Abstract
We discuss a case report of a 38-year-old uncircumcised male on pre-exposure prophylaxis for human immunodeficiency virus who presents to the emergency department for painful lesions over his penile region following unprotected sexual intercourse. Following the development of these lesions he developed painless, itchy pustules over his bilateral arms and back. He also had extensive pain and swelling over his penile region, which prevented him from unretracting his foreskin. Chlamydia trachomatis, Herpes simplex virus, Neisseria gonorrhoeae, and syphilis tests were negative. He was positive for orthopoxvirus using polymerase chain reaction. A diagnosis of paraphimosis as a complication of monkeypox infection was made.
Keywords: monkeypox virus, paraphimosis, genital diseases, male, infectious disease, emerging
INTRODUCTION
Monkeypox is a zoonotic infection caused by a double-stranded virus belonging to the Orthopoxvirus genus and the Poxviridae family [1]. It occurs mainly in the tropical rainforest areas of Central and West Africa and is occasionally exported to other regions including the USA [2–4]. The first case was identified in monkeys sent from Singapore to a research facility in Denmark [5]. It wasn’t until 1970 that the first human case was diagnosed in a child in the Democratic Republic of Congo [2]. There are two genetically distinct clads of monkeypox, the Central African clad and the West African clad. Most of the infections are caused by the Central African clad [6]. In endemic areas, an animal-to-human connection is common because of direct contact with blood, bodily fluids, and mucocutaneous lesions of infected animals [7]. Human-to-human transmission occurs through direct contact with infectious sores, body fluids and scabs, and indirectly through respiratory secretions or sharing contaminated items [8]. The incubation period lasts about 5–14 days and is self-limiting within 2–4 weeks [9]. It causes a systemic illness that includes fever, chills, fatigue, myalgias, and a characteristic rash. Severe complications include secondary infections, bronchopneumonia, sepsis, encephalitis, and infection of the cornea with ensuing loss of vision [10–12]. The current outbreak has been identified mostly in communities of men who have sex with men (MSM) [13]. We describe a case of a 38-year-old man with multiple sexual partners who developed paraphimosis as a complication of monkeypox infection.
HISTORY OF PRESENTATION
A 38-year-old-male patient presented to the emergency department (ED) with complaints of painful genital lesions for six days after having unprotected sexual intercourse with a male partner. Initially, the lesions started as thickening under his foreskin and over the shaft of his penis. Both these lesions evolved to become painful and vesicular. He also noticed small pustular itchy lesions with central umbilication and surrounding redness over his upper and lower extremities, back, and neck (Figs 1 and 2) prompting him to go to urgent care. He was discharged with valacyclovir 1 g every 12 h for 7 days. With no improvement in symptoms, the patient came to the outpatient clinic with complaints of increasing pain and swelling over his glans penis (Fig. 3). He denied dysuria, hematuria, fever, chills, joint or muscle aches, nausea, vomiting, and penile discharge. Physical examination was notable for two painful penile vesicles, one over the shaft and one underneath the foreskin with surrounding edema and erythema, causing painful retraction of his foreskin. Eleven whitish fluid-filled vesicles with central umbilication and surrounding erythema were also noted over both his forearms, neck, forehead, back, and ankle. His vital signs during the initial encounter were normal and was sent to the ED for further workup.
Figure 1.

Multiple central umbilicated lesions over the forearm.
Figure 2.

A closer view of the central umbilicated lesion.
Figure 3.
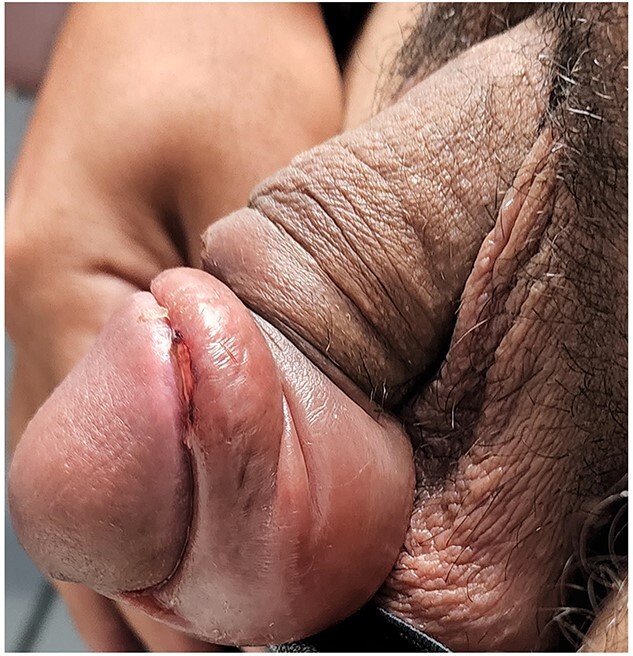
Edema around foreskin leading to paraphimosis.
