Abstract
Fibrovascular polyps are rare benign epithelial neoplasia of the cervical esophagus. Usually they are large and frequently require a thoracotomy/thoracoscopy. This is a case report of an elderly lady with a large Fibrovascular polyp who had anemia and weight loss due to dysphagia, managed by rendezvous technique.
Keywords: Benign esophageal neoplasm, Fibrovascular polyp, Rendezvous procedure
Introduction
A 67 year old lady was referred to our center with foreign body sensation, grade 2 dysphagia and weight loss of 6 months duration. Four months earlier, she was referred for a thyroidectomy elsewhere, with a clinical diagnosis of iodine deficiency goiter. On presentation to us, she had stridor and orthopnea. She gave history of coughing out a fleshy mass which she could push back, almost an year back. Examination showed an anteriorly placed neck swelling that moved on deglutition.
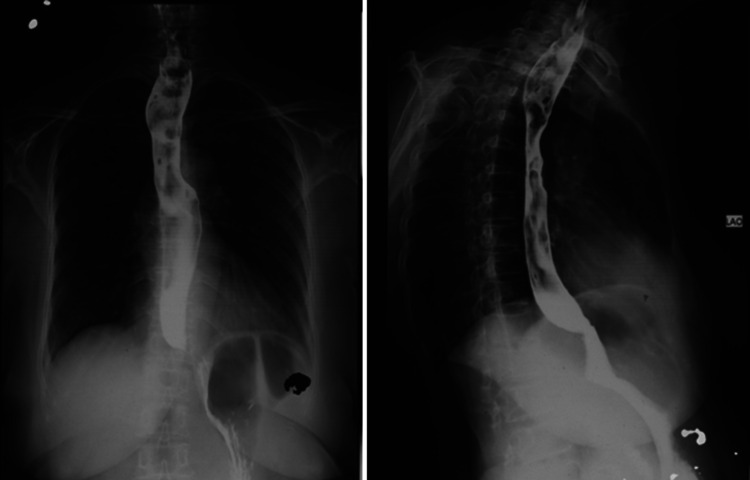
X-ray chest showed widening of the upper mediastinum with a soft tissue density in the tracheoesophageal region. Endoscopy revealed a large polypoidal mass, 20 cm from the incisors with the base not visualized, the overlying mucosa showing ulceration. Barium swallow showed filling defects in the upper esophagus with a smooth mucosa (Fig. 1). Clinical diagnosis of FVP was made and a CECT done for anatomic delineation.
Fig. 1.
Anteroposterior and oblique view of barium swallow showing filling defects
In view of the large size, she was planned for an operative polypectomy rather than an endoscopic approach. Intraoperatively, initially a rigid esophagoscopy was performed by an ENT surgeon under General anesthesia to identify the base of the polyp, which revealed a wide base just below the UES. Under the guidance of intraoperative esophagoscopy, an esophagotomy was done via a left cervical approach. The esophagotomy was extended up to the suprasternal notch as the polyp was large. The large polyp, which was filling the lumen and partly dipping into the thoracic esophagus was delivered out (Fig. 2) and excised at the base. The mucosal defect at the base was approximated with 4–0 polyglactin 910 sutures. Esophagotomy was closed with interrupted absorbable sutures and a drain left in the cervical region. A feeding jejunostomy was also done in the same setting. A water-soluble contrast study on POD 5 showed no extravasation or gross aspiration. Postoperatively initially there was swallowing difficulty, with frequent episodes of microaspirations which gradually settled with small frequent meals. Meanwhile, the feeding jejunostomy (FJ) came to the rescue. Histopathology confirmed the diagnosis of fibrovascular polyp (FVP). At follow up two and a half years later, the patient remains asymptomatic.
Fig. 2.

Polyp delivered via left cervical esophagotomy. Arrow- depicts base of polyp in upper esophagus
Discussion
Among the benign neoplasms of esophagus, barring leiomyomas, most are very rare and their knowledge limited to case reports. FVP is one such rare benign neoplasm, commonly arising from the proximal esophagus. So far only a few hundred of them have been reported [1]. Although benign, the late and occasional dramatic presentation makes it an interesting tumor.
