Abstract
Reconstruction of the anterior part of the anterior skull base with a nasoseptal flap (NSF) is technically demanding. This challenge is mainly related to the real possible length of the flap. Herein, we describe a new technique for extending the NSF such that it can sufficiently cover the far anterior part of the anterior skull base. Three cadaveric heads were used for mucosal graft extension of the NSF. The graft was harvested from the other side, sutured to the NSF, then repositioned over the skull base after opening all the paranasal sinuses. Each head was operated by a rhinologist and a skull base surgeon. The study variables were the initial length of the NSF, the length of the graft harvested, the new length of the graft-extended NSF, and the length of the new graft-extended NSF from the nasal spine. The average length of the NSFs was 6.4 cm (± 0.2); that of the harvested grafts was 2.93 cm (± 0.1); that of the graft-extended NSF was 9.33 cm (± 0.4); and that of the graft-extended NSF from the nasal spine was 3.93 cm. The graft-extended NSF is an easy and extremely useful technique for the reconstruction of the far anterior parts of the skull base. However, further prospective studies on the clinical usefulness of this technique and its long-term results are yet to be performed.
Level of evidence: IV.
Keywords: Nasoseptal flap, Mucosal graft, Flap extension, Skull base reconstruction
Introduction
Endoscopic skull base surgery is a rapidly developing field. It substitutes open surgical resection in the treatment of several pathologies. An important part of these surgeries is the effective reconstruction of the surgically or pathologically created defects. The principal reconstruction techniques are the nasoseptal flap (NSF) and Hadad-Bassagasteguy flap (HBF) [1]. Using this flap for reconstructing the most anterior part of the skull base—the cribriform plate and the posterior table of the frontal sinus—remains challenging. Therefore, many alternative, sophisticated flaps have been proposed to achieve noble reconstruction of the cribriform plate and frontal posterior table [2, 3]. In this study, we describe a novel and easy technique in which the conventional NSF and HBF is extended using a mucosal graft.
Methods
This study was conducted on three cadaveric heads by three rhinologists and neurosurgeons. Each head was operated on by one surgeon. The Draf III procedure was used to open all paranasal sinuses. The NSF is elevated on one side, and a mucosal graft is harvested from the floor and inferior meatus of the other side. The harvested graft was sutured to the caudal end of the NSF using absorbable sutures. The novel graft-extended NSF was repositioned over the skull from planum to the posterior table of the frontal sinus (Figs. 1 and 2). The width of the NSF on one side and the graft from the other side can be adjusted according to the needed reconstruction area. This width can extend from the septum to the inferior turbinate. We measured the length of the NSF along with the graft extension. We also measured the length of the harvested graft, along with the extent to which the new graft-extended flap can reach without tension, as well as the length of the graft-extended NSF from the anterior nasal spine.
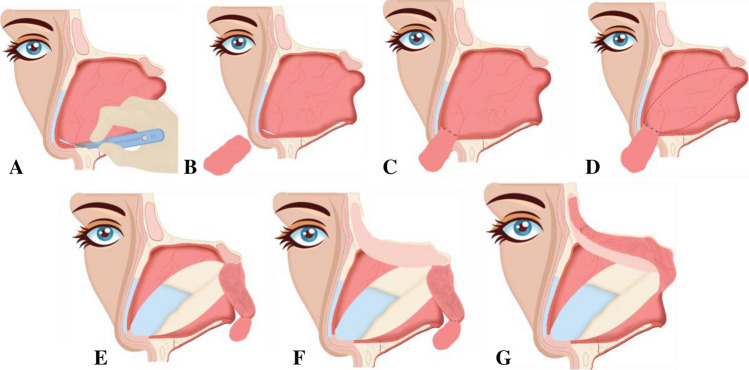
Fig. 1.
Illustration of the technique. a Incision for the NSF. b Mucosal graft obtained from the other side of the nasal cavity. c Mucosal graft is sutured to the caudal part of the NSF. d The NSF is elevated. e NSF + graft applied in the nasopharynx. f Preparing the defect site. g Placement of the flap + graft over the defect site. NSF nasoseptal flap
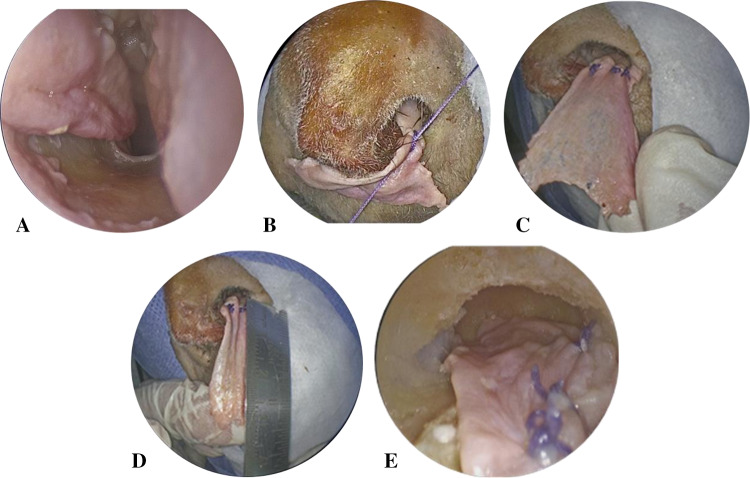
Fig. 2.
