Abstract
Abstract
Although frequently used head and neck reconstruction methods are perforator flaps and free flaps, supraclavicular artery (SCA) flaps are newly used in skin defect reconstructions. In this study, we shared the experience of the SCA flap to evaluate whether there is a strong option in the head and neck. This prospective clinical cohort study of 28 patients, including 11 men, 12 women, and 5 children was performed between 2016 and 2020 years in the patients who were planned with SCA flap for burns, tracheostomy, or after malignant skin tumor of head and neck region. Seventeen of our patients were burnt, 8 malignant skin tumors, and 3 were used to repair the wound that did not heal after tracheostomy. In one patient, the tissues could not be closed primarily because the skin lost its elasticity due to a burn in the surrounding tissues. No flap necrosis dehisens or any other complications were seen and our patients were discharged with complete recovery. While only two patients stated moderate satisfaction orally, the other patients liked the result very much. On the other side, all the patients declared no loss of functionality following this SCA flap surgery. The SCA proved itself as a strong reconstructive flap for the head and neck, and has consistently demonstrated a reliable flap to provide a perfect color match.
Level of Evidence
II, Randomized clinical cohort study.
Keywords: Head, Neck, Burn, Tracheostomy, Supraclavicular artery flap, Reconstruction
Introduction
Plastic reconstruction is one of the most important parts of burns and cancer surgery of the head and neck field [1, 2]. The comfort provided by a sufficient and appropriate reconstruction for the surgeon is also reflected in oncological resection [3, 4]. Knowing the existence of sufficient resection helps the surgeon to be much freedom of surgical resection [5]. The defects in the head and neck region are not only different in size and content, but also in terms of functional and aesthetic problems they cause [6]. Naturally, reconstructions of these kind defects are also very diverse. The basic principle in head and neck reconstruction is to determine and apply the most suitable reconstruction method among the tens of options in the current defect [7, 8].
The purpose of this reconstruction is not only the closure of the defect but also a result that can allow functional and cosmetic rehabilitation with the skin and color similar to the recipient area [9]. The fact that the donor area is anatomically close to the recipient will increase the likelihood that the skin will offer a comparable aesthetic quality [7]. In this sense, the use of shoulder skin as a flap close to the skin of the face and neck allows the construction of a functional anatomical unit equivalent to the original skin.
The supraclavicular artery (SCA) flap has recently come to the fore for plastic surgeons although the best flaps in head and neck oncology are discussed in these patients [10]. It is a fascio-cutaneous flap based on the SCA, which is a branch of the transverse cervical artery [11]. Nonetheless, it arises from arteria suprascapularis less frequently, which is not a large vessel [12]. Its drainage is accompanied by the transverse cervical vein that can be determined at its upper extent [13]. External jugular vein draining the distal portion of the SCA flap needs to be carefully preserved during the surgery [14]. If it is planned with a careful surgical approach and applied properly to the head/neck oncological patients, this flap, which is highly likely to be very satisfying, will be increasingly preferred with its reconstructive and esthetical outcomes.
Few studies in the literature have been reported the strong outcomes of SCA flap in head and neck reconstructions. In this study, we shared the experience with respect to the utility of the SCA flap to evaluate whether there is a useful and reliable flap option in the head and neck region that was planned for patients after burns, tracheostomy, or after malignant skin tumor.
Materials and Methods
Study Design
This prospective clinical cohort study of 28 patients, including 11 men, 12 women, and 5 children was performed between 2016–2020 years after obtaining the informed consent from all the patients who were planned with SCA flap for burns, tracheostomy or after malignant skin tumor of head and neck region. The skin flap is designed to fit the resulting defect and is based on the trans clavicular vascular pedicle in all cases, and almost all donor sites can be closed after first being damaged. All reconstructions were performed through the head and neck defects following radical radiotherapy or untreated malignant tumors.
