Abstract
Laryngo-tracheo-bronchial tuberculosis may be primary or secondary to pulmonary tuberculosis. It causes stenosis of the airway, leading to life threatening airway obstruction. We herein describe the challenges in managing a case of laryngo-tracheo-bronchial stenosis in a 22-year-old patient who presented with stridor post antituberculous therapy secondary to a malacic airway.
Keywords: Tuberculosis, Laryngeal tuberculosis, Stenosis, Stridor, Tracheomalacia
Introduction
Laryngo-tracheo-bronchial tuberculosis is defined as tuberculous infection of the larynx and tracheobronchial tree diagnosed either via a positive microbial culture or histopathological staining [1–3]. We will present the challenges and dilemma in managing a complicated laryngo-tracheo-bronchial tuberculosis presented with complex stenosis, tracheomalacia and distorted anatomy in a young female patient.
Case Report
A 22-year-old Malay lady was referred in 2008 for upper airway obstruction 1 month post completion of antituberculous therapy for pulmonary tuberculosis. She presented with stridor and dyspnoea, where a diagnostic microlaryngobronchoscopy revealed severe subglottic edema and tracheal stenosis. She was managed with emergency tracheostomy under local anesthesia. A contrast enhanced computed tomography (CECT) neck showed multisegment narrowing of the airway involving the subglottis, trachea, and right main bronchus. The repeated sputum smears and airway biopsy were negative for tuberculous infection. She progressed to develop a complete subglottic stenosis with resultant aphonia after 3 months. A Shian-Yann Lee procedure and T-tube insertion was performed which provided her with normal breathing and phonation.
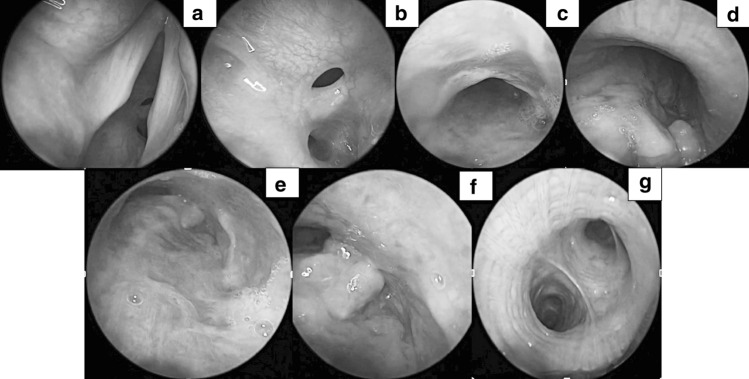
One year following T-tube stenting, a trial of decannulation was attempted but failed, hence a tracheostomy was performed. A laryngotracheal reconstruction (LTR) was performed 5 years following her presentation for the resultant subglottic stenosis (Fig. 1a,b). This too, was to no avail, and she still required serial dilatations and steroid injections post procedure.
Fig. 1.
Serial endoscopic examination of the airway showing (a) Normal vocal cord with subglottic stenosis seen below it, and (b) Cotton Meyer grade 3 subglottic stenosis prior to LTR in 2013; c significant reduction of antero-posterior diameter of the thoracic trachea concluding tracheomalacia in 2016; d worsening tracheomalacia up to the carina (e) with granulation tissue, completely obliterating the right main bronchus (f) seen in 2017 with endoscopic view of normal left main bronchus (g) where modified ETT stent was placed
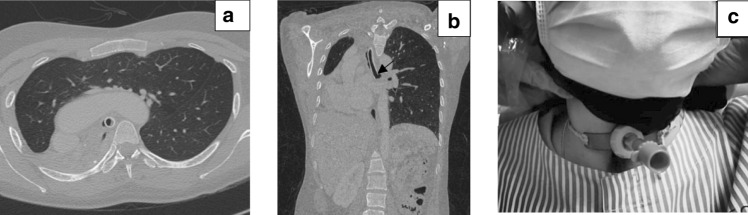
Two and a half years post LTR, she developed tracheomalacia at the distal trachea (Fig. 1c). An extended tracheostomy tube was initially able to relief her symptoms but her disease progressed to involve the carina (Fig. 1d) and insertion of modified endotracheal tube (ETT) to stent the malacic segment was performed under general anesthesia. She was able to change the modified ETT by herself daily and she remained well for one and a half years until she redeveloped symptoms of shortness of breath again. Granulation and stenosis of the carina was seen (Fig. 1e, f) and modified ETT was readjusted so that the tip is in the left bronchus (Fig. 1g). CECT thorax and bronchus was performed showing total right lung collapse (Fig. 2a) with compensatory expansion of the left lung, following successful stenting of the left main bronchus with the modified ETT (Fig. 2b). The ETT was later fenestrated to allow vocalization. Patient has remained well on follow up for the past 2 years now using the modified ETT (Fig. 2c).