The graft-extended NSF. a The graft donor site from the other side of the nasal floor. b Suturing the harvested graft to the NSF. c The graft sutured to the flap. d Added length of the flap by the graft. e The graft-extended NSF reaching the uppermost part of the frontal sinus posterior table without any tension. NSF nasoseptal flap
Results
In our study, the average NSF length was 6.43. ± 0.2 cm, with a graft gain of 2.93. ± 0.23 cm. The width of the graft can be adjusted according to the available extent from the septum to the inferior turbinate. The average total length of the graft-extended NSF was 9.33 cm (Table 1). A comparison was made between the flap with reference to the posterior wall of the frontal sinus before and after the graft extension. The NSF was limited just proximal to the frontal sinus. The extended flap reached the roof of the frontal sinus (Fig. 2).
Table 1.
The length added to the NSF with the new technique
| Head No | Length of the NSF (cm) | Length of the graft (cm) | Accumulative length of the extended NSF (cm) | Length from the anterior nasal (cm) |
|---|---|---|---|---|
| 1 | 6.4 | 3 | 9.4 | 4 |
| 2 | 6.6 | 3.1 | 9.7 | 4 |
| 3 | 6.2 | 2.7 | 8.9 | 3.8 |
| Average | 6.4 | 2.93 | 9.33 | 3.93 |
Discussion
In this cadaveric study, we established a novel and simple method to extend the NSF, which gives an additional length of 3 cm, allowing the easy use of this flap for reconstruction of the far anterior part of the skull base.
The benefit of NSF in preventing cerebrospinal fluid (CSF) leakage and mediating rapid healing has been well established. However, it fails to cover the far anterior defects because of size limitations. In our experience, a free graft is more appropriate to cover defects, such as the primary component. The graft is technically more challenging during manipulation and placement owing to the lack of anchoring, and therefore the graft has a relatively higher chance of migration, as seen in cases of postoperative CSF leak. Our newly proposed technique aims to combine the benefit of the NSF with the free graft by enhancing its stability and improving the chance for vascularization from the NSF pedicle.
The introduction of endoscope in skull base surgeries has led to tremendous gains in decreasing the overall invasiveness of such procedures. This technological advent indeed markedly improved the surgical outcomes. Further advancement with extended endoscopic skull base surgery enhanced our capability of tackling wider skull base territories. However, such practices have been faced with a myriad obstacles, mostly related to adequate reconstruction of the resulting skull base defect, which mainly manifests as postoperative CSF leak [4–7].
Wigand [8], initially proposed the use of a mucosal graft for skull base reconstruction. It has become one of the major facets of the endoscopic technique. Further development of multiple variations and subsequent use of vascularized flaps by Hadad et al. [1] resulted in the global acceptance of endoscopic techniques, primarily because of their superior results in preventing postoperative CSF leak, relative to graft reconstruction; moreover, the surgical outcomes were comparable to traditional open techniques using regional vascularized flap (periosteal flap) [9].
Despite its main advantage in reducing postoperative CSF leak, the classic NSF (HBF) did not fully replace the use of grafts in cases of large anterior skull base defect reconstruction because of its size limitations. Several modifications have been proposed to expand the flap area of coverage. Basset et al. described an extra third incision coursing along the maxillary crest from the posterior edge to the middle portion of the flap. This cut extends the flap length by an average of 1.9 cm [10]. Boetto et al. and Wu et al. described an alternative method for flap extension, wherein they combined both NSFs with the inferior turbinate flap with variation in pedicle supply [11, 12]. Recently, Shastri et al. described a new technique to extend the NSF by fully dissecting the sphenopalatine and internal maxillary arteries, and transecting the descending palatine artery. They reported an increase in the length of the NSF by 5–6 cm [13]. Achieving such excellent addition to the existing NSF length is highly risk to the flap pedicle as it requires high technical skills and meticulous dissection. All the previously mentioned studies and techniques are valid options for extended skull base procedures. Nevertheless, these techniques might be considered extensive in cases of far anterior skull base defects.
