Abstract
Allergic rhinitis (AR) is one of the commonest forms of allergy in the world which causes significant morbidity. The prevalence has all the more increased because of increasing air pollution. Though skin prick testing (SPT) and sublingual immunotherapy (SLIT) have now been widely accepted world wide as important tool, offering prospective long term remission or cure for allergic rhinitis yet some still debate the accuracy and efficacy of both. This prospective study was conducted from February 2018 to May 2020, from amongst the patients of allergic rhinitis, presenting to the author in his private clinic. There were total 37 patients who presented with symptoms suggestive of allergic rhinitis and who underwent SPT for various common aeroallergens, as suggested by their history. The age range of the patients was from 6 to 60 years, with a mean age of 27.62 years. There were 23 male and 14 female patients with a male to female ratio of 1.76:1. The commonest age group affected is 21–30 year group. Out of the total 37 patients of allergic rhinitis, who underwent SPT, 32 (86.5%) had a positive response and 05 (13.5%) patients had a negative response. Out of the 32 patients with positive response, 30 (93.8%) had positive reactions to multiple allergens and just 2 (6.2%) had positive reaction to single allergen. The commonest aeroallergen detected by SPT was house dust mite (bed mite) Dermatophagoides (D)-pteronyssinus, and another house dust mite (floor mite), D-farinae, followed by Blomia, another floor mite. Out of the 32 SPT positive cases 10 (31.3%) patients opted for SLIT, after knowing the pros and cons. It can be concluded from this preliminary study that there is no doubt that SPT is a very informative confirmatory test for diagnosing allergens causing allergic rhinitis. The commonest allergen involved in causing allergic rhinitis in and around Tripura are the dust mites, commonest being D-pteronyssinus and D-farinae. SLIT has a good acceptance in the allergic rhinitis patients and out of ten all of the patients reported significant symptomatic improvement. This allergen mapping in this area is probably the first of its kind, which will help in deciding future strategies in management of AR, by immunotherapy or avoidance measures. In future many more patients may get benefit of long term cure from it.
Keywords: Allergic rhinitis, Skin prick test (SPT), Sub lingual immunotherapy (SLIT)
Introduction
Allergic rhinitis is a fairly common disease affecting 10 to 30% of global population for adults and in children the prevalence can be as high as 40% [1, 2]. Allergic rhinitis is the most common form of allergy worldwide characterized by, excessive sneezing, nasal and eye itching and watery rhinorrhea and nasal stuffiness when immune system becomes sensitized and over reacts to airborne allergens [3]. Symptoms of allergic rhinitis usually develop before 20 years of age and peak at the age of 20–40 years before gradually declining [4]. Allergy refers to immediate (type I) hypersensitivity to environmental antigens. These antigens in case of allergic rhinitis are aero allergens which are usually present in the house hold or the environment like the dust and dust mites and the pollen of several trees and grass and insects like the cockroaches and the animal dander, moulds. The aero-allergens involved in allergic rhinitis vary from place to place. The objective of this prospective study is to find out the dominant aero allergens, with special reference to dust mite, involved in allergic rhinitis in this part of the country; complete data of offending aero-allergens from Tripura is not available. Also, the objective was to, do a preliminary study of the role of SPT and SLIT in the management of allergic rhinitis in Tripura.
Allergic rhinitis is an, immunoglobulin E (IgE) mediated disease with complex interaction of genetic and environmental factors. Allergic rhinitis is an immediate (type I) hypersensitivity reaction to various environmental factors. Allergic rhinitis and bronchial asthma are known to coexist and up to 40% of allergic rhinitis patients go on to develop allergic asthma. So it is evident that allergic rhinitis is fairly common ailment, occurring in up to 30% of the global population with significant morbidity [1, 2]. There are, basically three different types of allergic rhinitis viz. perennial allergic rhinitis (PAR), seasonal allergic rhinitis (SAR) and perennial allergic rhinitis with seasonal exacerbations [5]. We have followed these definitions in our study, though allergic rhinitis and its impact on asthma (ARIA), 2010 has categorized AR as 4 types namely, mild intermittent, moderate/severe intermittent, mild persistent and moderate/severe persistent types [6]. Perennial allergic rhinitis are characterized by symptoms all round the year, and mainly caused by dust and dust mites, cockroach, and animal dander. Seasonal allergic rhinitis occurs mainly in certain seasons like spring, late summer, rainy season and early fall when trees, grass, moulds and weeds respectively pollinate. The third variety perennial allergic rhinitis with seasonal exacerbation is characterized by AR symptoms all round the year which may aggravate in certain seasons due to allergy to certain pollens too.
