Abstract
To analyse the outcome of transnasal endoscopic repair of CSF Rhinorrhea in a tertiary care centre. This is a retrospective study conducted on 81 patients who underwent CSF Rhinorrhea repair in a tertiary care hospital for a period of 11 years. Following confirmation of diagnosis using bio-chemical and radiological investigations, all patients underwent transnasal endoscopic repair of CSF Rhinorrhea using a multilayer graft. Patients were followed up for 6 months. The most common etiology in our study was spontaneous CSF rhinorrhea (60.49%) and subjects with BMI > 25.5 kg/m2 were more prone to it. Cribriform plate was found to be the most frequent site of leak in our study (58.02%), followed by fovea ethmoidalis (12.35%). Overall success rate was 96.30%. Transnasal endoscopic approach for cerebrospinal fluid rhinorrhea repair shows good success rate and also offers the advantages of better visualization and identification of site of leak, less complications, rapid postoperative recovery, and low recurrence rate. Transnasal endoscopic CSF Rhinorrhea repair has shown good results in terms of low recurrence rates and high patient satisfaction among other advantages. Hence this approach should be commonly used for CSF rhinorrhea repair by surgeons.
Keywords: CSF Rhinorrhea, Endoscopic repair, Different techniques, Different materials, Body mass index
Introduction
Cerebrospinal fluid (CSF) is a physiological fluid to protect brain and maintaining intracranial pressure [1]. It is secreted by the choroid plexus in the lateral ventricles, travels to the third ventricle via the foramen of Monro. From the third ventricle, CSF reaches the fourth ventricle through the aqueduct of Sylvius. From here, it flows into the subarachnoid space via the foramina of Magendie and Luschka and is eventually reabsorbed into the dural venous sinuses by arachnoid granulation [2].
It is produced by choroid plexus in the ventricles at a rate of 20 ml per hour in adults and total CSF volume is 140 ml and a small amount of fluid come through the Blood Brain Barrier into the Extra Cellular Space of Brain by diffusion [3]. CSF is principally made up of Na + , Cl − and HCO3 − with lesser amounts of K + , Mg + + , Ca + + ; certain vitamins; and peptides and proteins actively transferred into CSF or synthesized in CP (e.g., transthyretin, insulin-like growth factor [IGF], brain-derived neurotrophic factor [BDNF]) and then transferred into CSF [4].
CSF rhinorrhea occurs when there is a breakdown of barrier between the intracranial subarachnoid space and the sinonasal mucosa. [5] The normal CSF pressure ranges from 40 mm in infants to 140 mm water in adults. Relative balance between CSF secretion by choroid plexus and resorption by arachnoid plexus play an important role in maintaining pressure.
The dehiscence of normal anatomical barrier and raised pressure gradient play an important role in CSF leak. The aetiology can be classified as spontaneous, post traumatic, iatrogenic or neoplastic [6]. The decision of conservative or surgical management depends on the site of leak, cause and timing of leak [1]. The risk of meningitis and intracranial infections are high if the patient is untreated and hence active intervention is required to prevent morbidity [7].
The transnasal endoscopic approach has become the preferred method for repairing CSF leaks in recent years preferred over intracranial approaches due to less complications. [8]
Objective
To analyse the outcome of transnasal endoscopic repair of CSF rhinorrhea in a tertiary care centre.
Materials and Methods
This is a retrospective study conducted on 81 patients who underwent CSF Rhinorrhea repair in a tertiary care hospital between February 2010–2020.
Inclusion Criteria
All cases of CSF rhinorrhoea repairs in a tertiary care hospital for a period of 11 years.
Exclusion Criteria
Large defects more than 3 cm requiring intracranial approach.
Intracranial tumours leading to CSF rhinorrhoea.
Diagnosis
Detailed history was taken followed by a complete otorhinolaryngoscopic examination.
Nasal discharge must first be positively identified as CSF. This was done by analysis of the fluid and glucose levels of > 30 mg/dl was strongly suggestive of CSF. B2 Transferrin assay was also performed to confirm the diagnosis.
