Abstract
To study the long term outcome of endoscopic septoplasty with microdebrider assisted inferior turbinoplasty (MAIT) versus medial flap turbinoplasty (MFT). The present study was conducted in the Department of ENT, Government Medical College, Amritsar. Patients with symptomatic persistent nasal obstruction were recruited from ENT outdoor clinics. The nasal obstruction was persistent despite medical therapy that included a minimum 4 weeks. The study was primarily a double blinded prospective randomized control study including 120 patients, where all patients enrolled at odd numbers were taken for endoscopic septoplasty with microdebrider assisted inferior turbinoplasty and all patients with even numbers were taken for endoscopic septoplasty with MFT. Patient-scored nasal obstruction (1–5) along with blindly assessed nasal airway patency ratings (1–4) was done at 3 and 24 months postoperatively. A total of 120 patients were recruited in the study. The mean ages of the MAIT and MFT groups were 28.61 ± 14.8 and 30.25 ± 8.36 years, respectively. Average follow-up period was 21.9 ± 6.3 months. Nasal obstruction was improved in both techniques at 3 months, but after long term follow up, it was highly significant for MFT along with improvement in preoperative symptoms p < 0.001. No patients complained of worsening of their obstruction. Nasal patency at 24 months, a significant proportion of patients had a greater nasal assessment by a blind assessor with 97.1% in MFT and 81.9% MAIT with mild to no obstruction. In MAIT group 16.6% had pain/discomfort, 23.6% had discharge which were the major complications, but crusting (MAIT 10% and MFT 3.3%), adhesions (MAIT 13.8% and MFT 1.6%). The medial flap inferior turbinoplasty (MFT) is technically straight forward procedure that provides long term more effective and satisfactory the patient in relieving nasal obstruction, without significant risk of complications. The long term follow up of MAIT is required as there was increase in need of decongestion and they might require second procedure as MFT.
Keywords: Endoscopic septoplasty, Microdebrider assisted inferior turbinoplasty (MAIT), Medial flap turbinoplasty (MFT), Nasal obstruction
Introduction
Chronic nasal obstruction is a widespread symptom of 9.5–15% general population [1]. Patients complaining of nasal obstruction with unilateral septal deviation have varying degrees of associated inferior turbinate hypertrophy (ITH) on the opposite side [2]. This compensatory mechanism due to an increase in erectile tissue with extension of venous sinusoids in the mucosa to protect the more patent nasal side from the excessive airflow [3]. In recent studies the conchal bone exerts bigger effect on ITH than the medial and lateral mucosa which causes mechanical bilateral nasal obstruction and mucocilliary dysfunction of nasal cavity [3, 4].
Recent radiological and histopathological studies have indicated that conchal bone hypertrophy is mainly responsible for ITH and that mucosal hypertrophy is less important [3, 4]. Septoplasty was started in nineteenth century and has been modified to provide maximum functional and respiratory improvement at the same time preserving other physiological functions of nose. Since the first surgical treatment of hypertrophied inferior turbinate in 1895, many techniques have been described and considerable debate continues as to the most effective method [5, 6].
There are number of procedures for turbinate reduction as follows; (a) non resection procedures—chemical cauterization of turbinate, intraturbinal injections, out fracturing of turbinate, cryotherapy, surface and submucosal electrocautery, LASER, assisted turbinoplasty, radiofrequency ablation, (b) resection procedures—partial inferior turbinectomy, subtotal inferior turbinectomy, submucous resection of turbinate, powered inferior turbinoplasty [7, 8].
Recently powered instruments like microdebrider and shavers have come into use of turbinate surgery. These instruments are used on turbinate surface as well as intraturbinally, often under the guidance of an endoscope. Our aim was to study the long term outcome of endoscopic septoplasty with microdebrider assisted inferior turbinoplasty (MAIT) versus medial flap turbinoplasty (MFT).”
Materials and Methods
The present study was conducted in the department of ENT, Government Medical College, Amritsar. Patients with symptomatic persistent nasal obstruction were recruited from ENT outdoor clinics from March 2018–2020. The nasal obstruction was persistent despite medical therapy that included a minimum 4 week trial of intranasal corticosteroids. The study was primarily a double blinded prospective randomized control study including 120 patients, where all patients enrolled at odd numbers were taken for endoscopic septoplasty with inferior turbinoplasty and all patients with even numbers were taken for endoscopic septoplasty with medial flap turbinoplasty. The approval from the Institutional Ethics Committee, GMC Amritsar was obtained and patients were enrolled in the study after obtaining written informed consent.