Fig. 2.
Following insertion of a modified ETT stent, corresponding CECT thorax showed (a) total collapse of the right lung with extensive compensatory hyperinflation of left lung, crossing the midline to the right side on axial cut, b modified ETT in the left main bronchus (arrow) with the heart and mediastinum completely shifted to the right (c) the clinical picture of the patient’s neck showing the modified ETT at 2 years follow-up
Discussion
We describe the challenges faced in managing this young lady for the past 12 years who developed complex narrowing of her airway, namely at multiple levels at the tracheobronchial tree, as a result of pulmonary and most possibly a concurrent endobronchial tuberculosis. Endobronchial tuberculosis reported to have a predilection for young females which is consistent with our patient [2–4]. It has been thought to be due to easy implantation of organisms from infected sputum, since women do not generally expectorate sputum possibly due to socio-cultural factors [4] and higher likelihood of sputum retention due to smaller size of bronchial lumen compared to adult male [2, 3].
This case was initially managed with Shian-Yann Lee procedure, T-tube insertion and subsequently laryngotracheal reconstruction, which failed to improve her symptoms. A review of adult laryngotracheal stenosis concluded that 50% of patients with complex stenosis develop recurrence following open airway interventions. In addition, grade 3 or 4 stenosis, those needing at least one post operative dilatation or secondary tracheostomy are all associated with higher rates of tracheostomy dependence [5]. True enough, our patient was tracheostomy dependent post T-tube stenting and laryngotracheal reconstruction.
Many studies show that the most common site of endobronchial tuberculosis involvement is at the right upper lobe and right main bronchus, and is most likely due to the lymph node erosion as seen in the CT scan [4]. The resultant tracheomalacia might be due to multiple factors which are weakness and atrophy of cartilage after tuberculosis, recurrent tracheobronchitis and lower respiratory tract infections and complications from frequent bronchoscopic interventions to alleviate her acute symptom.
Pulmonary tuberculosis is well known to cause chronic complication from minimal scarring, bronchiectasis with recurrent infection and in advanced case destruction of entire lung despite effective treatment [6]. Total right sided lung collapse in our patient led to post pneumonectomy syndrome with mediastinal shift, traction of the heart, great vessel and central airway [6]. This causes the airway to be distorted and not of normal configuration.
In complex airway stenosis, multidisciplinary approach and surgical intervention is required. Recently Liu et al. has proposed for interventional bronchoscopy in all benign central airway stenoses, and surgery is reserved for failed endoscopic treatment [7]. However, there is no strong consensus regarding treatment algorithm in complex airway stenosis. Management very much depends on availability of respective specialties in a particular centre and tailored to individual patient. In our patient, further surgical treatment is difficult due to multilevel stenoses with tracheomalacia.
Stenting is associated with complications such as growth of granulation tissue, mucus plugging, stent migration or fracture, recurrent infection and malacic airway post stent removal [8]. Bacon et al. proposed that stenting should be considered when patient is symptomatic and airway collapse is greater than 60% [8]. In our patient, the malacic airway was initially stented by using longer tracheostomy tube however this did not relieve her symptoms. Eventually modified endotracheal tube was inserted as no commercialized stent was able to fit the tortuous airway in our setting. Tay et al. used novel angulated stent by modifying straight stent to manage difficult tracheobronchial tuberculosis involving bronchus or tortuous airway [9] where only 33.3% out of 21 patients had successful stent removal. In concurrent tracheal and bronchial disease Y-shape stent has been used, however associated with recurrent stent obstruction with granulation tissue and mucus impaction as well as infection [8]. Recently, significant advances have been made for airway stenting for example 3D printed stent that is customized to fit individual airway’s anatomy [7]. This new development may solve the dilemma in managing complex airway disease however more research is needed to assess its safety and complication profile.
