Abstract
Osteoplastic flap surgery of the frontal sinus is still a relevant surgical technique for frontal sinus pathologies despite advancements in endoscopic techniques due to the complex anatomy of frontal sinus and limitations of endoscopic techniques for certain pathologies. The most crucial step in this surgery is accurate delineation of the frontal sinus pneumatisation which guides the osteotomies and this is conventionally done with radiographs which is not without errors. Here we present three cases where we have utilized image guidance technology for osteoplastic flap surgery of the frontal sinus with superior results.
Keywords: Frontal sinus, Osteoplastic frontal sinus flap, Image guided surgery
Introduction
Osteoplastic flap procedure with obliteration of the frontal sinus was considered the mainstay of surgical management of the frontal sinus in 1950′s and 1960′s [1]. However, with the advent of endoscopic techniques this open approach is now reserved for those conditions where endoscopic technique is inadequate for clearance of frontal sinus disease. This includes failed endoscopic surgeries for chronic frontal sinusitis, recurrent stenosis of frontal recess, fibrosseous lesions of frontal sinus, fractures of frontal sinus involving the frontal recess and cerebrospinal fluid leak due to defects in the posterior table of frontal sinus [2]. In the traditional surgical technique, the extend of pneumatisation and the margins of the frontal sinus is gauged using a Caldwell view radiograph taken at a distance of 6 feet from the point of focus [3]. A sterilized cut out of the radiograph is used as an intraoperative onlay template to delineate the frontal sinus. The template is placed such that the nasofrontal suture and supraorbital rims are aligned and the osteotomies are made accordingly. This is however a crude method and precise delineation of the frontal sinus is of crucial importance in osteoplastic surgeries of the frontal sinus due to its proximity to the orbit and cranial cavities [4]. The reliability of the template depends on the position of the patient, distance at which the radiograph is taken, penetration of the x-rays, and other technical aspects. This crucial step allows very little space for errors as any small variation can result in misled osteotomies which can be detrimental to the patient. This is where image guidance can be more advantageous due to its technology which offers high precision.
In cases of navigation assisted frontal sinus osteoplastic surgery, it is necessary to obtain a computed tomography (CT) scan taken according to image guidance protocol. At the beginning of surgery, a skull reference array is anchored percutaneously near the vertex of the cranium. In our operative set up we have used the fusion compact electromagnetic navigation system by Medtronic. The imaging data is loaded into the workstation via a CD-ROM and the registration of the patient is completed by cross checking of fiducial markers. After registration the instruments are calibrated by the system, accuracy is verified by testing various known landmarks on the patient’s face after which the navigation system is ready for use. A coronal or mid forehead incision is made and osteoplastic flaps are raised and dissected till the galea with the elevation of frontalis muscle to expose the frontal bone. Using the hand held probe the perimeter of the frontal sinus is demarcated and bony cuts are made through the anterior table to expose the sinus interior. Once the sinus has been opened the anatomic accuracy of the image guidance is once again verified and the surgeon proceeds with the surgery as per the indication and pathology.
Here we have compiled a case series of three navigation assisted frontal sinus osteoplastic flap surgeries performed in our centre.
Case 1
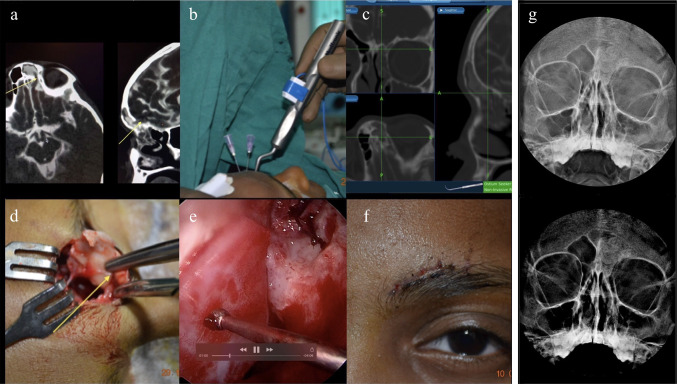
A nine year old female presented to our outpatient department with complaints of watery discharge from left nose since 3 months. She had no history of allergic sympoms. There was no past history of meningitis. She had suffered from a road traffic accident 8 months back following which she developed watery rhinorrhoea from left nose. She had undergone an open CSF leak repair through left frontal craniotomy and an anterior cranial fossa repair at another centre. She was asymptomatic immediately after the surgery but the symptoms recurred 2 months later for which she consulted our centre. CT cisternogram showed a small bony defect in the posterior wall of left frontal sinus measuring 1.5 cm × 2 cm along with a meningoencephalocele. Cerebrospinal fluid leak was confirmed with a positive Beta transferrin. She was planned for leak repair using osteoplastic flap technique via a brow incision.
