Abstract
The purpose of this study is to compare the success rates of endoscopic endonasal dacryocystorhinostomy (EN-DCR) and external DCR (EX-DCR) for the treatment of primary acquired nasolacrimal duct obstruction (PANLDO). Prospective randomized comparative study. Study was conducted for 2 years duration in a teaching hospital with 300 cases of endoscopic and 300 cases of external DCR with a follow-up of minimum 6 months. Data regarding surgical outcome and complications were analyzed and compared using χ2 test. In our study, the overall success rate of DCR for PANLDO was 92.6%, there was difference in terms of anatomical or functional success rate between EN-DCR (93.6%) and EX-DCR (91.6%). The incidence rate of post operative complication in our study was lower in Endonasal DCR (27.33%) as compared to External DCR (48%). Patients who underwent EN-DCR had shorter recovery time, less complications and higher satisfaction due to lack of external incision, although final surgical outcomes were comparable between two groups.
Keywords: Dacryocystorhinostomy, Endoscopic, External, Epiphora
Introduction
Dacryocystorhinostomy (DCR) is a surgical bypass procedure that creates an anastomosis between the lacrimal sac and the nasal mucosa via a bony ostium, thereby restoring the flow of tears into the nose from the lacrimal sac. It is commonly indicated in cases of nasolacrimal duct (NLD) obstruction. It can be performed externally through a skin incision or internally through the nasal cavity with or without endoscopic visualization. More and more surgeons rekindle their interest in EN-DCR and have developed various ways of doing it, from mechanical with or without powered device [1].
This study aimed to compare the success rates of two different approaches endonasal endoscopic DCR & External DCR.
Many reports have comparatively studied the external and endonasal DCR approaches. Most have demonstrated that despite the advantages and disadvantages inherent in each approach, both can be considered acceptable alternatives as they had similar success rates and surgical outcomes with minimal complications. Despite endoscopic DCR being more commonly practiced nowadays, only a few studies have compared the success rates for different surgical techniques used in this procedure.
Methods
All patients attending Ophthalmology/ENT OPD in PDMMC College for symptoms of epiphora & diagnosed as primary acquired nasolacrimal duct obstruction or chronic dacryocystitis were included in this study. The diagnosis of NLD obstruction was confirmed by the ophthalmologist. Endoscopic DCR was performed in all patients with the collaboration between an ENT surgeon and an ophthalmologist at the hospital.
Anatomical success was defined as patency confirmed by intranasal endoscopic inspection of the ostium and successful lacrimal irrigation; functional success was defined as complete resolution of epiphora which were assessed at postoperative 6th months.
Sample size
The study included 600 patients diagnosed as primary acquired nasolacrimal duct obstruction or chronic dacryocystitis between April 2018 and March 2020 (2 years) and those who fulfill inclusion criteria during study period. Randomized sampling was done, wherin plain envelopes with paper chits labelled as group I and group II were kept inside, shuffled and patients were selected according to group chosen.
Inclusion criteria
All symptomatic epiphora cases diagnosed for primary acquired nasolacrimal duct obstruction or chronic dacryocystitis on clinical backgrounds.
Both male/female patients in age group 20–70 years.
Exclusion criteria
Epiphora with no signs of nasolacrimal duct obstruction on sac syringing, Ectropion/Entropion/lower lid laxity.
Canalicular and punctual obstruction, Post traumatic bone deformity, History of radiation therapy covering nasal or periorbital region, Congenital NLDO & Previous trauma history of lacrimal passage system.
The diagnosis of PANLDO was based on the presence of symptoms with epiphora, documented obstruction by lacrimal irrigation and probing. All patients were well informed about the advantages and disadvantages of the EX-DCR and EN-DCR methods.
Data were analyzed using SPSS software. Categorical variables were presented as numbers and percentages. The significance of the difference among groups in terms of means was analyzed by Student's t-test, and categorical variables were analyzed by Chi-square test. P < 0.05 was considered statistically significant.
Procedure
All surgeries were under local anesthesia. About 1% lidocaine with 1:100,000 epinephrine was used for local infiltration of incision site of skin and nasal mucosa. Nasal packing with cotton sponges soaked with mixture of 4% lidocaine and 1:100,000 epinephrine were inserted for intranasal vasoconstriction 10 min before the surgery.