Inclusion criteria:
Age: 18–65 years of age of both the sexes
Patients with deviated nasal septum (DNS) with contralateral ITH
Exclusion criteria:
Patients with DNS having other obstructive pathologies like granulomatous diseases, neoplasm and hypertrophic adenoids
Patients with co-morbidities (e.g.: Diabetes Mellitus, cardiovascular diseases, sleep apnea)
Previous history of turbinate reduction surgeries
Patients with traumatic septal deformity
Nasal polyposis and other nasal mucosal diseases
Patients with history of allergy
After selection a complete history was obtained from each patient along with general physical and systematic examination, examination of ear, nose and throat examination including nasal endoscopy. We performed a computed tomography (CT) of nose and paranasal sinuses to assess the correlation between a deviated nasal septum and compensatory hypertrophy of inferior turbinate.
Relevant routine pre-operative investigations were done. All cases were subjected to routine pre anaesthetic check up and requisite clearance was obtained.
Nasal obstruction was measured using a subjective symptom score. Patients scored on a 5-point ordinal scale (worse than preoperative, no change from preoperative, improved but requiring regular decongestants, improved but occasional need for decongestants, improved and no need for decongestants).
Assessment of each nasal airway was made by anterior rhinoscopy and endoscopy and was carried out by a second blinded clinician. A 4-point ordinal scale of severe obstruction, moderate obstruction, mild obstruction, or no obstruction was given. This was based on the ability to visualize the nasopharynx without decongestion, the posterior aspect of the turbinate, middle portion of the turbinate, or only the anterior head. Outcomes were assessed postoperatively at 3 and 24 months.
Techniques
The anaesthesia preferred can either be local or general anaesthesia. In local anesthesia, the local anaesthetic preferred was 2% lignocaine with 1:100,000 adrenaline solution. Approximately 5–7 ml was injected into the submucoperichondrial layer of the nasal septum and the submucosa of both inferior turbinates each. In general anaesthesia 1:100,000 adrenaline solution was used for injection to reduce intraoperative blood loss. Endoscopic septoplasty was done first in all patients using routine method.
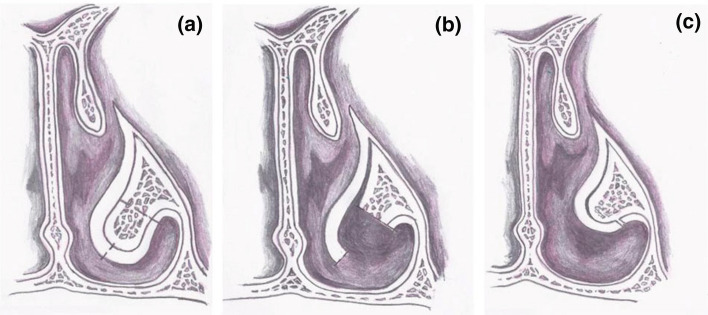
For the procedure of turbinoplasty (MAIT) a 5 mm vertical incision was made on the anterior end of the hypertrophied inferior turbinate on the roomier side of the nasal cavity. A turbinoplasty blade size 2.9 was attached to a microdebrider and it was inserted through the incision. The submucosal soft tissue was debrided along the inferior turbinate bone and outfractured then displace laterally to the residual turbiante. The submucosal microdebrider assisted turbinoplasty was done on the side of inferior turbinate hypertrophy (Fig. 1).
Fig. 1.
