Abstract
LPRD is a common condition in patients attending ENT OPDs. Although esophageal manometry and 24 h pH monitoring is considered the gold standard for diagnosis, it is an expensive and time consuming investigation. Newer clinical scales have been developed for diagnosing LPR such as RSI, RFS, Carlsson-Dent, ReQuest, GerdQ, etc. The objective of the study is to compare RSI with RFS and to establish its effectiveness in diagnosing LPRD among OPD patients. It’s a descriptive cross-sectional study. ENT outpatients with features of LPRD were asked to fill RSI proforma (score ≥ 13 abnormal), after which they were subjected to indirect laryngoscopy to obtain the RFS (score ≥ 7 diagnostic of LPRD). RSI was compared with RFS. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of RSI were noted. Of 165 patients, 53.9% were females. Mean RSI scores in males and females were 11.9 and 11.5 and mean RFS scores were 6.4 and 5.7 respectively. RSI had 79.1% sensitivity and 83.7% specificity in diagnosing LPRD with PPV 76.8%, NPV 85.4% and accuracy 81.8% (Chi square value 64.5, p ≤ 0.01). There was substantial agreement between RSI and RFS (Cohen’s kappa: 0.625, p ≤ 0.0001). RSI is a simple tool to diagnose LPRD which doesn’t mandate invasive procedures such as endoscopy or esophageal manometry. Hence it can be used effectively to diagnose LPRD in ENT outpatients and start the treatment at the earliest.
Keywords: Reflux Symptom Index, RSI, Reflux Finding Score, RFS, Laryngopharyngeal reflux disease
Introduction
Gastroesophageal Reflux Disease (GERD) is a common condition characterized by chronic symptoms or mucosal damage secondary to the abnormal reflux of gastric contents into the oesophagus [1]. When GER affects the laryngopharynx it is called Laryngopharyngeal Reflux Disease (LPRD). LPR is known to be associated with many clinical entities such as chronic laryngitis, chronic dysphonia, laryngotracheal stenosis, head and neck carcinoma, cough, asthma, otitis media, dental caries and erosion, laryngeal papilloma, vocal fold granulomas and ulcers, laryngospasm, recurrent croup, paradoxical vocal fold movement disorder and laryngomalacia [1].
LPR can present with symptoms such as hoarseness of voice, globus, chronic throat clearing, dysphagia, odynophagia, sore throat, excessive throat mucus, halitosis, exacerbation of asthma, heartburn etc. [2, 3]. The main pathophysiology of LPR is lower oesophageal sphincter incompetence causing regurgitation of gastric secretions into the oesophagus, hence the gold standard test for diagnosing LPR is 24-h pH-metry [1]. But it is an expensive and time consuming investigation. Thus there is delay in initiation of appropriate therapy. Therefore there are other newer clinical scales developed for diagnosing LPR such as Reflux Symptom Index [4], Reflux Finding Score [4], Carlsson-Dent [5], ReQuest [6], GerdQ [7], etc. These scales use either clinical symptoms or laryngoscopic findings to diagnose LPR and hence therapy can be initiated at the earliest.
The objective of the study is to compare RSI with RFS and to establish its effectiveness in diagnosing LPRD among OPD patients.
Materials and Methods
This study is a descriptive cross-sectional study conducted in two tertiary care hospitals attached to a medical college. Patients attending ENT OPDs with clinical features of Laryngopharyngeal Reflux Disease (LPRD) such as voice changes, frequent clearing of throat, excess throat mucus, dysphagia, chronic cough, breathing difficulty, globus in throat, heartburn and chest pain were selected for the study. Patients who had organic causes such as rhinitis, sinusitis, pharyngitis, laryngitis, tumorous lesions or patients who are already on treatment for LPRD or patients who refused to give consent were excluded from the study. After obtaining informed consent, they were asked to fill Reflux Symptom Index according to the severity of their illness, after which they were subjected to indirect laryngoscopy to obtain the Reflux Finding Score. RSI was compared with RFS. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of RSI were noted. Microsoft excel is used to compile the data and IBM SPSS software version 21 is used for various statistical analysis.
Reflux Symptom Index (RSI) is a simple questionnaire consisting of nine questions regarding the symptoms of LPRD, where the patient is asked to score from zero to five depending on the severity of the symptom. RSI of > 13 will be considered as abnormal (Table 1).
