Abstract
The objective of the study was to assess endoscopic coblation adenoidectomy and conventional cold curettage adenoidectomy in terms of safety and efficacy in pediatric patients. Study included 40 pediatric patients, aged between 4–17 years. 20 patients underwent cold curettage adenoidectomy and 20 underwent Coblation adenoidectomy. The 2 procedures were compared on various parameters like duration of surgery, intra—operative blood loss, and post –operative pain. To further the comparison, follow -up Nasal Endoscopy was done after 1 week and after 1 month to assess for injury to peripheral tissues and completeness of removal of adenoids. There was statistically significant difference, favouring Coblation adenoidectomy in terms of lesser intra-operative blood loss (mean blood loss of 19 mL Vs 28.5 mL) and lesser post -operative pain measured on Visual Analogue Scale (median VAS score of 2 Vs 2.67). Shorter duration of surgery (mean operative time of 10.3 min Vs 15.5 min) was the only parameter in favour of conventional cold curettage method. Injury to peripheral tissue and residual adenoid were seen in patients who underwent curettage adenoidectomy. The overall advantages of Coblation adenoidectomy when compared with cold curettage adenoidectomy are less intra-operative bleeding, less post -operative pain, completeness and preciseness of adenoid removal with minimal injury to adjacent tissues. For these reasons, Coblation adenoidectomy should be the standard technique adopted for adenoidectomy.
Keywords: Pediatric adenoidectomy, Cold curettage, Coblation
Introduction
The word Adenoid is derived from two words “adenos” (= gland) and “idos” (= form) [1]. The enlarged adenoids often manifest with clinical features like nasal obstruction, snoring, decreased sense of smell and pain in throat. In order to diagnose the enlarged adenoids a diagnostic nasal endoscopy (method of choice) or digital radiograph of lateral skull for nasopharynx is used. Though medical management has been found to be effective in bringing about marked improvement in a vast majority of patients, some patients need to undergo surgical removal of enlarged adenoids. Adenoidectomy can be accomplished with Curettes, Suction diathermy, Laser, Micro Debrider or Coblation [2].
The word Coblation is derived from “Controlled Ablation”. The principle of Coblation is passing of energy in form of radiofrequency through a conducting media like isotonic sodium chloride solution and producing a plasma field. By Coblation the medium is dissociated into nascent sodium ions which are responsible for destroying intercellular bonds resulting in tissue dissociation. This is possible when temperature reaches 60–70° C.
Objective
To assess endoscopic coblation adenoidectomy and conventional cold curettage adenoidectomy in terms of safety and efficacy in paediatric patients.
Methods
Sample size 40 pediatric patients (age 4–17 years).
Sampling technique Purposive sampling.
Study type Observational study.
Study setting ENT department of a tertiary health care teaching hospital.
Inclusion Criteria
Pediatric patients aged 4–17 years, whose complaints were suggestive of adenoid enlargement and/or chronic adenoiditis.
Patients not responding to medical management.
Patients who were willing to undergo surgery.
Having no co-existing morbidity.
Exclusion Criteria
Age less than 4 years and more than 17 years.
Patients with history of allergy, deviated nasal septum, nasopharyngeal growth, cleft palate/submucosal cleft palate, choanal atresia, bleeding diathesis.
Patient responding to medical management.
40 pediatric patients, aged between 4–17 years, who attended ENT department of our tertiary care teaching hospital with complaints related to adenoid enlargement (like nasal obstruction, mouth breathing, snoring, running nose, hyponasality, dry throat, getting up from sleep due to nasal blockage, adenoid facies, and Otitis Media with Effusion), after obtaining consent were enrolled in this study.
All the patients were evaluated by detailed history taking, clinical examination. Nasal obstruction was evaluated by cold spatula test. Diagnostic Nasal Endoscopy (DNE) was done to assess the adenoid status and Grade the enlargement according to Clemens McMurray scale [3]. Radiograph of lateral skull for nasopharynx was done. Fitness for anesthesia was ascertained as per protocol.
