Abstract
Mucoceles are benign, encapsulated, expansible, locally invasive masses within a paranasal sinus filled with mucus and lined by epithelium. Sphenoid sinus mucoceles are relatively rare, accounting for only 1% of all paranasal sinus mucoceles. Usually presenting with headache but can rarely result in visual defect, diplopia and at times, ptosis. We present two cases of sphenoid sinus mucocele where patient presented with ophthalmoplegia, ptosis and/or sudden onset vision loss. With the help of imaging studies like CT scan and MRI of paranasal sinus diagnosis was made and immediate surgical intervention was planned which resulted in acceptable improvement of symptoms and vision.
Keywords: Sphenoid mucocele, Sphenoidotomy, Ophthalmoplegia, Diplopia
Introduction
Mucoceles are benign, encapsulated, expansible, locally invasive masses within a paranasal sinus filled with mucus and lined by epithelium. Mucoceles occur in all of the paranasal sinuses but arise most commonly in the frontal sinus. Isolated sphenoid sinus mucocele is rare in paranasal sinus mucoceles. The mechanism in the development of mucocele is not clear, but postulated as the obstruction of the sinus initiates its development. There are other theories about its aetiology, including cystic degeneration of epithelial mucus glands, or cystic degeneration of an inflammatory polyp [1, 2]. Sphenoid sinus mucoceles are relatively rare, accounting for only 1% of all paranasal sinus mucoceles [3, 4]. Usually presenting with headache but can rarely result in visual defect, diplopia and ptosis [5, 6]. In this article, we present two cases of first-episode sphenoid sinusitis with persistent facial numbness, visual and ocular symptoms and point out the importance of early diagnostic imaging and immediate surgical intervention to achieve acceptable improvement of symptoms.
Case 1
43-year female patient presented with complaints of persistent left side unilateral headache for 1 year, numbness over left side of face since 3 months, progressive diminution of vision in left eye since 7 days these complaints were associated with left retro orbital pain and nasal blockage occasionally. There was no complaint of hyposmia, post nasal drainage or any other co-morbid illness like diabetes mellitus or hypertension etc.
On nasal endoscopy nasal mucosa was mildly congested and small amount of mucoid discharge was present in both nasal cavities. Extraocular muscle movement was normal in all direction and vision was 6/9 in right eye while in left eye she was able to perform figure counting from 1 feet. Fundus was normal. An urgent computerised tomography (CT) scan was performed which revealed gross inflammatory mucosal thickening in the left sphenoid sinus, along with irregularity and sclerosis in the bony wall favourable towards fungal sinusitis or mucocele and slight mucosal thickening in the left ethmoid sinus (Fig. 1).
Fig. 1.
a Saggital section, b axial section of CT scan of para nasal sinuses showing inflammatory mucosal thickening in the left sphenoid sinus, with irregularity and sclerosis in the bony wall
After urgent pre anaesthetic work-up considering deuteriation in vison patient was planned for trans-nasal endoscopic exploration under general anaesthesia on following day. Trans-nasal endoscopic sphenoidotomy was performed and sphenoid sinus was cleared of disease, and nasal packing was done, removed tissue was sent for histopathologic examination. On 2nd post-operative day nasal pack was removed which was uneventful. Next day following pack removal vison was tested which was 6/9 in right eye while in left eye it was 6/12 which was a significant improvement. Left sided facial numbness was also improved significantly. Although histopathology examination reported the presence of fungal ball.
On 6 month follow-up nasal endoscopy was performed, there was no recurrence although life time follow-up was advised.