Table 1.
Reflux Symptom Index [4]
| Within the last month, how did the following problems affect you? | 0 = no problem 5 = severe problem |
|||||
|---|---|---|---|---|---|---|
| 1. Hoarseness or a problem with your voice | 0 | 1 | 2 | 3 | 4 | 5 |
| 2. Clearing your throat | 0 | 1 | 2 | 3 | 4 | 5 |
| 3. Excess throat mucus or postnasal drip | 0 | 1 | 2 | 3 | 4 | 5 |
| 4. Difficulty swallowing food, liquids or pills | 0 | 1 | 2 | 3 | 4 | 5 |
| 5. Coughing after you ate or lying down | 0 | 1 | 2 | 3 | 4 | 5 |
| 6. Breathing difficulties or choking episodes | 0 | 1 | 2 | 3 | 4 | 5 |
| 7. Troublesome or annoying cough | 0 | 1 | 2 | 3 | 4 | 5 |
| 8. Sensation of something sticking in your throat or a lump in your throat | 0 | 1 | 2 | 3 | 4 | 5 |
| 9. Heartburn, chest pain, indigestion, or stomach acid coming up | 0 | 1 | 2 | 3 | 4 | 5 |
Reflux Finding Score is a simple scoring system that points to inflammatory laryngeal signs using indirect laryngoscopy that can be used by Otorhinolaryngologists in OPDs. A score of > 7 is considered as diagnostic of LPRD (Table 2).
Table 2.
Reflux Finding Score [4]
| Subglottic edema |
0 = absent 2 = present |
| Ventricular obliteration |
2 = partial 4 = complete |
| Erythema/hyperemia |
2 = arytenoids only 4 = diffuse |
| Vocal fold edema |
1 = mild 2 = moderate 3 = severe 4 = polypoid |
| Diffuse laryngeal edema |
1 = mild 2 = moderate 3 = severe 4 = obstructing |
| Posterior commissure hypertrophy |
1 = mild 2 = moderate 3 = severe 4 = obstructing |
| Granuloma/granulation |
0 = absent 2 = present |
| Thick endolaryngeal mucus |
0 = absent 2 = present |
Results
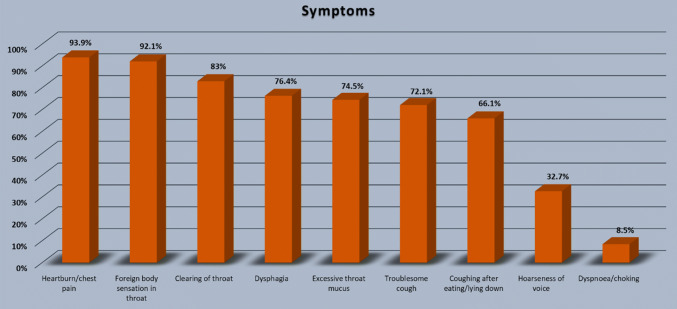
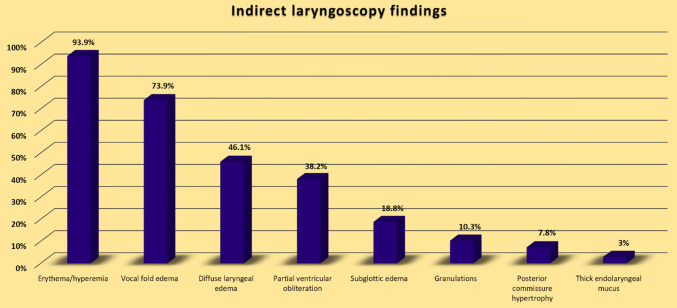
The study consisted of 165 patients of which, 89 (53.9%) were females. Our patients’ mean age was 44 ± 16 years (ranging from 17 to 80 years). The most common symptoms were heartburn/chest pain (93.9%) and foreign body sensation in the throat (92.1%). Other symptoms observed were frequent clearing of throat (83%), dysphagia (76.4%), excessive throat mucus (74.5%), troublesome cough (72.1%) with coughing after eating/lying down (66.1%), hoarseness of voice (32.7%) and dyspnoea/choking (8.5%) (Fig. 1). Abnormalities seen on indirect laryngoscopy were erythema/hyperemia (93.9%), vocal fold edema (73.9%), diffuse laryngeal edema (46.1%), partial ventricular obliteration (38.2%), subglottic edema (18.8%), granulations (10.3%), posterior commissure hypertrophy (7.8%) and thick endolaryngeal mucus (3%) (Fig. 2).