All the patients underwent diagnostic nasal endoscopy and CT cisternography or MRI with contrast if meningoencephalocele was suspected, to detect the site of CSF leak (Fig. 1).
Fig. 1.

CT Cisternogram showing bilateral cribriform plate defect with bilateral CSF rhinorrhea
After confirmation of the diagnosis, written informed consent was taken and the patients underwent transnasal endoscopic CSF rhinorrhea repair under general anaesthesia by the same experienced surgeon.
Pre-operatively all the patients were given a course of antibiotics and antihistaminics.
Procedure
Bilateral nasal cavities were packed with 4% xylocaine with adrenaline (1:1, 00,000) for 10 min to decongest the nasal mucosa and turbinates.
Using a 4 mm 0 degree rigid endoscope the nasal cavity was inspected and the site of the leak identified.
After uncinectomy and ethmoidectomy, skull base was visualised in case of cribriform plate defects.
For some cases exposure of the skull base was done by lateralising the middle turbinate.
For posterior ethmoid leaks—uncinectomy and clearance of ethmoid air cells was done to approach the skull base for adequate exposure.
For sphenoid sinus leaks—trans-sphenoidal approach by lateralising the superior turbinate and widening the ostium inferiorly & laterally and performing an adequate sphenoidotomy was done.
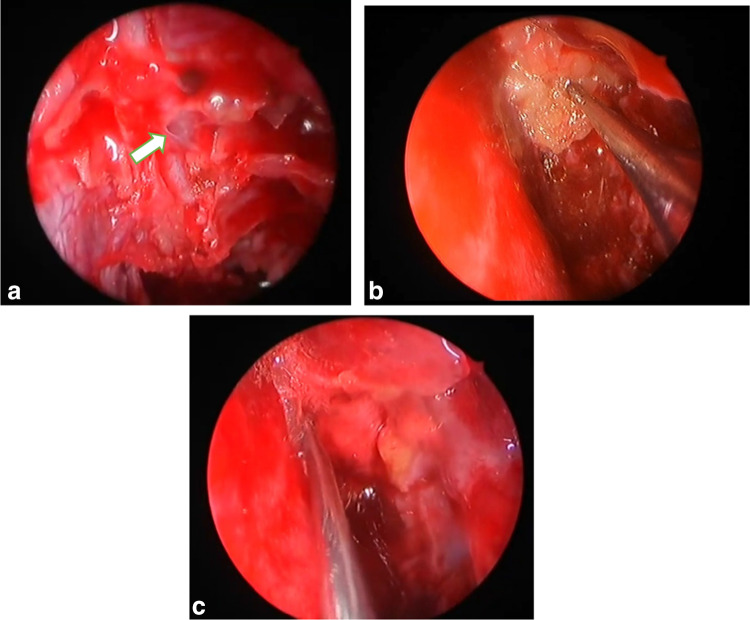
The defect in the skull base was identified and the mucosa around the defect was denuded by bipolar diathermy. Herniation of arachnoid if present was cauterised and removed.
Fat and fascia lata were harvested from the thigh.
The defect was sealed by insinuating the fat plug in the defect. In some patients collagen granules mixed with fresh frozen plasma was used primarily to cover the defect followed by fat plug. Fibrin glue was used in some patients with larger defects. (> 6 mm). Then fascia lata was used to strengthen the closure and prevent re-herniation (Fig. 2).
Fig. 2.
a White arrow points to the defect in the skull base through which CSF rhinorrhea is occurring b Defect being closed with a fat plug c Fascia lata placed covering the defect and strengthening the repair
For defects > 1 cm mashed muscle or septal cartilage was used as an additional layer to repair the defect.
Finally the repair was supported by medialising the middle turbinate. Posterior septal flap based on the sphenopalatine artery was used for closure of post-neurosurgical CSF leaks.
Bilateral nasal packing was done with merocel soaked in antibiotic solution.
