Abstract
Chronic rhinosinusitis is one of the most commonly diagnosed medical conditions affecting all age groups. Hypertonic saline solution and isotonic saline solution are used in management of chronic rhinosinusitis. In this study we compare the effectiveness of isotonic saline and hypertonic saline in alleviation of symptoms and clinical outcome of patients with chronic rhinosinusitis. In our study 60 patients diagnosed with chronic rhinosinusitis are divided into two groups; Group A treated with isotonic saline and Group B with 3.5% hypertonic saline for a period of 6 weeks. The symptoms were evaluated using SNOT-20 score before and after treatment. It was found that hypertonic saline solution is more efficacious than isotonic saline solution in the treatment of patients with chronic rhinosinusitis.
Keywords: Chronic rhinosinusitis, Nasal douching, SNOT-20 score, Hypertonic saline solution, Isotonic saline solution
Introduction
Chronic rhinosinusitis (CRS) is defined as an inflammatory condition of the nasal cavity and paranasal sinuses lasting for longer than 12 weeks. The pathophysiology of CRS remains incompletely understood, interactions between host anatomy, genetics, and the environment may be contributory factors. CRS can be thought of first resulting from mucosal inflammation, causing swelling and obstruction at the sinus ostium. This can lead to mucus stasis, which can then lead to bacterial superinfection. The signs and symptoms of CRS often vary in severity and prevalence. Nasal obstruction, is the most common symptom, followed by facial congestion-pressure-fullness, discoloured nasal discharge, post nasal drip and hyposmia. There is evidence of numerous factors contributing to CRS including: Biofilms, Osteitis, Allergy, Superantigens from Staphylococcus aureus, Fungi,etc. Medical management of CRS are antimicrobial medications, anti-inflammatory, and mechanical. Steroid Nasal Sprays and Oral Steroids, Nasal irrigaton, Decongestants, and Leukotriene Antagonists, Allergy Management and other therapies are widely employed in the field before surgical management. . Long term use of these drugs has detrimental effect both locally and systemically. Hypertonic saline nasal irrigation was formally identified as an adjunctive care for sinusitis in the 1990’s [1–4] though it was advocated since Vedic times. Nasal saline irrigation is an important component in the treatment of CRS. Frequent rinsing prevents the accumulation of nasal crusts and promotes mucociliary clearance. This reduces nasal symptoms and increase quality of life.
The aim of this study was to assess and compare the the effect of hypertonic saline nasal douching against normal saline nasal douching in patients with chronic rhinosinusitis. The objective of the study is to assess the change in the symptoms which were evaluated before and after treatment with SNOT-20 score over a period of 6 weeks.
Materials and Methods
This is a prospective randomized control study “Nasal Douching with Hypertonic saline versus Isotonic Saline in the management of Chronic Rhinosinusitis—A comparative study” was conducted in the Department of Otorhinolaryngology and Head and neck surgery at Meenakshi Medical College and Research Institute, Kanchipuram . During this period, sixty patients who were diagnosed as chronic rhinosinusitis in the age group of 15–50 years were selected.
Study design
This is a prospective randomized control study.
Inclusion criteria
Patients with Chronic Rhino Sinusitis (CRS)
Patients with Sinonasal Diseases Willing for Study
Exclusion criteria
Sino Nasal Malignancies
Acute Rhinosinusitis
Coexisting septic foci
Bleeding disorders
Geriatric and pediatric patients
Method of collection of data
Sample size: 60
Group A: 30 (Isotonic Saline)
Group B: 30 (Hypertonic Saline)
Subjective symptoms and findings were based on the CRS criteria and were divided into major and minor factors. A CRS diagnosis requires presence of at least 2 major factors or one major factor with 2 or more minor factors (Table 1) or nasal purulence on examination with duration of minimum 12 weeks.
Table 1.