Fig. 1.
Major symptoms of the patients
Fig. 2.
Indirect laryngoscopy findings
Mean RSI scores in males and females were 11.9 and 11.5 and mean RFS scores were 6.4 and 5.7 respectively (Table 3). RSI had 79.1% sensitivity and 83.7% specificity in diagnosing LPRD with positive predictive value 76.8%, negative predictive value 85.4% and accuracy 81.8% (Chi square value 64.5, p ≤ 0.01). There was substantial agreement between RSI and RFS (Cohen’s kappa: 0.625, p ≤ 0.0001).
Table 3.
RSI and RFS
| Frequency (N = 165) | Percentage (%) | Mean | ||
|---|---|---|---|---|
| Male | Female | |||
| Reflux Symptom Index | 11.9 | 11.5 | ||
| Positive (≥ 13) | 69 | 41.8 | 11.7 ± 4.3 | |
| Negative (< 13) | 96 | 58.2 | ||
| Reflux Finding Score | 6.4 | 5.7 | ||
| Positive (≥ 7) | 67 | 40.6 | 6.0 ± 3.5 | |
| Negative (< 7) | 98 | 59.4 | ||
Discussion
The word “reflux” is derived from Latin and it means “back flow”. Gastroesophgeal reflux is the reflux of the stomach contents into the esophagus which may be physiological and can occur up to 50 times per day, usually after meals. Gastroesophgeal reflux disease (GERD) refers to excessive reflux causing tissue damage or clinical symptoms [8]. Laryngopharyngeal reflux (LPR) includes symptoms, signs or tissue damage due to return of gastroduodenal contents into the upper aerodigestive tract [9]. Esophageal manometry helps to diagnose the disease. Though it is highly specific, it has low sensitivity, especially in cases of LPR. Esophageal pH monitoring allows the evaluation of reflux liquid or gaseous content and it considered gold standard for diagnosing GERD, but there is difficulty in accessing it, especially in developing countries.
As we compared mean RSI and RFS scores with various other studies (Table 4), our study had the least mean RSI and RFS values. However our study has established a strong positive correlation between RSI and RFS (p ≤ 0.0001), which is consistent with most of the studies [3, 10, 12, 13].
Table 4.
Comparison of mean RSI and RFS scores of various studies
Park K H et al. [14] found the sensitivity and specificity of RSI to be 75.6% and 18.8% respectively and RSI had lower validity than RFS. However our study showed RSI’s sensitivity and specificity to be 79.1% and 83.7% respectively with accuracy of 81.8%.
The diagnostic evaluation of LPR also includes laryngoscopic examination, to look for signs such as edema and diffuse laryngeal hyperemia, edema of the vocal folds, edema of vestibular folds, edema of the subglottic mucosa, interarytenoid region hypertrophy, thick endolarynx mucus, and granuloma or granulation tissue. These signs are common to other diseases affecting the larynx and pharynx, hence diagnosing the disease remains difficult [15]. To minimize the subjectivity of these signs, Belafsky et al. [4] proposed a scoring system, the RFS, based on the endolaryngeal inflammatory changes supposedly due to reflux and it has been widely used in the literature as a diagnosis parameter of LPR. The RFS has demonstrated high reproducibility and reliability, and a patient with scores above 7 points has 94% probability of presenting LPR.
Conclusion
RSI is a simple tool to diagnose LPRD which doesn’t mandate invasive procedures such as endoscopy or esophageal manometry. Hence it can be used effectively to diagnose LPRD in ENT outpatients and start the treatment at the earliest.
Funding
No funds received for this study.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional ethical committee (Institutional Ethical Committee, JJMMC, Davangere. Reference Number: JJMMC/IEC-Sy-68-2018) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
As photographs or identifying details or personal details of the participants have not been disclosed in this study, informed consent was not necessary. Complete anonymity of the participants has been maintained in this study.