If these allergens can be identified by the SPT in AR patients then a long term cure can be targeted by immunotherapy or avoidance measures. The aim of this preliminary prospective study is to have glimpse of the allergens involved in AR in Tripura by SPT and to find out the acceptability of the relatively newer mode of treatment, SLIT, in Tripura, given the costs and long duration involved in the SLIT. Probably this study is the first study of its kind in Tripura.
Allergic rhinitis (AR) and hyper-reactivity of the airway are IgE mediated diseases which occurs due to complex interplay of the T-helper 1 (Th1) and T-helper 2 (Th2) paradigm of CD4 T helper lymphocytes. Antigen presenting cells display dipeptide antigens, either allergen or infectious, on their cell surfaces to the native T lymphocytes. Native T cells differentiate into Th1 or Th2 cells depending on the nature of the antigen, Th1 cells secrete Interferon gamma (IFN-y), while Th2 cells secrete IL-4, IL-5 and IL-13 (IL = Interleukin). Th2 cells promote allergic response by promoting IgE producing plasma cells [7]. The desensitization or hypo sensitization is treatment by the way of immunotherapy in which the patient is vaccinated by increasingly large doses of the incriminated allergen, thereby suppressing the Th2 activity and increasing the immunoglobulin G (IgG) response over the IgE. In short, the person develops immunity to the increasing amounts of the allergen in question. The long term efficacy and protective effect of immunotherapy in reducing the development of new allergy has been demonstrated in several studies [8–11].
Materials and Methods
The study is a prospective study on the dominant allergens involved in causing allergic rhinitis in and around Tripura and a glimpse, on the acceptance and role of SPT and SLIT in the management of AR in Tripura. Probably, as per internet search, this study is first of its kind in Tripura. This study was conducted from February, 2018 to May, 2020 from patients attending the private OPD of the author and giving a history suggestive of AR. The patients between 6 and 60 years and who gave a history indicative of AR were included in the study. A detailed history was taken including family history of AR or bronchial asthma. Diagnosis was based on clinical history and physical examination. Patients of chronic rhino sinusitis or any other infective or non-infective causes of chronic rhinitis, other than AR, like atrophic rhinitis, occupational rhinitis, vasomotor rhinitis, aspirin sensitivity, nasal polyposis, endocrine disease, pregnancy and drug induced rhinitis were excluded from the study.
Treatment history was taken and patients on antihistamines and steroids, drugs liable to affect results of SPT, were asked to stop the medications at least 7 days before coming for SPT. Patients, with any skin condition like dermatographia or any other chronic skin condition were excluded from the study. Skin prick tests were performed with relevant antigens, as directed by the history, following standard norms of positive and negative control with histamine and saline. The SPT antigens included dusts and dust mites, cockroach, latex (as Tripura has plenty of rubber plantations), grasses and weeds flowering all round the year, fungi found all round the year and some tree pollens. The antigens were procured from Creative Diagnostic Medicare Pvt. Ltd, Vashi, Navi Mumbai, India. The SPT reaction was done on the anterior surface of the fore arm and read 15 to 20 min after the prick and a second reading was taken 30 min after the skin prick. Comparison with the positive and negative control was done and any wheal greater than the negative control by 3 mm was taken as positive. The wheal diameter should be at least 5 mm in case of positive control and any reaction equal to or more than the positive histamine control and developing pseudopodia was taken as strongly positive. Ten patients agreed to undergo SLIT after having understood the treatment method and duration. Vaccines were procured from Creative Diagnostic Medicare Pvt. Ltd., Navi Mumbai. The medical history and the severity of the disease in the patients were evaluated by visual analogue scoring system. (On a scale of 0–6; 0 = no symptoms, and 6 = maximum severity). In a few of the patients a SNOT score was also taken. In the initial phase the patients were asked to take the vaccine drop sub- lingually, on the under surface of the tongue, starting with one drop in empty stomach and refrain from taking any food for at least 1 h, on any 2 days of the week, say Monday and Friday for instance. In the following weeks on the same days drops were increased by one drop every week. Three vials of increasing strengths of the vaccines, with three different colour codes, were initially given to the patient and the vaccines were refrigerated at 6 to 8 °C. The patients took the vaccines sub-lingually, as mentioned above, and when the third vial was half way finished then the booster doses were procured and supplied to the patients. The booster doses were fixed doses, 5 drops per day sub-lingually in empty stomach, and twice a week with 2 days gap in between. The patients were asked to report any problem or improvement over telephone and come for follow up every week, for the first 1 month and the results recorded. Drops doses were adjusted if the patients had increased symptoms or itching.
