Abstract
Introductions
Interpolated flaps remain the mainstay of nasal reconstruction. In this regard Paramedian forehead flap has been combined and modified variously by different surgeons. However, still multiple stages are required to give shape to the nose and ensure that skin and cartilaginous vault of nose are aesthetically and functionally reconstructed. However, we describe a technique in which cartilage is reconstructed at the same stage as harvesting the flap without risk of vascular compromise.
Materials and Methods
We describe a retrospective chart review of reconstructive nasal procedure in 2 stages with reconstruction in the first sitting itself using Paramedian forehead flap and ipsilateral septal perichrondium and septal cartilage in 4 patients of lower nasal vault deficiency between Jan 2018 to Dec 2018. The patients age ranged from 10 to 67 Years. 2 of the patients needed surgery due to dog bite injury 1 due to excision of basal cell carcinoma and another due to road traffic accident. The technique involved harvesting an ipsilateral paramedian forehead flap along with ipsilateral septal perichondrial flap anteriorly based and using septal cartilage to make the skeleton. The flap was divided after 3 weeks and thinned suitably.
Results
All the patients reported complete uptake of flap without any cartilage necrosis. Functionally none of the patient reported more nasal block than that seen preoperatively. The average NOSE VAS score remained 17.5 reported 1 month after the second stage.
Conclusions
Planning is the key for appropriate and cosmetically feasible nasal con-struction. Emphasis must be given to nasal subunit being reconstructed and the choice of flap must be robust. Our forehead flap uses 2 stage design with septal flap to allow for cartilage reconstruction in situ. We utilized post op small vessel dilators along with BACTIGRAS dressings to prevent infection. Our technique in both cases allowed for a greater nasal airway and greater nasal valve suppor.t
Keywords: Rhinoplasty, Paramedian fore head flap, Septal mucoperichondrial flap, Single stage
Introduction
Nasal reconstruction is a complex surgery which requires reconstructive skills on the part of surgeon and needs a staged approach. Para median forehead flap is a versatile flap for lining the external nasal vault. Though reliably folded forehead flap offers good result for lining of nose. However, it does not alone allow for use of cartilaginous graft which is necessary for maintain the patency of nasal valve. The cartilage graft causes the blood supply to be supplemented by a different flap. In nose septal perichondrial flap provides an apt flap for this situation. ENT surgeons who are well versed with septal surgeries can raise the flap easily to provide support to the cartilage and better cosmesis.
Material and Methods
The study describes a retrospective chart review between Jan 2018 to Dec 2018 of 4 cases of paramedian forehead flap with septal perichondrial flap done at a rural higher medical centre in west Gujarat (Table 1). The patients included 3 male patients and one female patient. The average age of patients ranged from 10 years of age to 67 years of age. The primary indication for the flap in 1 case was basal cell carcinoma (Fig. 1A) and in another 2 dog bite (Fig. 2A) and in 1 case was trauma due to road traffic accident. The defect in all cases involved the ala, tip, lobule and soft triangle and the dorsum partially. In all cases the defect was full thickness with loss of alar cartilages (Tables 1 and 2).
Table 1.
Patient characteristics
| S. No | Age | Gender | Associated co morbidities | Units involved as per menick and burgets classification | Defect size |
|---|---|---|---|---|---|
| 1 | 67 | Female | Diabetes | Dorsum + Right lateral + Tip + Alar Lobule | 3 cm * 3.5 cm |
| 2 | 57 | Male | Tobacco Chewer and Bidi Smoker | Dorsum + Left lateral + Tip + Alar lobule + Columella | 3 cm * 3 cm |
| 3 | 35 | Male | None | Dorsum + Right Lateral + Tip + Alar Lobule | 3 cm * 2.5 cm |
| 4 | 10 | Male | None | Dorsum + Right Lateral + Tip + Alar Lobule | 2.5 * 2 cm |
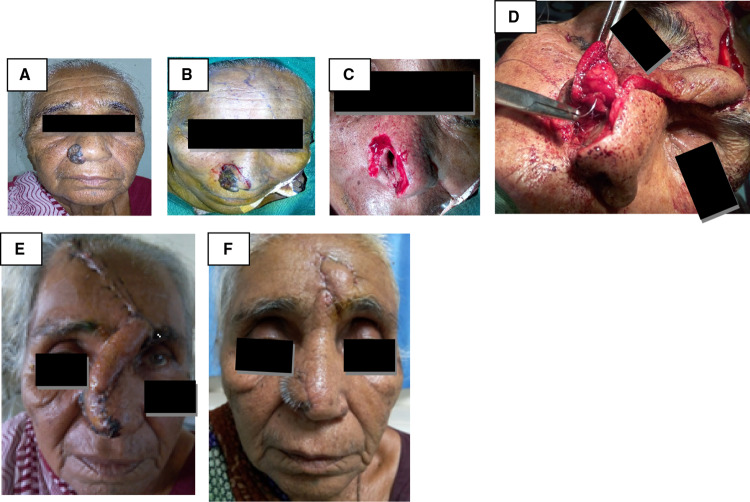
Fig. 1.