After vertical incision on anterior end of the inferior turbinate, submucosal pocket was made up to the posterior end of turbinate and soft tissue was removed with microdebrider and outfractured and displace laterally the residual turbinate
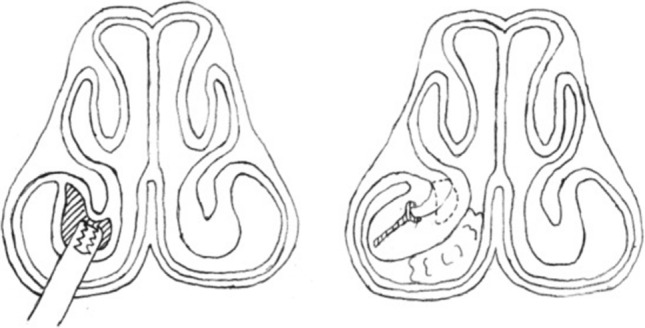
The medial flap turbinoplasty (MFT) procedure commences with the creation of a window to the inferior meatus, at the anterior inferior turbinate in the axilla between the inferior turbinate medially and the pyriform aperture laterally. The posterior soft tissue tail is removed with the microdebrider, and a medial flap is created by removal of the inferior border. The remaining mucosal flap is elevated in a subperiosteal plane using Cottle dissector. The turbinate bone and lateral mucosa are then removed along the vertex of the inferior meatus. The arterial supply, the medial and lateral branches of the inferior turbinate artery, is then identified and cautery is applied using a bayonet bipolar forceps. Attention is then directed at sculpting the anterior head, undermining the soft tissue with microdebrider or ensuring bone removal is flush to the pyriform sinus. The medial flap is then rotated laterally onto itself and surgicel dressing is placed to support the flap (Fig. 2). Nose was then packed with merocel or medicated gauze. During his/her hospital stay for 2 days, the patient was put on injectable antibiotics, oral anti histamines and analgesics. The pack removal was done after 48 h. Nasal irrigation commences on postoperative day 3, and the patient follows up between 7 and 10 days postoperatively for removal of any postoperative crusts. The patients were then followed up at 3 and 24 months.
Fig. 2.
Diagram of the right nose, coronal plane, showing the three consecutive surgical steps: a incision (dotted line); b medial and lateral mucosal flaps creation and turbinate bone and lateral mucosal flap removed; and c medial mucosal flap repositioning over the turbinate stump
Statistical analysis was performed using SPSS software Kendall’s tau-B was used for ordinal values. Chi squared analysis was used for relationships of nominal variables. Student t test (2-tailed) used for comparisons of parametric data. Results were deemed significant with a p value of < 0.05.
Results
A total of 120 patients were recruited in the study. The mean ages of the MAIT and MFT groups were 28.61 ± 14.8 and 30.25 ± 8.36 years, respectively. Average follow-up period was 21.9 ± 6.3 months ranging from 18 to 24 months. Males made up 71 and 59.15% and females 49 and 40.83%, respectively. Out of 120 patients 67 (55.83%) had right sided and 53 (44.1%) left sided inferior turbinate hypertrophy. There was no patient who dropped out from the study until at least 24 months after operation (Table 1).
Table 1.
Age and gender distribution
| Age groups (in years) | Sex | |
|---|---|---|
| Male | Female | |
| < 20 years | 12 (10.0%) | 7 (5.83%) |
| 21–40 years | 38 (31.66) | 29 (24.17%) |
| 41–60 years | 16 (13.33) | 11 (9.16%) |
| 61 and above | 5 (4.16%) | 2 (1.67%) |
| Total | 71 (59.15%) | 49 (40.83%) |
In our study both groups were post surgery, few patients faced problems like nasal bleeding (MAIT 11.6% and MFT 5%), crusting (MAIT 10% and MFT 3.3%), adhesions (MAIT 13.8% and MFT 1.6%) which were managed appropriately by nasal douching, nasal bleeding managed by nasal packing with nasal decongestants and Botropase (a hemocoagulase preparation used to arrest bleeding of different etiology) soaked cottonoids, synechiae formation which was released and nasal pack kept for half a day between two raw surfaces and then removed later, following which nasal douching were advised. In MAIT group 16.6% had pain/discomfort, 23.6% had discharge which were the major complications in short term and failure of procedure reported in 9.7% (Table 2).
Table 2.