Results
A total of 37 patients participated in the study in the private clinic of the author from April 2018 to May, 2020. There were total 37 patients who presented with symptoms suggestive of allergic rhinitis and who underwent skin prick test (SPT) for various common aeroallergens, as suggested by their history. The age range of the patients was from 6 to 60 years, with a mean age of 27.62 years. There were 23 male and 14 female patients (Fig. 1) with a male to female ratio of 1.76:1. The commonest age group affected is 21–30 year group. Out of the total 37 patients of allergic rhinitis, who underwent SPT, 32 (86.5%) had a positive response and 05 (13.5%) patients had a negative response, as shown in (Fig. 2). Out of the 32 patients with positive response, 30 (93.8%) had positive reactions to multiple allergens and just 2 (6.2%) had positive reaction to single allergen. The commonest aeroallergen detected by SPT was house dust mite (bed mite) Dermatophagoides (D)-pteronyssinus, and another house dust mite (floor mite), D-farinae, followed by Blomia tropicalis, another floor mite.
Fig. 1.
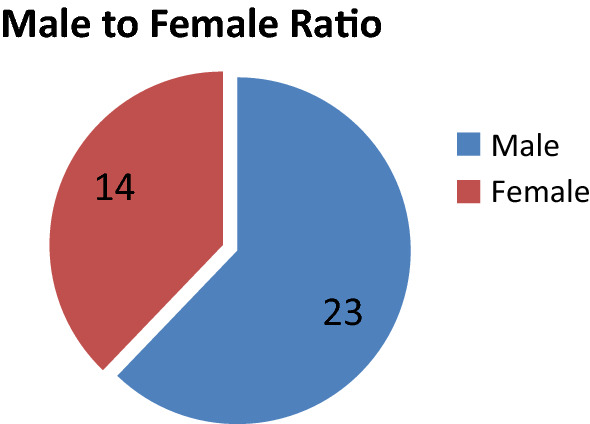
Pie chart showing sex distribution (N = 37, male = 23, female = 14)
Fig. 2.
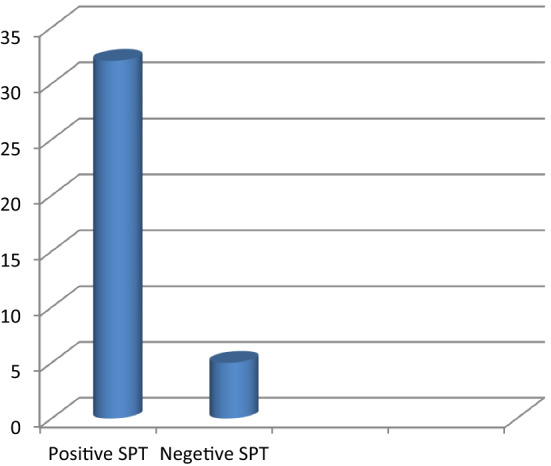
Bar diagram showing distribution positive and negative response in AR (N = 37, positive SPT = 32, negative SPT = 05)
Varieties of other allergens were detected among the patients in this study, like house dust, the third commonest and cockroach, spider web, cotton dust and grass pollens like Aramanthus spinosus and Parthenium hysterophorus etc. The detailed distribution the allergens are as in Table 1. Most of the patients, 30 out 32 patients (94%) were reactive to multiple antigens and only 2 patients (06%) were reactive to single antigen i.e. D-farinae.