Sexual history
He had seven sexual partners in the last 5 months and was not consistent with the use of protection.
Investigations
A sexually transmitted infection (STI) panel was made that included polymerase chain reaction (PCR) of herpes simplex virus (HSV), chlamydia, and gonorrhea; treponema pallidum screening test: rapid plasma reagin; treponema pallidum confirmatory test: fluorescent treponemal antibody confirmatory test; human immunodeficiency virus (HIV) fourth generation 1 and 2 antigen and antibody test; and culture for HSV. Because of the monkeypox pandemic, pertinent history, and characteristic lesions, a monkeypox PCR test was also sent. For the HSV and monkeypox PCR tests, two separate swabs were taken from the penile and the skin lesions. The STI panel was negative for HSV, chlamydia, gonorrhea, HIV, and treponema pallidum, however, monkeypox was positive.
Management
Urology and infectious disease consultation were requested. The urology team reduced the paraphimosis following a penile nerve block. The infectious disease team started him on clindamycin 600 mg three times a day for 5 days as a prophylactic treatment to prevent any secondary infection. He was asked to continue his valacyclovir 1 g every 12 h and was asked to follow up after a week or sooner in case the swelling of his foreskin got worse. For his pain, he was prescribed Tylenol 650 mg every 6 h as needed and was asked to quarantine for the duration of his illness. He was followed up after 1 week and mentioned marked improvement in his symptoms.
DISCUSSION
As of 30th September 2022, the Center for Disease Control data shows 26, 049 reported cases in the USA [14].
Our patient presented with a few of the characteristic symptoms of monkeypox including fever, chills, and pustular skin eruptions. Fever often varies between 38.5 and 40.5°C (101.3–104. F) and often declines on the day of or up to 3 days after the onset of the rash. Our patient’s maximum measured temperature was 103 F a day prior to his visit, which was approximately 2 days after the onset of pustular lesions [10]. Monkeypox lesions often present as maculopapular and progress to vesicular or pustular lesions. The number of lesions often varies between a few to thousands. In our patient, there were a total of 11 lesions on the back and upper/lower extremities [8]. Although most of the time the rash first appears on the face and spreads centrifugally, in our patient, the onset of lesions was on the upper back and extremities with one lesion noted over his forehead during the initial encounter [9]. There was no recent travel history, neither was there close contact with wild animals.
In the technical briefing of the UK Health Security Agency on the monkeypox outbreak, 151 of the 152 participants reported being MSM [13]. Our patient reported seven different sexual male partners in the last 5 months with intermittent usage of protection explaining his current symptoms.
In a case series published by Patel et al., 31 out of the 111 participants reported penile edema. Of the 31 participants, 5 had documented paraphimosis and phimosis. This further indicates that paraphimosis is a rare complication but one that needs to be closely monitored in patients with lesions located over the genital region to prevent emergent surgical intervention [15].
At present, treatment remains largely symptomatic. Tecovirimat, Cidofovir, and Brincidofovir are antivirals that can be used [8]. Two vaccines are currently available in the USA [16]. Our patient was treated symptomatically and was asked to isolate for the duration of his illness. He was followed up after 1 week in our outpatient clinic.
Contributor Information
Arun Umesh Mahtani, Department of Medicine, Richmond University Medical Center, Staten Island, NY 10310, USA.
Yolande Mbome Engome, Department of Medicine, Richmond University Medical Center, Staten Island, NY 10310, USA.
Muhammad Haider, Department of Medicine, Richmond University Medical Center, Staten Island, NY 10310, USA.
Thu Minh Vu, Department of Medicine, Richmond University Medical Center, Staten Island, NY 10310, USA.
Crystal Delp, Department of Medicine, Richmond University Medical Center, Staten Island, NY 10310, USA.