Flap Technique and Surgery
All the procedure was performed under general anesthesia with endotracheal intubation. The flap method we applied was as follows: primarily the draft of the flap was located center line in the foreground with the size of the defect designed laterally to the anterior border of the musculus trapezius. Then, the length of the pedicle, which identified the transposition arc, was calculated from the current point. All patients were informed about the possibility of stretching the scar for the postoperative period and a visible scar in the donor regions.
The flap boundary line is marked as 2 cm anterior to the scapular spine and a line parallel to the posterior line in front of the clavicle, while the lateral edge can be extended 2 cm lateral to the deltopectoral groove. We paid special attention not to lift the pedicle from the base of the posterior triangle with oily adipose tissues. The flap rises from distal to proximal in the subfacial plane, thereby preventing pedicle damage. The flap is raised at the subfacial level, which is superficial for deltoideus by sharp blade dissection. The natural length of the subcutaneous pedicle is directly related to the distance to the lateral third of the clavicle, where the medial edge of the trapezius muscle is inserted, starting from the medial edge of the place of the defect. We observed for distal tip bleeding to ensure and evaluate intraoperative flap viability of raised flaps. The area where the pedicle should be buried under the skin flaps has been deepened by fully protecting its subcutaneous fat on the superficial direction of the flap. The rotation directive can be expanded by carefully excising the subcutaneous adipose tissue between the epithelial component of the flap and the edge of the trapezus muscle.
We performed the primary closure of the donor area after the chest and subcutaneous area on the scapula, both front and back respectively. It is performed if there is a hard condition in bringing the flaps closer upon the acromion closure with split skin grafting. We observed all the patients for postoperative hematoma, complications in the intensive, and flap viability.
Results
In this study of 28 patients, including 11 men, 12 women, and 5 children, the youngest patient we operated was 3 years old, while the oldest patient was 66 years old with tracheostomy sequela. Seventeen of our patients were burnt, 8 malignant skin tumors, and 3 were used to repair the wound that did not heal after tracheostomy. All the patients’ details with diameters and demographics were given in Table 1.
Table 1.
Defect size/outcomes of all the patient we operated for reconstruction
| Defect (n: 28) | No | Age | Defect (cm) | Complication | Management |
|---|---|---|---|---|---|
| Tracheostomy defect | 3 | 39 | 5 × 4 | None | N/A |
| Malignant skin Tumor surgery | 8 | 52 | 7 × 5 | None | N/A |
| Unilateral burn contracture | 9 | 18 | 8 × 7 | Secondary surgery (7) | Full-thickness skin graft |
| Bilateral burn contracture | 8 | 20 | 14 × 8 | Secondary surgery [6] | Full-thickness skin graft |
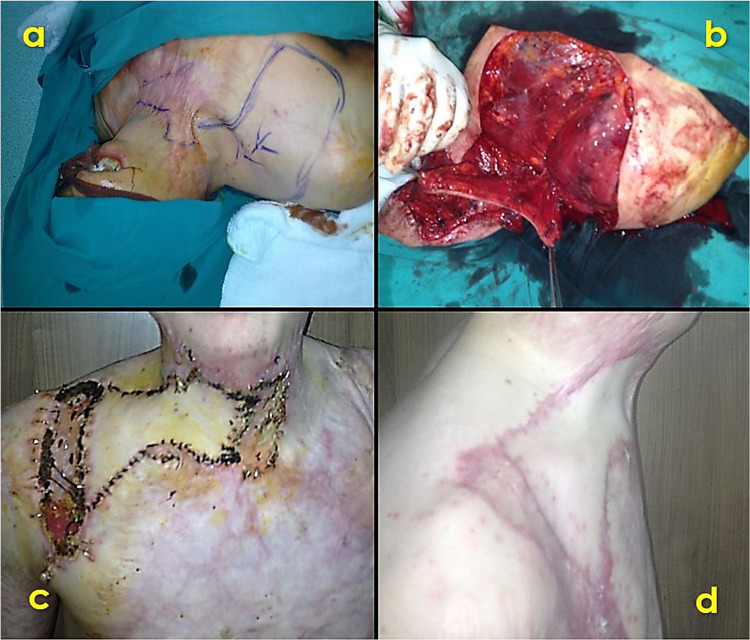
Donor sites were primarily closed in all patients except one. In one patient, the tissues could not be closed primarily because the skin lost its elasticity due to a burn in the surrounding tissues. Partial-thickness grafts were taken from the right thigh area of the patient and the donor site closure was completed. No flap necrosis dehisens or any other complications were seen and our patients were discharged with complete recovery (Fig. 1).