Table 1.
Distribution of common allergens involved in causing AR in Tripura
| Name of the antigen | Number of positive reactions |
|---|---|
| D-pteronyssinus (Bed mite) | 26 |
| D-farinae (Floor mite) | 26 |
| Blomia (Floor mite) | 22 |
| House dust mite | 06 |
| Cockroach | 05 |
| Spider web dust | 04 |
| Cotton dust | 03 |
| Aramanthus spinosus (Pollen) | 02 |
| Perthenium hysterophorus (Weed pollen) | 02 |
| Fusarium solani (Fungi) | 02 |
| Cynodon dactylon (Durva grass pollen) | 01 |
| Cenchrus barbatus (Grass pollen) | 01 |
| Rice dust | 02 |
| Wood dust | 01 |
| Xanthium strumarium (Weed pollen) | 01 |
| Ischaemium indicum (Grass pollen) | 01 |
| Mosquito | 01 |
| Cat | 01 |
| Aspergillus fumigatus (Fungi) | 01 |
| Helminthosporium (Fungi) | 01 |
| Penicillium (Fungi) | 01 |
There were 12 patients belonging to the scheduled tribe community, 7 from the scheduled caste community, and 7 from the other backward classes and 11 from the general community. Tripura is a state with a mixed population of various mongoloid tribes and non-tribal mostly Bengali community. It is observed here that out of 37 patients only 12 (32.4%) were from the tribal community and the rest 25 (67.5%) were from the non-tribal community.
Ten out of 32 (31.25%) SPT positive cases opted for SLIT after understanding the mode of treatment and time duration and costs involved and other alternative modes of treatment other than SLIT. Out of these 10 patients all had reported improvement in symptoms to start with however 06 patients discontinued the SLIT because of various reasons like early resolution of symptoms, familial and economic issues and others because of the long time period required for sustained treatment. Most of the patients had symptoms all round the year. In fact, 31 out of 32 patients (96.9%) were of PAR, and one patient (3.1%) was PAR with seasonal exacerbation in winter. There were no patients of SAR, so far in this study. There were 8 patients (25%) out of the SPT positive cases who also had bronchial asthma. There was one each patient of otitis media with effusion, chronic suppurative otitis media and two patients had concomitant food allergy too.
Discussion
Allergic rhinitis is characterized by inflammatory changes in the nasal mucosa caused by exposure to inhaled allergens. It is a common disease affecting between 0.8 and 39.7% of the world population (depending on location). It causes significant morbidity and is often poorly managed. There are several other co-morbidities like allergic conjunctivitis, bronchial asthma, urticaria and otitis media which are associated with AR [12]. In our study too, 25% of the SPT reactive AR patients had associated history of bronchial asthma.
It is an Ig E mediated disease which is expressed in various severity and form depending on certain genetic and environmental factors. Quite often close relatives, parents or siblings also suffer from allergic rhinitis or other allergic disorders like urticaria and asthma. Having parents who are atopic may increase the chances of a child developing allergic diseases by 3–6 times. The role of environment in AR cannot be over emphasized as it is seen that children living in unhygienic conditions in the rural areas are less prone to develop allergic diseases than their urban counterparts. Larger family size, more frequent infections and unhygienic contact may all be protective—the hygiene hypothesis [12]. This suggests that reduced infections in the urban, hygienic, well to do societies with more vaccination cover of the children reduces the Th1 response and leads to a Th2 immune overdrive leading excessive production of IgE and consequent atopy [13]. In our study too it is noticed that the indigenous tribal population living in the rural areas less affected by AR than the non-tribal Bengali population living in the more urban areas. The tribal patients comprised 32.4% and the non-tribal Bengali population comprised 67.6% and this shown in Fig. 3.
