Abstract
A laryngoscopically benign lesion with minimal hoarseness may turn out to be mimickers of malignancy or malignancy itself. Histopathological study is mandatory in such cases to rule out malignancy. A descriptive study of histopathological and laryngoscopic findings of benign laryngeal lesions were studies over a period of 4.5 years. Among the thirty-six patients studied, the mean age of the patients was 42 years. The most common presenting complaint was hoarseness of voice seen in 87.5% of cases. Twelve cases of vocal cord polyps were diagnosed based on clinical, laryngoscopical and histopathological features. Seven cases of vocal cord nodules, presenting with hoarseness of voice and laryngoscopic finding of a small nodular growth over the cord. Nine cases of laryngeal papillomas and papillomatosis showed branching papillae, lined by squamous epithelium with fibrovascular cores. A single case of amyloidosis and four cases of granulomatous lesions suggestive of tuberculosis were studied. One case each of rhabdomyoma and granular cell tumour was reported and confirmed by immunohistochemistry. Rare benign tumours and tumour-like lesions mimicking malignancy on laryngoscopy need histopathological evaluation. It is mandatory to study excised biopsies of the larynx as grossly similar lesions can vary from non-neoplastic to frankly malignant.
Keywords: Benign neoplasms, Papillomatosis, Amyloidosis, Laryngeal tuberculosis
Introduction
Lesions of larynx like benign tumours and tumour-like lesions show significant association with phonation, especially in singers, actors and teachers that can lead to a lot of mental and emotional turmoil in the patients and their families. These lesions may present with a variety of symptoms ranging from minimal hoarseness of voice to life-threatening stridor [1]. Accurate diagnosis is important for effective management and good recovery.
Moreover, a laryngoscopically benign lesion with minimal hoarseness may turn out to be mimickers of malignancy or malignancy itself. Hence, a microlaryngeal surgery followed by histopathological study is mandatory. It is therefore emphasized that the true nature of any laryngeal lesion should be determined by microscopy. Our study aims to discuss the histomorphology of benign tumours and tumour-like lesions of larynx among the population of coastal Karnataka.
Methods
A descriptive study was conducted in the Department of Pathology over a period of 4.5 years, i.e. 2 years prospectively (July 2014 to June 2016) and 2.5 years retrospectively (January 2012 to June 2014). Thirty-six cases of laryngeal lesions were studied. All surgical pathology specimens of laryngeal benign tumours and tumour-like lesions received for diagnostic purposes were included. However, post-surgery, chemotherapy, radiotherapy and blind mucosal biopsies sent to rule out malignancies were excluded from the study. Detailed clinical history and laryngoscopy findings were recorded. Immunohistochemistry (IHC) was done in all ambiguous cases using antigen retrieval method.
Results
Among the thirty-six patients studied, the mean age of the patients was 42 years with a standard deviation of 17. The male to female ratio was 1.77:1. The most common presenting complaint was hoarseness of voice seen in 87.5% of cases. Majority of patients (44.4%) presented within the first month of onset of symptoms. The history of smoking and alcohol was noted in 39.6% and 25% of the cases respectively.
The laryngoscopic appearance of vocal polyps was smooth, polypoidal and that of vocal nodules was smooth and nodular. Exophytic appearance was seen in all the cases of papillomas and papillomatosis. In many other lesions which were polypoidal or nodular on laryngoscopy, the histopathological diagnosis was discordant, as in granulomatous lesions and some of the benign tumours. The histopathological diagnosis obtained is as shown in Fig. 1 and Table 1.
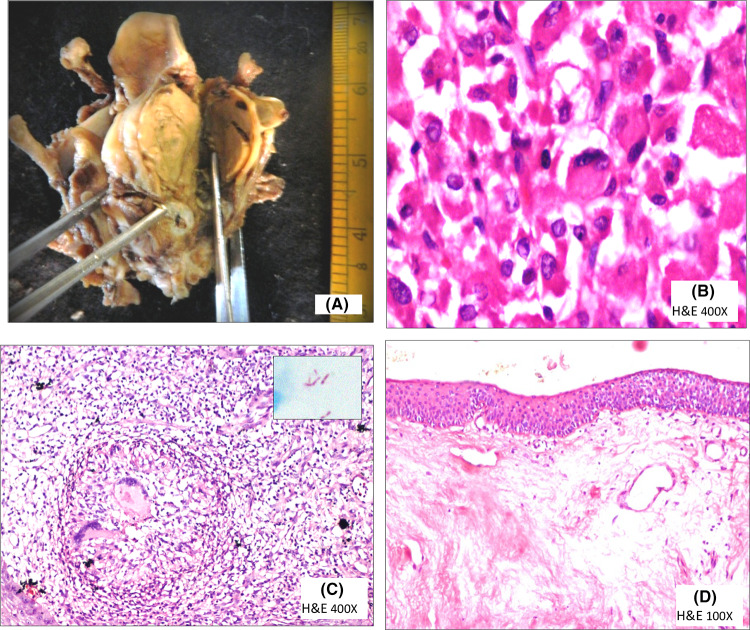
Fig. 1.
