Abstract
Anterior shoulder instability with bone loss is a challenging condition. The two most performed procedures, Bankart repair & Latarjet, are not without issues. We describe a technique where arthroscopic free bone grafting was performed in conjunction with remplissage. We feel that this combined arthroscopic procedure offers advantages that include reduced risk of conventional Latarjet complications, including neurological deficits and metal hardware complications while preserving subscapularis and coracoid. Furthermore, these advantages may not come at the cost of compromised outcomes, particularly recurrence rate, as the remplissage may compensate for the possible lack of “sling effect” with free bone graft reconstruction.
Key Words: Bipolar lesions, Bone block, Hill Sachs lesions, Instability, Remplissage
Introduction
Traumatic anterior shoulder instability is a common and old problem.1 Over the last century, many surgical techniques have been described to address recurrent anterior shoulder instability, but two have become dominant: the Bankart repair and the Latarjet procedure. Both have excellent track records, but neither is without issues.2 Bankart repair is associated with a high recurrence rate, especially in the presence of significant glenoid bone loss. 3, 4 Latarjet is a non-anatomic procedure that may be associated with a significant complication rate. 5-7 These possible issues with the two-pillar techniques have led investigators to explore other procedures, including remplissage and glenoid free bone block reconstrcution.8
The remplissage procedure involves a “capsulodesis and a tenodesis” of the infraspinatus to fill the Hills-Sacks (HS) lesion converting it to extracapsular and preventing its engagement.9-12 The GFBB (Eden-Hybinette procedures and their various modifications) is a possible alternative to Laterjet in those patients with significant bone loss.13-16 t is possibly associated with reduced risk of some of the Latarjet complication but crucially does not pose the “sling” effect which may be an important factor in Latarjet’s excellent recurrence rates. 17,18
In this communication, we describe a technique where arthroscopic GFBB was performed in conjunction with remplissage. We feel that this combined arthroscopic procedure may avoid some of the complications associated with Latarjet while addressing significant “off-track” HS lesions. Furthermore, performing the remplissage in addition to GFBB reconstruction may, to some extent, compensate for the lack of “sling effect” with GFBB reconstruction.
Technical note
The technique described here, combines and modifies two previously described techniques for arthroscopic GFBB and remplissage [Table 1]. 10,16,19, 20
