Introduction
Migration of objects used for abortion from uterus to various parts of abdominal cavity is not uncommon. They may remain asymptomatic for some years or become symptomatic depending upon type of foreign body and its location. We herein, present a rare case of migration of red rubber catheter from uterus to pleural cavity.
Case Report
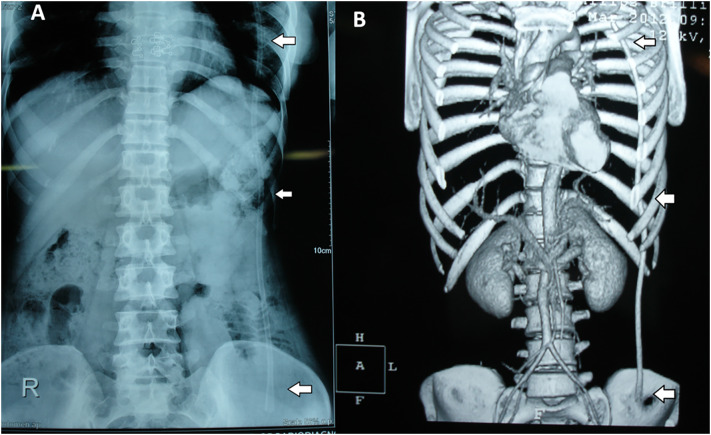
A 35-year-old thin-built female patient without any medical risk factors presented to us with history of left-sided chest pain and haemoptysis of 2 years duration. There was no history of abdominal pain, fever, night sweats, loss of weight or altered bowel habit. However, patient had history of abortion at home by untrained medical person. Based on the history, a provisional diagnosis of pulmonary tuberculosis was entertained which is the common cause of fever and haemoptysis in Indian subcontinent. Patient was afebrile, and there was no peripheral lymphadenopathy. Chest examination was unremarkable. On deep palpation of the abdomen, we could appreciate an intra-abdominal cord like structure in left iliac fossa extending up to left lumber area. Per-vaginal examination was unremarkable. Plain X-ray abdomen and chest revealed a radio-opaque shadow (Fig. 1A) extending from iliac fossa to the apex of the left lung, and there were no radiological signs of tuberculosis. Haemogram, LFT and ESR were within normal limits. Abdominal sonography was unremarkable except incidental gall stones. CECT of abdomen and pelvis revealed a long tubular hyperdense structure extending from left iliac fossa to the left side of thoracic cavity (Fig. 1B). With this clinical and radiological finding; diagnosis of a foreign body possibly a tube, extending from left iliac fossa to the left pleural cavity, was considered.
Fig. 1.
a Plain radiograph abdomen erect view showing a tubular object extending from pelvis to apex of left lung, b Contrast-enhanced computed tomography (CECT) image showing a catheter extending from iliac fossa to the apex of the left lung
She underwent laparotomy and removal of red rubber catheter. There was minimal adhesion into left paracolic gutter. A tubular structure was felt with distal end going into the sigmoid colon. The distal end was dissected out of sigmoid colon and used as a guide for the proximal dissection. A 15 Fr red rubber catheter was identified after separating the tract all around which was going into thoracic cavity (Fig. 2). The rubber catheter was pulled out of its tract which was extending through diaphragm into the pleural cavity. The rent in the sigmoid colon was closed with end to end anastomotic (EEA) stapler and oversewn with 3–0 proline suture. Adnexal structures and uterus were essentially normal.
Fig. 2.
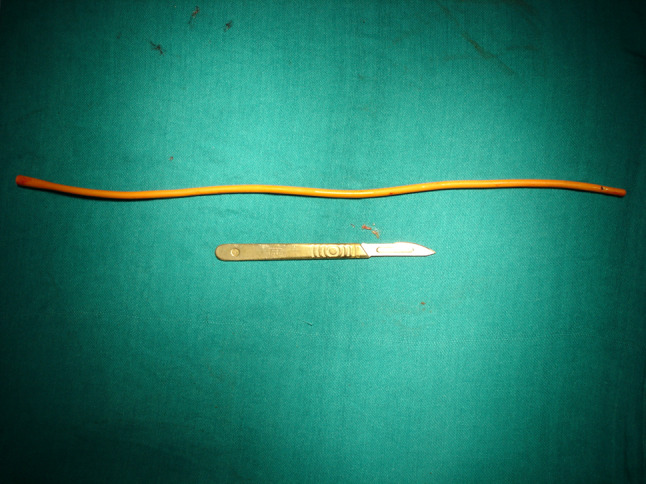
Retrieved red rubber catheter
Patient had a smooth post-operative course and was discharged on post-operative day 3. At last follow-up after 2 years of surgery, she was asymptomatic and doing well.