a Gross photograph of rhabdomyoma that caused surgical intervention, cut surface is pale pink. b Large polygonal cells with abundant pale pink cytoplasm and vesicular to hyperchromatic nuclei. c Granulomatous lesion with Langhan’s giant cells, inset shows Mycobacterium tubercle bacilli. d Homogenous granular pink amyloid material
Table 1.
Types and frequency of different benign lesions and their comparisons with other studies
| Singh et al. [5] | Hegde et al. [2] | Singhal et al. [3] | Present study (%) | |
|---|---|---|---|---|
| VC polyp | 40.7% | 40.47% | 66% | 33.3 |
| VC nodule | 28.4% | 28.57% | 16% | 19.4 |
| Papillomas and papillomatosis | 22.2% | – | 4% | 22.2 |
| Laryngeal tuberculosis | – | 14.3% | – | 11.1 |
| Amyloidosis | – | – | – | 2.7 |
| Rhadbdomyoma | – | – | – | 2.7 |
| Fibromyxoma | – | – | – | 2.7 |
| Granular cell tumor | – | – | – | 2.7 |
| Others | 8.7% | 16.6% | 14% | 2.7 |
Twelve cases of vocal cord (VC) polyps were diagnosed based on clinical, laryngoscopical and histopathological features. The patients presented with complaints of hoarseness. Laryngoscopy correlated with histopathological diagnosis of VC polyps in all but one, which was clinically diagnosed as a VC cyst. Microscopically, edema in lamina propria and telangiectasia were detected in all the cases. Epithelial appearance varied from normal to atrophic to hyperplastic and hyperkeratotic. The basement membrane showed a variable amount of inflammation and fibrosis.
The present study showed seven cases of VC nodules, presenting with hoarseness of voice and laryngoscopic finding of a small nodular growth over the cord. Hyperplasia of lining epithelium, basement membrane thickening (highlighted by PAS), fibrosis in lamina propria and mild angiectasia were observed consistently in all the cases.
Nine cases of laryngeal papillomas and papillomatosis showing single to multiple branching papillae, lined by squamous epithelium with fibrovascular cores were observed. A single case of amyloidosis and four cases of granulomatous lesions suggestive of tuberculosis were observed. One case each of rhabdomyoma and granular cell tumour was reported and confirmed by IHC.
Discussion
The present study includes thirty-six cases of benign lesions of larynx studied with respect to various clinical and histopathological factors. Maximum cases in our study were seen in the age group of 31–40 years, which is similar to other studies [2–4]. Males outnumbered females in our study. This was on par with other studies [2–6]. The predominant presenting complaint was hoarseness of voice, which is in concordance with studies by Singhal et al. [3] and Wani et al. [7] (Table 2).
Table 2.
Comparison of presenting symptoms in benign laryngeal lesions
In our study, maximum cases presented within the first month of onset of symptoms (44.4%) in contrast to Hegde et al. [2] who reported very few cases presenting during the first month. Though both the studies were carried out in the same institution, the discordance may be due to better awareness during the interval of more than a decade between the two studies. It may also be attributed to a higher number of cases (9 cases) of papillomatosis and papillomas with an intrinsic tendency of fast growth and early onset of symptoms, while Hegde et al. [2] did not have any of these lesions.
The history of smoking and alcohol abuse was found in 38% and 25% respectively in benign lesions in our study. Wani et al. [7] reported similar findings and found 47% of patients with a history of smoking and 7% with alcohol abuse.
Vocal nodules and polyps are characteristically associated with certain occupations related to voice abuse, e.g. singers, teachers, bus conductors, actors and others. In a study by Singhal et al. [3]. These lesions were most frequently seen in both non-professional and professional voice abusers, including housewives (24%), teachers and salesmen (16% each), bus conductors and politicians (5%). Another study by Sharma et al. [4] showed occurrence in labourers (25%), businessmen and housewives (20% each). Similarly, in the present study, these lesions were found in vocal abusers, in the form of hawking. Maximum cases were found in housewives (25%). Teachers, businessmen, students and drama artists constituted a small percentage.