Post-operative Care
Lumbar drain was placed for large defects (> 6 mm) and in patients with raised ICT to reduce the CSF pressure.
Absolute bed rest for 4 days with 30 degree head end elevation for all patients.
Appropriate antibiotics, stool softeners, anti-histaminics and anti-emetics were administered to avoid straining.
Nasal packs were removed 4 days post-surgery following which lumbar drain was removed.
Patients were discharged a week after the surgery and advised to avoid strenuous activity.
Follow-Up
The patients were followed up once in 15 days for a month and then once a month for the next 5 months.
Diagnostic nasal endoscopy was performed at each visit to look for recurrence of CSF rhinorrhea, adhesions and to maintain nasal hygiene by suction clearance.
Results
Out of the total study population of 81 patients, 49 were females (60.49%) and 32 were males (39.51%).
Majority of the patients i.e. 28.40% were in the 41–50 years age group (n = 23), followed by 51–60 years (24.69%) and 31–40 years (22.22%).
51.85% (n = 42) of the study population was found to be overweight (BMI: 25–29.9 kg/m2) and 38.27% (n = 31) was obese (BMI > 30 kg/m2).
Subjects with BMI > 25.5 kg/m2 were more prone to spontaneous CSF rhinorrhea and also were more prone to CSF leak post rhinosurgery & neurosurgery as shown in Table 1.
Table 1.
Percentage distribution of study participants according to BMI
| Body Mass Index (BMI) in kg/m2 | Number | Percentage(%) | |
|---|---|---|---|
| Male | Female | ||
| < 18.5 | 0 | 0 | 0 |
| 18.5–24.9 | 5 | 3 | 9.88 |
| 25–29.9 | 16 | 26 | 51.85 |
| > 30 | 11 | 20 | 38.27 |
79 (97.53%) patients underwent first surgical intervention for CSF rhinorrhea and 2(2.47%) were revision cases.
The most common etiology in our study was spontaneous CSF rhinorrhea (60.49%, n = 58) out of which 15.5% had raised ICT (n = 9) and showed female preponderance (n = 38, 65.5%).
The other causes for CSF rhinorrhea were traumatic (17.28%, n = 14), post transnasal transphenoidal neurosurgical procedures (7.41%, n = 6) and post rhinosurgical procedures. (3.70%, n = 3).
Cribriform plate was found to be the most frequent site of leak in our study (58.02%, n = 47), followed by fovea ethmoidalis (12.35%, n = 9), roof of sphenoid sinus (9.87%, n = 8).
Cribriform plate was the most common site of leak in both spontaneous and traumatic CSF rhinorrhea as shown in Table 2.
Table 2.
Etiology and distribution of sites of CSF leak
| Cribriform plate | Fovea ethmoidalis | Posterior ethmoid | Lateral recess of sphenoid | CLIVAL | Roof Of sphenoid | Cribriform plate + sphenoid sinus | Cribriform plate + posterior ethmoid | |
|---|---|---|---|---|---|---|---|---|
| Spontaneous | 36 | 9 | 5 | 5 | 1 | 1 | 0 | 1 |
| Trauma | 8 | 0 | 1 | 0 | 0 | 1 | 3 | 1 |
| Post Rhino surgery | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Post Neuro surgery | 0 | 0 | 0 | 0 | 0 | 6 | 0 | 0 |
Defect size ranged from < 3 mm to > 2 cm.
32 patients (39.51%) had a defect size of 3–6 mm through which CSF rhinorrhea occurred and 29 patients (35.80%) had a defect of < 3 mm as shown in Fig. 3. 1 patient (1.23%) had a large defect of > 2 cm.
Fig. 3.