Comparison between pre and post treatment outcome within group A
| Symptom | Mean | SD | t value | p |
|---|---|---|---|---|
| Nasal obstruction | ||||
| 1st week | 3.30 | 1.56 | 6.73 | < 0.001 |
| 6th week | 1.70 | 1.06 | ||
| Thick nasal discharge | ||||
| 1st week | 3.73 | 1.34 | 9.54 | < 0.001 |
| 6th week | 1.87 | 0.89 | ||
| Post nasal drip | ||||
| 1st week | 3.70 | 1.39 | 9.40 | < 0.001 |
| 6th week | 1.53 | 0.86 | ||
| Ear pain | ||||
| 1st week | 1.27 | 1.08 | 4.57 | < 0.001 |
| 6th week | 0.70 | 0.84 | ||
| Facial pain | ||||
| 1st week | 3.07 | 1.53 | 8.81 | < 0.001 |
| 6th week | 1.13 | 0.90 | ||
| Total | ||||
| 1st week | 15.07 | 3.11 | 20.42 | < 0.001 |
| 6th week | 6.83 | 2.12 | ||
The selected patients were randomized into two groups. Group A included 30 cases treated with normal saline (Solution A) nasal douching with 100 ml three times a day in both nostrils for a period of 6 weeks and the remaining 30 cases in Group B treated with 3.5% hypertonic saline (Solution B) 100 ml three times a day in both nostrils for the same period.
Detailed history was taken and clinical examination carried out in selected cases. The selected patients were explained about the mode of treatment and were asked to report every 3rd week for a period of two months to assess about the symptoms. Normal saline which is commercially available as 0.9% Sodium chloride solution was used for Group A. Hypertonic solution of 3.5% Sodium chloride was prepared by dissolving 3.5 gm. of sodium chloride in 100 ml of double distilled water and was used for Group B. The solution was dispensed in 100 ml sterile squeeze bottles.
In this study a concentration of 3.5% saline solution was chosen as it’s about sea water concentration, considered harmless and better tolerated by patients. To avoid aerosol deposition in lower airways and since nasal drops solution is easy to dispense, cost effective, simple to prepare freshly when required and not requiring any special device to deliver the solution.
Patients were randomly selected and either solution A or solution B was given as nasal douching and were advised to instill 100 ml intranasally three times a day. The douching was done fast upward in a sitting or standing position with the head bent forwards to allow secretions to flow downwards and out from the opposite nostril without the patient breathing them in. They were immediately removed from the nose in order to minimize the salty taste or burning feeling of the saline solutions.
The symptoms of the patients were evaluated on SNOT 20 for nasal congestion, facial pain, sense of smell, nasal discharge and overall symptomatic assessment. This was done once in the first week and at the end of the treatment. The Sino-Nasal Outcome Test 20 (SNOT-20) is one of the most widely used quality-of-life instruments for sinonasal conditions and is intended for populations of people with rhinosinusitis, rather than simply rhinitis. The SNOT-20 is a self-administered multiple-choice 20-item test that is usually scored with a single summary score (0–5) without domains or subscales. This instrument assesses a broad range of health and health-related quality-of-life problem including physical problems, functional limitations, and emotional consequences, but unlike many of the quality-of-life instruments designed to measure rhinitis symptoms, this rhinosinusitis measure is not divided into subscales or domains related to these different areas. All parameters are assessed and five main parameters affecting the patients in the present op setup were also identified and assessed.
Patient performing nasal douching 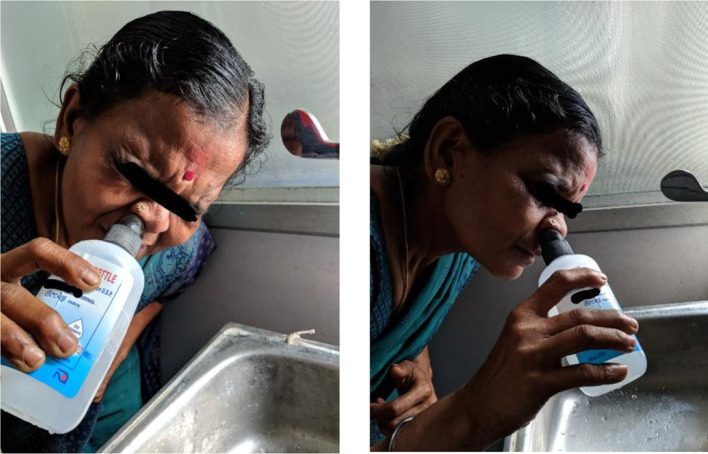
Statistical analysis was done using SPSS v25 software (IBM). Paired T Test will be used for comparison of mean values before and after treatment starts within groups(first week and sixth week). T test will be used to analyze values between groups and a ‘p’ value of < .05 will be considered significant.