Short and long term complications of surgery
| Short term (< 3 months) | MAIT | MFT | Long term (24 months) | MAIT | MFT |
|---|---|---|---|---|---|
| Bleeding (requiring review) | 7 (11.6%) | 3 (5%) | Atrophic rhinitis | – | – |
| Pain/discomfort (additional analgesia) | 10 (16.6%) | 4(6.7%) | Adhesions | 8 (13.8%) | 1 (1.6%) |
| Crusting (requiring additional debridement) | 6 (10%) | 2 (3.3%) | Anosmia | 3 (5%) | 1 (1.6%) |
| Malodor/discharge | 14 (23.6%) | 3 (5%) | Ephiphora | 1 (1.6%) | 2 (3.3%) |
| Increased hospital stay (> 1 day) | 4 (6.7%) | 1 (1.6%) | Failure of procedure | 5 (9.7%) | 0 |
At 3 months outcome of nasal obstruction with MAIT as: worse than preoperatively (0%), no change (8.5%), improved with regular decongestants (31.7%), improved with occasional decongestants (43.4%) and improved 16.7%. However, in MFT nasal obstruction no one was worse than preoperatively and no change (0%), improved with regular decongestants (18.3%), improved with occasional decongestants (35%) and improved 46.7%.
Nasal patency after 3 months as no obstruction (MAIT 46.7% and MFT 60%), mild (MAIT 33.3% and MFT 25%), 9% moderate in both MAIT and MFT and only 5% in MAIT with sever nasal obstruction. There was significant difference in relieving nasal obstruction and patency after reducing the inferior turbinates size between both techniques after 3 months p < 0.001 (Table 3).
Table 3.
Three-month status by patient reported outcome and blind assessor
| Nasal obstruction (3 months) | MAIT | MFT | p < 0.001 |
|---|---|---|---|
| Worse than preoperatively | 0 | 0 | |
| No change | 5 (8.5%) | 0 | |
| Improved (regular decongestants) | 19 (31.7%) | 11 (18.3%) | |
| Improved (occassional decongestants) | 26 (43.4%) | 21 (35.0%) | |
| Improved (no decongstants) | 10 (16.7%) | 28 (46.6%) | |
| Nasal patency (3 months) | < 0.001 | ||
| Severe obstruction | 3 (5.0%) | 0 | |
| Moderate obstruction | 9 (15%) | 9 (15%) | |
| Mild obstruction | 20 (33.3%) | 15 (25%) | |
| No obstruction | 28 (46.7%) | 36 (60.0%) |
In long term outcome of nasal obstruction in MFT highly significant 93.3% improved (without/occasional decongestants), 6.6.7% improved with regular decongestants but, in MAIT majority of dependent on decongestants as 78.5% patients and nearly 10% improved without decongestants and same number of patients had no change (Table 4).
Table 4.
Long term outcome of nasal obstruction at 24th month
| Nasal obstruction | MAIT | MFT | p < 0.001 |
|---|---|---|---|
| Worse than preoperatively | 0.0 | 0.0 | |
| No change | 11.7% | 0.0 | |
| Improved (regular decongestants) | 41.8% | 6.67 | |
| Improved (occasional decongestants) | 36.7% | 40.0% | |
| Improved (no decongestants) | 9.8% | 53.3% |
Nasal patency at 24 months, a significant proportion of patients had a greater nasal assessment by a blind assessor with 97.1% in MFT and 81.9% MAIT with mild to no obstruction. 18.1% in MAIT has moderate to server nasal obstruction (Table 5).
Table 5.
Long term outcome of nasal patency at 24th month
| Nasal patency | MAIT (%) | MFT | p < 0.001 |
|---|---|---|---|
| Severe obstruction | 9.7 | 0.0 | |
| Moderate obstruction | 8.4 | 3.33% | |
| Mild obstruction | 51.4 | 29.7% | |
| No obstruction | 30.5 | 67.4% |
In 3 months after the surgery, there was statistically significant reduction of nasal obstruction in either group. However this reduction was statistically highly significant with a p value of < 0.001 at 24 months with MFT.
Discussion
The ideal turbinate reduction along with septoplasty removes the obstructed portions of the turbinate and septum while preserving the medial physiologic mucosa, thus maintaining the sensory functions and humidification of inspired air while decreasing complications like increase the risk of dryness throat, nasal crusting, nasal bleeding, and extremely patent nasal cavities [9].
Such complications were not found to be significantly associated with described techniques, particularly those mucosal preserving techniques, submucoal and turbinoplasty, similar to additional reports in the literature. Several studies have examined the effectiveness of turbinate surgery in combination with septoplasty [2, 4, 10]. The microdebrider, initially used since the 1990s in endoscopic rhinosinusal surgery, was introduced into turbinate surgery as a submucosal corridor with the advantage of not altering the function of the nasal mucosa [11–13].