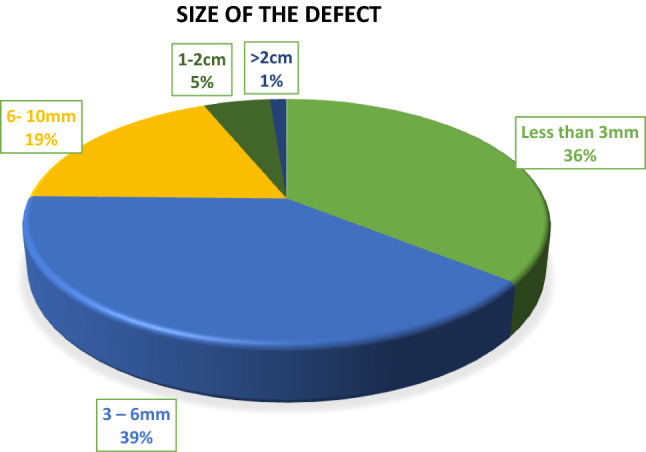
Pie chart showing the distribution of size of the defect
1 patients (1.23%) had associated meningoencephalocele and 31 patients (38.27%) had associated meningocele.
Post-operatively lumbar drain was placed for 30.86% patients (n = 25).
3 patients (3.70%) had recurrence of CSF rhinorrhea after surgery out of which 1 patient had recurrence at 2 weeks, 1 at 3 months and 1 at 6 months post-operatively.
2 patients (2.46%) out of the 3 recurrence cases developed meningitis post-operatively which may be the probable cause for recurrence of CSF rhinorrhea along with other factors like large size of defect.
Overall success rate was 96.30%.
Discussion
Confirmation of the diagnosis, identification of the site of leak & aetiology play a crucial role in management of CSF rhinorrhea repair [9].
B2 transferrin is the gold standard test for identification of nasal discharge as CSF, showing a sensitivity of 93–97% and specificity of 97–99% [10].
But in cases with associated orbital injuries this can be unreliable due to the presence of beta-2 transferrin in the vitreous humour [11].
Recently B Trace protein has been demonstrated to show higher predictive values [12].
Common sites for CSF leak are the cribriform plate, sphenoid sinus and the ethmoid roof [9, 13, 14].
Site of the leak is mainly identified using radiological investigations which is supplemented by diagnostic nasal endoscopy. CT cisternography is effective in localising the site of the defect. MRI is done in cases where CT is inconclusive and in cases of suspected meningoencephalocele [15].
The most common site of leak in our study was the cribriform plate followed by roof of sphenoid and lateral recess of sphenoid.
Cribriform plate is more prone for injury leading to CSF leak due to its lower bone density.
Most common etiology in our study was spontaneous CSF leak (71.6%), followed by traumatic (17.28%) and iatrogenic (11.1%), which is in contrast to other studies where traumatic etiology is the commonest cause [16–18].
In a study conducted by Jain et al. [15] Spontaneous CSF leak was the most common etiology (71.6%) which is in concordance with our study.
Spontaneous CSF leaks are commonly seen in middle aged women with high BMI. The increased intracranial pressure produces thinning of bone in susceptible & weak areas of the skull base like cribriform plate.
Herniation of brain and meninges along with CSF rhinorrhea, most commonly occur at the cribriform plate, fovea ethmoidalis, ethmoid roof and lateral recess of sphenoid sinus.
Transnasal endoscopic repair has revolutionised the surgical management of CSF rhinorrhea[19]. It is less invasive and provides a good view of the surgical field, has a higher success rate and is associated with lesser morbidity compared to transcranial repairs [20].
Graft materials like fat, fascia, muscle, cartilage, mucoperichondrium, mucoperiosteum, turbinates, free grafts, pedicled grafts and bone are used for repair of the defect [9].
There is no literature favouring one graft material over another. The choice of graft material depends on the surgeon’s preference, ease of manipulation and cost.
In our study multilayer autograft closure of the defect was done. For smaller defects (upto 6 mm) fat, collagen granules with fresh frozen plasma, fibrin glue and fascia lata was used. For defects greater than 6 mm fat, fibrin glue, mashed muscle, cartilage and fascia lata were used along with middle turbinate medialisation. Defects > 1 cm posterior septal flap based on the sphenopalatine artery was used.