Table 1.
Steps involved in the technique
| Step | Scope Position | Procedure |
|---|---|---|
| 1 | Posterior portal | Diagnostic scope: assessment of glenoid bone loss/labral tear/soft tissue quality |
| 2 | Antero-superior portal | Assessment of HS lesion |
| 3 | Antero-superior portal | Release of anterior labrum from anterior glenoid |
| 4 | Antero-superior portal | Anterior glenoid surface preparation |
| 5 | Antero-superior portal | Passage of two 2.8 cannulated sleeved drills through the jig |
| 6 | Antero-superior portal | Remplissage: Insertion of all-suture anchors |
| 7 | Posterior portal | Anchor insertion for anterior labral repair |
| 8 | Antero-superior portal | Passage and retriever of two suture loops through each sleeve |
| 9 | N/A | Preparation of bone block |
| 10 | N/A | Passage of implant with endo-button through bone block |
| 11 | Posterior portal | Passage of bone block to the ideal position |
| 12 | N/A | Insertion of posterior endobuttons |
| 13 | Antero-superior portal | Tensioning of bone block |
| 14 | Antero-superior portal | S ecuring the bone block with “Nice Knot” |
| 15 | Posterior portal | Completion of labral repair |
| 16 | Antero-superior portal | Completion of remplissage |
Camera in the Posterior Portal
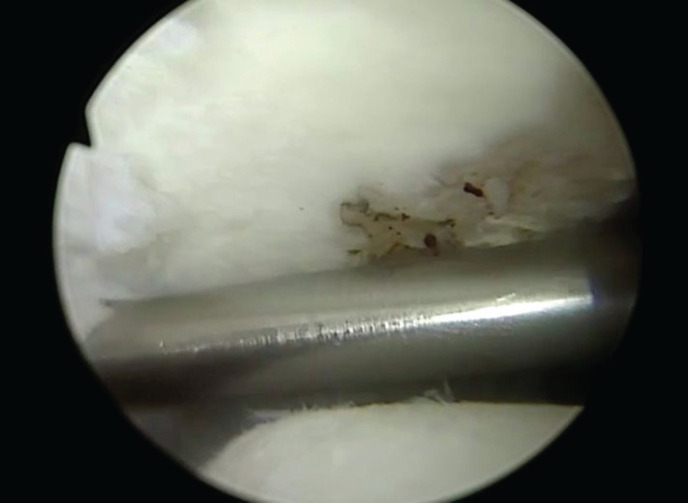
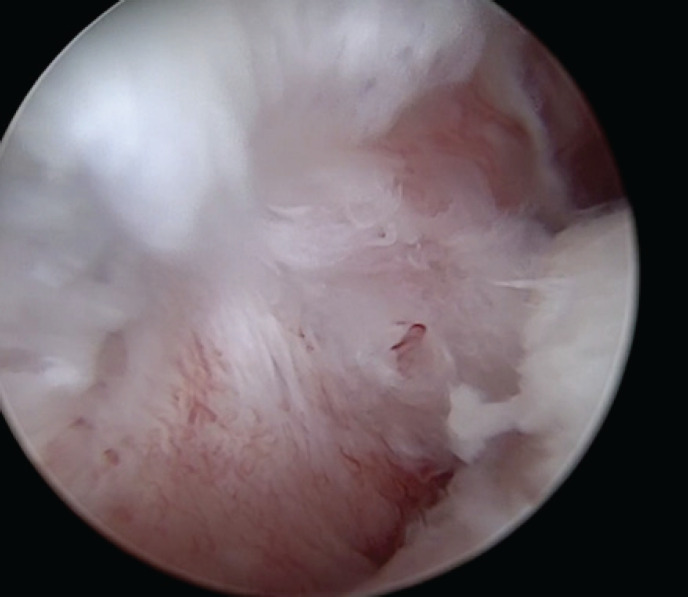
A diagnostic arthroscopy is performed with the camera in the standard posterior portal. Standard anterior portal in rotator interval and anterosuperior portal are created. The features of the anterior labral tear and the soft tissue’s quality are assessed [Figure 1].
Figure 1.
Arthroscopic view of scope in the posterior portal showing the anterior labral tear and the HS lesion
Camera in the Antero-superior Portal
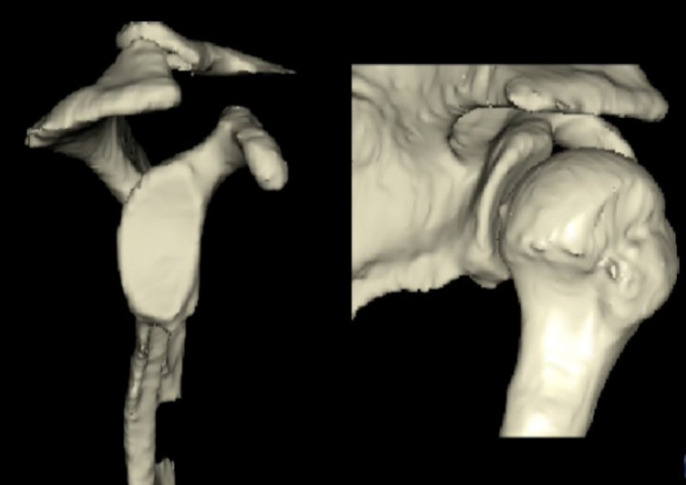
The camera is next switched to the anterosuperior, where a better assessment of the HS lesion and glenoid bone loss may be made. The decision to proceed with arthroscopic GFBB and remplissage is made only in the presence of significant glenoid bone loss (more than 15%) when the quality of labrum and soft tissue is adequate, and there is an “off-track” HS lesion (as measured from preoperative computed tomography scans [Figure 2, 3]. 3
Figure 2.
Preoperative 3D reconstruction CT scans showing the glenoid bone loss & HS lesion
Figure 3.
Arthroscopic view of scope in the anterosuperior portal showing the labral lesion, quality of the soft tissue, and the anterior glenoid morphology
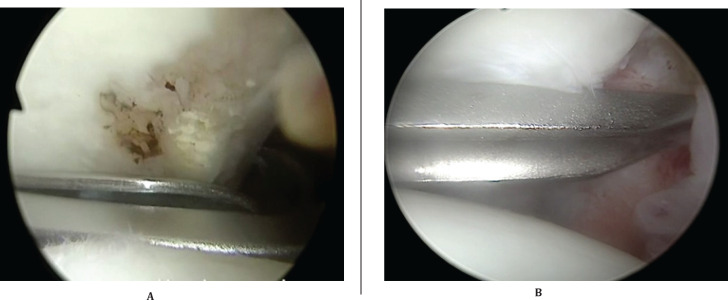
Glenoid Preparation
The anterior labrum is detached from the anterior glenoid rim. In addition, the glenoid surface is prepared to create a flat bleeding bony surface [Figure 4].
