Abstract
The shape and position of middle turbinate play an important role in ventilation and drainage of the osteomeatal complex. The preservation of middle turbinate is one of the major goals of functional endoscopic sinus surgery (FESS). Middle turbinate intervention is essential to prevent obliteration of osteomeatal complex. The aim of this prospective study is to postulate which middle turbinate intervention is most effective and compare the results with conventional technique. In this randomized controlled study, 60 patients were included of the age group of 15–60 years who presented to the Otorhinolaryngology OPD of our institute between November 2017 to June 2019 with symptoms of chronic sinusitis with clinical and radiological evidence and who underwent FESS. The patients were divided into three group, Group A—Bolgerization (n = 20), Group B—Vicryl—conchopexy (n = 20) and Group C—No intervention, Control group (n = 20). The patency of middle meatus and the status of middle turbinate (medialized or lateralized or neither of the two) was ascertained postoperatively. Improvement in symptoms was also evaluated. The middle turbinate was medialized in 90% of Group A and 95% of Group B cases. The middle turbinate was neither medialized nor lateralized in 70% of patients in Group C. 70% of the patients in Group A and 80% of patients in Group B had complete improvement in symptoms with no recurrence of sinusitis compared to Group C in which only 50% of the patients had improvement in symptoms due to development of synechiae. Medialization of the middle turbinate should be considered as one of the essential steps of FESS as it helps in improving the surgical outcome.
Keywords: Middle turbinate medialization, Middle turbinate intervention, FESS, Chronic sinusitis, Nasal polyposis, Synechiae
Introduction
The endoscopic sinus surgery (ESS) is considered as one of the widely performed procedures in rhinology. Since 1985 there have been continuous advances to improve the outcome which still depends on intervention on the middle turbinate as the cornerstone for relieving nasal obstruction and establishing drainage of most of the paranasal sinuses. ESS is based universally on providing sufficient ethmoidal infundibulectomy through performance of a complete uncinectomy. Despite adequate uncinectomy there is a risk for reobliteration of ethmoidal infundibulum with lateralized ipsilateral middle turbinate [1]. It is a well-known fact that the ethmoidal infundibulum is the main draining space of the osteomeatal complex which is bounded posteriorly by bulla ethmoidalis, anteromedially by the middle turbinate, and anterolaterally by the uncinate process. Therefore, in addition to uncinectomy and resection of bulla ethmoidalis, it is necessary to interfere with the middle turbinate to achieve enough ethmoidal infundibulectomy at the anteromedial aspect.
A pathological middle turbinate such as hypertrophied, pneumatized, paradoxical, floppy or duplicated middle turbinate plays a significant role in the pathogenesis of recurrent sinusitis by mechanical obliteration of the osteomeatal complex and needs to be interfered with surgery. Banfield et al. [2] have reported partial resection of middle turbinate as a useful modification of ESS.
It was found that the infracturing the middle turbinate to achieve access to the middle meatus during surgery is associated with a high risk for postoperative lateralization either due to bulk of the turbinate itself or due to development of synechiae. Hence in endoscopic surgery, it is required to interfere with the middle turbinate to maintain the patency of the middle meatus.
The middle turbinate should be assessed by means of endoscopy and imaging before surgery. An abnormal middle turbinate must be interfered with accordingly by means of lateral resection of concha bullosa, partial turbinectomy of hypertrophied turbinate, or resection of lower part for floppy middle turbinate. In addition, paradoxical and duplicated middle turbinates can be dealt with, by resecting the part of middle turbinate that causes obstruction. A normal looking middle turbinate can be managed by using different recommended techniques:
Deliberate creation of synechiae between nasal septum and middle turbinate by abrading medial wall of middle turbinate and adjoining septal mucosa using a microdebrider. This is called Bolgerization [3].
Fixation of the middle turbinate to the nasal septum by suturing the mucosa of the middle turbinate to the mucoperiosteal flap of the nasal septum using a vicryl suture material. This technique is described as the conchopexy [4].
Medialization and Stabilization of the Middle Turbinate using a Nasal Septal Flap [5].
The present study is an attempt to assess the outcome of middle turbinate intervention in endoscopic sinus surgery.
Objectives
To confirm the significance of middle turbinate intervention as one of the important steps for ESS.
