Abstract
To analyze the patterns of failure and factors affecting recurrence and overall survival in mucoepidermoid carcinoma of the salivary gland. The hospital records were retrospectively analyzed from October 2010 to January 2016. Patients diagnosed as mucoepidermoid carcinoma of the salivary gland were eligible for analysis. All patients received surgery as the primary treatment modality with or without post operative radiotherapy. Statistical analysis for factors affecting recurrence was done by cox regression analysis and p value less than 0.05 was considered significant. A total of 116 patients were diagnosed to have malignant salivary gland tumors of which 69 were mucoepidermoid carcinomas (69.5%). The median age was 43 years (8–75 years). Majority of the tumors occurred in major salivary glands gland (77%). 51% patients were females. Most common stage was stage II (36%) followed by stage I (27.5%), stage IV (20.3%) and stage III (16%). High grade carcinomas comprised 34.8%, intermediate grade 30.4% and low grade 34.8%. 36 patients (52.2%) received adjuvant radiotherapy (60 Gy in 30 fractions). At a median follow up of 42 months (8–70 months), 8 (11.6%) patients died (7 cancer related and 1 noncancer related). The locoregional recurrence rate was 4.3% whereas the distant metastasis rate was 11.6%. Most common site of distant metastasis was lung. The mean disease free survival time was 61.4 months and the mean overall survival was 62 months. On univariate analysis, age < 50 years, node positive, presence of PNI, high grade, presence of LVI and local recurrence were significant factors for distant metastasis (p < 0.05). On multivariate analysis, high grade, presence of LVI and local recurrence were significant factors for distant metastasis (p < 0.05). Mucoepidermoid carcinomas of salivary gland have good long term local control and overall survival. Majority of the recurrences are distant metastasis. High grade, LVI and local recurrence are significant risk factors for distant relapse.
Electronic supplementary material
The online version of this article (10.1007/s12070-019-01781-0) contains supplementary material, which is available to authorized users.
Keywords: Mucoepidermoid carcinoma, Salivary glands, Radiotherapy
Introduction
Mucoepidermoid carcinoma (MEC) is the most common malignancy of the major and minor salivary glands, comprising 34% of salivary gland malignancies [1]. It has a female preponderance, with a prevalence that is highest in the 5th decade of life [2]. Most grading systems for MEC are 3-tiered, classifying tumors into low, intermediate, and high grade. Although low-grade and high-grade cancers have an established correlation with good and poor prognosis, respectively, the prognosis for intermediate-grade MEC is not well defined [2–4]. Therefore, the treatment plan for patients with intermediate-grade MEC is not standardized.
Surgical resection is the mainstay of treatment for all grades of MEC. Local resection of the tumor is considered sufficient treatment for low-grade tumors. High-grade tumors are generally treated with surgical excision with wide margins followed by postoperative radiotherapy. Neck dissection is often used when regional metastasis is present. Intermediate-grade MEC treatment has varied from local excision to wide excision with lymphadenectomy and/or postoperative radiotherapy. The current study investigated the treatment protocols and survival outcomes of patients treated for head and neck MEC, with a focus on the comparison of outcomes for patients with low-grade, intermediate-grade and high-grade cancer.
The aim of this study was to analyze the patterns of failure and factors affecting recurrence and overall survival in mucoepidermoid carcinoma of the salivary gland.
Materials and Methods
Patient Inclusion and Exclusion Criteria
The hospital records were reviewed to analyze cases of salivary gland neoplasms treated from October 2010 to January 2016. All patients were histologically confirmed salivary gland carcinomas. Patients who were inoperable or metastatic at presentation were excluded from analysis. Staging was done as per the AJCC 7th edition. The staging evaluation for all patients included history and physical examination, computed tomography (CT scan) of head and neck, chest radiographs, ultrasonography of abdomen and pelvis, complete blood count and renal function tests. All patients were stratified into low, intermediate and high grade histology as per Armed Forces Institute of Pathology (AFIP) system.
Treatment Details
All patients included were treated by radical surgery with or without post operative radiotherapy. Post operative radiotherapy consisted of a total dose of 60 Gy in 30 fractions by conventional or Intensity Modulated Radiotherapy (IMRT) technique.
Follow Up
Patients were followed up after 2 months of completion of treatment, every 3 months for the first 2 years after diagnosis, every 6 months for the next 3 years and yearly thereafter.