Research Involving Human Participants and/or Animals
Yes, human participants.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kavitt RT, Vaezi MF. Diseases of the esophagus. Cummings otolaryngology head and neck surgery. 6. Philadelphia: Elsevier; 2015. pp. 1007–1012. [Google Scholar]
- 2.Nunes HS, Pinto JA, Zavanela AR, Cavallini AF, Freitas GS, Garcia FE. Comparison between the reflux finding score and the reflux symptom index in the practice of otorhinolaryngology. Int Arch Otorhinolaryngol. 2016;20(3):218–221. doi: 10.1055/s-0036-1579557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karakaya E, et al. Reflux finding score and reflux symptom index. JAREM. 2015;5:68–74. doi: 10.5152/jarem.2015.698. [DOI] [Google Scholar]
- 4.Belafsky PC, Postma GN, Amin MR, Koufman JA. Symptoms and findings of laryngopharyngeal reflux. Ear Nose Throat J. 2002;81(Suppl 2):10. [PubMed] [Google Scholar]
- 5.Carlsson R, Dent J, Bolling-Sternevald E, et al. The usefulness of a structured questionnaire in the assessment of symptomatic gastroesophageal reflux disease. Scand J Gastroenterol. 1998;33:1023–1029. doi: 10.1080/003655298750026697. [DOI] [PubMed] [Google Scholar]
- 6.Bardhan KD, Stanghellini V, Armstrong D, Berghöfer P, Gatz G, Mönnikes H. Evaluation of GERD symptoms during therapy. Part I: development of the new GERD questionnaire ReQuest TM. Digestion. 2004;69:229–237. doi: 10.1159/000079707. [DOI] [PubMed] [Google Scholar]
- 7.Jones R, Junghard O, Dent J, et al. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther. 2009;30:1030–1038. doi: 10.1111/j.1365-2036.2009.04142.x. [DOI] [PubMed] [Google Scholar]
- 8.Koufman JA, Aviv JE, Casiano RR, Shaw GY. Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg. 2002;127(1):32–35. doi: 10.1067/mhn.2002.125760. [DOI] [PubMed] [Google Scholar]
- 9.Koufman J, Sataloff RT, Toohill R. Laryngopharyngeal reflux: consensus conference report. J Voice. 1996;10(3):215–216. doi: 10.1016/S0892-1997(96)80001-4. [DOI] [PubMed] [Google Scholar]
- 10.Mesallam TA, Stemple JC, Sobeih TM, Elluru RG. Reflux symptom index versus reflux finding score. Ann Otol Rhinol Laryngol. 2007;116(6):436–440. doi: 10.1177/000348940711600608. [DOI] [PubMed] [Google Scholar]
- 11.Pokharel M, Shrestha I, Dhakal A, Purbey B, Amatya RCM. Reflux symptom index and reflux finding score in diagnosis of laryngopharyngeal reflux. Kathmandu Univ Med J. 2016;56(4):332–336. [PubMed] [Google Scholar]
- 12.Gelardi M, et al. Correlation between the reflux finding score and the reflux symptom index in patients with laryngopharyngeal reflux. J Biol Regul Homeost Agents. 2018;32(1 Suppl. 2):29–31. [PubMed] [Google Scholar]
- 13.Vázquez de la Iglesia F, FernándezGonzález S, Gómez Mde L. Laryngopharyngeal reflux: correlation between symptoms and signs by means of clinical assessment questionnaires and fibroendoscopy. Is this sufficient for diagnosis? Acta Otorrinolaringol Esp. 2007;58(9):421–425. doi: 10.1016/S0001-6519(07)74959-2. [DOI] [PubMed] [Google Scholar]
- 14.Park KH, Choy SM, Kwon SUK, Yoon SW, Kim SUK. Diagnosis of laryngopharyngeal reflux among globus patients. Otolaryngol Head Neck Surg. 2006;134:81–85. doi: 10.1016/j.otohns.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 15.Almeida AGP, Saliture TBS, Silva ASS, Eckley CA. Translation and cultural adaptation of the Reflux Finding Score into Brazilian Portuguese. Braz J Otorhinolaryngol. 2013;79(1):47–53. doi: 10.5935/1808-8694.20130009. [DOI] [PMC free article] [PubMed] [Google Scholar]