The patients were recruited in two groups, Group A and B on alternate basis of admission. Patients of Group A underwent cold curettage adenoidectomy and patients of Group B underwent Coblation adenoidectomy.
Surgical Procedure
General anesthesia was administered via oral endotracheal tube, which was placed in midline and fixed securely. Rose’s position was given. An appropriately sized Boyle-Davis mouth gag was carefully inserted and then suspended on Magauran’s plate. Conventional adenoidectomy was carried out using St. Clair Thompson adenoid curette of appropriate size, with the surgeon sitting at the head end of the table.
For Coblation adenoidectomy, after general anesthesia patient was placed in the supine position and Boyle- Davis mouth gag was inserted to open the mouth. Catheter was passed through the nostril to retract the soft palate. 4 mm or 2.7 mm 0 ° rigid nasal endoscope was passed through the nasal cavity to visualize the adenoids. The surgeon stood on the right side of patient and Coblation wand was introduced through the oral cavity to the nasopharynx. Under endoscopic guidance the adenoidectomy was performed (Fig. 1).
Fig. 1.

Image showing coblator wand acting on adenoid
Data are presented and analysed as mean, Standard deviation and percentages, as required. Statistical analysis was performed using the Chi-square test and t-test. The value of p < 0.05 was considered as statistically significant.
Results
The patient demographics, complaints and grade of adenoid enlargement were documented.
In our study we had 40 patients between age 4–17 years; 20 patients of age below 10 years and 20 patients of age above 10 years; 24 were males and 16 were females.
Nasal obstruction/discharge and mouth breathing were the most common symptom (= 32), followed by pain in throat (= 27). Sleep disturbance was complained of by 25 patients. 10 patients had adenoid facies. (Table 1).
Table 1.
Symptoms of the patients
| Symptoms/signs | No | Percentage |
|---|---|---|
| Nasal obstruction/discharge | 32 | 80 |
| Sleep disturbance | 25 | 60 |
| Mouth breathing | 32 | 80 |
| Pain throat | 27 | 70 |
| Adenoid facies | 10 | 25 |
Adenoid enlargement was graded according to Clemens McMurray scale. Grade I, II, III and IV were seen in 2, 15, 13 and 10 patients respectively.
The following parameters namely operative duration, intra-operative blood loss, post-operative pain, injuries to peripheral tissues, and completeness of removal were compared between the 2 groups. (Table 2 and Fig. 2).
Table 2.
Comparison of Operative duration, Blood loss, VAS Score, Injury to peripheral tissue, Completeness of removal
| Group | A (Cold curettage) |
B (Coblation) |
p value |
|---|---|---|---|
|
Operative duration (minutes) |
10.3 + / − 3.1 | 15.55 + / − 3.49 | 0.0001 |
|
Blood loss (mL) |
28.5 + / − 3.66 | 19 + / − 3.88 | 0.0001 |
| VAS score | 2.67 + / − 0.9 | 2 + / − 0.95 | 0.0066 |
| Injury to peripheral tissue (No.) | 4 | 0 | – |
| Completeness of removal (No.) | 16 | 20 | – |
Fig. 2.