Figure 4.
Arthroscopic view of scope in the anterosuperior portal: anterior glenoid preparation
Glenoid Guide Jig Insertion
The technique initially described by Taverna is used for GFBB reconstruction.20A spinal needle is inserted from the posterior, aiming for the center of the glenoid defect parallel to the glenoid surface [Figure 5].
Figure 5.
Arthroscopic view from anterosuperior portal: Introduction of the needle from the posterior portal aiming towards the center of the glenoid bone defect
A small skin incision is made posterior where the needle enters the skin. A switching stick is introduced through this incision and passed anteriorly in the same direction as the needle [Figure 6].
Figure 6.
Arthroscopic view from anterosuperior portal: Introduction of switching stick aiming towards the center of the glenoid bone defect
The glenoid drill guide (Smith & Nephews) is introduced through the same incision, sliding it over the switching stick. Once happy with the position of the guide, the switching stick is removed, and the guide hook is slid through the guide track [Figure 7].
Figure 7.
Arthroscopic view from anterosuperior portal: Introduction of guide and hook
The guide is then rotated so that the tip of the hook is positioned at the center of the anterior glenoid defect. The “semi-tunnel of the guide is then removed while holding the guide hook firmly [Figure 8].
Figure 8.
Arthroscopic view from anterosuperior portal: Positioning of the hook
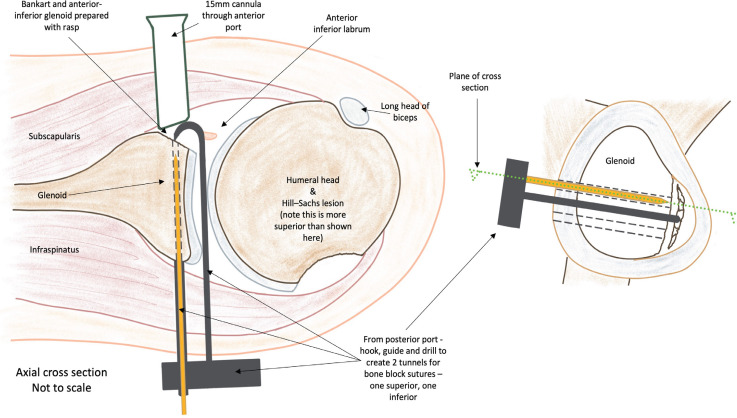
Two bullets are then passed posteriorly through the guide to the posterior aspect of the glenoid neck to secure the guide. Furthermore, 2.8mm cannulated sleeved drills are passed over each bullet using the power drill, so they exit the anterior glenoid 10mm apart.20 Once happy with the position, the inner drills, bullets, and the guide are removed[Figure 9, 10].