Recently, power instruments like “microdebriders” and “shavers” have come into use in turbinate surgery [14]. These instruments are used on the turbinate surface as well as intraturbinally, often in combination with an endoscope. Many surgeons resect parts from the lateral and inferior borders of the turbinate, while others use the microdebrider intraturbinally [2, 15].
In our study, the septoplasty were performed along with reduction of inferior turbinate and relief of nasal obstruction was best achieved with the endoscopic medial flap inferior turbinoplasty (MFT). This technique was associated with low rates of nasal crusting and troublesome primary hemorrhage (Table 2). Puterman et al. [14] showed minimised post-operative side effects and complications such as dryness, infection, bleeding and pain. Barham et al. [15] reported no post-operative complications. Cingi et al. [16] concluded that no crusting was observed post-operatively.
It seems like that the positive effects of turbinate reduction in MAIT and MFT on the nasal airway, appear equally good. However, with MFT nasal breathing begins to improve starting from the first week after the operation. Symptoms of nasal obstruction and congestion regressed significantly on the first evaluations and thereafter stabilized until the 90th postoperative day. In addition, Cingi et al. [16] and Gupta et al. [17] showed the effectiveness of this technique for the recovery of respiration and they noted significant improvement in nasal obstruction at the first post-operative week.
In contrast, release of nasal obstruction by MAIT technique although initially good was not maintained long term; however at 24 months postoperatively there was increased need of 78.5% for decongestant therapy to sustain subjective patient improvement in nasal obstruction; whereas in MFT highly significant 93.3% improved nasal obstruction (without/occasional decongestants). (p < 0.001) Our results show that resection of turbinate bone, preservation of nasal mucosa, and a controlled volume reduction contributes to a more robust long-term outcome in MFT (Table 4).
Nasal Patency at 24 months, a significant proportion of patients had a greater nasal assessment by a blind assessor with 97.1% in MFT p < 0.001, while MAIT 51.4% mild obstruction, 18.1% moderate to server nasal obstruction and 30.5% showed no obstruction (Table 5).
Our findings of MAIT are consistent with the other studies. Wight et al. [18] showed anterior trimming of the inferior turbinate, whilst being an objective success in decreasing nasal resistance, frequently failed to produce a significant fall in subjective obstruction in the first 2 months. Cingi et al. [16] found significant improvement in nasal obstruction in patients treated with MAIT at the first and third post-operative month. Lee and Chen [19] reported that MAIT is a minimally invasive technique, safe and effective for the treatment of hypertrophy of the inferior turbinates. Chen et al. [20] who compared endoscopic submucosal tissue resection with resection with microdebrider. They found no significant differences between improvements in nasal obstruction at 1 year, which continued to be the case 3 years later. Neri et al. [21] confirmed that by respecting nasal turbinate mucosa during MAIT surgery it is possible to achieve a long-term resolution of nasal obstruction but with use of regular decongestants.
Our present study was correlated with Wormald et al. [22] there was significant improvement in nasal obstruction in the immediate (first 3 weeks) post-operatively in 19 patients treated by MFT.
Kassab et al. [23] they carried out their study on 20 patients with bilateral nasal obstruction due to ITH, they reported that the total success rate was 90% post-operatively and concluded that microdebrider turbinoplasty is superior to conventional submucosal resection with regard to preserving the nasal mucosa. Puterman et al. [14] endoscopic, assisted, modified turbinoplasty with mucosal flap technique can reduce a large volume of the turbinate while preserving the mucosal continuity and the submucosa by covering the raw surface with a mucosal flap. Barham et al. [15] studied a total of 100 patients were recruited (age 32.79 ± 13.58 years; 39% female). This represented 200 nasal airway surgeries with 100 submucosal procedures, 50 electrocautery and 50 medial flap turbinoplasties. No patients complained of worsening of their obstruction. At 60 months patients in the turbinoplasty group had greater outcomes, with 90.2% having occasional or no decongestant use compared to electrocautery (15.8%) and submucosal (37.8%).
MAIT has benefit to preserve the entire turbinal mucosa, except for a notch in the anterior pole of the turbinate. Keeping its functional structures intact, the turbinate can remain fully normal after the procedure; however a more rebound effect on tissue was observed in long-term outcome.