Fig. 1.
Unilateral reconstruction of the burn contracture; a preop. design, b operative preparation, c postop. condition, d postop. long-term follow-up
Patient satisfaction and external views in the head and neck region showed very high satisfaction at a 1-month follow-up and long follow-up. While only two patients stated moderate satisfaction orally, the other patients liked the result very much. On the other side, all the patients declared no loss of functionality following this SCA flap surgery.
Discussion
We evaluated it as a useful and reliable flap option in the neck region for flap cases planned for tissue loss after burns, tracheostomy, and malignant skin tumors in patients. This flap donor site is a method that can be used safely in tissue loss in the region due to its low morbidity, adequate tissue transfers to the desired area, and a safe method. According to the literature, our method is a very new and bright future method since it is tried by a few surgeons in the world (Fig. 2).
Fig. 2.
Bilateral defect reconstruction of the patient with burn contracture; a preop. design, b operative preparation, c postop. condition, d postop. long-term follow-up
As we have experienced, SCA flap, which has a strong use in the head and neck region reliably and quickly and resembles a free flap with aesthetic and functional results, has a strong reconstruction profile. Besides the lower rate of complications using this flap, it is a good result choice for head and neck reconstruction in some hospital environments with insufficient resources and facilities. Hence, the SCA flap has recently come to the fore for plastic surgeons although the best flaps in head and neck oncology are innovatively discussed [10]. It has been used innovatively for different kinds of plastic and reconstructive approaches [15]. Chean et al. reported 24 patients who took the SCA flap to the reconstruct post-oncologic resection defects of the head and neck, which had a similar number of in 24 patients [16]. Epps et al. reported that they applied the SCA flap to defect reconstruction following parotidectomy, with satisfied outcomes, [17], while Chiu et al. used in the post-resection oropharyngeal defect reconstruction [18]. Hetland et al. tried the SCA flap for the surgical revision of the Noma disease that required a second surgical reconstruction. 6 of their cases were children as well as being our patients [19]. In our study, 28 patients, including 11 men, 12 women, and 5 children, underwent the SCA flap. The indifference with the other studies, there were not only malignancy patients but also seventeen of them were burnt.
Contrary to successful results, some negative results are included in the literature [16, 19–22]. First, Lamberty reported the use of the SCA in two patients following thirteen cadaveric dissections that one of the two flaps generated a minor complication [20]. A similar number to our study, Palua et al. shared successful results with 28 flaps, including one free flap; they observed one flap necrosis and two cases of infections in donor sites [21]. In a study by Vinh et al. most of the cases they operated had no complications [22]. Four showed distal tip necrosis, with two failures. In our series, donor sites were primarily closed in all patients except one. In one patient, the tissues could not be closed primarily because the skin lost its elasticity due to a burn in the surrounding tissues. Partial-thickness grafts were taken from the right thigh area of the patient and the donor site closure was completed. No flap necrosis dehisens or any other complications were seen and our patients were discharged with complete recovery.