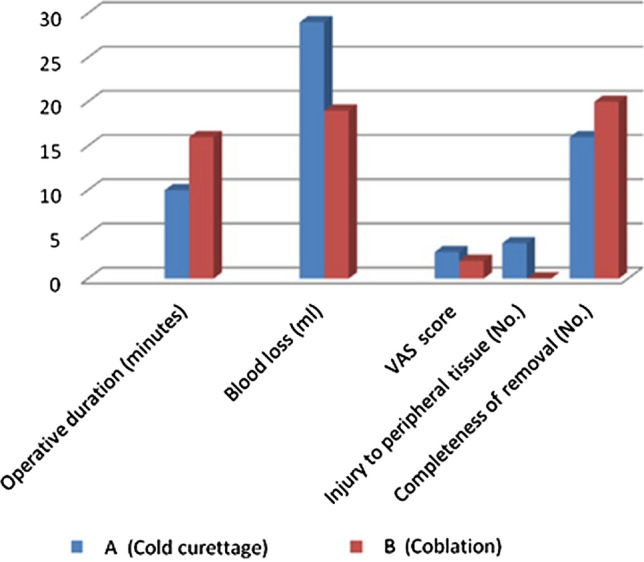
Bar chart showing different parameters compared
Operative Duration
The time taken for completing the surgery was measured from when appropriate position was given after introducing Boyle Davis mouth gag and till haemostasis was achieved after removal of adenoids. Average mean time for surgery in Group A (cold curettage) was 10.3 ± 3.66 min and that for Group B (Coblation) was 15.55 ± 3.49 min [p value < 0.0001]. The time taken to perform adenoidectomy by curettage was lesser. The wand of the Coblation needed to be cleaned repeatedly as the dissection progressed, adding to the operative duration.
Intraoperative Blood Loss
Blood loss during any surgery is inevitable and the same applies to adenoidectomy. The intra-operative blood loss was variable in both the groups. We calculated the amount of blood loss by counting the number of roller packs removed from nasopharynx which were used for achieving haemostasis. We assumed that a fully soaked roller pack of length 10 cm equalled approximately 10 mL of blood loss, while partially soaked ones equalled 5 mL of blood loss. The amount of blood lost during the procedure was obtained after subtracting the amount of Normal Saline used from the total volume of fluid collected in the suction machine after the conclusion of procedure; and it was added to the blood loss calculated from number of soaked roller packs.
The amount of blood loss in Group A (Cold curettage) was around 20–35 mL, with mean and standard deviation of 28.5 ± 3.66. In Group B (Coblation) it was 15–25 ml, with mean and standard deviation of 19 ± 3.88 [p value < 0.0001]0.95% confidence interval of the difference of two means was 11.9145–7.0855. The intraoperative blood loss is lesser in Group B, and this was statistically significant.
Visual Analogue Scale (VAS)
This is a scale that tries to measure a characteristic or attitude of pain that ranges from 0, which is no pain to 10, which is worst possible, unbearable and excruciating pain. We gave a VAS scale to patients in presence of their guardians to score a particular amount of pain that he/she was experiencing. The median VAS score for Group B (Coblation) was 2 ± 0.95 and for Group A (Cold curettage) it was 2.67 ± 0.9 [p value < 0.0066]. 95% Confidence interval for same was 0.251–1.44. This value was statistically significant.
Additionally we observed that from Group B, 17 patients scored 0 (no pain) or 2 (mild annoying pain),3 patients scored more than 2 (nagging, uncomfortable troublesome pain); whereas from Group A,10 patients scored 0 (no pain) or 2 (mild annoying pain) and 10 patients scored more than 2 (nagging, uncomfortable, troublesome pain) on VAS. In our study, none of the patients recorded 5, 6 (distressing, miserable pain) 7, 8 (intense dreadful, horrible pain) or 9,10 (worst possible, unbearable, excruciating pain). This was indeed a useful measure to assess the pain experienced, as a child may not exactly convey severity of his/her pain.
The patients were followed up weekly and on 15th day, to assess amount of pain and absenteeism from school if pain was severe. Average days of pain in Group B was 2, while average days of pain in Group A was 3[p value > 0.5].
Injury to Peripheral Tissues
Nasal Endoscopy was done under local anaesthesia on 7th postoperative day and after one month. Injuries to peripheral tissues were seen (on posterior pharyngeal wall and in the vicinity of eustachian tube opening) in 4 patients. All these 4 patients had undergone adenoidectomy by cold curettage (Group A). There were no peripheral injuries in patients undergoing adenoidectomy by Coblation (Group B).
Completeness of Removal
Incomplete removal of adenoids was seen in 4 patients on follow up—they belonged to Group A. In Group B patients no such residual adenoids were observed.