The frontal sinus outlines were marked using the navigation system and needles were used to mark the margins. After raising the flap, a unipolar cautery was used to mark the margins before removing the needles. Then an osteoplastic flap pedicled inferiorly was raised and defect in the posterior wall of frontal sinus was localised and confirmed. The meningoencephalocele was cauterised using bipolar and sinus mucosa was removed completely. The defect was repaired with fascia and autograft cartilage using underlay technique. Then the outflow tract was examined, mucosa everted and sinus obliteration done using bioactive glass. The advantages of using bioactive glass are that it promotes new bone formation, avoids donor site morbidity, it is non-toxic and minimises chances of infection. Following this the flap was repositioned and wound sutured in layers. The postoperative course was uneventful. The patient has been on regular follow up for the last 3 years and is doing well (Fig. 1).
Fig. 1.
a CT cisternography image showing the defect in the inner table of left frontal sinus, b Frontal sinus delineation using navigation and use of needles to mark the margins, c Navigation image showing left frontal sinus in coronal, axial and sagittal planes, d osteoplastic flap raised (yellow arrow), e Image showing autologous cartilage used as graft for repairing defect in the posterior wall of left frontal sinus, f postoperative image showing the healed brow incision, g Post-operative X-ray of the paranasal sinuses in Caldwell luc view showing obliterated left frontal sinus using bioglass
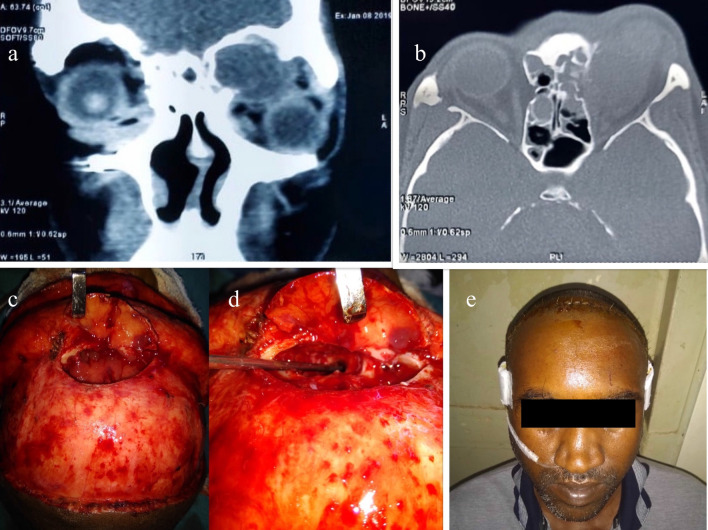
Case 2
A thirty four year old male presented with complaints of left eye proptosis since ten days. He had consulted an ophthalmologist one month back and undergone an anterior orbital decompression for the same. There was past history of a road traffic accident 10 years back, details of which was unavailable. Computed tomography revealed an expansile soft tissue density in the left frontal sinus suggestive of a mucocele with associated bone erosion and extension of the lesion into superomedial aspect of left orbit causing extraconal compression and proptosis. The frontal recess was narrow radiologically and hence he was planned for an external approach of osteoplastic repair under general anaesthesia with navigation guidance. After a bicoronal incision left frontal sinus outline was mapped with a navigation probe. Then drill holes were made. The holes were connected with the help of an oscillating saw and an inferiorly pedicled flap was raised. Then the mucocele was drained and mucosa from the frontal sinus removed. As the frontal recess was narrow on the left side, the inter frontal septum was removed and the right frontal sinus was opened and both sinuses were drained into the right frontal sinus outflow tract. No sinus obliteration was done. A cannula was placed in the right nasal cavity to drain the frontal sinuses through the right frontal recess which was removed after a week. Flap was repositioned back and sutured in layers. Postoperative course was uneventful. Patient is on follow up since the last 2 years and is asymptomatic (Fig. 2).