A–F Case of Basal Cell Carcinoma reconstructed
Fig. 2.

A–E Case 2 : Dog bite of nose reconstructed
Table 2.
Outcome of paramedian forehead flap and Septal Flap
| SNo | Age | Gender | Outcome of paramedian flap | Outcome of septal flap | ||||
|---|---|---|---|---|---|---|---|---|
| Complete necrosis | Partial necrosis | Healed | Flap necrosis | Septal perforation | Healed | |||
| 1 | 67 | Female | No | No | Yes | No | No | Yes |
| 2 | 57 | Male | No | No | Yes | No | No | Yes |
| 3 | 35 | Male | No | No | Yes | No | No | Yes |
| 4 | 10 | Male | No | No | Yes | No | No | Yes |
Surgical Technique
In the first stage,the paramedian forehead flap was pedicle was identified by preoperative doppler sonography in both the case and the flap was marked between 0.7 cm and 1.2 cm from midline. First the septal flap which was based anteriorly was elevated and rotated and fixed on to remnant nasal ala and cartilaginous vault area using vicryl 3.0 round bodies sutures (Fig. 1D and 2B).
The flap was premarked using a template made from surgical gloves. The flap harvest was started peripherally in the subcutaneous plane and then shifted to sub galeal plane. At about 1 cm from the eye brow line the dissection went into sub periosteal plane to avoid injury to the pedicle. The pedicle was rotated in anticlockwise manner. (Figures 1E and 2C) Post operatively for 1 week patients were maintained on IV antibiotics and pentoxifylline.
After 3 weeks of conservative management the paramedian forehead flap and septal flap were divided at the second stage under local anaesthesia with some thinning of flap.
Results
The procedure was well tolerated by all patients. In 100% of cases (n-4). The paramedian forehead flap and septal flap took up nicely in all patients. (n = 4) and there was no residual septal perforation. Though 2 of the patients were habitual tobacco users no influence was seen on graft survival. The cartilage graft took up completely without any evidence of necrosis in all patients. (Table 3).
Table 3.
Status of cartilage graft
| S. No | Age | Gender | Status of cartilage graft At 3 weeks postop | |||
|---|---|---|---|---|---|---|
| Completely | Pattial epitheliolysis | Incomplete necrosis | Total necrosis | |||
| 1 | 67 | Female | Yes | No | No | No |
| 2 | 57 | Male | Yes | No | No | No |
| 3 | 35 | Male | Yes | No | No | No |
| 4 | 10 | Male | Yes | No | No | No |
Cosmetically, 2 of the patients had some residual hair. (Figures 1F and 2D,E). However, the evaluation of nose rim revealed that in 3 out of 4 patients the nose rim were symmetrical and 1 patient the child the rim which was reconstructed had minimal deformity in the soft triangle which was noted by the surgeon however the same was not considered as troublesome by the parents.
Functionally, the patients reported no increased sensation of nose block after surgery as compared to before. The subjective average mean postoperative NOSE and VAS score remained 17.5 reported a month after the second stage.
Discussion
A detailed analysis of defect is required before planning any treatment. In general shape, size and thickness of defect with respect to nasal subunit involved is assessed critically. A defect size of less than 1.5 cm is amenable to local flap while more than 2 cm will require interpolated/free flaps. Even when the defect is small but if the region involves includes ala or the patients skin is thick sebaceous only skin grafting may not provide the sufficient strength for valve collapse.
There are many options like skin flap and chondrocutaneous cartilaginous auricular grafts when defect size is less than 2 cm. However, when the defect size is more than 2 cm then the options in terms of aesthetic reconstruction require the use of multiple flaps with separate flap for lining and most authors prefer support reconstruction at a later date when the flap has been taken up. However, in resource poor setting where patients may not prefer multiple surgeries this kind of nasal reconstruction may be a challenge.
The common interpolated flaps used for total thickness defect more than 2 cm include the melolabial flap and paramedian forehead flap. The forehead flap has been described since 700 BC in Sushruta Samhita originally has been the workhorse of nasal reconstruction. However the procedure has since evolved and is staged many times to ensure cartilage is put into nose and ensure proper aesthetic reconstruction. Gillies popularized the use of composite chondrocutaneous grafts for structural support and lining [1, 2]. Converse alternatively used a septomucoperichondrial graft as an alternative. [3] Lining defects in full thickness defects may be done depending on size of defect. The convenient options available to ENT surgeons include septal and inferior turbinate. The lining also provides the vascularity needed to maintain the blood supply of cartilage as the cover flap may not provide sufficient vascularity. Inferior turbinate flap advocated by Murakami et al. offers a maximum length of 2.8 cm and width of 1.7 cm for lateral based defects [4].