Conclusion
Modified fenestrated endotracheal tube is an unusual management of complex tracheobronchial stenosis secondary to endobronchial tuberculosis. However, it can be successfully employed in centers with limited resources to alleviate airway obstruction.
Availability of Data and Material
Relevant clinical data is presented within this manuscript.
Acknowledgements
The authors have no conflict of interest to disclose. Images are courtesy of Department of Radiology, Hospital Tuanku Fauziah. We thank the patient for allowing us to publish the clinical images associated with this publication. Author contributions are listed as below: Substantial contributions to the conception or design of the work: NAK, XYY, MZI, IWAR, MA. Data acquisition: NAK, IWAR. Data analysis and interpretation: XYY, MZI, MA. Drafting of this work: NAK. Revising this work critically for important intellectual content: IWAR, XYY, MZI, MA. Final approval of the version to be published: NAK, XYY, MZI, IWAR, MA. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: NAK, XYY, MZI, IWAR, MA.
Funding
This work did not receive any funding from governmental or non-governmental organizations for the purpose of study design, data collection, data interpretation or manuscript writing.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics Approval
The conduct of this study was approved by the institutional Ethical Review Board on November 2020 with the approval code FF-2020.
Consent to Participate
This manuscript contains patient’s endoscopic and radiological images. The patient provided a written consent to publish the clinical data and related images. A copy of the written consent is available upon request made to the corresponding author.
Consent for Publication
This manuscript contains patient’s endoscopic and radiological images. The patient provided a written consent to publish the clinical data and related images. A copy of the written consent is available upon request made to the corresponding author.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Siow WT, Lee P. Tracheobronchial tuberculosis: a clinical review. J Thorac Dis. 2017;9:E71–E77. doi: 10.21037/jtd.2017.01.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Su Z, Cheng Y, Wu Z, Zhang P, Chen W, Zhou Z, et al. Incidence and predictors of tracheobronchialtuberculosis in pulmonary tuberculosis: a multicentre, large-scale and prospective study in Southern China. Respir. 2019;97(2):153–159. doi: 10.1159/000492335. [DOI] [PubMed] [Google Scholar]
- 3.Jung SS, Park HS, Kim JO, Kim SY. Incidence and clinical predictors of endobronchial tuberculosis in patients with pulmonary tuberculosis. Respir. 2015;20(3):488–495. doi: 10.1111/resp.12474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kashyap S, Solanki A. Challenges in endobronchial tuberculosis: from diagnosis to management pulmonary medicine. London: Hindawi Publishing Corporation; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosow D, Barbarite E. Review of adult laryngotracheal stenosis pathogenesis, management and outcomes. Curr Opin Otolaryngol Head Neck Surg. 2016;24:489–483. doi: 10.1097/MOO.0000000000000305. [DOI] [PubMed] [Google Scholar]
- 6.Shah M, Reed C (2014) Complications of tuberculosis. Current Opinion in Infectious Diseases. Lippincott Williams and Wilkins, pp 403–10 [DOI] [PubMed]
- 7.Liu L, Kong J, Georg C. Recent advances in airway stenting. Shanghai Chest. 2020;4:6–6. doi: 10.21037/shc.2019.11.02. [DOI] [Google Scholar]
- 8.Bacon JL, Patterson CM, Madden BP. Indications and interventional options for non-resectable tracheal stenosis. J Thorac Dis Pioneer Biosci Publ. 2014;6:258–270. doi: 10.3978/j.issn.2072-1439.2013.11.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tay CK, Jeong BH, Kim H. Angulated stents-a novel stent improvisation to manage difficult post-tuberculosis bronchial stenosis. ASAIO J. 2018;64(4):565–569. doi: 10.1097/MAT.0000000000000692. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Relevant clinical data is presented within this manuscript.