To assess the outcomes of middle turbinate intervention techniques after ESS.
To compare these techniques and conclude as to which technique has the best results after ESS.
Method
Study population The study population consists of sixty patients with chronic sinusitis and/or nasal polyposis who presented to us with clinical as well as radiological evidence of sinusitis and polyposis and underwent ESS.
Study area Department of ENT, SDM College of Medical Sciences and Hospital, Dharwad.
Study period From November 2017 to June 2019.
Study design Randomized controlled study
Sample size 60 patients were included in the study, 20 patients underwent Bolgerization, 20 patients underwent Conchopexy and 20 patients underwent no active intervention on the middle turbinate. These patients were followed up on 7th postoperative day and after 6 weeks of surgery and were evaluated for postoperative relief of symptoms. Sample size estimation:
Sample size estimation The previous year’s hospital statistics in SDM Medical College and Hospital, of patients presenting with at least chronic rhinosinusitis with or without polyposis was found to be 45 cases. Based on this a minimum sample size of 60 patients was expected to be included in this study.
Study analysis Descriptive statistics were applied. Data was analyzed by proportions and percentages. Further Chi-square test was applied to find out association between two attributes. Statistical significance was set at 0.05% level of significance (p < 0.05).
Inclusion Criteria
Patients with chronic sinusitis who presented with clinical and radiological evidence of maxillary and ethmoidal sinusitis with or without frontal and sphenoid sinus involvement.
Patients with nasal polyposis with clinical as well as radiological evidence of the same.
Age Group—15–60 years.
Exclusion Criteria
Patients less than 14 years.
Patients who had already undergone ESS (revision case) or any other endoscopic rhinological operative intervention.
Patients with chronic granulomatous disease.
Patients with benign and malignant nasal tumors.
Materials and Method
During the study period, cases of chronic sinusitis and nasal polyposis posted for ESS, willing to give a written informed consent to participate, were enrolled in the trial. Basic socio-demographic data (Figs. 1, 2) and clinical history were obtained (Table 1). Among the study population, 43 patients were male (71.6%) and 17 patients were female (29.4%). The Chi-square test (p < 0.720) was not significant. Each patient then underwent anterior rhinoscopy, diagnostic nasal endoscopy, computerized tomography of the paranasal sinuses and the findings were recorded. Laboratory investigations were also noted. The patients were randomly allotted into three groups- Group A, B and C.
Fig. 1.
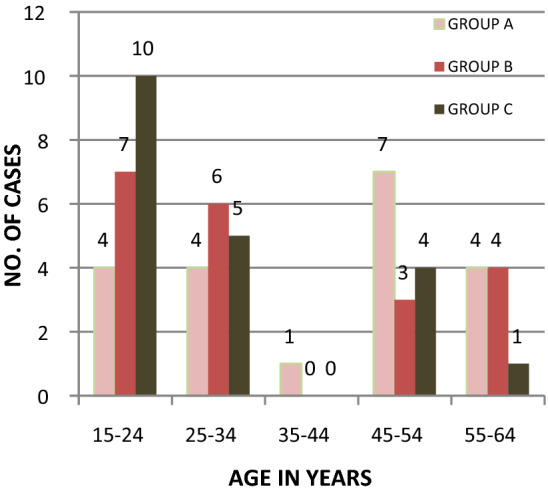
Age distribution
Fig. 2.
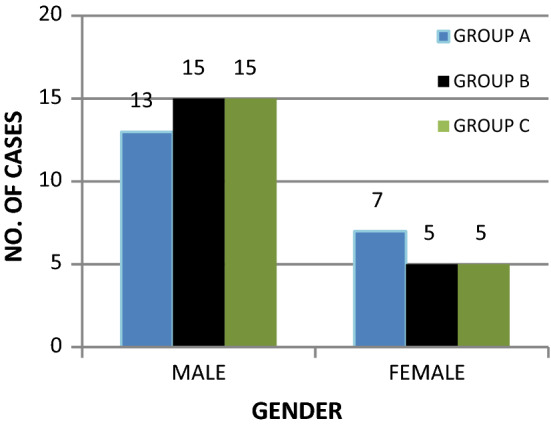
Gender distribution
Table 1.