Keck et al. described two staged reconstruction using forehead and nasolabial flap for cover flap and and support and nasal lining being provided by Chondrocutaneous auricular graft (CCAG) including conchal skin, anterior perichondrium, conchal cartilage, and posterior perichondrium. Their results showed satisfactory results in 18/19 patients however in 1 patient there was complete resorption of chondrocutaneous auricular graft [5]
The paramedian forehead flap remains the workhorse of nasal reconstruction. There have been many modifications. Menick modified Millard’s design and made the pedicle thinner and therefore giving its versatility [6]. In his paper has outlined the indications for a two stage versus three stage flap design. Menick [7] popularized a three-stage forehead flap approach and others have employed this technique as well with their own modifications [8–10] Quetz and Ambrosch [9] described their 6-year experience using a three-stage approach in which the first stage involves septal and and internal lining reconstruction with a septal pivotal flap and external cover reconstruction with a full thickness paramedian forehead flap. Their second stage involves re-elevation of the forehead flap, subsequent thinning of all layers, and cartilage reconstruction of the nasal framework. The third and final stage involves pedicle division and inset in addition to any minor surgical corrections.
Single stage forehead flap technique has been advocated by Park [11], Fudem [12], Kishi [13] avoid external pedicle and related complications. Basically, the technique involves de epithelialising the pedicle and transferring it as single stage island forehead flap by burying below the procerus muscle after preparing the lining and the cartilaginous skeleton of nose. However, these techniques need rigorous patient selection by excluding patients with small vessel disease, collagen vascular diseases, tobacco chewing, diabetes mellitus, hypertension among others. These techniques are however skill intensive as greater chances of vascular compromise are there in case the skin flap becomes too thin, also strict indications result in these techniques not being used as frequently.
More recently, in 2012, Kishi et al. [13] studied the vascular anatomy of the forehead and nasal regions by performing angiography in 10 cadavers. Their study suggested that the supratrochlear artery can limit the rotation of the forehead flap. Consistent with the findings by Reece et al. [14] their imaging demonstrated an extensive collateral network between the supratrochlear, dorsonasal, and angular arteries. Using this data, they designed a single-stage island paramedian forehead flap reconstruction based on angular artery. Their technique involves using a Doppler probe to identify the location of angular and supratrochlear arteries.
The paramedian forehead flap is then raised in a subgaleal plane. Subsequently, the skin is dissected subcutaneously in the region of the subcutaneous pedicled area and the supratrochlear artery is ligated and separated at its base. These authors were able to dissect the pedicle approximately 1.5 cm below the level of the medial canthus. Using this technique based on island paramedian forehead flap, they reported successful results in six patients without any cases of flap necrosis.
Other interpolated flaps include melolabial flap however they cannot be used for debulking and for defects greater than 4 cm2 as pointed out by Baker et al. [15].The flap may be made as an island flap or a superior pedicle based flap. The flap is good for alar defects extending upto tip and sidewalls with the use of cartilage and without the need for debulking. However, the scar on face may not be preferred by many patients. Free flaps have also been used.
Nowadays, most authors are propagating a tailored approach based on age, sex and comorbidities. Yong, Christophel, and Park provide an algorithm for approaching intermediate (1.5–2.5 cm) nasal defects at different subsites based on their study in 315 patients [16]. Similarly, Woodard CR and Park SS review 213 small nasal defects (1.5 cm or less) to demonstrate a variety of flap or graft design by subsites [17]. Fischer presents detailed surgical techniques for the use of the paramedian forehead flap applied to different nasal defects [18].
Conclusion
Planning is the key for appropriate and cosmetically feasible nasal construction. Emphasis must be given to nasal subunit being reconstructed and the choice of flap must be robust. Our forehead flap uses 2 stage design with septal flap to allow for cartilage reconstruction in situ. We utilized post op small vessel dilators along with BACTIGRAS dressings to prevent infection.
Our technique in these 4 cases allowed for a greater nasal airway and greater nasal valve support. We believe that this technique can provide an effective single stage alternative to nasal reconstruction which will offer an increased rate of success even in relatively less skilled hands. It also offers the patient the option of a single stage reconstruction which is highly relevant in a resource poor setting.
Acknowledgements
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Gujarat Adani Institute of Medical Sciences Bhuj approved this study and the approval number is GAIMS/IEC/APPROVAL/1/2019 Date: 26/01/2019
Authors Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Dr.Mohit Sinha, Dr. Narendra Hirani and Dr.Ajeet Khilnani. The first draft of the manuscript was written by Dr. Mohit Sinha and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
None.
Declarations
Conflict of interest
This authors are declare no conflict of interest.
