]
- 78.Kristjansson K, Treleaven EJ. Sensorimotor function and dizziness in neck pain: implications for assessment and management. J Orthop Sports Phys Ther. 2009;39(5):364–377. doi: 10.2519/jospt.2009.2834. [DOI] [PubMed] [Google Scholar]
- 79.Alsalaheen BA, Mucha A, Morris LO, Whitney SL, Furman JL, Camiolo-Reddy CE, Collins MW, Lovell PJ, Sparto M. Vestibular rehabilitation for dizziness and balance disorders after concussion. J Neurol Phys Ther. 2010;34(2):87–93. doi: 10.1097/NPT.0b013e3181dde568. [DOI] [PubMed] [Google Scholar]
- 80.Sjolander P, Michaelson P, Jaric S, Djupsjobacka M. Sensorimotor disturbances in chronic neck pain–range of motion, peak velocity, smoothness of movement, and repositioning acuity. Man Ther. 2008;13(2):122–31. doi: 10.1016/j.math.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 81.Bourdon PC, Cardinale M, Murray A, Gastin P, Kellmann M, Varley MC, Gabbett TJ, Coutts AJ, Burgess DJ, Gregson W, Cable NT. Monitoring athlete training loads: consensus statement. Int J Sports Physiol Perform. 2017;12(1):161–170. doi: 10.1123/IJSPP.2017-0208. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.