Statistical Analysis
Local recurrence was defined as tumor recurrence within the External Beam Radiotherapy (EBRT) volume. Regional recurrence was defined as tumor recurrence adjacent to and outside of the EBRT volume in the same organ or structure. Distant metastasis was defined as tumor progression in a previously non involved organ or structure. Overall survival was measured from the date of diagnosis. Disease-free survival was measured from the completion of treatment, confirmed by biopsy or image exam. Statistical analysis for factors affecting recurrence and mortality was done by cox regression analysis and p value of less than 0.05 was considered significant.
Results
A total of 116 patients were diagnosed to have malignant salivary gland neoplasms of which 69 were mucoepidermoid carcinomas (69.5%). The median age was 43 years (8–75 years).
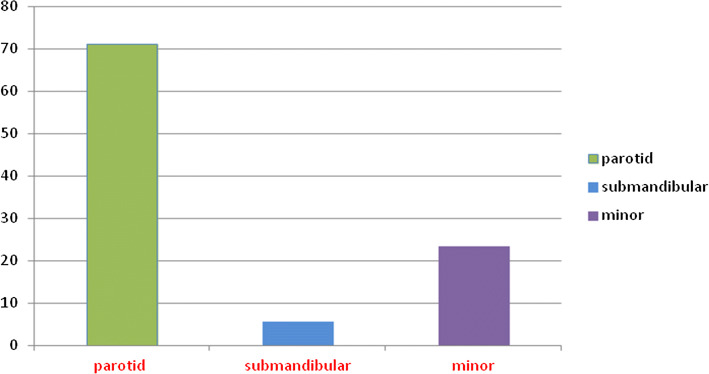
Majority of the tumors (77%) occurred in major salivary glands (Fig. 1). 51% patients were females. Most common stage at presentation was stage II (36%) followed by stage I (27.5%), stage IV (20.3%) and stage III (16%). High grade carcinomas comprised 34.8%, intermediate grade 30.4% and low grade 34.8%.
Fig. 1.
Distribution of muco epidermoid carcinomas according to site
Treatment Details
All patients underwent upfront surgery after confirmation of diagnosis. 3 patients presented with facial nerve palsy at diagnosis whereas facial nerve had to be sacrificed in 16 patients during surgery. An ipsilateral selective neck dissection was performed in patients with suspicious or clinically palpable lymph nodes (61%). All patients were stratified into low, intermediate and high grade histology as per Armed Forces Institute of Pathology (AFIP) system. 36 patients received post operative radiotherapy due to one or more risk factors to a total dose of 60 Gy in 30 fractions by conventional or IMRT technique. The details of post operative histopathology are given in Table 1.
Table 1.
Postoperative histopathology details
| T stage | |
| T1 | 20 |
| T2 | 25 |
| T3 | 12 |
| T4 | 12 |
| Nodal status | |
| Node positive | 14 |
| Node negative | 28 |
| LVI | |
| Present | 9 |
| Absent | 60 |
| PNI | |
| Present | 10 |
| Absent | 59 |
| Margins | |
| Free | 58 |
| Positive | 11 |
| Grade | |
| Low | 24 |
| Intermediate | 21 |
| High | 24 |
Treatment Outcomes
At a median follow up of 42 months (8–70 months), of the 69 patients treated, 3 developed locoregional recurrence (4.3%). Of these 3 recurrences, 2 patients also developed synchronous distant metastasis. A total of 8 patients (11.6%) developed distant metastasis, all of which were high grade MECs (Table 2). The most common site of distant metastasis was lung. All the patients who were high grade MECs and who developed distant metastasis died (7 cancer related deaths, 1 non cancer related death). The mean disease free survival time was 61.4 months and the mean overall survival was 62 months.
Table 2.
Treatment outcomes according to grade of mucoepidermoid carcinomas
| Grade | N | Port | LRR | DM | Deaths |
|---|---|---|---|---|---|
| LG | 24 | 7 | 1 | 0 | 0 |
| IG | 21 | 10 | 0 | 0 | 0 |
| HG | 24 | 18 | 2 | 8 | 8 |
LG low grade, IG intermediate grade, HG high grade
Statistical analysis was performed using cox regression. On univariate analysis, age < 50 years, node positivity, presence of Lymphovascular Invasion (LVI) and Perineural Invasion (PNI), high grade and development of local recurrence were significant risk factors for distant metastasis (p < 0.05). On multivariate analysis (Table 3), high grade, presence of LVI and development of local recurrence were significant factors for distant metastasis and decreased overall survival (p < 0.05).