Pre-operative symptoms
| Pre-op. symptoms | Groups | p-value | ||
|---|---|---|---|---|
| Group-A | Group-B | Group-C | ||
| Facial pain/facial congestion | 0 | 0 | 1 | 0.362, NS |
| Headache | 6 | 5 | 7 | 0.788, NS |
| Nasal obstruction | 15 | 15 | 16 | 0.911, NS |
| Rhinorrhea | 1 | 1 | 0 | 0.596, NS |
| PND | 0 | 0 | 1 | 0.362, NS |
NS not significant
The study included patients with chronic rhinosinusitis (CRS + NP) with nasal polyposis and chronic rhinosinusitis sans nasal polyposis (CRSsNP).
In group A 12 patients had CRS + NP and 8 patients had CRSsNP.
In group B 10 patients had CRS + NP and 10 patients had CRSsNP.
In group C 8 patients had CRS + NP and 12 patients had CRSsNP
Surgical Procedure
Informed consent was taken from all the patients for the planned procedure in proforma approved by our institutional ethical committee (SDMIEC) and the procedure used in the study adheres to the tenets of Declaration of Helsinki. Endoscopic sinus surgery was done in all the patients. The internationally recommended steps of basic ESS are as follows:
Infracturing of ipsilateral middle turbinate to achieve access to the middle meatus.
Uncinectomy.
Anterior ethmoidectomy which was performed by means of complete exenteration of bulla ethmoidalis.
Posterior ethmoidectomy, which was performed by means of resection of the vertical portion of the basal lamella of the middle turbinate and further exenteration of posterior ethmoidal air cells.
Draf-I frontal sinusotomy and/or sphenoidotomy, which was performed using preserved as well as non-preserved Bullar techniques.
Middle meatal antrostomy, which was performed subsequently. At beginning of the surgery, the contour of the middle turbinate with the most lateral part of the uncinate process was preserved just to be used as significant anatomical landmarks for finishing safe and proper further resection steps.
Finally, the intervention with the middle turbinate was performed accordingly.
GROUP A: 20 patients underwent synechiae formation between middle turbinate and adjoining septum by creating raw surface by abrading intervening mucosal surface using debrider -Bolgerization
GROUP B: 20 patients underwent Middle turbinate medialization where the mucosa of the turbinate was sutured with adjoining mucoperiosteal flap of septum using vicryl—Conchopexy.
GROUP C: 20 patients underwent no active intervention on the middle turbinate.
Postoperative treatment and follow up: Patients were discharged on 2nd postoperative day. Antibiotic, antihistamines and nasal drops were given to all patients for a period of one week. All patients were followed-up on postoperative day 7 and after 6 weeks to look out for any occurrence of postoperative middle meatal obliteration with synechiae or lateralization of the ipsilateral middle turbinate. The three groups were compared to each other with respect to postoperative improvement in terms of symptomatology and endoscopic findings. (Table 2).
Table 2.
Post-operative symptoms
| Post-op. symptoms | Groups | p-value | ||
|---|---|---|---|---|
| Group-A | Group-B | Group-C | ||
| No complaints | 14 | 16 | 10 | 0.122, NS |
| Nasal obstruction | 0 | 2 | 6 | 0.01, S |
| Headache | 3 | 0 | 3 | 0.189, NS |
| Rhinorrhea | 0 | 2 | 2 | 0.342, NS |
| PND | 0 | 0 | 1 | 0.362, NS |
NS not significant, S significant
Results
After the first postop week, Group A showed only one case where middle turbinate was lateralized which was statistically significant whereas in Group B there was no lateralization and all the cases showed medialization which is statistically significant. Group C showed neither medialization nor lateralization in any of the cases in the first postoperative week. Crusting in the middle meatus was common during the first week which is expected after every FESS surgery and alkaline nasal douching was advised. (Table 3).
Table 3.