Figure 9.
Arthroscopic view from anterosuperior portal: passage & positioning of cannulated sleeves
Figure 10.
Schematic diagram showing the bone block guide and sleeves in place
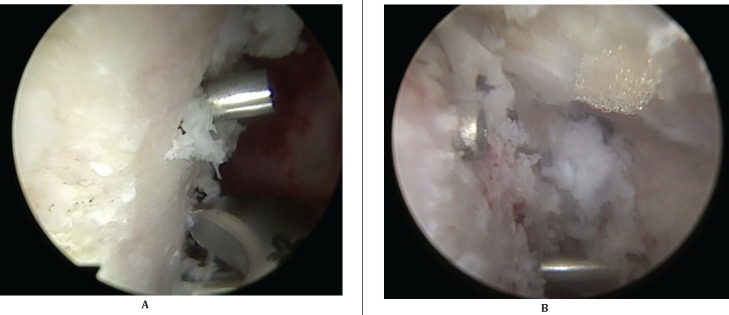
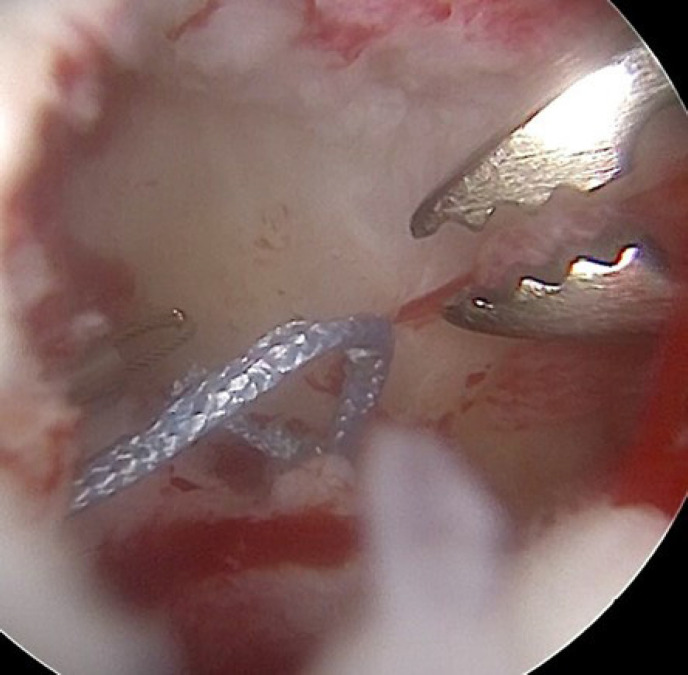
Remplissage- Insertion of all-suture anchors (first part)
With sleeves in position, the first part of the remplissage procedure is initiated. The exact remplissage technique has been previously described. 10-19 A spinal needle is used to mark the best skin site incision posterolaterally for the approach to the HS lesion. An 8.25mm cannula is inserted in this posterolateral portal, positioning it through the deltoid muscle while taking care not to violate the integrity of the infraspinatus tendon. Three (or two if HS is not too large) 2.3mm all-suture double-stranded anchors (Stryker Iconix) are passed into the HS with two anchors medially and on anchor laterally (if HS is large enough otherwise just two anchors are used) [Figure 11].
Figure 11.
Arthroscopic view from anterosuperior portal: 2.3 all suture anchors in the HS lesion
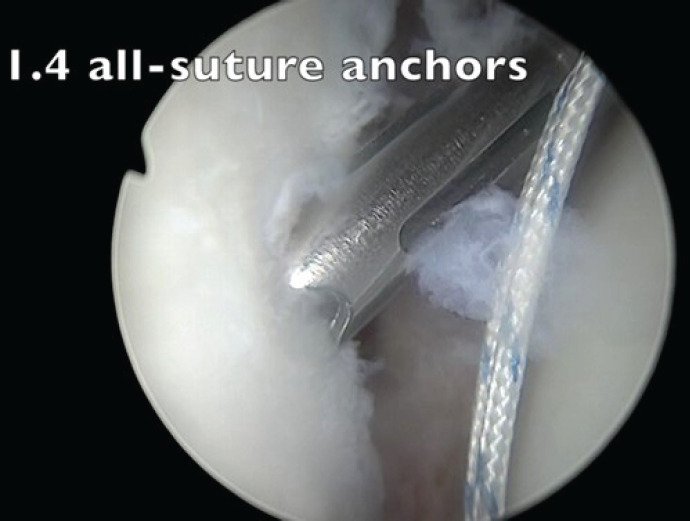
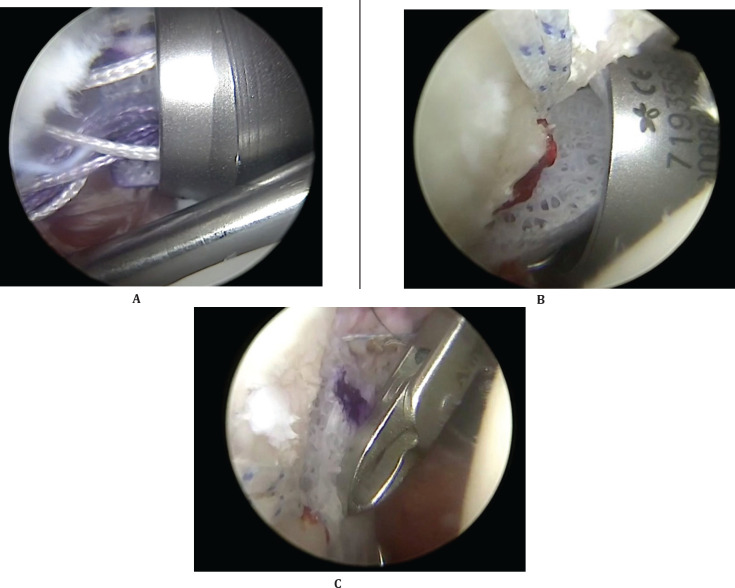
Anchor Insertion for Anterior Labral Repair
We like to repair the anterior labrum over the bone block once the bone block is secured. Anchors for labral repair are inserted before positioning and securing the bone graft to prevent damaging bone graft implant sutures while drilling the anterior glenoid edge for the labral repair anchors. Two or three 1.4mm all-suture anchors (Iconix-Stryker) are placed anteroinferior on the glenoid edge for labral repair (which will be completed later in the procedure) [Figure 12].