Discussion
There are many reports of foreign body migration. It can migrate from any part of the body to anywhere in abdomen, from extra luminal to intra-luminal and vice versa. Uterus is a site of applications of various inanimate objects viz. knitting needles, wooden or metal sticks, roots of plants, or even a Bougie for induced abortions, copper T used for contraception or surgical sponges used during caesarean section [1] or hysterectomy. Authors have also reported migration of copper T from uterus to stomach [2] and migration of Ryles tube used for abortion into the peritoneal cavity [3].
Though foreign body migration is a rare occurrence; however, it is not uncommon. Mechanism of migration also varies. The common foreign bodies which enter and remain in tissue are splinters of wood and metal, needles and bullets. Metallic foreign bodies elicit less infection so remain in tissue for long. Suppuration however may cause migration of objects for a considerable distance through path of suppuration. Another mechanism may be muscular contraction and pressure from without might cause some degree of migration [4].
Foreign bodies can present immediately or in early post-procedural period or late. Immediate complications include pain, bleeding from site of entry or injury to some nearby vessels or anaesthesia-related complications. Early complications include infection viz. local or systemic and organisms can vary from bacterial to fungal or parasites as there may be applications of unsterile objects with unsterile method. Late complications can be related to local or distant site of lodgement. Locally objects can induce inflammation, fibrosis and involvement of local structures. Distant complications depend upon the final destination of the object. Our patient presented with chest pain and haemoptysis that lead to hospital visit. She didn’t have other intra-abdominal complaints as it migrated through retroperitoneal route.
This is possibly the only case report where a red rubber catheter used for abortion has migrated from the uterus to the retroperitoneum and then to the apex of left pleural cavity. Pre-operative suspicion was tuberculosis clinically but on imaging, a foreign body was identified. It was a red rubber catheter used during previous unsafe abortion and it could be removed safely with open surgical approach and patient was relieved of her symptoms.
So foreign bodies can travel from anywhere to everywhere. Missed foreign body should not be ignored as they can cause significant morbidity and unusual symptoms. A vigilant eye should be kept on possible untoward complications.
This case gives the following message:
This case gave an insight into the outcome and result of abortion by an untrained person.
This unusual site of migration of the foreign body from uterus was not thought of. The patient presented with unusual symptoms leading to misdiagnosis of a respiratory illness.
The past history was very important in this patient after the imaging revealed a foreign body.
Acknowledgments
None.
Dr. Ashok Kumar
is currently positioned as the Professor in the Department of Surgical Gastroenterology, SGPGIMS, Lucknow, India. He has obtained fellowship in colorectal surgery (St Mark’s Hospital, London), UICC Fellowship (Mayo Clinic Rochester, USA), FRCS. He has been a mentor to many PhD, Post Doc Fellows and MD students. He has served as Secretary & President of the ACRSI and President of UPASI (2019) and secretary of IASG. Currently he is on editorial board of Annals of Coloproctology, World J of Surgical Gastroenterology, Indian Journal of Surgery, Journal of Pancreatic Cancer and Current Cancer Drug Target. He has expertise in HPB, UGI surgeries with special interest in sphincter saving surgery for rectal cancer, pouch surgery for ulcerative colitis, surgery for rectovaginal fistula, surgery for anal sphincter injury, surgery for fecal incontinence, surgery for constipation, rectocele, Obstructed Defecation Syndrome (ODS), Stapled Hemorrhoidectomy and pelvic floor disease.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest to this work.
Informed consent
Informed consent was obtained from the patient.
Footnotes
Ashok Kumar is a Professor, Department of Surgical Gastroenterology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raebareli Road, Lucknow, INDIA, 226014. Nalini Kanta Ghosh is an Assistant Professor Department of Surgical Gastroenterology, Sanjay Gandhi Post Graduate Institute of Medical Sciences Raebareli Road, Lucknow, INDIA, 226014.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Silva CS, Caetano MR, Silva EA, Falco L, Murta EF. Complete migration of retained surgical sponge into ileum without sign of open intestinal wall. Arch Gynecol Obstet. 2001;265(2):103–104. doi: 10.1007/s004040000141. [DOI] [PubMed] [Google Scholar]
- 2.Rani AK, Kumar A, Dash NR. Copper-T Migration into Stomach: A Laparoscopic Management. Journal of Obstetrics and Gynaecology of India. 2015;65(1):54. doi: 10.1007/s13224-014-0597-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nayak PK, Mitra S, Padma A, Agrawal S. Late presentation of unsafe abortion after 5 years of procedure. Case Reports in Obstetrics and Gynecology. 2014;2014.
- 4.Howard A.L Boston Med Surg J 1912; 167:933–934