Fig. 2.
a, b Computed tomography images of paranasal sinuses in coronal and axial planes respectively showing displacement of globe inferiorly and laterally by soft tissue mass (c) osteoplastic flap approach to frontal sinus showing mucocele. d Image after removing mucocele and interfrontal septum. e Postoperative picture with right frontal sinus cannula insitus
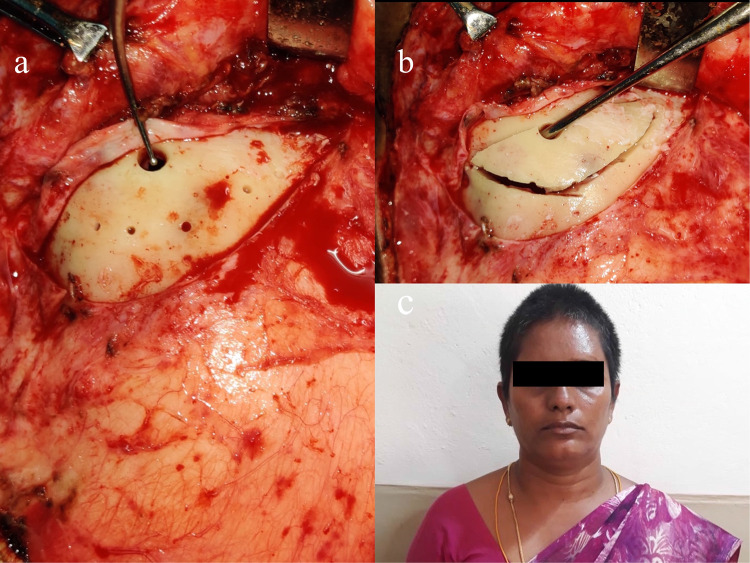
Case 3
A forty one year old lady with no comorbidities presented with complaints of recurrent right eye proptosis since childhood. The proptosis was painless and spared extra-ocular movements and vision. She had undergone multiple surgical procedures for the same complaints the details of which were unavailable with the patient. There were no nasal complaints. MRI brain showed an expansile T2 hyperintense cystic lesion within the left frontal sinus with extension into the left orbit and associated proptosis suggestive of a recurrent mucocele of right frontal sinus. She was planned for an osteoplastic flap procedure through a bicoronal incision.
After outlining the frontal sinus on the right side with navigation system, burr holes were made. Through these burr holes a ball probe was used to delineate the internal boundaries and further burr holes were made. An oscillating saw was used to connect the holes made and an inferiorly pedicled osteoplastic flap was made. Right Frontal sinus was entered and mucocele was drained. Sinus mucosa from inside was removed and outflow tract mucosa everted. Sinus obliteration was done with abdominal fat. Flap repositioned and wound sutured in layers. Post operative period was uneventful. Patient has been on follow up since last 6 months and is doing well (Fig. 3).
Fig. 3.
