Abstract
Laryngeal tuberculosis is a rare condition, isolated laryngeal tuberculosis without pulmonary manifestations is even more rare. Patients usually presents with voice change, difficulty in swallowing and other constitutional symptoms. The symptoms and findings can look like malignancy in most of the cases. Here, we present a case of primary laryngeal tuberculosis without pulmonary tuberculosis. A 24 year old man who presented to us with hoarseness of voice with 1 year duration. Laryngoscopic study showed a proliferative growth in the epiglottis, aryepiglottic folds and vocal cords and was diagnosed to have laryngeal tuberculosis on histopathology by the typical appearance of granuloma and caseous necrosis. The patient was started on standard antitubercular therapy and he had an excellent response to the same within 6 months. Isolated laryngeal tuberculosis should be suspected in patients with laryngeal complaints with no pulmonary symptoms, especially in a developing country like India where pulmonary tuberculosis is prevalent. Even though isolated laryngeal tuberculosis cases are rare, we should keep in mind the possibility of tuberculosis in the differential diagnosis of laryngeal tumors, as the incidence of tuberculosis is steadily increasing.
Keywords: Tuberculosis, Primary, Larynx, Anti tubercular drugs
Introduction
The incidence of pulmonary tuberculosis in India has decreased drastically due to advancements in Public Healthcare and standardization in treatment protocols by national programmes for the same. Extra pulmonary tuberculosis is usually secondary to pulmonary tuberculosis in the bygone era but according to the recent literature review, isolated extra pulmonary tuberculosis alone can be seen due to an increase in life expectancy and by a decline in BCG vaccination.
Laryngeal tuberculosis can develop either due to direct spread of mycobacterium tuberculosis to the larynx from the contaminated sputum or by hematogenous spread. The clinical findings can mimic laryngeal carcinoma and has to be diagnosed correctly. The incidence of laryngeal tuberculosis was about 33% in the pre antibiotic era, but with the advent of antitubercular drugs, the incidence has come down to less than 1%. In this study, we present a case of primary laryngeal tuberculosis.
Case Presentation
A 24 year-old male patient, shop keeper by occupation presented with 1 year history of change in voice to the outpatient department of Otorhinolaryngology at Vydehi Institute of Medical Sciences and Research Centre, Bangalore. He had occasional episodes of dry cough, but no other symptoms like fever, chest pain, stridor, dyspnoea, dysphagia, odynophagia, odynophonia. He has no habits and no significant medical or family history or contact to patients with tuberculosis.
On General Examination, he was conscious, oriented, well nourished and afebrile, with no cervical lymphadenopathy, scars or sinuses. Indirect laryngoscopic examination showed pale proliferative lesion involving the laryngeal surface of epiglottis and aryepiglottic folds, pale proliferative false cords and true cords on both sides. Vocal cord mobility could not be assessed.
Due to its laryngoscopic appearance and a high index of suspicion for laryngeal tuberculosis, a provisional diagnosis of laryngeal tuberculosis was made and planned for direct laryngoscopy and biopsy under general anesthesia. Pulmonologist opinion was taken preoperatively and a 2 day early morning sputum samples were sent for Acid Fast Bacilli (AFB) examination which came negative. The respiratory system examination and chest X-ray were normal. His hematological and biochemical parameters were within normal limits except erythrocyte sedimentation rate was higher than normal limits (21 min/ 1st h) (Figs. 1, 2).
Fig. 1.
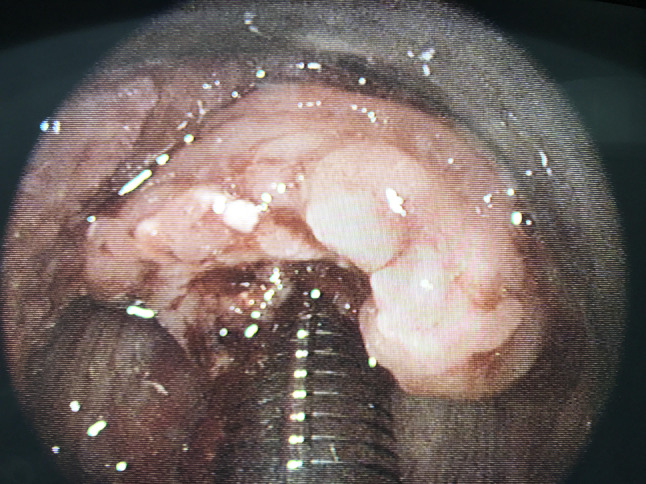
Direct Laryngoscopic finding of the pale and proliferative epiglottis
Fig. 2.