Middle turbinate status after 1 week
| Post-op. findings | Groups | Chi-square test | |||
|---|---|---|---|---|---|
| Group A | Group B | Group C | |||
| Right | Middle turbinate medialized | 19 | 20 | 0 | p < 0.000, HS |
| Middle turbinate lateralized | 1 | 0 | 0 | ||
| No middle turbinate medialization of lateralization | 0 | 0 | 20 | ||
| Left | Middle turbinate medialized | 20 | 20 | 0 | p < 0.000, HS |
| No middle turbinate medialization of lateralization | 0 | 0 | 20 | ||
HS highly significant
After the 6th postoperative week, 18 cases in group A had medialized middle turbinate and only 2 cases had lateralized turbinates which was statistically highly significant. Group B showed 19 cases of medialized middle turbinates and only 1 case showed lateralization. This too was statistically highly significant. Group C showed 14 patients where the turbinate was neither medialized nor lateralized and 6 patients had lateralization which was statistically highly significant. (Table 4).
Table 4.
Middle turbinate status after 6 weeks
| Post-op. symptoms | Groups | Chi-square test | |||
|---|---|---|---|---|---|
| Group A | Group B | Group C | |||
| Right | Middle turbinate medialized | 18 | 18 | 1 | p < 0.000, HS |
| Middle turbinate lateralized | 2 | 1 | 5 | ||
| No middle turbinate medialization of lateralization | 0 | 0 | 14 | ||
| Left | Middle turbinate medialized | 18 | 19 | 1 | p < 0.000, HS |
| Middle turbinate lateralized | 2 | 1 | 5 | ||
| No middle turbinate medialization of lateralization | 0 | 0 | 14 | ||
| HS = Highly significant | |||||
In Group A, turbinate lateralization seen in 2 cases during the 6th postoperative week was due to extensive polypoidal changes in the mucosa. In Group B, one case of middle turbinate lateralization 6 weeks postoperatively was due to boggy nasal septum with mucopurulent discharge lateralizing the middle turbinate. In Group C, six cases had synechiae between the lateral nasal wall and middle turbinate leading to lateralization and recurrence of symptoms. Interestingly, in the Group A, one case where the middle turbinate was found to be lateralized during the first week postoperatively was found to be medialized during the sixth week as a result of gelfoam application endoscopically during the first postoperative week follow-up. There were 4 patients in the group A and 4 patients in group B who had symptoms 6 weeks postoperatively despite the middle turbinate being in medialized position.
By using discussed techniques in this study, high rates of middle turbinate medialization were achieved. The Bolgerization technique achieved 90% success rate of medialization but failed to prevent lateral synechiae in 10% of patients. As expected, successful medialization was associated with high rate of asymptomatic patients (70%). Similarly conchopexy suture technique achieved 95% success rate of medialization but failed to prevent lateralization in 5% of patients and this success was associated with 80% of patients being asymptomatic. Conventional FESS without any middle turbinate intervention (group C) had a success rate of 70% in terms of the turbinate being neither medialized nor lateralized and this technique resulted in a far lower rate of asymptomatic patients (50%).
Discussion
In 1978, Messerklinger [6] published the first systematic and detailed work documenting endoscopic findings. It was popularized in Europe by Stammberger, and in North America by Kennedy. FESS (functional endoscopic sinus surgery) has been accepted as a minimally invasive technique for treatment of chronic rhinosinusitis (CRS) resistant to medical therapy. FESS restores sinus drainage, improves mucociliary clearance and reverts the sinus function to normal [7, 8]. Many studies have demonstrated the success of FESS. Nayak et al. [9] studied a group of 78 patients with CRS over a period of 16 months and found that 47 of these patients had total relief, 12 had partial relief and 7 had no relief. A retrospective study by Fageeh et al. [10] of 129 patients with CRS refractory to medical treatment and who underwent FESS revealed 85% of the patients had a satisfactory improvement.
Middle turbinate is the key structure recognized in FESS. Adequate intervention on a normal middle turbinate remains controversial. It is recommended for maintaining the patency of osteomeatal complex as it achieves two purposes.
Sufficient drainage and ventilation for all the sinuses.
Provides wide access to facilitate endoscopic postoperative activities like suction and removal of pathologies like granulations, polyps and synechiae.
Others tried to solve the problem by partial or complete resection of middle turbinate. In a systematic review done by Choby et al. [11] they concluded that middle turbinate can be resected when appropriately indicated and there is no adverse effect compared to middle turbinate preservation in terms of outcome. Although the nose can function without middle turbinate, it should be preserved whenever possible. It plays a vital role in directing airflow, humidifying inspired air, mucociliary transport of particulate matter and providing local immunity by secreting IgA.