In the present study, we only get subcutaneous soft tissues and fascia; and thus, since the muscle and deep tissues are not removed, the donor area provides superiority over other large flaps or free flaps since it is possible to repair large tissue defects with this method by reducing the risk of morbidity in the field. Patient satisfaction and external views in the head and neck region showed very high satisfaction at a 1-month follow-up and long follow-up. While only two patients stated moderate satisfaction orally, the other patients liked the result very much. On the other side, all the patients declared no loss of functionality following this SCA flap surgery.
Conclusion
In the study, we have seen in the light of our experience that the SCA flap is a strong reconstructive tool for the head and neck, and has consistently demonstrated a reliable flap for these regions with a perfect color match. This can be used safely in tissue loss in the region due to its low morbidity, adequate tissue transfers to the desired area, and a safe method.
Compliance with Ethical Standards
Conflict of interest
The author declares no conflict of interest for the present research article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hung WY, Tung CC, Fang WY, Kao WP, Lin SL, Poon Y, et al. Free flap transfer for head and neck reconstruction using local anesthesia in elderly patients. Ann Plast Surg. 2018;80:S30–s5. doi: 10.1097/SAP.0000000000001303. [DOI] [PubMed] [Google Scholar]
- 2.Kass JL, Lakha S, Levin MA, Joseph T, Lin HM, Genden EM, et al. Intraoperative hypotension and flap loss in free tissue transfer surgery of the head and neck. Head Neck. 2018;40(11):2334–2339. doi: 10.1002/hed.25190. [DOI] [PubMed] [Google Scholar]
- 3.Welz C, Canis M, Schwenk-Zieger S, Spiegel JL, Weiss BG, Pilavakis Y. Oral cancer reconstruction using the supraclavicular artery island flap: comparison to free radial forearm flap. J Oral MaxillofacSurg. 2017;75(10):2261–2269. doi: 10.1016/j.joms.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 4.Cannady SB, Hatten KM, Bur AM, Brant J, Fischer JP, Newman JG, et al. Use of free tissue transfer in head and neck cancer surgery and risk of overall and serious complication(s): an American college of surgeons-national surgical quality improvement project analysis of free tissue transfer to the head and neck. Head Neck. 2017;39(4):702–707. doi: 10.1002/hed.24669. [DOI] [PubMed] [Google Scholar]
- 5.Uçak M. Alternative methods to local flap applications in large tissue losses caused by gunshot injuries in the Syrian war. J Craniofac Surg. 2020;31(5):1208–1211. doi: 10.1097/SCS.0000000000006347. [DOI] [PubMed] [Google Scholar]
- 6.Patel SY, Meram AT, Kim DD. Soft tissue reconstruction for head and neck ablative defects. Oral MaxillofacSurgClin North Am. 2019;31(1):39–68. doi: 10.1016/j.coms.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Alfouzan AF. Review of surgical resection and reconstruction in head and neck cancer. Traditional versus current concepts. Saudi Med J. 2018;39(10):971–80. doi: 10.15537/smj.2018.10.22887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ucak M. Shrapnel injuries on regions of head and neck in Syrian war. J Craniofac Surg. 2020;31(5):1191–1195. doi: 10.1097/SCS.0000000000006345. [DOI] [PubMed] [Google Scholar]
- 9.Ucak M, Celikkaya ME. Surgical evaluation of flame burn injuries in syrian civilians. J Burn Care Res. 2019;40(6):864–868. doi: 10.1093/jbcr/irz104. [DOI] [PubMed] [Google Scholar]