No significant major complications were observed during this study.
Discussion
Hans Wilhelm Meyer collaborated with an instrument maker to devise a sharp ring knife that was used for his first operation in February 1868 [1]. This gradually gave way to curettes; and with advancing technological developments in the field of biomedical sciences, today we see many instruments being used for performing adenoidectomy. The surgery has progressed from being performed blindly to being performed with endoscopic assistance. Endoscopic assisted adenoidectomy has advantages over conventional curettage adenoidectomy as was shown in a meta-analysis carried out by Yang et al. [4].
The primary aim of adenoidectomy is the complete removal of the adenoids with little damage to surrounding tissues and minimal blood loss. To facilitate early resumption of routine activities the recovery period should also be short with minimal post -operative pain. In this regard the present study is compared with the study of other authors on various parameters. (Table 3).
Table 3.
Comparison of different parameters across studies quoted
| Author | Operative duration (minutes) | Blood loss (ml) | VAS | Injury to peripheral tissues (no.) | Completeness of removal (no.) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | A | B | A | B | A | B | A | B | |
| Timms et al. [2] | – | 5–15 | – | < 1 | – | – | Increased likelihood | – | – | Precise |
| Ferriera et al. [5] | 9.6 | 23.0 | – | – | – | – | – | – | 20% | 80% |
| Abd El Rahman El Tahan et al. [6] | 10 | 15 | 25 | 10 | – | – | – | – | 10/200 | 2/200 |
| Di Rienzo et al. [7] | 12 | 19 | 30.7 | 2.3 | 7.15 | 3.85 | – | – | – | – |
| Chauhan et al. [9] | 11 | 29 | 51 | 23 | 5–7 | 0–4 | – | – | – | – |
| Songu et al. [13] | 7.15 | 12.02 | 22.97 | 26.32 | – | – | – | – | ||
| Bidaye et al. [14] | 4.17 | 18.27 | 44.33 | 32.47 | 6.37 | 3.87 | – | – | 40% | 0 |
| Sarvana et al. [15] | – | – | 32.7 | 2.5 | 7.2 | 7.15 | – | – | – | – |
| Our study | 10.3 | 15.55 | 28.5 | 19 | 2.67 | 2 | 4/20 | 0 | 4/20 | – |
The use of Coblation resulted in an increase in operative duration in the present study. The surgery was completed in a comparatively shorter time when done with curettes, as it is a simple procedure. The mean operative duration in the present study for Group A (Cold curettage) was approximately 10 min, ranging from 7–10 min; while the mean time required for the surgery in Group B (Coblation) was 15 min, ranging from 15–20 min. These results are consistent with a study conducted by Ferreira M S et al. and Abd El Rahman El Tahan et al. [5, 6]. Di Rienzo Businco et al. and Chauhan et al. have also shown similar results.
The pioneers of Coblation, Timms et al. have mentioned in their paper that when they started this procedure, it would take them 15 min, but later on they were able to complete this procedure in less than 5 min [2]. This reflects the importance of learning curve.
The amount of blood loss in Group A (Cold curettage) was around 20–35 mL. In Group B (Coblation), it was 15–25 mL and this was significant. Abd El Rahman El Tahan et al. in their study reported that the mean blood loss was significantly lower in Coblation method compared with curettage method, being 10 and 25 ml respectively [6]. Less blood loss in coblation method was also reported by DiRienzo Businco et al. and Ozkiris et al. [7, 8]. Timms et al. have shown that coblation can be accomplished with less than 1 mL of blood loss [2].
The median VAS score for Group B (Coblation) was 2 and for Group A (Cold curettage) was 3 in our study; the difference being significant. According to Chauhan et al., post-operative pain VAS score 0–4 was more common in patients undergoing adenoidectomy by Coblation and higher scores of 5–7 in patients undergoing curettage adenoidectomy [9]. Significantly less postoperative pain in the Coblation group compared with the curettage group was reported in the study by Di Rienzo Businco et al. [8]. Abd El Rahman El Tahan did not find significant difference in pain scores which they evaluated at different intervals [7]. These differences could be due to patient or procedure related variables.