Upper esophagus is the most common area of origin [1], reason being the triangle of Laimer, an area deficient in muscle fibers [2]. Recurrent swallowing, peristaltic movements, and gravitational pull lead to prolapse of the mucosa with subsequent growth of the polyp.
They are usually asymptomatic, until they attain a large size (> 5 cm), giving rise to dysphagia, stridor, globus sensation, weight loss. Rare presentations such as coughing out of polyp and sudden respiratory arrest due to laryngeal obstruction are described in literature. Mucosal ulcerations can present as anemia due to chronic blood loss. Clinically it may mimic a thyroid swelling in the anterior portion of the neck.
Upper GI endoscopy is often sufficient to establish a diagnosis. However, a biopsy is advised to avoid missing any malignancy. Treatment is excision via endoscopic or surgical approach. Excision is usually curative; recurrence is rare unless the excision is incomplete. As the knowledge of FVP is limited to case reports, the natural history is unknown. One case of malignancy in FVP has been reported by Beylergil et al. [3].
The crux lies in complete excision at the base to prevent any recurrence for which multiple approaches and techniques are described. Endoscopic excision is feasible when the polyp hasn’t acquired a very large size, when maneuverability can become difficult. Surgically, it can be approached by a left cervical esophagotomy. Due to the long stalk and size of the polyp, a cervical esophagotomy may not be sufficient to deliver the polyp, which commonly dips into the thoracic esophagus. However, in the current case, we were able to deliver the polyp out, nevertheless, with difficulty. There have been reports where a simultaneous laparotomy or thoracotomy is required for excision [4]. It should be kept in mind that the feeding vessel is at the base, which is usually in the upper 1/3rd of the esophagus. Initial On -table Rigid esophagoscopy helped us to establish the base to be in the cervical oesophagus and make the esophagotomy over the tip of the esophagoscope, right at the base of the polyp. A synchronous primary lesion is rare and when present, it may be a second polyp limb arising from the same base [5]. It can be debated whether it may be justified to perform a piecemeal excision to facilitate excision via cervical approach and avoid the morbidity of a thoracotomy.
Conclusion
FVP is a rare benign epithelial neoplasm of the esophagus. Unless large, the symptoms are subtle and clinical signs may not be contributory. Careful history taking may clinch the diagnosis. However, when discovered, it must be subjected to excision, as it possesses life-threatening complications. Delineating the base of the polyp by On-table esophagoscopy is helpful in siting the esophagotomy accurately, as most often, the base is in the upper esophagus and a thoracotomy may be avoided if the access to the polyp base is optimal.
Acknowledgment
None
Funding
None.
Compliance with Ethical Standards
Conflict of interest
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Caceres M, Steeb G, Wilks SM, Garrett HE. Large pedunculated polyps originating in the esophagus and hypopharynx. Ann Thorac Surg. 2006;81(1):393–396. doi: 10.1016/j.athoracsur.2005.05.106. [DOI] [PubMed] [Google Scholar]
- 2.McLean JN, DelGaudio JM. Endoscopic resection of a giant esophageal polyp: case report and review of the literature. Am J Otolaryngol Head Neck Med Surg. 2007;28(2):115–117. doi: 10.1016/j.amjoto.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 3.Beylergil V, Simmons MZ, Ulaner G, Jurcic J, Hibshoosh H, Carrasquillo JA. FDG PET/CT findings in a rare case of giant fibrovascular polyp of the esophagus harboring atypical lipomatous tumor/well-differentiated liposarcoma. Clin Nucl Med. 2014;39(3):288–291. doi: 10.1097/RLU.0000000000000358. [DOI] [PubMed] [Google Scholar]
- 4.Lee SY, Chan WH, Sivanandan R, Lim DTH, Wong WK. Recurrent giant fibrovascular polyp of the esophagus. World J Gastroenterol. 2009;15(29):3697. doi: 10.3748/wjg.15.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Di Mitri R, Mocciaro F, Lipani M, Corrao S. One-step endoscopic removal of a giant double esophageal fibrovascular polyp. Dig Liver Dis. 2014;46(7):660–662. doi: 10.1016/j.dld.2014.02.008. [DOI] [PubMed] [Google Scholar]