- 10.Granzow JW, Suliman A, Roostaeian J, Perry A, Boyd JB. Supraclavicular artery island flap (SCAIF) vs free fasciocutaneous flaps for head and neck reconstruction. Otolaryngol Head Neck Surg. 2013;148(6):941–948. doi: 10.1177/0194599813476670. [DOI] [PubMed] [Google Scholar]
- 11.Alves HR, Ishida LC, Ishida LH, Besteiro JM, Gemperli R, Faria JC, et al. A clinical experience of the supraclavicular flap used to reconstruct head and neck defects in late-stage cancer patients. J PlastReconstrAesthetSurg. 2012;65(10):1350–1356. doi: 10.1016/j.bjps.2012.04.050. [DOI] [PubMed] [Google Scholar]
- 12.Kim RJ, Izzard ME, Patel RS. Supraclavicular artery island flap for reconstructing defects in the head and neck region. CurrOpinOtolaryngol Head Neck Surg. 2011;19(4):248–250. doi: 10.1097/MOO.0b013e328347f811. [DOI] [PubMed] [Google Scholar]
- 13.Sukato DC, Timashpolsky A, Ferzli G, Rosenfeld RM, Gordin EA. Systematic review of supraclavicular artery island flap vs free flap in head and neck reconstruction. Otolaryngol Head Neck Surg. 2019;160(2):215–222. doi: 10.1177/0194599818803603. [DOI] [PubMed] [Google Scholar]
- 14.Kozin ED, Sethi RK, Herr M, Shrime MG, Rocco JW, Lin D, et al. Comparison of perioperative outcomes between the supraclavicular artery island flap and fasciocutaneous free flap. Otolaryngol Head Neck Surg. 2016;154(1):66–72. doi: 10.1177/0194599815607345. [DOI] [PubMed] [Google Scholar]
- 15.Tayfur V, Magden O, Edizer M, Menderes A. Supraclavicular artery flap. J CraniofacSurg. 2010;21(6):1938–1940. doi: 10.1097/SCS.0b013e3181f4ee38. [DOI] [PubMed] [Google Scholar]
- 16.Chen W-L, Zhang D-M, Yang Z-H, Huang Z-Q, Wang J-G, Zhang B, et al. Extended supraclavicular fasciocutaneous island flap based on the transverse cervical artery for head and neck reconstruction after cancer ablation. J Oral MaxillofacSurg. 2010;68(10):2422–30. doi: 10.1016/j.joms.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 17.Epps MT, Cannon CL, Wright MJ, Chaffin AE, Newsome RE, Friedlander PL, et al. Aesthetic restoration of parotidectomy contour deformity using the supraclavicular artery island flap. PlastReconstrSurg. 2011;127(5):1925–1931. doi: 10.1097/PRS.0b013e31820cf40a. [DOI] [PubMed] [Google Scholar]
- 18.Chu MW, Levy JM, Friedlander PL, Chiu ES. Tracheostoma reconstruction with the supraclavicular artery island flap. Ann PlastSurg. 2015;74(6):677–679. doi: 10.1097/SAP.0b013e3182a9e9bd. [DOI] [PubMed] [Google Scholar]
- 19.Heitland AS, Pallua N. The single and double-folded supraclavicular island flap as a new therapy option in the treatment of large facial defects in noma patients. PlastReconstrSurg. 2005;115(6):1591–1596. doi: 10.1097/01.prs.0000160694.20881.f4. [DOI] [PubMed] [Google Scholar]
- 20.Lamberty BGH. The supra-clavicular axial patterned flap. Br J PlastSurg. 1979;32(3):207–212. doi: 10.1016/S0007-1226(79)90033-X. [DOI] [PubMed] [Google Scholar]
- 21.Pallua N, von Heimburg D. Pre-expanded ultra-thin supraclavicular flaps for (full-) face reconstruction with reduced donor-site morbidity and without the need for microsurgery. PlastReconstrSurg. 2005;115(7):1837–1844. doi: 10.1097/01.prs.0000165080.70891.88. [DOI] [PubMed] [Google Scholar]
- 22.Vinh VQ, Ogawa R, Van Anh T, Hyakusoku H. Reconstruction of neck scar contractures using supraclavicular flaps: retrospective study of 30 cases. PlastReconstrSurg. 2007;119(1):130–135. doi: 10.1097/01.prs.0000244843.49596.e5. [DOI] [PubMed] [Google Scholar]