Fig. 3.
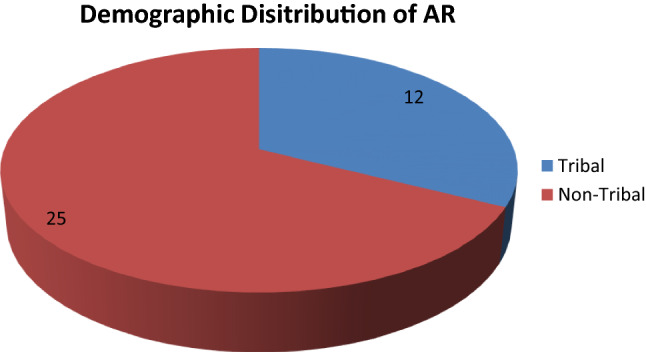
Pie-chart is showing distribution of AR amongst tribal and non tribal population of Tripura
In this study there was a male predominance with the male to female ratio being 1.76:1 and the commonest age group affected is 21–30 years. This is also corroborated in other studies which showed that though there is male predominance in AR in childhood in other parts of the world yet in Asia male predominance continued even beyond childhood and adolescence [14].
In this study predominant allergens involved in causing AR is found to be dust mite, D-pterronysinus, D-farinae and Blomia-tropicalis closely followed other dusts and cockroach and only a few cases of pollen allergy. Tripura being situated in tropical climate zone, house dust mite and other dusts and cockroach were found to be predominant aero-allergens involved in causing AR. Similar results were found in nearby Kolkata, West Bengal, India [15].
In this study, among the 37 patients presenting with AR 32 (86.5%), had positive response to skin prick test and 05 had no significant response to the selective aero-allergens tested by SPT. SPT is one of the confirmatory tests for IgE mediated allergic disorders like AR and BA. Similar results were found in a study in Kashmir [7]. In another study sensitivity and specificity were found to be 85% and 77% respectively [16]. The 5 patients who had no identifiable aero-allergens could possibly be reactive to some other allergens not in our panel. More over SPTs may not identify patients with low-level IgE hypersensitivity reactions (triggering smaller than 3 mm size wheals) [17].
In our study SLIT was taken up by 10 patients and all of them reported significant improvement in their symptoms. In our state of Tripura and adjoining areas, the concept of SLIT is new and the long duration of treatment involved in SLIT and the costs involved may be the cause of less number of patients opting for SLIT. More over SLIT does not give immediate relief in AR symptoms like anti histamines and corticosteroids, rather in the initial phase symptoms may aggravate a bit. None the less 25% of the patients in this study took up SLIT and got reported significant relief.
Conclusion
In Tripura and surrounding areas the dominant aero-allergens are house dust mite especially D-pteronyssinus, D-farinae and Blomia-tropicalis followed by cockroach. This is probably the first mapping of the aero-allergens in this part of the country and this will definitely help in planning avoidance measures and other treatment modalities like SLIT in the management of AR. Skin prick test is definitely an indispensible and easy to perform confirmatory test for AR and very much required to identify the offending aero-allergens involved in causing allergic rhinitis. Prevalence of perennial allergic rhinitis is found to be more in this part of the country.