Observation and Results
The present study was conducted in patients with chronic rhinosinusitis attending Department of Otorhinolaryngology and Head and neck surgery at Meenakshi Medical College and Research Institute, Kanchipuram during the period of January 2017 to September 2018.
The following observations were made in sixty patients who completed the treatment schedule in the study.
The gender distribution of the study sample. There were 23 males and 37 females out of a total of 60 patients. It shows a female preponderance of 62% in this study as a whole with males constituting the remainder 32% (Fig. 1).
Fig. 1.
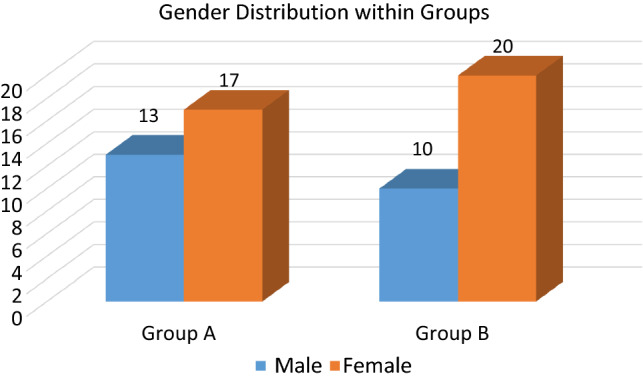
Gender distribution within Group A & Group B
The following graph shows the gender distribution within the two groups of the study sample. A total of 60 patients were divided randomly into two groups, A & B based on the treatment modality. There were 13 males (43%) and 17 females (57%) in Group A (Isotonic saline); 10 males (33%) and 20 females (67%) in Group B (Hypertonic saline).
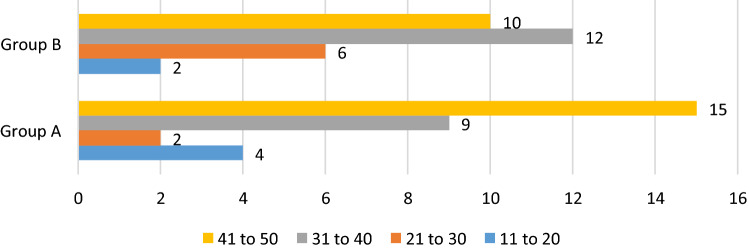
The comparison of mean age group between the two groups of the study sample. The mean age group of the study sample as a whole was 37 years. The mean age in Group A was 37.1 years and that in Group B was 36.9 years (Fig. 2).
Fig. 2.
Graph showing age distribution in Group A & Group B
The following graph shows the proportion of cases in each age group in Group A and Group B. In Group A, there were 4 patients (13%) aged 11–20 years, 2 (7%) aged 21–30 years, 9 (30%) aged 31–40 years & 15 (50%) aged 41–50 years. In Group B there were 2 patients (7%) aged 11–20 years, 6 (21%) aged 21–30 years, 12 (40%) aged 31–40 years & 10 (33%) aged 41–50 years. It was observed that the number of patients in the age group of 41–50 were 50% which happened to be the highest in Group A compared to 33% in Group B. It was observed that the number of patients in the age group of 31–40 were 40% which happened to be the highest in group B compared to 30% in group A.
The table shows the comparison of the different symptoms in relation to pre treatment (1st week) and post treatment (6th week) along with comparison of the total outcome within Group A treated with isotonic saline. Each symptom had statistically significant improvement at the end of six weeks of treatment with isotonic saline. It can be observed that in Group A, at the beginning of first week the mean for total outcome was 15.07 ± (3.11) and after six weeks it was 6.83 ± (2.12), which was found to be statistically significant (p < 0.001). Thus it can be inferred that isotonic saline significantly improved symptoms in Group A.
The table shows the comparison of the different symptoms in relation to pre treatment (1st week) and post treatment (6th week) along with comparison of the total outcome within Group A treated with isotonic saline. Each symptom had statistically significant improvement at the end of six weeks of treatment with hypertonic saline. It can be observed that in Group B, at the beginning of first week the mean for total outcome was 14.8 ± (3.58) and after six weeks it was 3.87 ± (1.36), which was found to be statistically significant (p < 0.001). Thus it can be inferred that hypertonic saline significantly improved symptoms in Group B (Table 2).