For EX-DCR, a 15–20 mm curved skin incision was made medially to the angular vein at the level of the anterior lacrimal crest. The orbicularis muscle was then blunt dissected deep down to the periosteum, and the lacrimal sac was exposed by partial incision of the medial canthal ligament. The periosteum was opened by surgical blade and lifted from the anterior lacrimal crest by the freer elevator. The periosteum along with the lacrimal sac was displaced laterally. A squared bony window, sized 15 mm × 15 mm in diameters, was created with the help of drill between the insertion of the medial canthal tendon superiorly and the proximal nasolacrimal duct inferiorly, extending from anterior to posterior lacrimal crest. The lacrimal sac and nasal mucosa were opened with surgical blade in the shape of letter H, and the opposing mucosa flaps were sutured with interrupted 5–0 Vicryl. The skin was closed with interrupted 6–0 nylon sutures.
For EN-DCR, the surgery was performed by the double flap technique in all the cases. A sickle knife was used to make a vertical mucosal incision, starting 10–12 mm anterior to the axilla of the middle turbinate along the maxillary line, and extend 15–20 mm inferiorly just above the insertion of inferior turbinate. Freer elevator was used to raise the nasal mucosal flap and dissected posteriorly over frontal process of maxilla to its junction with the lacrimal bone. The nasal mucosal flap was removed by Blakesley nasal forceps. A bony window, sized 12 mm × 15 mm in diameters, was created by Kerrison rongeur and sometimes with the help of chisel and hammer.
After full exposure of the lacrimal sac, a vertical incision with horizontal releasing incisions at both superior and inferior end was made to cut the sac open. In addition to elevating the mucosal flap over the lacrimal bone, an additional flap in the lacrimal sac is created. Both flaps were used to cover any exposed bone, thus achieving marsupialization of the lacrimal sac into the nasal cavity. The upper part of the mucosal flap was repositioned on the axilla of the middle turbinate and the mucosa that covers the wall of the agger nasi was also juxtaposed to the medial wall of the lacrimal sac flap. A 10 mm × 10 mm sized absorbable hemostatic gelatin sponge, was packed onto the lacrimal sac, which helped the sac flaps to roll out against the lateral nasal wall and allowed better approximation of sac mucosa to the nasal mucosa edges. Merocel packing was inserted in the nasal cavity at the end of the surgery which was removed next day.
It is believed that with the use of such measures, leaving any exposed bone can be minimized or avoided, therefore improving postoperative healing. Since re-closure of the nasolacrimal stoma is commonly due to aberrant healing with granulation tissue and synechiae after endoscopic DCR, it seems probable that mucosa-sparing techniques may offer better success rates, better healing at the stoma site and prevention of granulation tissue and epithelialization. Thus, this may lead to a reduction of the chance of blockage of the new stoma.
All patients were discharged home on the next day of surgery with prophylactic oral antibiotic and nasal spray. The first follow up visit was scheduled at 1 week after surgery.
During the postoperative period, all patients were prescribed Antibiotic eye drops four times a day for 1 month. The skin sutures of the patients with EX-DCR were removed 1-week postoperatively. All patients were assessed at the postoperative 1st week, 15 days, 1st month, 3rd month and 6th month. During the follow-up visit, patients were asked about the symptom relief of epiphora and check patency by lacrimal sac irrigation, and intranasal endoscopic examination.
Primary outcome measurements were the anatomical and functional success at the final visit. Anatomical success was defined as patency confirmed by intranasal endoscopic inspection of the ostium and successful lacrimal irrigation. Functional success was defined as complete resolution of epiphora. Secondary outcome measurements were the postoperative time to the resolution of epiphora and surgical-related complications. All patients were followed up for at least 6 months.
Observations and Results
Age Distribution of Cases
| S. No | Age in years | Group I | Group II | Total (%) |
|---|---|---|---|---|
| 1 | 20–30 | 10 (3.33%) | 25(8.33%) | 35 (5.83%) |
| 2 | 31–40 | 20 (6.66%) | 25(8.33%) | 45 (7.5%) |
| 3 | 41–50 | 55 (18.33%) | 85(28.33%) | 140 (23.33%) |
| 4 | 51–60 | 140 (46.66%) | 105(35%) | 245 (40.83%) |
| 5 | 61–70 | 75 (25%) | 60(20%) | 135 (22.5%) |
| 6 | Total | 300 | 300 | 600 |
In our study of total 600 patients, the maximum number of patients, 245 (40.83%) belonged to 51–60 years age group, minimum number, 35 (5.83%) belonged to 20-30 years age group.