a Burr holes made over the frontal sinus margins with probe insitu to delineate internal boundaries. b Osteotomy made by connecting the burr holes using oscillating saw. c Postoperative image with bicoronal incision within the hairline
Discussion
Image guidance is an important tool in surgeries of the paranasal sinuses as they aid the surgeon with intraoperative anatomical localization. It is particularly of importance in frontal sinus surgeries due to its variable development, complex anatomy and proximity of the sinus to cranial and orbital contents. In this era where endoscopic surgeries are the mainstay in surgical management of paranasal sinus disease there is limited role for open or external approaches. However, management of frontal sinus disease still remains a challenge to most otorhinolaryngologists and careful selection of the surgical technique is of utmost importance in maximizing exposure and minimizing complications. Despite the evolution of advanced endoscopic surgeries of the frontal sinus the open approach such as the osteoplastic flap technique continues to be relevant due to its long term proven success [5]. One amongst the indications for osteoplastic flap surgeries of the frontal sinus is failed endoscopic surgeries, which in-turn reinforces the need for image guidance due to distorted anatomy and loss of surgical landmarks. Although osteoplastic flap surgery of the frontal sinus has good success rates, it is not without complications. In 20% of patients, there is risk of major intraoperative complications such as dural exposure, dural injury leading to cerebrospinal fluid leak and orbital fat exposure [2]. Most of these complications arise from over estimation of the pneumatisation of frontal sinus which indeed results in misdirected osteotomies that extend beyond the confines of the frontal sinus and result in an osteoplastic flap which is too large. On the other hand, underestimation of the size can result in a small bony flap hindering the complete view of the sinus interior resulting in incomplete removal of mucosa thus increasing the risk of postoperative mucocele formation [6]. The first to report the use of image guidance technology for delineating the osteoplastic flap in frontal sinus surgery was Carrau et al. in 1994 [6]. He compared the radiographic template method versus image guidance technique and found that the latter was more accurate [6]. In his study the image guidance assisted cases did not overestimate the boundaries of the frontal sinus. Another study compared four techniques of frontal sinus mapping including 6 foot Caldwell radiograph, sinus trans illumination, sinus trephination with probing and image guidance and found image guidance to be the most accurate and safe method while the radiographic template method was the least accurate and had high chances of error [3]. A recent study also confirmed a significant reduction of intraoperative complications when image guidance was used for determining the frontal sinus contours in osteoplastic technique [7]. Image guidance besides being more accurate is also a non-invasive method and does not involve intraoperative radiation exposure. However, it is much more expensive, requires an immobile head, its initial set up is time consuming and it is not widely available.
Conclusion
Image guidance technology is a reliable method of frontal sinus delineation in osteoplastic flap surgeries and ensures accuracy and safety compared to conventional methods. When available, the utilization of this technology helps to improve the surgical outcome by minimizing complications and obviating the need for further surgeries due to incomplete removal of disease which may result from incomplete exposure.
Author contributions
All authors made substantial contribution to this paper and all the authors have approved the version to be published.
Funding
No funds, grants, or other support was received.
Data Availability
Data transparency has been maintained.
Compliance with Ethical Standards
Conflicts of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Consent for Publication
The participants have consented to the submission of the case report and photographs to the journal.
Consent to Participate
Informed consent was obtained from parents of case 1 and individual participants of case 2 and 3 included in the study.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the institution ethics committee.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Goodale RL, Montgomery WW. Experience with osteoplastic anterior wall approach to the frontal sinus. Arch Otolaryngol. 1958;68:271. doi: 10.1001/archotol.1958.00730020281001. [DOI] [PubMed] [Google Scholar]
- 2.Weber R, Draf W, Keerl R, Kahle G, Schinzel S, Thomann S, Lawson W. Osteoplastic frontal sinus surgery with fat obliteration: technique and long- term results using magnetic resonance imaging in 82 operations. Laryngoscope. 2000;110:1037–1044. doi: 10.1097/00005537-200006000-00028. [DOI] [PubMed] [Google Scholar]
- 3.Ansari K, Seikaly H, Elford G. Assessment of the accuracy and safety of the different methods used in mapping the frontal sinus. J Otolaryngol. 2003;32:254–258. doi: 10.2310/7070.2003.41622. [DOI] [PubMed] [Google Scholar]
- 4.Daniel M, Watson J, Hoskison E, et al. Frontal sinus models and onlay templates in osteoplastic flap surgery. J Laryngol Otol. 2011;125:82–85. doi: 10.1017/S0022215110001799. [DOI] [PubMed] [Google Scholar]
- 5.Silverman JB, Gray ST, Busaba NY. Role of osteoplastic frontal sinus obliteration in the era of endoscopic sinus surgery. Int J Otolaryngol. 2012;2012:501896. doi: 10.1155/2012/501896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carrau RL, Snyderman CH, Curtin HB, et al. Computer-assisted frontal sinusotomy. Otolaryngol Head Neck Surg. 1994;111:727–732. doi: 10.1177/019459989411100605. [DOI] [PubMed] [Google Scholar]
- 7.Sindwani R, Metson R. Impact of image-guidance on complications during osteoplastic frontal sinus surgery. Otolaryngol Head Neck Surg. 2004;131:150–155. doi: 10.1016/j.otohns.2004.03.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data transparency has been maintained.