Table 2.
Comparison between pre and post treatment outcome within group B
| Symptom | Mean | SD | t value | p |
|---|---|---|---|---|
| Nasal obstruction | ||||
| 1st week | 2.90 | 1.65 | 8.55 | < 0.001 |
| 6th week | 0.67 | 0.71 | ||
| Thick nasal discharge | ||||
| 1st week | 3.23 | 1.67 | 8.34 | < 0.001 |
| 6th week | 0.70 | 0.70 | ||
| Post nasal drip | ||||
| 1st week | 3.73 | 1.20 | 11.24 | < 0.001 |
| 6th week | 0.73 | 0.74 | ||
| Ear pain | ||||
| 1st week | 1.03 | 0.96 | 3.84 | < 0.001 |
| 6th week | 0.43 | 0.57 | ||
| Facial pain | ||||
| 1st week | 3.90 | 1.06 | 17.20 | < 0.001 |
| 6th week | 1.33 | 0.99 | ||
| Total | ||||
| 1st week | 14.8 | 3.58 | 15.59 | < 0.001 |
| 6th week | 3.87 | 1.36 | ||
The comparison of nasal obstruction in relation to both the groups post treatment. Patients showed relief in both test groups. However it can be observed that in Group A the mean was 1.70 ± (1.06) and Group B it was 0.67 ± (0.71), which was found to be statistically significant (p < 0.001). This implies that the improvement in Group B was better when compared to Group A.
The comparison of thick nasal discharge in relation to both the groups post treatment. Patients showed significant relief in both test groups. However it can be observed that in Group A the mean was 1.77 ± (0.89) and Group B it was 0.70 ± (0.70), which was found to be statistically significant (p < 0.001). This implies that the improvement in Group B was significantly better when compared to Group A.
The comparison of post nasal drip in relation to both the groups post treatment. Patients showed significant relief in both test groups. However it can be observed that in Group A the mean was 1.53 ± (0.86) and Group B it was 0.73 ± (0.74), which was found to be statistically significant (p < 0.001). This implies that the improvement in Group B was significantly better when compared to Group A.
The comparison of ear pain in relation to both the groups post treatment. Patients showed significant relief in both test groups. However it can be observed that in Group A the mean was 0.70 ± (0.84) and Group B it was 0.43 ± (0.57), which was found to be statistically insignificant (p > 0.001). This implies the improvement was statistically insignificant when compared between the groups.
The comparison of facial pain in relation to both the groups post treatment. Patients showed significant relief in both test groups. However it can be observed that in Group A the mean was 1.13 ± (0.9) and Group B 1.33 ± (0.9), it was which was found to be statistically insignificant (p > 0.001). This implies the improvement was statistically insignificant when compared between the groups.
The comparison of outcomes in relation to pre and post treatment with isotonic saline in Group A. It can be observed that in the first week before treatment the mean was 15.07 ± (3.1) and by six weeks it was 6.8 ± (2.1), which was found to be statistically significant (p < 0.001). This implies that there was significant improvement in Group A post treatment with isotonic saline.
The comparison of outcomes in relation to pre and post treatment with hypertonic saline in Group B. It can be observed that in the first week before treatment the mean was 14.8 ± (3.6) and by six weeks it was 3.9 ± (1.4), which was found to be statistically significant (p < 0.001). This implies that there was significant improvement in Group B post treatment with hypertonic saline.
The above table shows the comparison of the total outcome score post treatment in relation to Group A and Group B. It can be observed that in Group A post treatment the mean was 6.83 ± (2.12) and in Group B it was 3.87 ± (1.36), which was found to be statistically significant (p < 0.001). This implies that there was significant improvement in Group B treated with Hypertonic Saline compared to Group A treated with Isotonic Saline (Table 3).
Table 3.