The commonest lesions were polyps (33.3%) and VC nodules (19.4%). Similar findings were observed by Singh et al. [5] and Hegde et al. [2]. However, Singhal et al. [3] reported a higher incidence of VC polyps in their study (66%). Papilloma and papillomatosis constituted 22.2% cases in our study, which was same as that reported by Singh et al. [5]. Laryngeal tuberculosis was encountered in 11.1% cases, which was in concordance with the study by Hegde et al. [2]. In addition, we also identified certain rare benign lesions like rhabdomyoma, fibromyxoma and granular cell tumour of the larynx.
Telangiectasia is the most characteristic feature of VC polyps [8]. Martins et al. [9] reported similar histological features in VC polyps as reported in our study, i.e. increased number of capillaries in lamina propria, edema, variable pithelial hyperplasia and inflammation. Nunes et al. [10] studied the histopathology of VC polyps in detail to point out the differences between this clinical entity and VC nodules. VC polyps were found to have edematous lamina propria and vascular changes like marked angiectasia, which was in corroboration with the present study.
The histological features for VC nodules are epithelial hyperplasia, fibrosis of lamina propria and basement membrane thickening, seen in 73.33%, 93.33% and 86.66% cases respectively by Martins et al. [9, 10]. All our cases showed similar features.
Nine cases of laryngeal papillomas and papillomatosis were observed, of which three were in patients less than 10 years old and all showed exophytic appearance on laryngoscopy. The early age at presentation of papillomatosis and exophytic appearance has also been reported by Martins et al. [9] and Malick et al. [11]. However, the age group of papillomas varied between 20 and 50 years in our study. These are described as adult-onset papillomas [12]. The symptoms are more serious and require immediate treatment in children because of the narrow diameter of airways [11]. The gross appearance ranges from white to red in colour, 1–10 mm in diameter with friable and polypoidal structures. Microscopically, papillae with fibrovascular cores are seen. Koilocytic change is frequently seen in laryngeal papillomatosis and is correlated with HPV infection [9]. This change was seen in 66.6% of our cases.
Amyloidosis is an uncommon, slowly progressive disease contributing to 0.2 to 1.5% of benign laryngeal tumours [13, 14]. In the present study as well, there is a single case of amyloidosis in a 53-year-old female. Indirect laryngoscopy showed a smooth mucosa covered nodule on the left false cord. Biopsy showed amorphous homogenous eosinophilic material in the subepithelium suggestive of amyloid that was confirmed by Congo red staining. Deviprasad et al. [13] who studied five cases of laryngeal amyloidosis, obtained similar findings.
Rhabdomyomas are rare benign mesenchymal tumours. Tumours arising in the head and neck usually originate from the musculature of the pharynx, oral cavity or larynx. Fewer than 200 extra cardiac rhabdomyomas have been reported. The median age at presentation is 60 years with a male predominance (3:1) [15]. Tumours can present as a mass in the upper aerodigestive tract with airway obstruction or as a soft tissue mass. Larynx is the third most common mucosal site after oral cavity and pharynx. Rhabdomyoma is usually solitary but may be multinodular (25%). Grossly, it appears as tan to yellow–brown, circumscribed, lobulated soft or fleshy nodules (Fig. 1). Rhabdomyoma was reported in a 50-year-old non-smoker male. Microscopically, the tumour cells were round to polygonal with abundant eosinophilic granular cytoplasm (spider cells) and peripherally placed vesicular nuclei, arranged in sheets and vaguely nested pattern. Intranuclear cytoplasmic inclusions were present. The tumour cells were positive for desmin, vimentin and focally for SMA and negative for chromogranin, synaptophysin and S-100. PTAH showed cross striations. Hence, the use of IHC is essential for accurate diagnosis in these tumours.
Granular Cell Tumour (GCT) is an uncommon benign laryngeal neoplasm first described by Abrikossoff in 1926 as myoblastoma. Fifty per cent of the GCTs occur in the head and neck regions, most commonly in the tongue. The mean age is 34 years with a female preponderance. Grossly, these tumours are well-circumscribed, small, rounded, firm, sessile mucosal covered masses that grow slowly and often resemble vocal fold polyps or granuloma. The microscopy is characterized by sheets of large, round to polygonal cells with abundant granular eosinophilic cytoplasm. These cells are positive for S-100 protein, vimentin, neuron-specific enolase, myelin-associated glycoprotein (antibody Leu-7), and CD68 (KP-1) but negative for keratin, desmin, myoglobin, and muscle-specific actin. A case of GCT was reported in a 27 years old male in our study with similar findings and was confirmed by S-100 positivity in the tumour cells.
Conclusion
The present study highlights the histomorphology of benign lesions of larynx and closely related lesions like VC nodules and VC polyps. Rare benign tumours and tumour-like lesions mimicking malignancy on laryngoscopy need histopathological evaluation. It is mandatory to study all excised biopsies of the larynx as grossly similar lesions can vary from non-neoplastic to frankly malignant. Also, verrucous lesions like papillomas could be differentiated from their malignant counterparts, thus altering the surgical management.