Despite the strengths, our study is limited by the use of a small number of cadaveric specimens with no clinical validation of its applicability. Further prospective clinical application and long-term follow-up are warranted to determine the healing potential and rate of postoperative CSF leak with graft-extended NSF.
Conclusion
This study proposes a new, promising technique to improve reconstruction and healing of the anterior skull base defect using vascularized NSF with graft extension. However, further clinical studies are needed to assess the wound healing and long-term postoperative surgical outcomes.
Acknowledgements
The authors extend their appreciation and gratitude to the Saudi Association of Neurological Surgery (SANS) for offering cadaveric heads to conduct this demonstration trial as part of the skull base surgery course.
Funding
This study did not receive any funding.
Compliance with Ethical Standards
Conflict of interest
None declared.
Ethical approval
This cadaveric demonstration and assessment of the extended flap additional length were performed in part of an endoscopic skull base surgery course and no IRB review was requested for it.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hadad G, Bassagasteguy L, Carrau RL, et al. A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope. 2006;116:1882–1886. doi: 10.1097/01.mlg.0000234933.37779.e4. [DOI] [PubMed] [Google Scholar]
- 2.Castelnuovo P, Ferreli F, Khodaei I, Palma P. Anterior ethmoidal artery septal flap for the management of septal perforation. Arch Facial PlastSurg. 2011;13(6):411–414. doi: 10.1001/archfacial.2011.44. [DOI] [PubMed] [Google Scholar]
- 3.Hadad G, Rivero-Serrano CM, Bassagaisteguy LH, et al. Anterior pedicle lateral nasal wall flap: a novel technique for the reconstruction of anterior skull base defects. Laryngoscope. 2011;121:1606–1610. doi: 10.1002/lary.21889. [DOI] [PubMed] [Google Scholar]
- 4.Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL. Expanded endonasal approach: the rostrocaudal axis. Part II. Posterior clinoids to the foramen magnum. Neurosurg Focus. 2005;19:E4. [PubMed] [Google Scholar]
- 5.Kassam A, Gardner P, Snyderman CH, Mintz A, Carrau R. Expanded endonasal approach: fully endoscopic, completely transnasal approach to the middle third of the clivus, petrous bone, middle cranial fossa, and infratemporal fossa. Neurosurg Focus. 2005;19:E6. doi: 10.3171/foc.2005.19.1.7. [DOI] [PubMed] [Google Scholar]
- 6.Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL. Expanded endonasal approach: the rostrocaudal axis. Part I. Crista galli to the sella turcica. Neurosurg Focus. 2005;19:E3. [PubMed] [Google Scholar]
- 7.Kassam A, Carrau RL, Snyderman CH, Gardner P, Mintz A. Evolution of reconstructive technique following endoscopic expanded endonasal approaches. Neurosurg Focus. 2005;19:E8. doi: 10.3171/foc.2005.19.1.9. [DOI] [PubMed] [Google Scholar]
- 8.Wigand ME. Transnasal ethmoidectomy under endoscopical control. Rhinology. 1981;19:7–15. [PubMed] [Google Scholar]
- 9.Harvey RJ, Parmar P, Sacks R, Zanation AM. Endoscopic skull base reconstruction of large dural defects: a systematic review of published evidence. Laryngoscope. 2012;122:452–459. doi: 10.1002/lary.22475. [DOI] [PubMed] [Google Scholar]
- 10.Bassett E, Farag A, Iloreta A, et al. The extended nasoseptal flap for coverage of large cranial base defects. Int Forum Allergy Rhinol. 2016;6:1113–1116. doi: 10.1002/alr.21778. [DOI] [PubMed] [Google Scholar]
- 11.Boetto J, Labidi M, Watanabe K, et al. Combined nasoseptal and inferior turbinate flap for reconstruction of large skull base defect after expanded endonasal approach: operative technique. OperNeurosurg (Hagerstown) 2019;16:45–52. doi: 10.1093/ons/opy046. [DOI] [PubMed] [Google Scholar]
- 12.Wu P, Li Z, Liu C, Ouyang J, Zhong S. The posterior pedicled inferior turbinate-nasoseptal flap: a potential combined flap for skull base reconstruction. SurgRadiolAnat. 2016;38:187–194. doi: 10.1007/s00276-015-1516-6. [DOI] [PubMed] [Google Scholar]
- 13.Shastri KS, Leonel LC, Patel V, et al. Lengthening the nasoseptal flap pedicle with extended dissection into the pterygopalatine fossa. Laryngoscope. 2020;130:18–24. doi: 10.1002/lary.27984. [DOI] [PubMed] [Google Scholar]