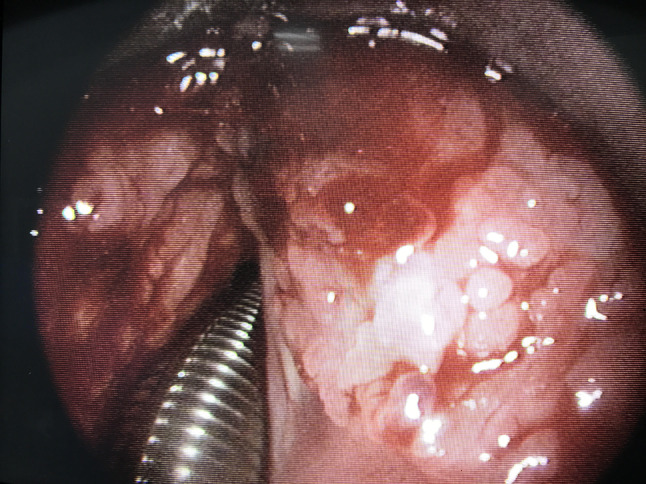
Direct Laryngoscopic finding of the pale and proliferative false cords
His histopathological examination revealed fragments lined by stratified squamous epithelium exhibiting focal areas of ulceration. Sub epithelial stroma shows focal areas of necrosis surrounded by epitheloid granulomas containing langhan’s type of giant cells. Also vast areas of caseous necrosis were seen. Sections were negative for malignancy. Histopathological findings suggested necrotizing granulomatous inflammation, probably due to tuberculosis (Figs. 3, 4, 5).
Fig. 3.
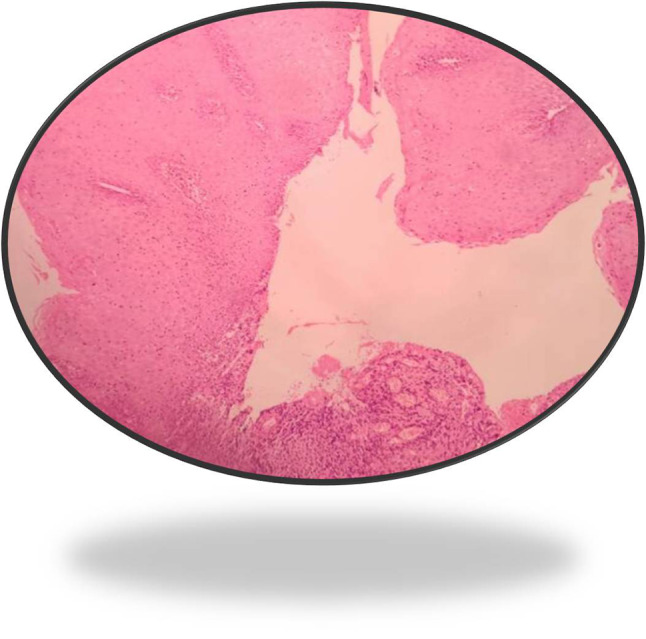
Histopathological examination of sample from epiglottis (H&E 10 ×)
Fig. 4.
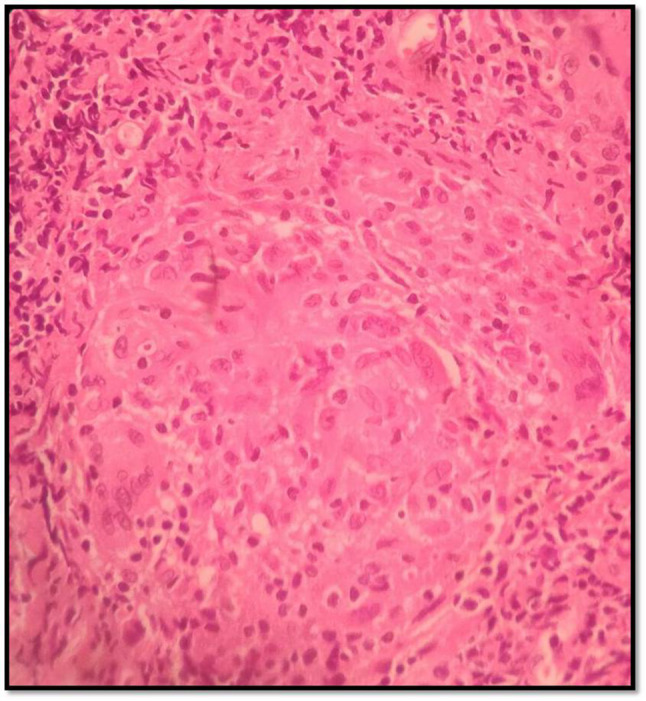
Histopathological examination of sample from epiglottis (H&E 40 ×) showing epitheloid granuloma
Fig. 5.