The principal merit of the Medial flap technique is its excellent visualization during the entire procedure. This allows precise elevation of the both mucosal flaps without unguarded tearing, resection of turbinate bone even at the most posterior end of the inferior turbinate. There is significant improvement in nasal patency with controlled volume reduction contributes to which lasts for a long time. It provides excellent outcomes in a wide variety of patients with minimal complications.
Limitations
One of the major limitations to this study was exact recording of any additional maintenance therapy used by patients. Included patients were not restricted to avoidance of medical management during the follow up period and only data regarding the use of decongestive therapy was recorded.
Summary
To our knowledge, this is the first study that compares the MAIT technique to MFT with a very large sample of 120 patients and long term follow-up. Given the results obtained, that both techniques are very effective in reducing nasal obstruction while respecting the nasal mucosa and thus the function of the turbinate. The long term follow up of MAIT is required as there was increase in need of decongestion and they might require second procedure as MFT.
Conclusion
The medial flap inferior turbinoplasty is technically straight forward procedure that provides long term more effective and satisfactory the patient in relieving nasal obstruction, without significant risk of complications. The removal of both the lateral mucosa and bone as well as a organize reduction of the medial mucosa is less likely to lead to re-expansion of the turbinate with the passage of time compared to submucosal microdebrider technique.
Funding
No.
Compliance with Ethical Standards
Conflict of interest
No.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kulwinder Singh Sandhu, Email: kssandhu3735@gmail.com.
Satinder Pal Singh, Email: satinderpalsingh44@gmail.com.
Oshin Thomas, Email: oshinthomas1992.ot@gmail.com.
Priyanka Choudhary, Email: dr.priyanka1607@gmail.com.
Arvinder Singh, Email: mannarvinder@yahoo.com.
Manjit Singh, Email: drmanjitsingh62@yahoo.com.
References
- 1.Åkerlund A, Millqvist E, Öberg D, Bende M. Prevalence of upper and lower airway symptoms: the Skövde population-based study. Acta Otolaryngol. 2006;126(5):483–488. doi: 10.1080/00016480500416835. [DOI] [PubMed] [Google Scholar]
- 2.Illum P. Septoplasty and compensatory inferior turbinate hypertrophy: long-term results after randomized turbinoplasty. Eur Arch Otorhinolaryngol. 1997;254(1):S89–S92. doi: 10.1007/BF02439733. [DOI] [PubMed] [Google Scholar]
- 3.Berger G, Hammel I, Berger R, Avraham S, Ophir D. Histopathology of the inferior turbinate with compensatory hypertrophy in patients with deviated nasal septum. The Laryngoscope. 2000;110(12):2100–2105. doi: 10.1097/00005537-200012000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Rohrich RJ, Krueger JK, Adams JW, Marple BF. Rationale for submucous resection of hypertrophied inferior turbinates in rhinoplasty: an evolution. Plast Reconstr Surg. 2001;108(2):536–544. doi: 10.1097/00006534-200108000-00041. [DOI] [PubMed] [Google Scholar]
- 5.Larrabee YC, Kacker A. Which inferior turbinate reduction technique best decreases nasal obstruction? The Laryngoscope. 2014;124(4):814–815. doi: 10.1002/lary.24182. [DOI] [PubMed] [Google Scholar]
- 6.Passàli D, Passàli FM, Passàli GC, Damiani V, Bellussi L. Treatment of inferior turbinate hypertrophy: a randomized clinical trial. Ann Otol Rhinol Laryngol. 2003;112(8):683–688. doi: 10.1177/000348940311200806. [DOI] [PubMed] [Google Scholar]
- 7.Huizing EH, De Groot JA. Functional reconstructive nasal surgery, 943 illustrations & 23 tables. New York: Thieme; 2003. [Google Scholar]