Figure 12.
Arthroscopic view from posterior portal: 1.4 all suture anchors for the labral repair to be performed later
Preparations and Passage of Free Bone Graft
The cannula in the standard anterior port (rotator interval) is exchanged with a special 15mm metal cannula. A suture retriever is then used to pass two suture loops through each sleeve from the posterior to the anterior direction. The loops are brought through the metal cannula using standard suture graspers (scope in anterosuperior port) [Figure 13]. These suture loops are clipped separately, and the sleeves are then removed.
Figure 13.
Arthroscopic view from anterosuperior portal: Retrieval of suture limbs
The free bone graft is then prepared by fashioning a human allograft (Hospital Innovation) to a 20x10x10 mm cuboid. The two 2.8mm drill holes are made 10 mm apart (Smith & Nephews).
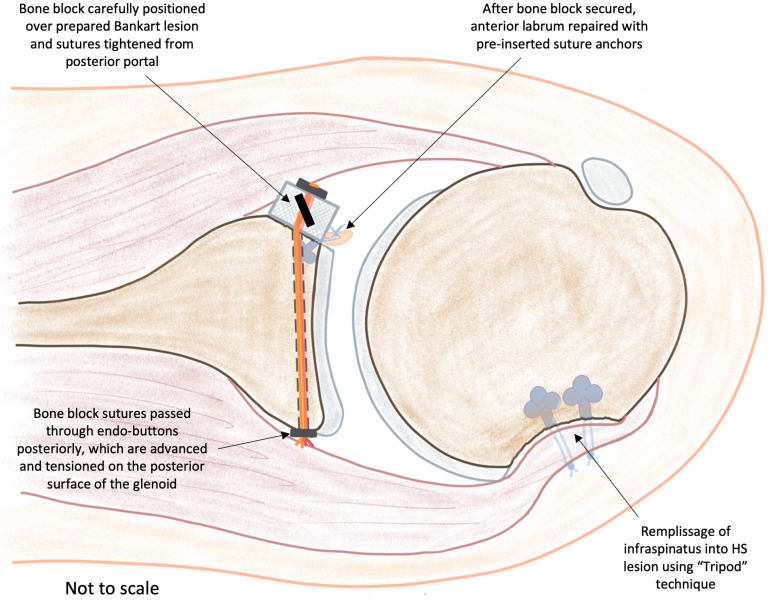
The superior loop suture is passed through the superior hole of the bone block and the inferior one through the inferior hole. These two suture loops are then used to shutter the endo-button and suture implant through each bone block hole. The implant limbs are tensioned; hence, the endo-buttons sit flush with the bone block surface. The bone block is then guided passed through the metal cannula (inferior part first) by pulling and tensioning the looped shutter sutures posteriorly one by one [Figure 14,16].
Figure 14.
Schematic diagram showing the prepared bone block just before insertion with remplissage & glenoid anchors in situ
Figure 16.
Arthroscopic view from posterior portal: the passage of bone block graft
Once happy with the bone block position, the implant suture limbs are then passed through two endo-buttons posteriorly using suture retrievers. The two endo-buttons are then advanced anteriorly (with a sliding knot and knot pusher) until they come to rest flushed on the posterior glenoid surface (as described in the original technique by Taverna.20 The posterior endo-buttons are then subsequently tensioned and secured using a special tensioning device and “Nice Knot” [Figure 17]. 20
Figure 17.