The average number of days in which there was a complaint of pain by the patients in Group B (Coblation) was 2 days, while that in Group A (cold curettage) was 3 days. This difference is basically attributed to the method in which both the techniques work. Adenoid curette shaves off the adenoid tissue with sheer force and without direct vision. Hence chances of peripheral injuries increase, including damage to the underlying muscle such as the superior constrictor muscle. While in Coblation, movement of wand occurs under endoscopic vision, dissecting layer-by-layer of adenoid tissue till its bed is reached. Inadvertent injuries to peripheral tissues are avoided. As a consequence, the recovery period in the Coblation group was shorter than in the cold curettage group. At follow up, injuries to posterior pharyngeal wall, uvula, soft palate and torus around the Eustachian tube were observed in 4 patients of Group A, and none in group B. Timms et al. and others have also observed increased likelihood of injury to surrounding tissues when curettes are used blindly [2].
Coblation wand used in conjunction with endoscope facilitates precise removal of adenoid tissues. Removal of adenoids from areas around the Eustachian tube opening and posterior choanae can be achieved—these areas are said to be common sites of adenoid recurrence [10, 11]. A study conducted by Ismail Elnashar et al. stated that conventional curettage misses a substantial volume of adenoid tissue in these areas [12]. Murat Songu et al. in their study concluded that Coblation adenoidectomy ensured complete removal [13]. A study by Bidaye et al. showed 40% of patients who underwent conventional cold curettage adenoidectomy had adenoid tissue post-surgery, while it was absent in endoscopic assisted coblation adenoidectomy patients [14]. In our study, residual adenoids were seen in 4 patients, all of them were of Group A, i.e. curettage group and none in Group B.
To summarise, our study results are consistent with that of the study by Abd El Rahman El Tahan et al., Di Rienzo Businco et al. and Bidaye et al. After comparing the 2 techniques, they all concluded that Coblation took longer intra-operative time but resulted in lesser intra-operative blood loss. All their studies showed that conventional curettage took lesser intra-operative time, but resulted in comparatively more blood loss and had relatively more chance of recurrence or of residual adenoid [6, 7, 14]. V Saravana Selvan et al. in their study opined that Coblation adenoidectomy offers the advantages of better safety, precision of adenoid removal and lesser injury to peripheral tissues [15].
Conclusion
There are always 2 sides of a coin, which means there are a few drawbacks of Coblation technique. There is a requirement of complete setup of endoscopic unit along with Coblation unit. The procedure takes comparatively longer time for preparation—time is required for adequate decongestion of nasal cavities with decongestant soaked patties. In addition, there is a specific learning curve required to achieve competency in use of Nasal Endoscopes and Coblation wands.
On the various parameters evaluated in this study to compare the 2 techniques, it is evident that Coblation adenoidectomy is better as compared to cold curettage adenoidectomy in terms of lesser intra-operative blood loss, shorter period of post-operative discomfort, and lower likelihood of injury to adjacent tissues, and precision of adenoid removal. For these reasons Coblation adenoidectomy should be the standard technique.