Table 3.
Risk factors for developing distant metastasis among patients with mucoepidermoid carcinoma (N = 69)
| Study variable | N | Mean time to distant metastasis (months) | HR (95% CI) | p value | aHR (95% CI) | p value |
|---|---|---|---|---|---|---|
| Age category | ||||||
| < 50 years | 45 | 67.2 | 1 | 0.018 | 1 | 0.228 |
| ≥ 50 years | 24 | 50.0 | 6.9 (1.4–34.3) | 3.4 (0.5–25.7) | ||
| Gender | ||||||
| Male | 34 | 53.5 | 8.3 (1.0–67.2) | 0.048 | 2.9 (0.3–30.4) | 0.384 |
| Female | 35 | 68.1 | 1 | 1 | ||
| Node | ||||||
| Positive | 14 | 39.0 | 5.1 (1.3–20.8) | 0.022 | 5.0 (0.7–35.1) | 0.106 |
| Negative | 55 | 65.5 | 1 | 1 | ||
| Lymphovascular invasion | ||||||
| Positive | 09 | 25.0 | 17.8 (4.1–78.6) | < 0.001 | 18.9 (1.7–215.6) | 0.018 |
| Negative | 60 | 66.7 | 1 | 1 | ||
| Perineural invasion | ||||||
| Positive | 10 | 36.4 | 5.3 (1.2–22.6) | 0.024 | 1.3 (0.2–8.9) | 0.822 |
| Negative | 59 | 64.6 | 1 | 1 | ||
| Local recurrence | ||||||
| Yes | 03 | 29.0 | 6.9 (1.4–34.4) | 0.018 | 77.0 (4.2–1405.4) | 0.003 |
| No | 66 | 64.0 | 1 | 1 |
HR hazarad ratio, aHR adjusted hazard ratio
Discussion
Mucoepidermoid carcinoma is the most common malignant neoplasm observed in the major and minor salivary glands among children and adults [5] and shows a wide, nearly uniform age distribution, with diminution in paediatric and geriatric life. There is a 3:2 female predilection. Approximately half of the tumors occur in the major salivary glands, with about 45% of MECs occurring in the parotid gland [5]. In our study, the tumors were almost equally distributed between both genders and 77% of MECs occurred in the parotid gland.
Surgical resection is the mainstay of treatment for salivary gland tumors. Adjuvant radiation therapy appears to aid in local control for intermediate or high-grade MEC in case of advanced stage, close or positive surgical margins, high-grade histology, perineural invasion, or lymphovascular invasion. In the case of low-grade disease, the indications are less clear; traditionally, low-grade disease has been treated with surgical excision alone [6]. Indications for treatment of the neck, especially for patients with clinically negative lymph nodes (N0), remain unclear. The strongest predictors for occult lymph node metastasis in a clinically N0 patient have traditionally been tumor histology, pathologic grade, tumor size, and site of disease [7]. In our study, neck dissection was done in case of advanced T stage, high grade histology or clinically palpable lymph nodes.
Terhaard et al. [8] examined the role of radiation therapy in the treatment of malignant salivary gland tumors, and although surgery alone was generally recommended for MEC, postoperative radiation improved 10-year local control for patients with malignant tumors and advanced T stage (T3 and T4), close or positive surgical margins, bone invasion, or perineural invasion. In our study, majority of the patients who received post operative radiotherapy had advanced T stage, node positivity or positive margins.
Chen et al. reviewed 61 patients with localized MEC treated with surgery and postoperative radiation therapy to a median dose of 60 Gy. The 5-year estimate of overall survival for patients with non-high-grade tumors was 83% [9]. The mean disease free survival time was 61.4 months and the mean overall survival was 62 months in our study.
A retrospective review of 125 patients by Mc Hugh et al. concluded that patients with either low or intermediate grade tumors uniformly have favourable local control and survival. High histological grade, advanced stage, perineural invasion, positive surgical margins, and submandibular location all portend for poor outcomes in MEC [10]. Our patients with low or intermediate grade MECs also had excellent 5 year local control (98%) and overall survival (100%). High grade, presence of LVI and development of local recurrence were significant factors for distant metastasis and decreased overall survival in our study.