Sex Distribution

Female preponderance was observed in our study with 340 (56.66%) as compared to 260 (43.33%) in male population.
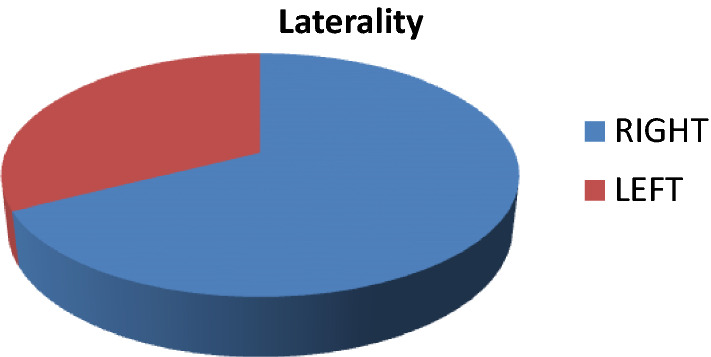
Laterality of Symptoms
In our study, Right side was the dominant affected side affected 405 (67.5%); whereas on 195 (32.5%) were having disease on left side.
Clinical Features

Epiphora was the most common clinical symptom in Both groups I (60%) & Group II (65%).
Nasal Pathology
| S. No | Nasal pathology | Group I (n = 300) | Group II (n = 300) | Total |
|---|---|---|---|---|
| 1 | DNS | 20 (6.66%) | 30(10%) | 50(8.33%) |
| 2 | Normal | 280 (93.33%) | 270 (90%) | 550(91.66%) |
Incidence of Intraoperative complications in Group I & II
| S. No | Intraoperative complications | Group I (N = 300) | Group II (N = 300) | Total (N = 600) |
|---|---|---|---|---|
| 1 | Present | 115 (38.33%) | 70 (23.33%) | 185 |
| 2 | Absent | 185 | 230 | 415 |
Intra operative complication rate was less in case of Endonasal DCR (23.33%) as compared to External DCR (38.33%) This can be explained by better &wide lacrimal sac exposure, less bleeding & crusting and ability to concurrently address nasal mucosa as compared to external approach.
Intraoperative complications
Post-Operative Complications in Group I (144/300)
The incidence rate of post operative complication was lower in EN- DCR than in EX- DCR.
Incidence of Post Operative Complications in Group I & II (N = 600)
| S.No | Intraoperative complications | Group I (N = 300) | Group II (N = 300) | Total(N = 600) |
|---|---|---|---|---|
| 1 | Present | 144 | 82 | 226 |
| 2 | Absent | 156 | 218 | 374 |
Post-Operative Evaluation by Sac Syringing in Group I (N = 300)
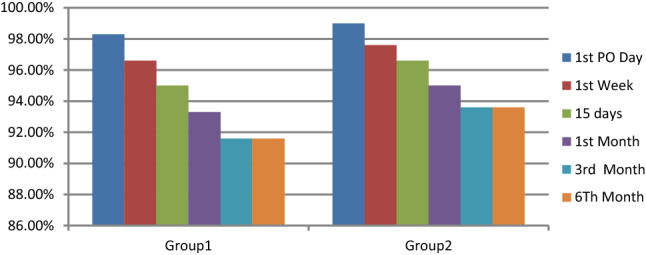
Out of 300 patients selected for Exteranl DCR 275(91.6%) remained patent in case at end of 6th month follow up, as compared to 300 patients selected for Endonasal DCR 281(93.6%) remained patent at end of 6th month follow up.
Comparison of Success rates in Group I &Group II
| S. No | Surgery | Success | Failure | Total |
|---|---|---|---|---|
| 1 | Group I | 275 (91.6%) | 25 (8.33%) | 300 |
| 2 | Group II | 281 (93.6%) | 19 (6.33%) | 300 |
| 3 | Both I + II | 556 (92.6%) | 44 (7.33%) | 600 |
The above table shows that the success rate of Endonasal DCR (93.6%) was higher than External DCR (91.6%). Success was defined by the presence of patent lacrimal passage by lacrimal sac syringing at the end of 6 months followup. Failure rate was higher in External DCR (8.33%) than Endonasal DCR (6.33%).