Funding
None.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Informed Consent
Informed consent was obtained from parent/guardian of all participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ruben RJ. The adenoid: its history and a cautionary tale. Laryngoscope. 2017;127:S13–28. doi: 10.1002/lary.26634. [DOI] [PubMed] [Google Scholar]
- 2.Timms MS, Ghosh S, Roper A. Adenoidectomy with the coblator: a logical extension of radiofrequency tonsillectomy. J Laryngol Otol. 2005;119:398–399. doi: 10.1258/0022215053945840. [DOI] [PubMed] [Google Scholar]
- 3.Clemens J, McMurray JS, Williging JP. Electrocautery versus curette adenoidectomy: comparision of postoperative results. Int J Pediatr Otorhinolaryngol. 1998;43:115–122. doi: 10.1016/S0165-5876(97)00159-6. [DOI] [PubMed] [Google Scholar]
- 4.Yang L, Shan Y, Wang S, Cai C, Zhang H. Endoscopic assisted adenoidectomy versus conventional curettage adenoidectomy:a meta-analysis of randomized controlled trials. SpringerPlus. 2016;5:426. doi: 10.1186/s40064-016-2072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferreira MS, Mangussi Gomes J, Ximendes R, Evangelista AR, Garera LB, Miranda EL, Stanum AC. Comparison of three different adenoidectomy techniques in children - has the conventional technique been surpassed? Int J Pediatr Otorhinolaryngol. 2018;104:145–149. doi: 10.1016/j.ijpori.2017.11.012. [DOI] [PubMed] [Google Scholar]
- 6.El Rahman A, Tahan El, Elzayat S, Hegazy H, et al. Adenoidectomy: comparison between the conventional curettage technique and the coblation technique in pediatric patients. Egypt J Otolaryngol. 2016;32(3):152–155. doi: 10.4103/1012-5574.186528. [DOI] [Google Scholar]
- 7.Di Rienzo BL, Angelone AM, Mattei L, et al. Paediatric adenoidectomy: endoscopic coblation technique compared to cold curettage. Acta Otolaryngol. 2012;32:124–129. [PMC free article] [PubMed] [Google Scholar]
- 8.Ozkiris M, Karakavus S, Kapusuz Z, Saydam L. Comparision of two different adenoidectomy techniques with special emphasis on postoperative nasal mucociliary clearance rates: coblation technique vs cold curettage. Int J Pediatr Otorhinolayngol. 2013;77(3):389–393. doi: 10.1016/j.ijporl.2012.11.033. [DOI] [PubMed] [Google Scholar]
- 9.Chauhan VM, Patel PKB, Vishwakarma R. Plasma dissection versus tissue dissection in adenoid surgery. Indian J Otolaryngol Head Neck Surg. 2020;72(2):156–159. doi: 10.1007/s12070-019-01721-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Emerick KS, Cunningham MJ. Tubal tonsil hypertrophy: a cause of recurrent symptoms after adenoidectomy. Arch Otolaryngol Head Neck Surg. 2006;132(2):153–156. doi: 10.1001/archotol.132.2.153. [DOI] [PubMed] [Google Scholar]
- 11.Khafagy YW, Mokbel KM. Choanal adenoid in adults with persistent nasal symptoms: endoscopic management to avoid misdiagnosis and unsuccessful surgeries. Eur Arch Otorhinolaryngol. 2011;268(11):1589–1592. doi: 10.1007/s00405-011-1635-6. [DOI] [PubMed] [Google Scholar]
- 12.Elnashar I, Waheed M, Waleed ElAnwar, Basha M, Aishwadfy M. Objective assessment of endoscopy assisted adenoidectomy. Int J Pediatric Otorhinolaryngol. 2014;78(8):12391242. doi: 10.1016/j.ijporl.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 13.Songu M, Altay C, Adibelli ZH. Endoscopic assisted versus curettage adenoidectomy:a prospective, randomized, double blind study with objective outcome measures. Laryngoscope. 2010;120:1895–1899. doi: 10.1002/lary.21045. [DOI] [PubMed] [Google Scholar]
- 14.Bidaye R, Vaid N, Desarda K. Comparative analysis of conventional cold curettage versus endoscopic assisted coblation adenoidectomy. J Laryngol Otol. 2019;133(4):294–299. doi: 10.1017/S0022215119000227. [DOI] [PubMed] [Google Scholar]
- 15.Selvan VS, Silambu M, Kumaran DV. A comparative study between coblation adenoidectomy and conventional adenoidectomy. Int J Oyorhinolaryngol Head Neck Surg. 2018;4:721–725. doi: 10.18203/issn.2454-5929.ijohns20181859. [DOI] [Google Scholar]