Arthroscopic view from anterosuperior portal: tensioning & securing the bone graft using posterior endo-buttons, tensioning device & Nice knot
Completion of Anterior Labral Repair
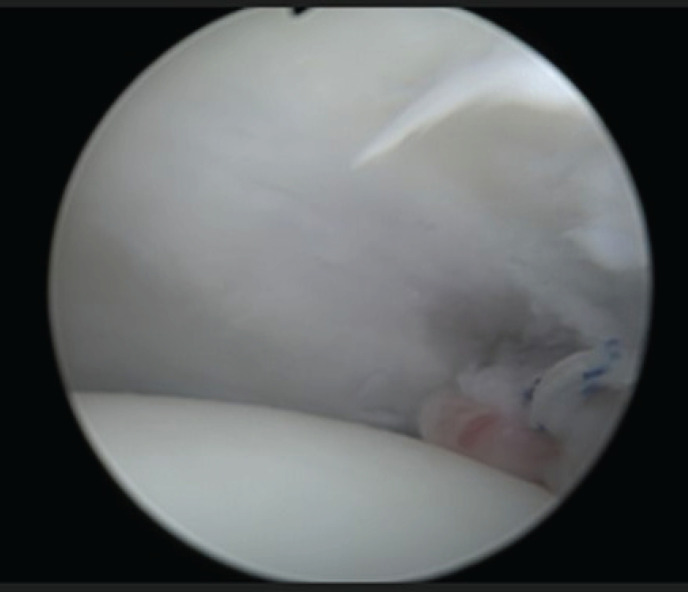
With the bone block firmly secured, the anterior labrum is subsequently repaired over the glenoid bone block using previously inserted anchors [Figure 18].
Figure 18.
Arthroscopic view from posterior portal: completion of labral repair over bone graft block
Completion of Remplissage
The scope is next placed in the superolateral port, and the remplissage is completed. The modified “Pulley technique used as previously described.10,19 The technique involves tying one suture limb on each anchor to another suture limb in a triangular/tripod fashion to optimize healing by maximizing surface contact between the infraspinatus and the HS’s lesion [Figure 19].
Figure 19.
Arthroscopic view from anterosuperior portal: completion of remplissage
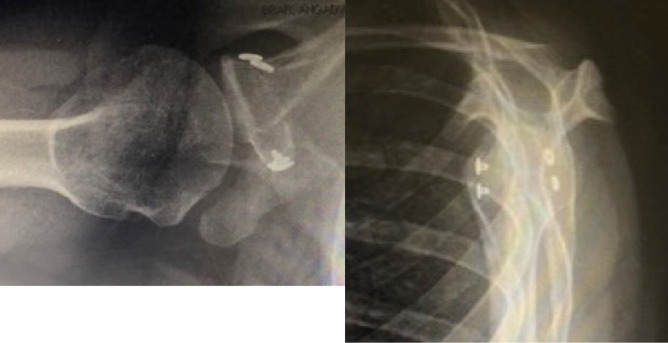
The final configuration includes bone block secured with labrum repaired over it and remplissage of HS lesion [Figure 20, 21]. Postoperative radiographs confirm the position of bone block allograft [Figure 22].
Figure 20.
Final arthroscopic view from the anterosuperior portal with labral repair covering the bone block
Figure 21.
Diagram showing bone block secured with labrum repaired over it & remplissage of HS lesion
Figure 22.
Postoperative X-ray images (Axillary and Y views)
Discussion
Bankart’s repair and Latarjet have become the pillar of stability surgery but Bankart’s repair is associated with a relatively high recurrence rate (2) and Latarjet maybe associated with a complication rate as high as 30%. 1,2,5,7,8,21-26
The GFBB reconstruction, not a new technique, has evolved to involve the reconstruction of the glenoid with J-shaped bicortical iliac graft, distal tibial allograft, distal clavicular autograft, and even xenograft.27-30 Furthermore, all-arthroscopic means of performing the procedure have recently gained popularity.16-31 The possible advantages of GFBB over Latarjet are that it is not a nonanatomical reconstruction, preserves coracoid, reduces the risk of neurological complications, and can address large glenoid bone loss. Additionally, the arthroscopic technique preserves subscapularis, avoids metal screw complications, and potentially permits other pathologies such as HS lesions to be addressed arthroscopically at the same time.16 Although there are a number of studies that demonstrate comparable outcomes to Latarjet with the free bone block, the worry is the lack of the “sling effect”.14-15,32 The sling effect does appear to play a role in the effectiveness of Latarjet.17-18 With the technique described in this communication, GFBB is combined with remplissage with the aim for remplissage to compensate for the possible lack of “sling effect” with GFBB.
The described technique may offer advantages that include reduced risk of some important complications of conventional Latarjet, including neurological deficits and metal hardware complications, subscapularis preservation, and a more anatomical reconstruction. Furthermore, these advantages may not come at the cost of compromised outcomes, particularly recurrence rate as the remplissage may compensate to an extent for the possible lack of “sling effect” influence with free bone graft reconstruction.
Figure 15.