- 8.Bergmark RW, Gray ST. Surgical management of turbinate hypertrophy. Otolaryngol Clin N Am. 2018;51(5):919–928. doi: 10.1016/j.otc.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Ikeda K, Oshima T, Suzuki M, Suzuki H, Shimomura A. Functional inferior turbinosurgery (FITS) for the treatment of resistant chronic rhinitis. Acta Otolaryngol. 2006;126(7):739–745. doi: 10.1080/00016480500472853. [DOI] [PubMed] [Google Scholar]
- 10.Van Delden MR, Cook PR, Davis WE. Endoscopic partial inferior turbinoplasty. Otolaryngol Head Neck Surg. 1999;121(4):406–409. doi: 10.1016/S0194-5998(99)70229-9. [DOI] [PubMed] [Google Scholar]
- 11.Al-Reefy H, Hopkins C. Endoscopic assisted modified turbinoplasty with mucosal flap. J Laryngol Otol. 2013;127(7):728. doi: 10.1017/S0022215113000728. [DOI] [PubMed] [Google Scholar]
- 12.Nunez DA, Bradley PJ. A randomised clinical trial of turbinectomy for compensatory turbinate hypertrophy in patients with anterior septal deviations. Clin Otolaryngol Allied Sci. 2000;25(6):495–498. doi: 10.1046/j.1365-2273.2000.00362.x. [DOI] [PubMed] [Google Scholar]
- 13.Yáñez C. New technique for turbinate reduction in chronic hypertrophic rhinitis: intraturbinate stroma removal using the microdebrider. Oper Tech Otolaryngol Head Neck Surg. 1998;9(3):135–137. doi: 10.1016/S1043-1810(98)80017-1. [DOI] [Google Scholar]
- 14.Puterman M, Segal N, Joshua B. Endoscopic, assisted, modified turbinoplasty with mucosal flap. J Laryngol Otol. 2012;126(5):525–528. doi: 10.1017/S0022215112000163. [DOI] [PubMed] [Google Scholar]
- 15.Barham HP, Thornton MA, Knisley A, Marcells GN, Harvey RJ, Sacks R. Long-term outcomes in medial flap inferior turbinoplasty are superior to submucosal electrocautery and submucosal powered turbinate reduction. Int Forum Allergy Rhinol. 2016;6:143–147. doi: 10.1002/alr.21574. [DOI] [PubMed] [Google Scholar]
- 16.Cingi C, Ure B, Cakli H, Ozudogru E. Microdebrider-assisted versus radiofrequency-assisted inferior turbinoplasty: a prospective study with objective and subjective outcome measures. Acta Otorhinolaryngol Ital. 2010;30(3):138. [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta A, Mercurio E, Bielamowicz S. Endoscopic inferior turbinate reduction: an outcomes analysis. The Laryngoscope. 2001;111(11):1957–1959. doi: 10.1097/00005537-200111000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Davis WE, Nishioka GJ. Endoscopic partial inferior turbinectomy using a power microcutting instrument. J ENT. 1996;75:49–50. [PubMed] [Google Scholar]
- 19.Lee CF, Chen TA. Power microdebrider-assisted modification of endoscopic inferior turbinoplasty: a preliminary report. Chang Gung Med J. 2004;27(5):359–365. [PubMed] [Google Scholar]
- 20.Chen YL, Tan CT, Huang HM. Long-term efficacy of microdebrider-assisted inferior turbinoplasty with lateralization for hypertrophic inferior turbinates in patients with perennial allergic rhinitis. Laryngoscope. 2018;118(7):1270–1274. doi: 10.1097/MLG.0b013e31816d728e. [DOI] [PubMed] [Google Scholar]
- 21.Neri G, Mastronardi V, Traini T, D’Orazio F, Pugliese M, Cazzato F. Respecting nasal mucosa during turbinate surgery: end of the dogma? Rhinology. 2013;51(4):368–375. doi: 10.4193/Rhino12.124. [DOI] [PubMed] [Google Scholar]
- 22.Wormald PJ. Chapter 4. Powered inferior turbinoplasty and endoscopic septoplasty. In: Al-Helo S, Falih H, Jumma A, editors. Endoscopic sinus surgery: anatomy, three-dimensional reconstruction, and surgical technique. 3. New York: Thieme; 2013. pp. 19–27. [Google Scholar]
- 23.Kassab NA, Rifaat M, Madian Y. Comparative study of management of inferior turbinate hypertrophy using turbinoplasty assisted by microdebrider or 980 nm diode laser. J Laryngol Otol. 2012;126:1231–1237. doi: 10.1017/S0022215112002320. [DOI] [PubMed] [Google Scholar]