Case 2
A 45-year old female visited in outpatient department with complaints of progressive diminution of vison in right eye, drooping of right eyelid and diplopia for 5 days. She also complained of persistent fronto-temporal headache since 1 month and she was a known case of Diabetes mellitus and hypertension, on medication for 5 years. On examination it was found that there is binocular diplopia, right side ptosis (Fig. 2a) and isolated right-sided oculomotor nerve palsy while ipsilateral pupil was spared. There was moderate reduction of elevation, depression, and adduction in the right eye with 6/48 vision while in left eye extraocular muscle examination was normal with vision of 6/12. Bilaterally fundus was normal. Urgent computerised tomography scan of head, paranasal sinuses and orbit was performed which revealed Opacification of sphenoid sinus with bony expansion/erosion likely suggesting mucocele. Subsequently Magnetic resonance imaging was performed. The lesion was hyperintense on both T1- and T2-weighted images completely filling and expanding the sphenoid sinus with mild elevation of sella turcica. Pituitary gland and optic chiasma grossly normal. Findings of Imaging studies were consistent with cystic lesion predominantly an isolated mucocele in sphenoid sinus (Fig. 3).
Fig. 2.
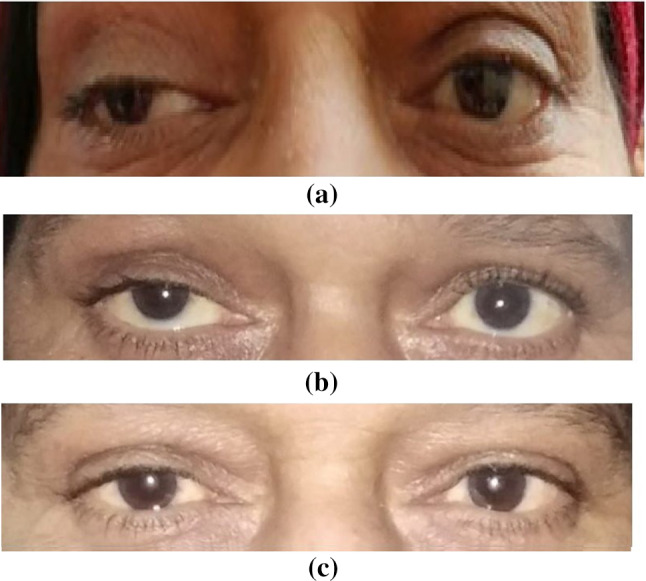
a Pre-operative image showing right ptosis. b Post-operative day 2. c 2 week follow-up images showing significant improvement
Fig. 3.
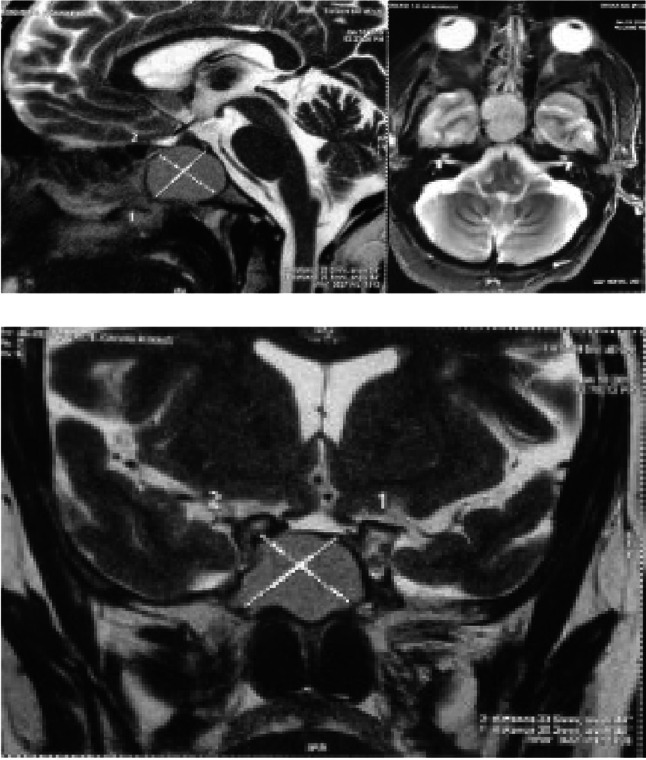
Non-enhancing T2-hyperintensity lesion completely filling and expanding the sphenoid sinus with mild elevation of sella turcica
After pre-anaesthetic workup urgent trans-nasal endoscopic decompression was planned and mucocele was decompressed by sphenoidotomy and marsupialisation, mucus like fluid was drained (Fig. 4).
