Case Presentation
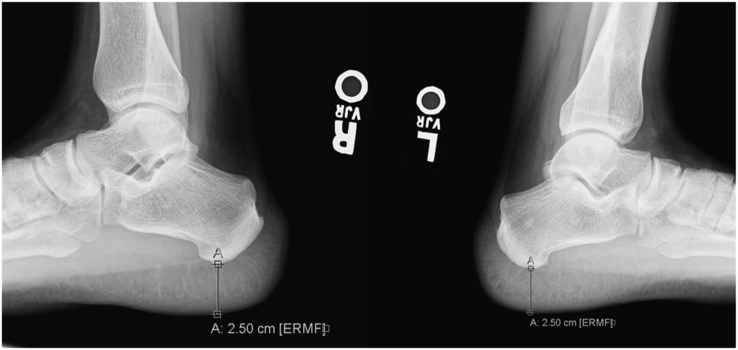
A 24-year-old man presented with blurry vision and bitemporal hemianopia for the past month. He also reported recent fatigue, depression, and decreased libido but denied any changes in glove or shoe size, hyperhidrosis, skin tags, galactorrhea, gynecomastia, muscle weakness, alopecia, heat/cold intolerance, abnormal weight changes, or palpitations. He reported no family history of pituitary adenoma, hyperparathyroidism, or pancreatic tumors. Physical examination was notable for mildly increased frontal bossing and jaw protrusion as noted in his driver’s license along with prominent thenar hypertrophy bilaterally. Pituitary magnetic resonance imaging showed a 2.6-cm partially cystic lesion arising from the pituitary fossa (Fig. 1). Laboratory studies showed the following: (1) insulin-like growth factor 1 (IGF-1) level of 633 ng/mL (reference, 109-353), (2) growth hormone (GH) level of 6.2 ng/mL (reference, 0.0-10.0), (3) prolactin level of 30.6 ng/mL (reference, 4.04-15.2), (4) serum cortisol level of 16.7 mcg/dL (reference, >10), (5) corticotropin level of 41 pg/mL (reference, 7.2-63.3), (6) total testosterone level of 284 ng/dL (reference 264-916), free thyroxine level of 1.03 ng/dL (reference 0.93-1.7), and (7) thyroid-stimulating hormone level of 1.58 mcIU/mL (reference 0.27-4.2). Hand radiographs showed hypertrophied terminal phalangeal tufts (Fig. 2). Lateral ankle radiographs showed a heel pad thickness of 25 mm (reference, <23) (Fig. 3).
Fig 1.
Fig 2.
Fig 3.
What is the diagnosis?
Answer
Acromegaly secondary to a cystic pituitary macroadenoma. Given this patient’s visual field deficits and the risk of mass effect that could pose to his vision, he underwent endonasal transsphenoidal resection. Histology confirmed a GH-secreting tumor. Cystic pituitary adenomas secreting GH can often cause acromegaly and can occur at any age but most often affect middle-aged individuals. While relatively rare, they are the third most prevalent type of pituitary adenoma, after prolactinomas and clinically nonfunctioning adenomas.1 Acromegaly presents clinically through complications resulting from increased peripheral IGF-1 and GH levels along with features of mass effect as seen with this patient. In fact, mass effect is one of its most common presentations, as >65% of GH-secreting adenomas are macroadenomas.2 Bitemporal hemianopia most often occurs secondary to mass effect from a suprasellar mass against the optic chiasm and is a primary indication for tumor resection.3 The widespread complications of elevated IGF-1 and GH levels include visceromegaly, hyperhidrosis, and skeletal and cartilaginous changes. These complications are believed to stem from disordered gene expression of glucose metabolism, cell proliferation, and growth factor functions.2 Surgical resection is often followed by radiation along with medical treatment aimed at normalizing GH levels, with commonly used agents including octreotide, lanreotide, and cabergoline. Our patient recovered well postoperatively with symptom relief; his vision and libido returned to normal; however, the GH and IGF-1 levels were still elevated at 4.4 and 550 ng/mL, respectively. The plan is to initiate somatostatin analog therapy. This case highlights the rare and sometimes subtle physical findings of acromegaly in a patient with a cystic pituitary adenoma, along with the importance of early diagnosis and treatment to minimize possible complications.
Disclosure
The authors have no multiplicity of interest to disclose.
Footnotes
Editor’s Note: Submissions to “Visual Vignettes” are welcomed. Please submit online via the Journal’s Editorial Manager site.
References
- 1.Molitch M.E. Diagnosis and treatment of pituitary adenomas: a review. JAMA. 2017;317(5):516–524. doi: 10.1001/jama.2016.19699. [DOI] [PubMed] [Google Scholar]
- 2.Melmed S. In: The Pituitary. 4th ed. Melmed S., editor. Elsevier Inc; 2017. Acromegaly; pp. 423–466. [Google Scholar]
- 3.Yalamanchili S., Lee A.G. In: Ophthalmology Review: a Case-Study Approach. Singh K., editor. Thieme Medical Publishers, Inc.; 2018. Neuro-ophthalmology; pp. 191–238. [Google Scholar]