Schematic diagram demonstrating the passage of bone block through the metal cannula
References
- 1.Rashid MS, Arner JW, Millett PJ, Sugaya H, Emery R. The Bankart repair: past, present, and future. J Shoulder Elbow Surg. 2020;29(12):e491–8. doi: 10.1016/j.jse.2020.06.012. [DOI] [PubMed] [Google Scholar]
- 2.Imam MA, Shehata MS, Martin A, et al. Bankart repair versus latarjet procedure for recurrent anterior shoulder instability: a systematic review and meta-analysis of 3275 shoulders. Am J Sports Med. 2021;49(7):1945–53. doi: 10.1177/0363546520962082. [DOI] [PubMed] [Google Scholar]
- 3.Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy: Arthroscopy. 2014;30(1):90–8. doi: 10.1016/j.arthro.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Burkhart SS, De Beer JF, Barth JR, Criswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy: Arthroscopy. 2007;23(10):1033–41. doi: 10.1016/j.arthro.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 5.Hendy BA, Padegimas EM, Kane L, et al. Early postoperative complications after Latarjet procedure: a single-institution experience over 10 years. J Shoulder Elbow Surg. 2021;30(6):e300–8. doi: 10.1016/j.jse.2020.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Domos P, Lunini E, Walch G. Contraindications and complications of the Latarjet procedure. Shoulder Elbow. 2018;10(1):15–24. doi: 10.1177/1758573217728716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Griesser MJ, Harris JD, McCoy BW, Hussain WM, Jones MH, Miniaci A. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. J Shoulder Elbow Surg. 2013;22(2):286–92. doi: 10.1016/j.jse.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Hurley ET, Matache BA, Wong I, et al. Anterior shoulder instability part II-Latarjet, remplissage, and glenoid bone-grafting-an international consensus statement. Arthroscopy. 2022;38(2):224–233. doi: 10.1016/j.arthro.2021.07.023. [DOI] [PubMed] [Google Scholar]
- 9.Wolf EM, Pollack ME. Hill-Sachs “Remplissage”: an arthroscopic solution for the engaging Hill-Sachs lesion (SS-32) Arthroscopy. 2004;20:e14–5. doi: 10.1016/j.arthro.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 10.Koo SS, Burkhart SS, Ochoa E. Arthroscopic double-pulley remplissage technique for engaging Hill-Sachs lesions in anterior shoulder instability repairs. Arthroscopy: Arthroscopy. 2009;25(11):1343–8. doi: 10.1016/j.arthro.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Purchase RJ, Wolf EM, Hobgood ER, Pollock ME, Smalley CC. Hill-Sachs “remplissage”: an arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy: Arthroscopy. 2008;24(6):723–6. doi: 10.1016/j.arthro.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 12.Zhu YM, Lu Y, Zhang J, Shen JW, Jiang CY. Arthroscopic Bankart repair combined with remplissage technique for the treatment of anterior shoulder instability with engaging Hill-Sachs lesion: a report of 49 cases with a minimum 2-year follow-up. Am J Sports Med. 2011;39(8):1640–8. doi: 10.1177/0363546511400018. [DOI] [PubMed] [Google Scholar]
- 13.Auffarth A, Schauer J, Matis N, Kofier B, Hitzl W, Resch H. The J-bone graft for anatomical glenoid reconstruction in recurrent posttraumatic anterior shoulder dislocation. Am J Sports Med. 2008;36(4):638–47. doi: 10.1177/0363546507309672. [DOI] [PubMed] [Google Scholar]
- 14.Moroder P, Plachel F, Becker J, et al. A Clinical and radiological long-term results after implant-free, autologous, iliac crest bone graft procedure for the treatment of anterior shoulder instability. Am J Sports Med. 2018;46(12):2975–80. doi: 10.1177/0363546518795165. [DOI] [PubMed] [Google Scholar]
- 15.Gilat R, Haunschild ED, Lavoie-Gagne OZ, et al. Outcomes of the Latarjet procedure versus free bone block procedures for anterior shoulder instability: a systematic review and meta-analysis. Am J Sports Med. 2021;49(3):805–16. doi: 10.1177/0363546520925833. [DOI] [PubMed] [Google Scholar]
- 16.Taverna E, Garavaglia G, Perfetti C, Ufenast H, Sconfienza LM, Guarrella V. An arthroscopic bone block procedure is effective in restoring stability, allowing return to sports in cases of glenohumeral instability with glenoid bone deficiency. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3780–7. doi: 10.1007/s00167-018-4921-7. [DOI] [PubMed] [Google Scholar]