The only study analyzing long term outcomes of mucoepidermoid carcinomas from India was reported by Ghosh Laskar et al. [11]. They concluded that histologic grade was the most important factor affecting outcome in parotid MEC. Adjuvant radiotherapy was recommended for high-grade tumors and should be tailored according to the expected risk of recurrence for low-grade and intermediate-grade tumors. However, this study analyzed only parotid MECs.
Conclusion
We believe that our study on mucoepidermoid carcinomas of major and minor salivary glands is the first of its kind from India. In our study, mucoepidermoid carcinomas had good long term local control and overall survival. Majority of the recurrences were distant metastasis. High grade, LVI and local recurrence were significant risk factors for distant relapse. Future research on tailored treatment and therapies aimed at reducing distant relapses is essential for proper management of these rare neoplasms.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Funding
We did not receive any funding for this study.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rohith Singareddy, Email: rohithsingareddy@gmail.com.
Harjot Kaur Bajwa, Email: harjotbajwa1987@gmail.com.
References
- 1.Spiro RH. Salivary neoplasms: overview of a 35-year experience with 2807 patients. Head Neck Surg. 1986;8:177–184. doi: 10.1002/hed.2890080309. [DOI] [PubMed] [Google Scholar]
- 2.Thompson LD. Mucoepidermoid carcinoma. Ear Nose Throat J. 2005;84:762–763. doi: 10.1177/014556130508401207. [DOI] [PubMed] [Google Scholar]
- 3.Emerick KS, Fabian RL, Deschler DG. Clinical presentation, management, and outcome of high-grade mucoepidermoid carcinoma of the parotid gland. Otolaryngol Head Neck Surg. 2007;136:783–787. doi: 10.1016/j.otohns.2006.11.045. [DOI] [PubMed] [Google Scholar]
- 4.Kokemueller H, Brueggemann N, Swennen G, Eckardt A. Mucoepidermoid carcinoma of the salivary glands—clinical review of 42 cases. Oral Oncol. 2005;41:3–10. doi: 10.1016/j.oraloncology.2004.01.017. [DOI] [PubMed] [Google Scholar]
- 5.Goode RK, El Naggar AK. Mucoepidermoid carcinoma. WHO organization classification of tumours. Pathology and genetics of head and neck tumours. Lyon: IARC Press; 2005. pp. 219–220. [Google Scholar]
- 6.Byrd SA, Spector ME, Carey TE, Bradford CR, McHugh JB. Predictors of recurrence and survival for head and neck mucoepidermoid carcinoma. Otolaryngol Head Neck Surg. 2013;149(3):402–408. doi: 10.1177/0194599813489659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen AM, Garcia J, Lee NY, Bucci MK, Eisele DW. Patterns of nodal relapse after surgery and postoperative radiation therapy for carcinomas of the major and minor salivary glands: What is the role of elective neck irradiation? Int J Radiat Oncol Biol Phys. 2007;67(4):988–994. doi: 10.1016/j.ijrobp.2006.10.044. [DOI] [PubMed] [Google Scholar]
- 8.Terhaard CH, Lubsen H, Rasch CR, et al. The role of radiotherapy in the treatment of malignant salivary gland tumors. Int J Radiat Oncol Biol Phys. 2005;61(1):103–111. doi: 10.1016/j.ijrobp.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 9.Chen AM, Lau VH, Farwell DG, Luu Q, Donald PJ. Mucoepidermoid carcinoma of the parotid gland treated by surgery and postoperative radiation therapy: clinicopathologic correlates of outcome. Laryngoscope. 2013;123(12):3049–3055. doi: 10.1002/lary.24238. [DOI] [PubMed] [Google Scholar]
- 10.McHugh CH, Roberts DB, El-Naggar AK, et al. Prognostic factors in mucoepidermoid carcinoma of the salivary glands. Cancer. 2012;118:3928–3936. doi: 10.1002/cncr.26697. [DOI] [PubMed] [Google Scholar]
- 11.Ghosh-Laskar S, et al. Mucoepidermoid carcinoma of the parotid gland: factors affecting outcome. Head Neck. 2011;33:497–503. doi: 10.1002/hed.21477. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.