Edip Cemil Katayifci, Department of Medicine, Richmond University Medical Center, Staten Island, NY 10310, USA.
Muzhafar Surahio, Department of Medicine, Richmond University Medical Center, Staten Island, NY 10310, USA.
Ambreen Khalil, Department of Infectious Diseases, Richmond University Medical Center, Staten Island, NY 10310, USA.
Azza Elemam, Department of Infectious Diseases, Richmond University Medical Center, Staten Island, NY 10310, USA.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
FUNDING
No financial support.
AUTHOR CONTRIBUTIONS
A.U.M.: prepared, reviewed and edited the manuscript.
Y.M.E.: prepared, reviewed and edited the manuscript.
M.H.: prepared, reviewed edited the manuscript.
C.D.: prepared, reviewed, edited the manuscript.
T.M.V.: edited the manuscript/figures.
E.C.K.: prepared, reviewed, edited the manuscript.
M.S.: proofread and edited the manuscript.
A.K.: proofread and edited the manuscript.
A.E.: proofread and edited the manuscript.
CONSENT FOR PUBLICATION
Consent was obtained from the patient.
References
- 1. Alakunle E, Moens U, Nchinda G, Okeke MI. Monkeypox virus in Nigeria: infection biology, epidemiology, and evolution. Viruses 2020;12:1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ladnyj ID, Ziegler P, Kima E. A human infection caused by monkeypox virus in Basankusu Territory, Democratic Republic of the Congo. Bull World Health Organ 1972;46:593–7. [PMC free article] [PubMed] [Google Scholar]
- 3. Hobson G, Adamson J, Adler H, Firth R, Gould S, Houlihan C, et al. Family cluster of three cases of monkeypox imported from Nigeria to the United Kingdom, May 2021. Euro Surveill 2021;26:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rao AK, Schulte J, Chen TH, et al. Monkeypox in a traveler returning from Nigeria – Dallas, Texas, July 2021. MMWR Morb Mortal Wkly Rep 2022;71:509–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cho CT, Wenner HA. Monkeypox virus. Bacteriol Rev 1973;37:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sklenovská N, Van Ranst M. Emergence of monkeypox as the most important orthopoxvirus infection in humans. Front Public Health 2018;6:241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jezek Z, Grab B, Szczeniowski M, Paluku KM, Mutombo M. Clinico-epidemiological features of monkeypox patients with an animal or human source of infection. Bull World Health Organ 1988;66:459–64. [PMC free article] [PubMed] [Google Scholar]
- 8. Titanji BK, Tegomoh B, Nematollahi S, Konomos M, Kulkarni PA. Monkeypox: a contemporary review for healthcare professionals. Open Forum. Infect Dis 2022;9:ofac310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moore MJ, Rathish B, Zahra F. Monkeypox StatPearls. StatPearls Publishing Copyright © 2022. StatPearls Publishing LLC, Treasure Island, Florida, USA 2022. [Google Scholar]
- 10. Huhn GD, Bauer AM, Yorita K, et al. Clinical characteristics of human monkeypox, and risk factors for severe disease. Clin Infect Dis 2005;41:1742–51. [DOI] [PubMed] [Google Scholar]
- 11. McCollum AM, Damon IK. Human monkeypox. Clin Infect Dis 2014;58:260–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Learned LA, Reynolds MG, Wassa DW, et al. Extended interhuman transmission of monkeypox in a hospital community in the Republic of the Congo, 2003. Am J Trop Med Hyg 2005;73:428–34. [PubMed] [Google Scholar]
- 13. Vivancos R, Anderson C, Blomquist P, Balasegaram S, Bell A, Bishop L, et al. Community transmission of monkeypox in the United Kingdom, April to May 2022. Euro Surveill 2022;27:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.2022 U.S. Map & Case count. Centers for Disease Control and Prevention. https://www.cdc.gov/poxvirus/monkeypox/response/2022/us-map.html (6 October 2022, date last accessed).
- 15. Patel A, Bilinska J, Tam JC, et al. Clinical features and novel presentations of human monkeypox in a central London centre during the 2022 outbreak: descriptive case series. BMJ 2022;378:e072410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Monkeypox. Centers for Disease Control and Prevention . https://www.cdc.gov/poxvirus/monkeypox/index.html. (6 October 2022, date last accessed).