Fig. 4.

Endoscopic view after Marsupialization of sphenoid sinus mucocele
Microscopic study of the mucocele showed a columnar epithelium lined cyst, with acute and chronic inflammation. No growth was observed on bacterial cultures of retained secretions. Occular symptoms like diplopia and ptosis were improved significantly on following day (Fig. 2b).
On 12 month follow-up there was no recurrence, there was no visual or neurological symptom.
Discussion
Mucoceles are cyst-like lesions lined with respiratory epithelium they commonly lead to thinning, erosion and furthermore, destruction of the bony walls of sinus [7]. More than half of them are found to be involving frontal sinuses. Isolated sphenoid sinus mucoceles are quite rare, constituting nearly 1–2% of all cases of paranasal sinus mucoceles. They usually start unilaterally, but in most of the cases at the time of presentation, the entire sphenoid sinus complex may be opacified and expanded with thinning of its bony walls [3, 4]. The most common symptom is headache, which is most often described as frontal or retroorbital in nature and is found in around 70% of patients [8]. In both the cases described above patients had headache It has been suggested that headache results from stretching of the dura over the planum sphenoidale [8]. The second most common symptom is visual disturbance, which is found in 65% of patients [9]. In both our cases patients suffered significant vison loss and had features of third cranial nerve palsy in the form of visual disturbances, diplopia or ptosis which is a rare presentation.
The diagnosis of sphenoid sinus mucocele is mainly radiological. The bony changes are best picked up by CT-scans [10]. In cases of sphenoid sinus mucocele, CT scan of the paranasal sinuses will reveal an expansile, homogeneous lesion with no contrast enhancement [11]. Mucoceles can be hypo, iso-, or hyperintense or signal void on both T1- and T2-weighted images based on their biochemical constituents. On various occasions they may show peripheral enhancement with contrast material [12]. Due to peripheral location of the pupillary fibres in the oculomotor nerve, compressive lesions such as aneurysms or tumours that produce third nerve palsy usually produce ocular motility disturbance and iridoplegia. Although isolated oculomotor nerve palsy with papillary sparing is characteristic of diabetic ophthalmoplegia. Pupillary sparing is believed to result from microvascular ischemia of the central portion of the nerve with sparing of the more peripherally placed parasympathetic fibers [13]. The most recommended treatment of sphenoid sinus mucocele is surgical, historically complete removal via transfacial or transcranial approach was used but these days trans nasal endoscopic drainage and marsupialization of the mucocele is considered treatment of choice, usually resulting in rapid regression of the ophthalmic manifestations [10], as occurred in both our cases, the patient’s symptoms gradually diminished. Sparing of pupil function mimics a vasculopathic process in 46.6% of cases [14], as in our patients they underwent endoscopic marsupialization of the mucocele which demonstrated dramatic improvement in vision and symptoms of third cranial nerve palsy. 1 month after surgery, the third cranial nerve palsy had completely resolved. Proper and timely intervention usually results in rapid regression of the ophthalmic manifestation, but in most cases, vision seldom returns to normal [14]. The visual dysfunction may be due to optic nerve compression with vascular compromise or extension of the sinus infection and inflammation to the optic nerve. A delay in surgery may result in poor prognosis. Early diagnosis by imaging and immediate surgical intervention is mandatory for best results.
Conclusion
For cases of pupil sparing 3rd cranial nerve palsy with visual disturbances isolated sphenoid sinus lesions should be considered as an important differential diagnosis. Early diagnosis by CT scan and MRI imaging studies and immediate surgical intervention by endoscope assisted transnasal sphenoidotomy and disease clearance can save vision and regress ophthalmic symptoms.
Compliance with Ethical Standards
Ethical Approval
Ethical approval taken from institutional ethical committee.
Informed Consent
Consent taken from all individual participants.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ankit Mishra, Email: mishra.ankitt@gmail.com.