- 17.Giles JW, Boons HW, Elkinson I, et al. Does the dynamic sling effect of the Latarjet procedure improve shoulder stability? A biomechanical evaluation. J Shoulder Elbow Surg. 2013;22(6):821–7. doi: 10.1016/j.jse.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Yamamoto N, Muraki T, An KN, et al. The stabilizing mechanism of the Latarjet procedure: a cadaveric study. J Bone Joint Surg Am. 2013;95(15):1390–7. doi: 10.2106/JBJS.L.00777. [DOI] [PubMed] [Google Scholar]
- 19.Consigliere P, Morrissey N, Imam M, Narvani AA. The tripod-pulley technique for arthroscopic remplissage in engaging Hill-Sachs lesions. Arthrosc Tech. 2017;6(5):e1675–84. doi: 10.1016/j.eats.2017.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taverna E, D’Ambrosi R, Perfetti C, Garavaglia G. Arthroscopic bone graft procedure for anterior inferior glenohumeral instability. Arthrosc Tech. 2014;3(6):e653–60. doi: 10.1016/j.eats.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murphy AI, Hurley ET, Hurley DJ, Pauzenberger L, Mullett H. Long-term outcomes of the arthroscopic Bankart repair: a systematic review of studies at 10-year follow-up. J Shoulder Elbow Surg. 2019;28(11):2084–9. doi: 10.1016/j.jse.2019.04.057. [DOI] [PubMed] [Google Scholar]
- 22.Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir. 1954;49:994–997. [PubMed] [Google Scholar]
- 23.Ekhtiari S, Horner NS, Bedi A, Ayeni OR, Khan M. The learning curve for the Latarjet procedure: a systematic review. Orthop J Sports Med. 2018;6(7):2325967118786930. doi: 10.1177/2325967118786930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Domos P, Lunini E, Walch G. Contraindications and complications of the Latarjet procedure. Shoulder Elbow. 2018;10(1):15–24. doi: 10.1177/1758573217728716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Delaney RA, Freehill MT, Janfaza DR, Vlassakov KV, Higgins LD, Warner JJ. 2014 Neer Award paper: neuromonitoring the Latarjet procedure. J Shoulder Elbow Surg. 2014;23(10):1473–80. doi: 10.1016/j.jse.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 26.Siegert P, Plachel F, Akgün D, et al. Comparison of Structural Subscapularis Integrity After Latarjet Procedure Versus Iliac Crest Bone Graft Transfer. Orthop J Sports Med. 2020;8(10):2325967120958007. doi: 10.1177/2325967120958007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eden R. Zur Operation der habituellen Schulterluxation unter Mitteilung eines neuen Verfahrens bei Abriss am inneren Pfannenrande. Deutsche Zeitschrift für Chirurgie. 1918;144(3):269–80. [Google Scholar]
- 28.Hybbinette SR. De la transplantation d’un fragment osseux pour remédier aux luxations récidivantes de l’épaule: Constatations et résultats opératoires. Acta Chir Scand. 1932;71(411-445):26. [Google Scholar]
- 29.Kwapisz A, Fitzpatrick K, Cook JB, Athwal GS, Tokish JM. Distal clavicular osteochondral autograft augmentation for glenoid bone loss: a comparison of radius of restoration versus Latarjet graft. Am J Sports Med. 2018;46(5):1046–52. doi: 10.1177/0363546517749915. [DOI] [PubMed] [Google Scholar]
- 30.Frank RM, Romeo AA, Richardson C, et al. Outcomes of Latarjet versus distal tibia allograft for anterior shoulder instability repair: a matched cohort analysis. Am J Sports Med. 2018;46(5):1030–8. doi: 10.1177/0363546517744203. [DOI] [PubMed] [Google Scholar]
- 31.Avramidis G, Kokkineli S, Trellopoulos A, et al. Excellent clinical and radiological midterm outcomes for the management of recurrent anterior shoulder instability by all-arthroscopic modified Eden-Hybinette procedure using iliac crest autograft and double-pair button fixation system: 3-year clinical case series with no loss to follow-up. Arthroscopy. 2021;37(3):795–803. doi: 10.1016/j.arthro.2020.10.036. [DOI] [PubMed] [Google Scholar]
- 32.Bhatia S, Van Thiel GS, Gupta D, et al. Comparison of glenohumeral contact pressures and contact areas after glenoid reconstruction with Latarjet or distal tibial osteochondral allografts. Am J Sports Med. 2013;41(8):1900–8. doi: 10.1177/0363546513490646. [DOI] [PubMed] [Google Scholar]