Shih et al. did not find any deleterious effect of middle turbinate resection on the results of ESS while Ramadan et al. did not find a significant statistical decrease in the rate of lateral synechiae formation in patients who underwent partial resection of middle turbinate as the superior part of the turbinate that is preserved may lateralize and cause iatrogenic frontal sinus obstruction [12, 13]. There are exceptions to middle turbinate preservation policy. It is probably not worthy preserving it when there is marked inflammation, polypoidal changes or trauma. It may be better to perform a partial resection than to leave a large raw surface for potential adhesions and lateralization.
A study was conducted by Bofares on the effect of middle turbinate interventions in outcomes of ESS in 60 patients. Nearly 49% of the patients who underwent just infracturing of the turbinate without any further fixations developed symptoms either due to lateral synechiae formation or due to lateralization of middle turbinate [1].
Friedman and Landsberg [14] reported lateralization of middle turbinate as the most common complication (43%) of FESS which leads to synechiae and scarring and subsequent surgical failure. Excessive synechiae between the middle turbinate and the lateral wall disrupts local mucociliary clearance. Blockage in the osteomeatal complex results in recurrent sinus infection. Following uncinectomy and middle meatal antrostomy a raw area is created on the lateral nasal wall. Abraded lateral surface of the turbinate and further mobilization results in instability, scarring and lateralization. Therefore, medialization of middle turbinate is essential to minimize problems in the postoperative period and ensure successful outcome. Moreover, the anterior aspect of the turbinate is attached to the skull base and should be carefully handled to avoid CSF leak.
Researchers ponder on which is the most suitable intervention on the middle turbinate. Several techniques have been designed to keep middle turbinate medialized, allow aeration of sinuses and delivery of topical steroids if indicated following surgery as in case of polyposis. These include middle meatal packing using absorbable (Nasopore) or nonabsorbable (Merocel) spacer, silastic splint placement, nasal septal flap, Bolgerization and conchopexy.
A study was conducted by Baky et al. [15] to prevent lateralization of middle turbinate after FESS. Partial resection of middle turbinate was done in 20 patients. 80% patients had improvement in symptoms following surgery and only 10% developed synechiae with no lateralization and better stability of the turbinate. Medialization and stabilization of the middle turbinate using a nasal septal flap allows precise determination of site of medial synechia. It can be done without using a microdebrider and is useful in cases of unstable turbinates [5]. Hu et al. studied the effects of Meropacking of the middle meatus after FESS in 60 children with CRS and concluded that it did not significantly reduce the formation of synechiae and its use can be reserved for revision cases or when there is large denuded area on the turbinate [16]. Baguley et al. placed silastic splint in the middle meatus on one side of the nose in 33 patients for 2 weeks following ESS and the other side was not splinted. There no adhesions on the splinted side compared to the 9 on nonsplinted side at the end of 12 weeks of follow- up [17]. Grisel et al. [18] used bioresorbable implant which has three lateral barbs inserted to middle turbinate and one medial barb fastened to nasal septum with 100% success in medicalization. Xu et al. used steroid-impregnated spacer after ESS in 146 patients and compared the results with 128 patients in whom nonabsorbable spacer was placed in middle meatus. There was no statistically significant reduction in postoperative synechiae formation when the two groups were compared [19]. Zhao et al. [20] did a systematic review comparing nonabsorbable, absorbable and steroid impregnated spacers and concluded that there was no significant difference in adhesion rates between the first two groups but steroid spacers might reduce adhesions.
The technique of Bolgerization was published by Bolger et al. [3] and has become popular ever since. Mucosal abrasion was created on medial aspect of the anteroinferior portion of middle turbinate and the adjacent septal mucosa using sickle knife or microdebrider. Subsequently, nasal packing of the middle meatus was done to medialize the turbinate and approximate against both raw surfaces. Dutton et al. [4] suggested it was effective in prevention of lateralization in as many as 88% of patients. In our study, prevention of lateralization was 90%.
Friedman and Schalch did Bolgerization using microdebrider and applied BioGlue to fix middle turbinate to nasal septum followed by application of pressure. This allowed the adhesive to polymerize and prevented the use of middle meatal packing [21]. Friedman et al. and Dutton et al. and also found no adverse effect on olfaction in patients who underwent Bolgerization and Conchopexy respectively [4, 22].