Discussion
External DCR surgery was regarded as the gold standard in treatment for nasolacrimal duct obstruction. This procedure has got advantages of direct visualization of the anatomical structures surrounding the lacrimal sac compared to endoscopic DCR. Disadvantages of this procedure includes cutaneous scar and the potential for injury to medical canthal structures, cerebrospinal fluid rhinorrhoea and functional interference with the physiological action of lacrimal pump. However, endoscopic DCR is getting popularity among patients due to equal promising results and especially due to lack of external scar [2]. Endoscopic DCR allows direct inspection of lacrimal sac for underlying pathology. Assessment of failure can also be viewed endoscopically, so mistakes can be corrected immediately. Again it can be converted to external DCR in difficult cases or those with lacrimal sac tumours.
In our study of total 600 patients, the maximum number of patients, 245 (40.83%) belonged to 51–60 years age group, minimum number, 35 (5.83%) belonged to 20–30 years age group. Female preponderance was observed in our study with 340 (56.66%) as compared to 260 (43.33%) in male population. This result corroborates with previous studies [3–5].
Right side was the dominant affected side affected 405 (67.5%); whereas on 195 (32.5%) were having disease on left side. This does not correlate with previous studies [5, 6]. However Nichlani et al., found right eye involvement more than left eye, which corroborates with our study [7]. Epiphora was the most common clinical symptom in Both groups I (60%) & Group II(65%)which corresponds to previous studies [4, 7].
Intra operative complication rate was less in case of Endonasal DCR (23.33%) as compared to External DCR (38.33%) This can be explained by better &wide lacrimal sac exposure, less bleeding & crusting and ability to concurrently address nasal mucosa as compared to external approach [8].
The incidence rate of post operative complication was lower in EN- DCR than in EX- DCR.
Debate continues regarding EX-DCR versus EN-DCR. Our current study directly compares the success rate of two distinct techniques with different utilization of the nasal or lacrimal mucosa in endoscopic DCR for NLD obstruction. We have found that maximizing coverage of any bare-bone by utilizing the double-flap technique where two mucosal flaps, one nasal and one lacrimal, are created and used has a clear benefit.
Several points of strength in our study can be mentioned including a standardized diagnostic approach for detection of NLD patency or obstruction including objective (by probing and irrigation) and subjective (symptoms including epiphora) methods, standardized surgeon, surgical settings, and techniques in endoscopic DCR, extended follow up for the patients of at least 6 months after surgery to detect any recurrence of the condition and a reasonably high number of cases in our cohorts.
In our study, the overall success rate of DCR for PANLDO was 92.6%, which was similar to previous reports in the literature. There was difference in terms of anatomical or functional success rate between EN-DCR (93.6%) and EX-DCR (91.6%). The incidence rate of post operative complication in our study was lower in Endonasal DCR (27.33%) as compared to External DCR (48%).
Previous Studies
| S.No | Author | External DCR (success rate) (%) | Endonasal DCR (success rate) (%) |
|---|---|---|---|
| 1 | Cokkesser et al. [9] | 89.8 | 88.2 |
| 2 | Dolman et al. [13] | 90.2% | 89.1 |
| 3 | Tsirbas et al. [14] | 100 | 93.5 |
| 4 | Simon et al.[15] | 70 | 84 |
| 5 | Sharma [16] | 90.5 | 88.5 |
| 6 | Goyal et al. [19] | 95 | 90 |
| 7 | Karim et al. [17] | 82.4 | 81.6 |
| 8 | Walker et al. [10] | 89.8 | 90.2% |
| 9 | Saha et al. [17] | 96.7 | 90 |
| 10 | Huang et al. [18] | 87 | 77 |
| 11 | Present study | 91.6 | 93.6 |
The reported success rate of EN-DCR in the literature ranges from 77 to 93.5% and EX-DCR from 70 to 100% [9–18]
Studies for comparison of surgical outcomes of two approaches had been conducted and the results varied in the literature. There is still no consensus that which procedure is superior to the other. Lacking of standardized outcome measurements, variable surgical techniques, nonrandomized case selection, experience of the surgeon may all contribute to the variable reported outcomes.