Author’s Contribution
HS, MN: conception of work; HS, MN: design of the work; HS, MN, SS, FDL, RP, SS: the acquisition of data and analysis; HS, MN, NP, SS: interpretation of data; HS, MN, NP: the creation of new software used in the work; MN, NP, SS: have drafted the work or substantively revised it; HS, MN, NP, SS, FDL, RP, SS: approved the submitted version; HS, MN, NP, SS, FDL, RP, SS: agreed to be personally accountable.
Funding
None.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for Publication
Obtained from the institution Kasturba Medical College, Mangalore.
Ethical Approval
Permission obtained from the institutional Ethics committee of Kasturba Medical College, Mangalore (IEC KMC MLR 01-14/22).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Armstrong WB, Netterville JL. Anatomy of the larynx, trachea, and bronchi. Otolaryngol Clin N Am. 1995;28:685–699. doi: 10.1016/S0030-6665(20)30488-6. [DOI] [PubMed] [Google Scholar]
- 2.Hegde MC, Kamath MP, Bhojwani K, Peter R, Babu PR. Benign lesions of larynx—a clinical study. Indian J Otolaryngol Head Neck Surg. 2005;57:35–38. doi: 10.1007/BF02907624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singhal P, Bhandari A, Chouhan M, Sharma MP, Sharma S. Benign tumours of the larynx: a clinical study of 50 cases. Indian J Otolaryngol Head Neck Surg. 2009;61:26–30. doi: 10.1007/s12070-009-0013-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma DK, Sohal BS, Bal MS, Aggarwal S. Clinico-pathological study of 50 cases of tumours of larynx. IJO & HNS. 2013;65:29–35. doi: 10.1007/s12070-011-0420-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh M, Bandyopadhyay S, Gupta SC, Rai A. Benign laryngeal lesions—a clinicopathological study of eleven years andacasereportofpleomorphiclipoma. Indian J Otolaryngol Head Neck Surg. 2002;54(3):242–245. doi: 10.1007/BF02993115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El Lackany M, Shalaby AMR. The frequency of laryngeal cancer among different laryngeal swellings in adult patients. JMRI. 2005;26:350–355. [Google Scholar]
- 7.Wani AA, Rehman A, Hamid S, Akhter M, Baseena S. Benign mucosal fold lesion as a cause of hoarseness of voice—a clinical study. Otolaryngology. 2012;2:120. [Google Scholar]
- 8.Wallis L, Jackson-Menaldi C, Holland W, Giraldo A. Vocal fold nodule vs. vocal fold polyp: answer from surgical pathologist and voice pathologist point of view. J Voice. 2004;18:125–129. doi: 10.1016/j.jvoice.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Martins RH, Dias NH, Gregório EA, Marques MA, Silva MG, Candeias JM. Laryngeal papillomatosis: morphological study by light and electron microscopy of the HPV-6. Braz J Otorhinolaryngol. 2008;74:539–543. doi: 10.1016/S1808-8694(15)30600-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nunes RB, Behlau M, Nunes MB, Paulino JG. Clinical diagnosis and histological analysis of vocal nodules and polyps. BJORL. 2013;79:434–440. doi: 10.5935/1808-8694.20130078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malick N, Cheikh NI, Arnaud IOF, Abdourahnane T, Karim DB. Laryngeal papillomatosis in children. ORL. 2008;94:379–381. [Google Scholar]
- 12.Wenig BM. Neoplasms of the larynx, hypopharynx and trachea. In: Wenig BM, editor. Atlas of head and neck pathology. 2. Philadelphia, PA: WB Saunders-Elsevier; 2008. pp. 448–453. [Google Scholar]
- 13.Deviprasad D, Pujary K, Balakrishnan R, Nayak DR. KTP laser in laryngeal amyloidosis: five cases with review of literature. Indian J Otolaryngol Head Neck Surg. 2013;65:36–41. doi: 10.1007/s12070-011-0435-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dabholkar JP, More M, Avanindra K, Sharma A. Primary exophytic laryngeal amyloidosis presenting as sudden airway obstruction. Indian J Otolaryngol Head Neck Surg. 2007;59:357–359. doi: 10.1007/s12070-007-0101-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gensler MSB, Mahadevia P, Gnepp DR. Nonsquamous pathological diseases of the hypopharynx, larynx and trachea. In: Gnepp DR, editor. Diagnostic surgical pathology of head and neck. 2. Amsterdam: Elseiver; 2009. pp. 381–383. [Google Scholar]