Consent to Participate
Retrospective study only chart review was done so consent to participate is not required.However informed consent was taken from the patients before each procedure and for photograph publication.
Informed Consent
None.
Open Choice
The authors consent for the study to be provided on Open choice platforms.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mohit Sinha, Email: Drmohit1981@yahoo.com.
Narendra Hirani, Email: narendra.hirani@gaims.ac.in.
Ajeet Kumar Khilnani, Email: ajeetkhilnani@gmail.com.
References
- 1.Gillies H. A new free graft applied to reconstruction of the nostril. Br J Surg. 1943;30:305. doi: 10.1002/bjs.18003012004. [DOI] [Google Scholar]
- 2.Gillies HD. Experiences with the tubed pedicle flaps. Surg Gynecol Obstet. 1935;60:291. [Google Scholar]
- 3.Converse JM. Composite graft from septum for nasal reconstruction. Trans Am Cong Plast Surg. 1956;8:281. [Google Scholar]
- 4.Murakami CS, Kriet JD, Ierokomos AP. Nasal reconstruction using the inferior turbinate mucosal flap. Arch Facial Plast Surg. 1999;1(2):97–100. doi: 10.1001/archfaci.1.2.97. [DOI] [PubMed] [Google Scholar]
- 5.Keck T, Lindeman J, Kuhnemann S, et al. Healing of composite chondrocutaneous auricular grafts covered by skin flaps in nasal reconstructive surgery. Laryngoscope. 2003;113:248–253. doi: 10.1097/00005537-200302000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Menick FJ. Aesthetic refinements in use of forehead for nasal reconstruction: the paramedian forehead flap. Clin Plast Surg. 1990;17(4):607–622. doi: 10.1016/S0094-1298(20)30643-X. [DOI] [PubMed] [Google Scholar]
- 7.Menick FJ. A 10-year experience in nasal reconstruction with the three-stage forehead flap. Plast Reconstr Surg. 2002;109:1839–1855. doi: 10.1097/00006534-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Fudem GM, Montilla RD, Vaughn CJ. Single-stage forehead flap in nasal reconstruction. Ann Plast Surg. 2010;64:645–648. doi: 10.1097/SAP.0b013e3181c925fc. [DOI] [PubMed] [Google Scholar]
- 9.Quetz J, Ambrosch P. Total nasal reconstruction: a 6-year experience with the three-stage forehead flap combined with the septal pivot flap. Facial Plast Surg. 2011;27:266–275. doi: 10.1055/s-0031-1275776. [DOI] [PubMed] [Google Scholar]
- 10.Bhrany AD. Complex nasal reconstruction: a case study: reconstruction of fullthickness nasal defect. Facial Plast Surg Clin North Am. 2011;19:183–195. doi: 10.1016/j.fsc.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Oo KK, Park SS. The midline forehead flap in nasal reconstruction. Facial Plast Surg Clin North Am. 2011;19:141–155. doi: 10.1016/j.fsc.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 12.Park SS. The single-stage forehead flap in nasal reconstruction: an alternative with advantages. Arch Facial Plast Surg. 2002;4:32–36. doi: 10.1001/archfaci.4.1.32. [DOI] [PubMed] [Google Scholar]
- 13.Kishi K, Imanishi N, Shimizu Y, et al. Alternative 1-step nasal reconstruction technique. Arch Facial Plast Surg. 2012;14:116–121. doi: 10.1001/archfaci.2011.1402. [DOI] [PubMed] [Google Scholar]
- 14.Reece EM, Schaverien M, Rohrich RJ. The paramedian forehead flap: a dynamic anatomical vascular study verifying safety and clinical implications. Plast Reconstr Surg. 2008;121:1956–1963. doi: 10.1097/PRS.0b013e3181707109. [DOI] [PubMed] [Google Scholar]
- 15.Baker SR. Principles of Nasal Reconstruction. New York, NY: Springer; 2011. Interpolated melolabial flaps: reconstruction of alar and columellar units; pp. 265–306. [Google Scholar]
- 16.Yong JS, Christophel JJ, Park SS. Repair of intermediate-size nasal defects: a working algorithm. JAMA Otolaryngol Head Neck Surg. 2014;140(11):1027–1033. doi: 10.1001/jamaoto.2014.2258. [DOI] [PubMed] [Google Scholar]
- 17.Woodard CR, Park SS. Reconstruction of nasal defects 1.5 cm or smaller. Arch Facial Plast Surg. 2011;13(2):97–102. doi: 10.1001/archfaci.2011.6. [DOI] [PubMed] [Google Scholar]
- 18.Fischer H. Nasal reconstruction with the paramedian forehead flap-details for success. Facial Plast Surg. 2014;30(3):318–331. doi: 10.1055/s-0034-1376918. [DOI] [PubMed] [Google Scholar]