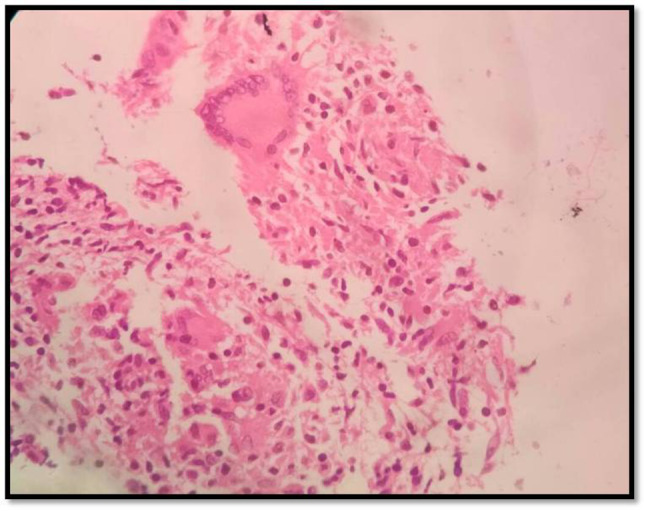
Histopathological examination of sample from epiglottis (H&E 40×) showing Langhan’s type of giant cells
The patient received intravenous antibiotics and steroids for 3 days post operatively. A pulmonologist opinion was sought after the biopsy report and the patient was started on category I Anti-tubercular drugs: Isoniazid, Rifampicin, Pyrazinamide, and Ethambutol as per RNTCP guidelines for 6 months (Intensive phase of 2 months and continuation phase of 4 months). Patient is on regular follow-up and is symptomatically better and the mass has also improved.
Discussion
Primary laryngeal tuberculosis of larynx is a rare clinical entity. In a study conducted by Rohwedder et al. on 843 patients with tuberculosis, only 11 patients (1.3%) had laryngeal involvement [1]. The development of laryngeal tuberculosis can be either primary or secondary [2]. In the absence of a pulmonary involvement, it is known as primary lesion. In this case, the laryngeal involvement was probably a primary lesion without any history of known contact to tuberculosis patients or any pulmonary involvement. Alonso et al. in their report of 11 cases, reported that the dominant symptom was dysphonia in 82% of cases, which is associated with or without odynophagia or dyspnea [3]. Difficulty in swallowing, hoarseness, and chronic cough are main symptoms in patients suspicious to laryngeal carcinoma. In the present case, the only symptom was hoarseness of voice. Nishiike et al. has described various findings of laryngeal involvement on a study of 15 patients with laryngeal tuberculosis and broadly categorized into 3 different types: ulcerative lesions, granulomatous lesions and non specific inflammatory lesions [4]. A non specific inflammatory lesion was seen in our case. The diagnostic modality of choice is direct laryngoscopy with biopsy from the lesion and demonstration of caseating granuloma and langhans type of giant cells.
The exclusion of laryngeal cancer is the diagnostic challenge in such cases, as the treatment is entirely different for both these conditions. Timely administration of anti tubercular drugs provides good prognosis, completely curing the disease without any complications, subsiding the lesions over a 2 month period [5].
Conclusion
This case report would like to fill in the lacunae in ENT practice about the occurrence of isolated primary laryngeal tuberculosis without any known history of exposure to tuberculosis patients in an immuno-competant patient. There are very few cases of primary laryngeal tuberculosis in medical literature and hence it should be kept in mind with a high index of suspicion when treating any laryngeal lesions in India.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Research Involving Human Participants and/or Animal
Not applicable.
Informed Consent
Informed consent was obtained from the patient for use of data for publication.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rohwedder JJ. Upper respiratory tract tuberculosis. Sixteen cases in a general hospital. Ann Intern Med. 1974;80:708–713. doi: 10.7326/0003-4819-80-6-708. [DOI] [PubMed] [Google Scholar]
- 2.Richter B, Fradis M, Kohler G, Ridder GJ. Epiglottic tuberculosis: differential diagnosis and treatment Case report and review of literature. Ann Otol Rhinol Laryngol. 2001;110:197–201. doi: 10.1177/000348940111000218. [DOI] [PubMed] [Google Scholar]
- 3.Alonso PE, Mateos AM, Perez-Requena J, Serrano EA. Laryngeal tuberculosis. Rev Laryngol Otol Rhinol. 2002;2002(14):352–356. [PubMed] [Google Scholar]
- 4.Nishiike S, Irifune M, Sawada T, Doi K, Kubo T. Laryngeal tuberculosis: a report of 15 cases. Ann Otol Rhinol Laryngol. 2002;111(10):916–918. doi: 10.1177/000348940211101010. [DOI] [PubMed] [Google Scholar]
- 5.Verma SK, Verma SK, Sanjay Laryngeal tuberculosis clinically similar to laryngeal cancer. Lung India. 2007;24:87–89. doi: 10.4103/0970-2113.44221. [DOI] [Google Scholar]