Compliance with Ethical Standards
Conflict of interest
The author declares that there is no conflict of interest with anybody participating in the study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Meltzer EO, Blaiss MS, Dereberry MJ, Mahr TA, Gordon BR, Sheth KT, et al. Burden of allergic rhinitis: results from the paediatric allergies in America survey. J Allergy Clin Immunol. 2009;124:S43–S70. doi: 10.1016/j.jaci.2009.05.13. [DOI] [PubMed] [Google Scholar]
- 2.Keith PK, Desrosiers M, Laister T, Schellenberg RR, Waserman S. The burden of allergic rhinitis (AR) in Canada; perspectives of physicians and patients. Allergy Asthma Clin Immunol. 2012;8(7):1–11. doi: 10.1186/1710-1492-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bosquet J, Khaltaev N, Cruz A, Denburg J, Fokkers W, Togia A, et al. Allergic rhinitis and its impact on asthma (ARIA) Eur J Allergy Clin Immunol. 2008;63(S86):8–160. doi: 10.1111/j-1398-9995.2007.01620.x. [DOI] [Google Scholar]
- 4.Wheatly LM, Togias A. Allergic rhinitis. N Engl J Med. 2015;372(5):456–463. doi: 10.1056/NEJMcp1412282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wallace DV, Dykewicz MS, Bernstein DI, et al. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol. 2008;122(2 Suppl):S1–S84. doi: 10.1016/j.jaci.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 6.Bousquet J, Van Cawenberge P, Khalteiv N. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol. 2001;108(5 Suppl):S147–S334. doi: 10.1067/mai.2001.118891. [DOI] [PubMed] [Google Scholar]
- 7.Roohi R, Irfan Ali S, Saniya N, Zafar AS, Niyaz N, Mushtaq AS, Aga SS. Role of skin prick test in allergic disorders: a prospective study in Kashmiri population in light of review. Basic Res. 2013;58(1):12–17. doi: 10.4103/0019-5154.105276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross RN, Nelson HS, Finegold I. Effectiveness of specific immunotherapy in treatment of allergic rhinitis an analysis of randomized, prospective, single or double blind, placebo controlled studies. Clin Ther. 2001;22:342–350. doi: 10.1016/S0149-2918(00)80038-7. [DOI] [PubMed] [Google Scholar]
- 9.Rank MA, Li JT. Allergen immunotherapy. Mayo Clin Proc. 2007;82:1119–1191. doi: 10.4065/82.9.1119. [DOI] [PubMed] [Google Scholar]
- 10.Passalacqua G, Durham SR. Allergic rhinitis and its impact on asthma update; allergen immunotherapy. J Allergy Clin Immunol. 2007;119:881–891. doi: 10.1016/j.jaci.2007.01.045. [DOI] [PubMed] [Google Scholar]
- 11.Frew AJ, Powell RJ, Corrigan CJ, Durham SR. UK Immunotherapy Study Group. Efficacy and safety of specific immunotherapy with subcutaneous allergen extract in treatment resistant seasonal allergic rhino-conjunctivitis. J Allergy Clin Immunol. 2006;117:319–325. doi: 10.1016/j.jaci.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 12.Quentin G. Allergic rhinitis. In: John CW, Raymond WC, editors. Scott–Brown’s otorhinolaryngology head and neck surgery. 8. Boca Raton: CRC Press; 2018. pp. 999–1010. [Google Scholar]
- 13.Platts-Mills TA, Erwin E, Heymann P, et al. Is the hygiene hypothesis still viable explanation for the increased prevalence of asthma? Allergy. 2005;60:S25–S31. doi: 10.1111/j.1398-9995.2005.00854.x. [DOI] [PubMed] [Google Scholar]
- 14.Mariona P, Theresa K, Andreas R, Matthias F, et al. Sex-related allergic rhinitis prevalence switch from childhood to adulthood: a systematic review and meta-analysis. Int Arch Allergy Immunol. 2017;172(4):224–235. doi: 10.1159/000464324. [DOI] [PubMed] [Google Scholar]
- 15.Amlan G, Shampa D, Sanjoy P, et al. Sensitivity to House dust Mites allergens and its relationship with CD14 C(-159 T) polymorphism in patients of West Bengal, India. J Med Entomol. 2018;55(1):14–19. doi: 10.1093/jme/tjx178. [DOI] [PubMed] [Google Scholar]
- 16.Immaculate FN, Karen B, Conrad K. Diagnostic accuracy of skin-prick testing for allergic rhinitis: a systematic review and meta-analysis. Allergy Asthma Clin Immunol. 2016;12:20. doi: 10.1186/s13223-016-0126-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pierson-Mullay LK, Jackola DR, Blumenthal MN, Rosenberg A. Evidence of affinity threshold for IgE-allergen binding in the percutaneous skin test reaction. Clin Exp Allergy. 2002;32:107–116. doi: 10.1046/j.0022-0477.2001.01244.x. [DOI] [PubMed] [Google Scholar]