The decision of surgical approach, through either external or endoscopic routs, for DCR often reflects the surgeon's training background. Ophthalmologist is familiar with the surgical incision through medial canthal area, while otorhinolaryngologist favors the transnasal endoscopic view to approach the lacrimal sac. With the increasing collaboration between these specialties,the practice pattern changes.
A study by Gauba V [19] comparing EN-DCR to EX-DCR suggested that both procedures have high success rate and equivalent low risk of complications. However, absence of skin scar and quicker recovery time led to significant higher patient satisfaction for those who underwent EN-DCR.
Although surgical success was comparable between two groups at final visit in our study, time to relief of symptoms after the surgery was statistical significantly shorter in EN-DCR compare to EX-DCR (1.7 vs. 3.7 weeks). We also observed few cases with transient lagophthalmos, which mostly resolved in 1-month postoperatively, that resulted in prolonged tearing despite anatomical patency in EX-DCR. That might result from disruption of medial canthal tendon along with orbicularis muscle and superficial branches of facial nerve that interfered the lacrimal pumping function by external skin incision. With the convincing data that supported in our study, we believe it is worthwhile to shift EX-DCR to EN-DCR for patients’ own good.
Intranasal endoscopic findings of these patients included cicatricial closure of the ostium, adhesion of the nasal mucosa involving the middle turbinate or nasal septum, granulation tissue obscured the ostium, or membrane obstructing common canalicular opening. In a review of 100 revision DCRs performed in India, Dave et al.[20]. found most common causes of surgical failure included inadequate osteotomy, inappropriate sac marsupialization, and cicatricial closure.
Here, we would like to emphasize the importance of intranasal endoscopic examination during follow-up period since it is helpful for understanding the wound healing process, periodic cleaning of debris from osteotomy site and improving surgical outcomes. Endonasal DCR offers several possible advantages over external DCR. It theoretically does not interfere with lacrimal pump function as an external incision might, and cosmesis is better because there is no external scar. Some surgeons claim that the operative time and the postoperative recovery period are shorter using endoscopic techniques as soon as the learning curve has plateaued. Furthermore, an endoscopic DCR is a viable option in the setting of active dacryocystitis or in the presence of a lacrimal sac abscess.
The drawbacks of the EN-DCR include high cost of the instrument, steep learning curve of the endoscope technique for ophthalmologist, and difficulty of lacrimal sac-nasal mucosal flaps suturing and manipulation.
Conclusions
Both EX-DCR and mechanical EN-DCR surgeries for the treatment of PANLDO in our study revealed high success rate and low risk of complications. However, patients underwent EN-DCR had shorter recovery time, less complications and higher satisfaction due to lack of external incision, although final surgical outcomes were comparable between two groups. Ophthalmologists should definitely find ourselves a role in endoscopic lacrimal surgery and consider EN-DCR as primary treatment of choice for PANLDO.
Acknowledgements
We are highly thankful to our Dean Dr. Somvanshi for allowing us to conduct this study and provided us necessary support for the same. We are also very thankful to our staff for necessary technical support to conduct the study. Finally, we express deep appreciation to the patients who willing provided us information utilized in the study.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflicts of interest, and it was a non-funded project.