Success rate for multilayer closure in our study for smaller defects ( upto 6 mm) was 98.3% and for larger defects (> 6 mm) was 90% which is in accordance with a study conducted by Banhawy OA et al. [21].
Single layer autograft closure technique with fibrin glue was tried by Holger G et al. for smaller defects.
(< 5 mm) with success rate of 91.6% [22].
Complications included meningitis in 2 patients in our study. Rest of the patients had an uneventful post-operative recovery.
Overall success rates of CSF leak repair according to Kirtane et al. was 98.8% in their study. [23].
Success rate of our study was 96.29%
Conclusion
From our study we can derive the following conclusions:
The most common site for CSF rhinorrhea is cribriform plate.
Spontaneous CSF rhinorrhea is the most common etiology and is commonly seen in middle aged females with a high body mass index.
The overall success rate was 96.29% which is in accordance with other studies in literature.
Transnasal endoscopic approach for cerebrospinal fluid rhinorrhea repair shows good success rate and also offers the advantages of better visualization and identification of site of leak, less complications, rapid postoperative recovery, low recurrence rate and high patient satisfaction. Thus, this approach should be used more often for CSF rhinorrhea repair by surgeons.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Oh J, Kim S, Whang K. Traumatic cerebrospinal fluid leak: diagnosis and management. Korean J Neurotrauma. 2017;13(2):63. doi: 10.13004/kjnt.2017.13.2.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pinto V, Tadi P, Adeyinka A (2020) Increased Intracranial Pressure. [online] Ncbi.nlm.nih.gov. Available at: <https://www.ncbi.nlm.nih.gov/books/NBK482119/> [Accessed 17 June 2020]
- 3.Mokgokong R, Wang S, Taylor C, Barrand M, Hladky S. Ion transporters in brain endothelial cells that contribute to formation of brain interstitial fluid. Pflügers Archiv Eur J Physiol. 2013;466(5):887–901. doi: 10.1007/s00424-013-1342-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spector R, Johanson C. Sustained choroid plexus function in human elderly and Alzheimer’s disease patients. Fluids Barriers CNS. 2013;10(1):28. doi: 10.1186/2045-8118-10-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Presutti L, Mattioli F, Villari D, Marchioni D, Alicandri-Ciufelli M. Transnasal endoscopic treatment of cerebrospinal fluid leak: 17 years’ experience. Acta Otorhinolaryngol Ital. 2009;29(4):191–196. [PMC free article] [PubMed] [Google Scholar]
- 6.Marshall AH, Jones NS, Robertson IJA. CSF rhinorrhea: the place of endoscopic sinus surgery. Br J Neurosurg. 2001;15:8–12. doi: 10.1080/02688690020024319. [DOI] [PubMed] [Google Scholar]
- 7.Yadav Y, Parihar V, Janakiram N, Pande S, Bajaj J, Namdev H. Endoscopic management of cerebrospinal fluid rhinorrhea. Asian J Neurosurg. 2016;11(3):183. doi: 10.4103/1793-5482.145101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta D, Dinesh S, Manavadaria A. Transnasal Endoscopic Repair of Cerebrospinal Fluid Rhinorrhea. An Int J Clin Rhinol. 2017;10(2):45–48. doi: 10.5005/jp-journals-10013-1305. [DOI] [Google Scholar]
- 9.Banks C, Palmer J, Chiu A, O'Malley B, Woodworth B, Kennedy D. Endoscopic closure of CSF rhinorrhea: 193 cases over 21 years. Otolaryngol-Head Neck Surg. 2009;140(6):826–833. doi: 10.1016/j.otohns.2008.12.060. [DOI] [PubMed] [Google Scholar]