Conchopexy is done using a 3-0 Vicryl suture with the needle straightened partially for easy passage through the tissue. The needle is introduced into the nasal cavity oriented vertically, visualized with a nasal 0 degree scope and passed through the head of middle turbinate septum and contralateral middle turbinate in a single pass. It is then brought back to opposite middle turbinate and passed through the septum to initial side to be knotted. This intervention is technically difficulty and lengthens the operating time. It was described by Hudson et al. [4] as a definite method to prevent lateralization with 90–92% success rate. The success rate in our study was 95%.
Chen et al. [23] study of Conchopexy vs. absorbable nasal packing of middle meatus using Nasopore in 120 patients also revealed Conchopexy as an effective medialization procedure with 95% success. Thornton [24] described middle turbinate stabilization with transeptal suturing of the turbinate in 30 cases (60 operated sides) and only 1 patient had lateralization (97% success). Lee and Marple [25] suggested that Conchopexy done at the beginning of surgery significantly improves access to the middle meatus as well as the postoperative outcomes.
Bolgerization may fail if the abraded surfaces are not opposed precisely or the nasal pack is placed between middle turbinate and septum inadvertently. Conchopexy may fail if the suture is taken far too posteriorly. The superior attachment of middle turbinate serves as an axis, bringing the anterior edge of turbinate closer to the lateral nasal wall.
Conclusion
Medialization techniques should not be considered as an adjunct while performing FESS and should be included as an essential step of FESS as it can have a profound impact on the surgical outcome. It can be done in the beginning of the surgery to improve access to middle meatus or at the end of the surgery to prevent adhesions postoperatively. Both Bolgerization and Conchopexy are effective in preventing lateralization and improving symptoms following FESS while having no other adverse effect.
Funding
This research received no specific grant from any funding agency in the public, commercial or not—for—profit sectors.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
Institutional review board at SDM College of medical sciences & hospital, Dharwad approved the study for publication.
Informed Consent
Written informed consent was obtained from all the patients.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bofares KM. Effect of middle turbinate intervention on outcomes of middle meatal endoscopic surgery. Pan Arab J Rhinol. 2016;06:27–32. doi: 10.4103/2090-7540.186905. [DOI] [Google Scholar]
- 2.Banfield GK, McCombe A. Partial resection of middle turbinate at functional endoscopic sinus surgery. J R Army Med Corps. 1999;145:18–12. doi: 10.1136/jramc-145-01-05. [DOI] [PubMed] [Google Scholar]
- 3.Bolger WE, Kuhn FA, Kennedy DW. Middle turbinate stabilization after functional endoscopic sinus surgery: the controlled synechiae technique. Laryngoscope. 1999;109:1852–1853. doi: 10.1097/00005537-199911000-00025. [DOI] [PubMed] [Google Scholar]
- 4.Dutton JM, Hinton MJ. Middle turbinate suture conchopexy during endoscopic sinus surgery does not impair olfaction. Am J Rhinol Allergy. 2011;25(2):125–127. doi: 10.2500/ajra.2011.25.3560. [DOI] [PubMed] [Google Scholar]
- 5.Abelardo E, Sanuki T, Yumoto E (2005) Medialization and stabilization of the middle turbinate using a nasal septal flap in endoscopic sinus surgery. Philipp J Otolaryngol Head Neck Surg 21(1–2):42–44
- 6.Messerklinger W (1978) Endoscopy of the nose and paranasal sinuses. Urban and Schwartzenberg
- 7.Stammberger H (986). Endoscopic sinus surgery-concepts in treatment of recurring rhinosinusitis. Part-I. Anatomic and pathophysiologic considerations. Otolaryngol Head Neck Surg 29(2): 143–147. [DOI] [PubMed]