Vishal R. Munjal, Email: vishalmunjal@gmail.com
References
- 1.Friedman A, Batra PS, Fakhri S, Citardi MJ, Lanza DC. Isolated sphenoid sinus disease: etiology and management. Otolaryngol Head Neck Surg. 2005;133:544–550. doi: 10.1016/j.otohns.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 2.Kösling S, Hintner M, Brandt S, Schulz T, Bloching M. Mucoceles of the sphenoid sinus. Eur J Radiol. 2004;51:1–5. doi: 10.1016/j.ejrad.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Prepageran N, Subramaniam KN, Krishnan GG. Ocular presentation of sphenoid mucocele. Orbit. 2004;23:45–47. doi: 10.1076/orbi.23.1.45.28986. [DOI] [PubMed] [Google Scholar]
- 4.Sethi DS, Lau DP, Chan C. Sphenoid sinus mucocoele presenting with isolated oculomotor nerve palsy. J Laryngol Otol. 1997;111:471–473. doi: 10.1017/S0022215100137673. [DOI] [PubMed] [Google Scholar]
- 5.Lund VJ, Milroy CM. Fronto-ethmoidal mucocoeles: a histopathological analysis. J Laryngol Otol. 1991;105:921–923. doi: 10.1017/S0022215100117827. [DOI] [PubMed] [Google Scholar]
- 6.Soon S, Lim C, Singh H, Sethi D. Sphenoid sinus mucocele: 10 cases and literature review. J Laryngol Otol. 2010;124:44–47. doi: 10.1017/S0022215109991551. [DOI] [PubMed] [Google Scholar]
- 7.Akan H, Cihan B, Celenk C. Sphenoid sinus mu-cocele causing third nerve paralysis: CT and MR findings. Dentomaxillofac Radiol. 2004;33:342–344. doi: 10.1259/dmfr/92903178. [DOI] [PubMed] [Google Scholar]
- 8.Nugent GR, Sprinkle P, Bloor BM. Sphenoid sinus mucoceles. J Neurosurg. 1970;32:443–451. doi: 10.3171/jns.1970.32.4.0443. [DOI] [PubMed] [Google Scholar]
- 9.Kron TK, Johnson CM., 3rd Diagnosis and management of the opacified sphenoid sinus. Laryngoscope. 1983;93:1319–1327. doi: 10.1002/lary.1983.93.10.1319. [DOI] [PubMed] [Google Scholar]
- 10.Yong WW, Zhou SH, Bao YY. Sphenoid sinus mucocele presenting with oculomotor nerve palsy and affecting the functions of trigeminal nerve: a case report. Int J Clin Exp Med. 2015;8(9):16854–16857. [PMC free article] [PubMed] [Google Scholar]
- 11.Di Girolamo S, Cannizzaro P, Picciotti P, Nardi C. Ophthalmoplegia and ptosis as onset symptoms of an isolated primary mucocele of the sphenoid sinus. J Oral Maxillofac Surg. 2002;60:1500–1502. doi: 10.1053/joms.2002.36142. [DOI] [PubMed] [Google Scholar]
- 12.Lim CC, Dillon WP, McDermott MW. Mucocele involving the anterior clinoid process: MR and CT findings. AJNR Am J Neuroradiol. 1999;20:287–290. [PMC free article] [PubMed] [Google Scholar]
- 13.Lee JC, Park SK, Jang DK, YM Han. Isolated sphenoid sinus mucocele presenting as third nerve palsy. J Korean Neurosurg Soc. 2010;48(4):360–362. doi: 10.3340/jkns.2010.48.4.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson LN, Hepler RS, Yee RD, et al. Sphenoid sinus mucocele (anterior clinoid variant) mimicking diabetic ophthalmoplegia and retrobulbar neuritis. Am J Ophthalmol. 1986;102:111–115. doi: 10.1016/0002-9394(86)90219-9. [DOI] [PubMed] [Google Scholar]