- 10.Meurman O, Irjala K, Suonpää J, Laurent B. A new method for the identification of cerebrospinal fluid leakage. Acta Otolaryngol. 1979;87(3–6):366–369. doi: 10.3109/00016487909126434. [DOI] [PubMed] [Google Scholar]
- 11.Ryali R, Peacock M, Simpson D. Usefulness of β2-transferrin assay in the detection of cerebrospinal fluid leaks following head injury. J Neurosurg. 1992;77(5):737–739. doi: 10.3171/jns.1992.77.5.0737. [DOI] [PubMed] [Google Scholar]
- 12.Arrer E, Meco C, Oberascher G, Piotrowski W, Albegger K, Patsch W. β-Trace protein as a marker for cerebrospinal fluid Rhinorrhea. Clin Chem. 2002;48(6):939–941. doi: 10.1093/clinchem/48.6.939. [DOI] [PubMed] [Google Scholar]
- 13.Kim S, Park C, Park K. Cerebrospinal fluid rhinorrhea caused by a congenital defect of stapes mimicking otorrhea. Clin Nucl Med. 2000;25(8):634–635. doi: 10.1097/00003072-200008000-00019. [DOI] [PubMed] [Google Scholar]
- 14.McMains K, Gross C, Kountakis S. Endoscopic management of cerebrospinal fluid Rhinorrhea. Laryngoscope. 2004;114(10):1833–1837. doi: 10.1097/00005537-200410000-00029. [DOI] [PubMed] [Google Scholar]
- 15.Grover M, Singhal P, Singh S, Sharma M, Jain A. Transnasal endoscopic cerebrospinal fluid Rhinorrhea repair: our experience of 35 cases. An Int J Clin Rhinol. 2014;7(2):47–51. doi: 10.5005/jp-journals-10013-1193. [DOI] [Google Scholar]
- 16.Zweig J, Carrau R, Celin S, Schaitkin B, Pollice P, Snyderman C, et al. Endoscopic repair of cerebrospinal fluid leaks to the sinonasal tract: predictors of success. Otolaryngol Head Neck Surg. 2000;123(3):195–201. doi: 10.1067/mhn.2000.107452. [DOI] [PubMed] [Google Scholar]
- 17.Mirza S, Thaper A, McClelland L, Jones N. Sinonasal Cerebrospinal Fluid Leaks: Management of 97 Patients Over 10 Years. Laryngoscope. 2005;115(10):1774–1777. doi: 10.1097/01.mlg.0000175679.68452.75. [DOI] [PubMed] [Google Scholar]
- 18.Cassano M. Endoscopic treatment of cerebrospinal fluid leaks with the use of lower turbinate grafts: a retrospective review of 125 cases. Rhinol J. 2009;47(4):362–368. doi: 10.4193/Rhin08.175. [DOI] [PubMed] [Google Scholar]
- 19.Sanderson J, Kountakis S, McMains K. Endoscopic Management of Cerebrospinal Fluid Leaks. Facial Plast Surg. 2009;25(01):029–037. doi: 10.1055/s-0028-1112229. [DOI] [PubMed] [Google Scholar]
- 20.Senior B, Jafri K, Benninger M. Safety and efficacy of endoscopic repair of CSF leaks and encephaloceles: a survey of the members of the American rhinologic society. Am J Rhinol. 2001;5(1):21–25. doi: 10.2500/105065801781329356. [DOI] [PubMed] [Google Scholar]
- 21.El-Banhawy Endonasal endoscopic simultaneous surgical repair for recurrent multiple traumatic bilateral cerebrospinal fluid rhinorrhea. J Rhinolaryngo-Otolog. 2013;1(1):20–25. [Google Scholar]
- 22.Gassner H, Ponikau J, Sherris D, Kern E. CSF Rhinorrhea: 95 consecutive surgical cases with long term follow-up at the mayo clinic. Am J Rhinol. 1999;13(6):439–447. doi: 10.2500/105065899781329610. [DOI] [PubMed] [Google Scholar]
- 23.Kirtane M, Gautham K, Upadhyaya S. Endoscopic CSF Rhinorrhea closure: our experience in 267 cases. Otolaryngol Head Neck Surg. 2005;132(2):208–212. doi: 10.1016/j.otohns.2004.09.004. [DOI] [PubMed] [Google Scholar]