Ethical Approval
Ethical approval was obtained from institutional research committee(PDMMC) regarding involvement of human participants, wherein they were explained about risk involved and procedure details.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wormald PJ. Powered endoscopic dacryocystorhinostomy. Laryngoscope. 2002;112:69–72. doi: 10.1097/00005537-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Durvasula VSP, Gatland GJ. Endoscopic dacryocystorhinostomy: long term results and evolution of surgical technique. J Laryngol Otol. 2004;118:628–632. doi: 10.1258/0022215041917835. [DOI] [PubMed] [Google Scholar]
- 3.Hurwitz JJ, Rutherford S. Computerized survey of lacrimal surgery patients. Ophthalmology. 1986;93:14–19. doi: 10.1016/S0161-6420(86)33779-5. [DOI] [PubMed] [Google Scholar]
- 4.Tan NC, Rajapaksa SP, Gaynor J, Nair SB. Mechanical endonasal dacryocystorhinostomy-a reproducible technique. Rhinology. 2009;47:310–315. doi: 10.4193/Rhin08.150. [DOI] [PubMed] [Google Scholar]
- 5.Moras K, Bhat M, Shreyas CS, Mendonca N, Pinto G. External dacryocystorhinostomy versus endoscopic dacryocystorhinostomy: a comparison. J Clin Diagn Res. 2011;5:182–186. [Google Scholar]
- 6.Vishwakarma R, Singh N, Ghosh R. A study of 272 cases of endoscopic dacryocystorhinostomy. Indian J Otolaryngol Head Neck Surg. 2004;56:259–261. doi: 10.1007/BF02974382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nichlani SS, Jagade MV, Ganeshan A. A comparative study between endoscopic and external approach dacryocystorhinostomy. Bombay Hosp J. 2010;52:189–96. [Google Scholar]
- 8.Lee DW, Chai CH, Loon SC. Primary external dacryocystorhinostomy versus primary endonasal dacryocystorhinostomy: a review. Clin Exper Ophthalmol. 2010;38(4):418–426. doi: 10.1111/j.1442-9071.2010.02254.x. [DOI] [PubMed] [Google Scholar]
- 9.Cokkesser Y, Evereklioglu C, Er H. Comparative external versus endoscopic dacryocystorhinostomy: results of 115 patients. Otolaryngol Head Neck Surg. 2000;13:488–491. doi: 10.1067/mhn.2000.105470. [DOI] [PubMed] [Google Scholar]
- 10.Walker RA, Al-Ghoul A, Conlon MR. Comparison of nonlaser nonendoscopic endonasal dacryocystorhinostomy with external dacryocystorhinostomy. Can J Ophthalmol. 2011;46(2):191–195. doi: 10.3129/i10-096. [DOI] [PubMed] [Google Scholar]
- 11.Huang J, Malek J, Chin D. Richard harvey; systematic review and meta-analysis on outcomes for endoscopic versus external dacryocystorhinostomy. Orbit. 2014;33(2):81–90. doi: 10.3109/01676830.2013.842253. [DOI] [PubMed] [Google Scholar]
- 12.Dolman PJ. Comparison of external dacryocystorhinostomy with nonlaser endonasal dacryocystorhinostomy. Opthalmology. 2003;110:78–84. doi: 10.1016/S0161-6420(02)01452-5. [DOI] [PubMed] [Google Scholar]
- 13.Tsirbas A, Wormald PJ. Mechanical endonasal dacryocystorhinostomy with mucosal flaps. Br J Ophthalmol. 2003;87:43–47. doi: 10.1136/bjo.87.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ben Simon GJ, Joseph J, Lee S, Schwarcz RM, McCann JD, Goldberg RA. External versus endoscopic dacryocystorhinostomy for acquired nasolacrimal duct obstruction in a tertiary referral center. Ophthalmology. 2005;112:1463–1468. doi: 10.1016/j.ophtha.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 15.Sharma BR. Non endoscopic endonasal dacryocystorhinostomy versus external Dacryocystorhinostomy. Kathmandu Univ Med J. 2008;6(24):437–442. doi: 10.3126/kumj.v6i4.1731. [DOI] [PubMed] [Google Scholar]
- 16.Karim R, Ghabrial R, Lynch TF, Tang B. A comparison of external and endoscopic endonasal dacryocystorhinostomy for acquired nasolacrimal duct obstruction. Clin Ophthalmol. 2011;5:979–989. doi: 10.2147/OPTH.S19455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saha R, Sinha A, Phukan JP. Endoscopic versus external approach dacryocystorhinostomy: A comparative analysis. Nigerian Med J. 2013;54(3):165–169. doi: 10.4103/0300-1652.114580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goyal R, Gupta S. Analysis of 104 cases of endonasal dacryocystorhinostomy in a tertiary care hospital: a prospective study. Indian J Otolaryngol Head Neck Surg. 2014;66(1):102–105. doi: 10.1007/s12070-013-0693-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gauba V. External versus endonasal dacryocystorhinostomy in a specialized lacrimal surgery center. Saudi J Ophthalmol. 2014;28(1):36–39. doi: 10.1016/j.sjopt.2013.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dave TV, Mohammed FA, Ali MJ, Naik MN. Etiologic analysis of 100 anatomically failed dacryocystorhinostomies. Clin Ophthalmol. 2016;10:1419–1422. doi: 10.2147/OPTH.S113733. [DOI] [PMC free article] [PubMed] [Google Scholar]