- 8.Stammberger H (1986) Endoscopic sinus surgery-concepts in treatment of recurring rhinosinusitis. Part-II. Surgical technique. Otolaryngol Head Neck Surg 29(2):147–156. [DOI] [PubMed]
- 9.Nayak SR, Kirtane MV, Ingle MV. Functional endoscopic sinus surgery—a preliminary study. J Post grad Med. 1991;37:31–34. [PubMed] [Google Scholar]
- 10.Fageeh NA, Peluausa EO, Quarrington A. Functional endoscopic sinus surgery-University of Ottawa experience and an overview. Ann Saudi Med. 1996;16(6):711–714. doi: 10.5144/0256-4947.1996.711. [DOI] [PubMed] [Google Scholar]
- 11.Choby GW, Hobson CE, Lee S, Wang EW (2014) Clinical effects of middle turbinate resection after endoscopic sinus surgery: a systematic review. Am J Rhinol Allergy 28(6):502–507. [DOI] [PubMed]
- 12.Shih C, Chin G, Rice DH. Middle turbinate resection: impact on outcomes in endoscopic sinus surgery. Ear Nose Throat J. 2003;82(10):796–797. doi: 10.1177/014556130308201013. [DOI] [PubMed] [Google Scholar]
- 13.Ramadan HH. Nonsurgical versus endoscopic sinonasal surgery for rhinogenic headache. Am J Rhinol. 1999;13(6):455–457. doi: 10.2500/105065899781329656. [DOI] [PubMed] [Google Scholar]
- 14.Friedman M, Landsberg R, Tanyeri H. Middle turbinate medialization and preservation in endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2000;123:76–80. doi: 10.1067/mhn.2000.105921. [DOI] [PubMed] [Google Scholar]
- 15.Baky HM, Azzem HMA, Ras AB (2001) Evaluation of partial middle turbinate resection during functional endoscopic sinus surgery. Benha Med J 18(3 part 2): 665–676
- 16.Hu KH, Lin KN, Li WT, Huang HM. Effects of Meropack in the middle meatus after functional endoscopic sinus surgery in children with chronic sinusitis. Int J Pediatr Otorhinolaryngol. 2008;72(10):1535–1540. doi: 10.1016/j.ijporl.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 17.Baguley CJ, Stow NW, Weitzel EK, Douglas RG (2012) Silastic splints reduce middle meatal adhesions after endoscopic sinus surgery. Am J Rhinol Allergy 26(5):414–417 [DOI] [PubMed]
- 18.Grisel JJ, Atkin JH, Fleming DJ, Kuppersmith RB (2011) Clinical evaluation of a bioresorbable implant for medialization of the middle turbinate in sinus surgery. Int Forum Allergy Rhinol 1(1): 33–37 [DOI] [PubMed]
- 19.Xu JJ, Busato GM, McKnight C, Lee JM. Absorbable steroid-impregnated spacer after endoscopic sinus surgery to reduce synechiae formation. Ann Otol Rhinol Laryngol. 2016;125(3):195–198. doi: 10.1177/0003489415606446. [DOI] [PubMed] [Google Scholar]
- 20.Zhao X, Grewal A, Briel M, Lee JM. A systematic review of nonabsorbable, absorbable and steroid-impregnated spacer following endoscopic sinus surgery. Int Forum Allergy Rhinol. 2013;3(11):896–904. doi: 10.1002/alr.21201. [DOI] [PubMed] [Google Scholar]
- 21.Friedman M, Schalch P. Middle turbinate medialization with Bovine serum albumin tissue adhesive (Bioglue) Laryngoscope. 2008;118(2):335–338. doi: 10.1097/MLG.0b013e318158198f. [DOI] [PubMed] [Google Scholar]
- 22.Friedman M, Tanyeri H, Landsberg R, David C (1999) Effects of middle turbinate medialization on olfaction. Laryngoscope 109:1442–1445 [DOI] [PubMed]
- 23.Chen W, Wang Y, Bi Y, Chen W (2015) Turbinate-septal suture for middle turbinate medialization: a prospective randomized trial. Laryngoscope 125(1): 33–35 [DOI] [PubMed]
- 24.Thornton RS. Middle turbinate stabilization technique in endoscopic sinus surgery. Arch Otolaryngol Head Neck Surg. 1996;122:869–872. doi: 10.1001/archotol.1996.01890200059013. [DOI] [PubMed] [Google Scholar]
- 25.Lee MR, Marple BF. Middle turbinate medialization for improved access during endoscopic sinus surgery. Int Forum Allergy Rhinol. 2011;1:187–190. doi: 10.1002/alr.20013. [DOI] [PubMed] [Google Scholar]