Comparison of total outcome post treament in relation to Group A & Group B
| Group | Number of patients | Mean ± SD | t value, p |
|---|---|---|---|
| A | 30 | 6.83 ± (2.12) | t = 6.46, p < 0.001 |
| B | 30 | 3.87 ± (1.36) |
Discussion
In our study sixty patients completed the treatment, out of which 10% were in the age group of 11–20 years, 13% in 21 to 30 years, 35% in 31 to 40 years and 42% in 41–50 years.
David Shoseyov4 reported improvement but no significant difference between the groups treated with 3.5% hypertonic and 0.9% normal saline nasal drops. In hypertonic saline group.
(3.5%) nasal secretion/post nasal discharge pre-treatment mean was 2.86 ± 0.35 and a post treatment mean was 1.60 ± 0.74. Nasal secretion/ post nasal discharge score in normal saline group before treatment was 2.66 ± 0.49 and after treatment was 1.53 ± 0.83.
Furthermore, in the present study we were able to observe clinical improvement with respect to sneezing in both the groups of patients. In Group A, the mean difference between first week of treatment and sixth week of treatment was 1.7 ± (1.05) while in Group B it was 0.67 ± (0.71) (p < 0.001). Hence, we can state that in Group B the improvement was more significant when compared to Group A. Both groups experienced an improvement in ear pain symptom. However neither of the groups were better when compared to each other as seen by the statistical analysis. In Group A the mean difference between first and sixth weeks of treatment were 0.07 ± (0.84) and in Group B was 0.43 ± (0.57) (p > 0.001).
In Hatha Yoga, Jala-neti is described as a nasal cleansing technique for Sinonasal diseases [5].
Our study shows hypertonic saline nasal solutions to reduce symptoms of chronic rhinosinusitis and its efficacy over normal saline nasal solution. In various studies different concentration of hypertonic saline solutions were used. We used 3.5% saline solution because it is about the concentration of sea water and was considered harmless and better tolerated by the patients, even children4. It has been hypothesized that it improves mucociliary function [6–8], decreases mucosal oedema and inflammatory mediators and mechanically clears inspissated mucus [9, 10]. In addition, hypertonic saline is said to have a mild vasoconstrictive effect [14] and antibacterial property [13]. Study of the pulmonary epithelial barrier showed that after instillation of hyperosmolar seawater, there is a rapid influx of water from the plasma into the bronchoaleveolar space. The osmotic equilibrium was reached within 3 min and there was no injury to the epithelial or endothelial barriers of the lung [15]. The Intrinsic ciliary beat frequency and ultrastructure are not inherently impaired in chronic rhinosinusitis, because impaired ciliary function caused by chronic rhinosinusitis reverses to normal after removal and cleansing the mucosa of infected mucous and other material [10]. It appears that respiratory ciliated cells have a functional reserve that permits them to autoregulate their mechanical output response to changing respiratory mucus viscosity [11]. The dynamic viscoelastic properties of nasal mucosa determined by oscillary rheometry has revealed significant improvement in elasticity after repeated antral lavages in chronic rhinosinusitis [12] Isotonic saline solution irrigation has been found to reduce inflammatory mediators (histamine, prostaglandin D2, and leukotriene C4) and allergens in nasal secretions [16]. For these reasons, nasal washing with saline is effective against pathologies of the upper respiratory tract that occur via inflammatory mediators, namely, the common cold, acute and chronic sinusitis, and, in particular, rhinitis [16]. Hypertonic saline has been shown to increase mucociliary transit times, but is irritating for nasal membranes [17].
From the above discussion of the results and analysis, it can be inferred that hypertonic saline (3.5%) nasal irrigation has a clear role in the treatment of patients with chronic rhinosinusitis. The efficacy of hypertonic saline over normal saline nasal irrigation has been proved conclusively as evidenced from SNOT 20 scoring system symptomatically in the treatment of patients with chronic rhinosinusitis. In our study side effects were minimal and well tolerated by the patients. Treatment of patients with hypertonic saline is a simple solution to a common and expensive clinical problem and improves the quality of life.
Conclusion
The study showed that 3.5% hypertonic saline nasal solution is more efficacious than 0.9% normal saline solution in the treatment of patients with chronic rhinosinusitis and that the treatment of patients with chronic rhinosinusitis with 3.5% hypertonic saline nasal solution improves quality of life.
Compliance with ethical standards
Conflict of interest
There is no conflict of interest and no funding was provided.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wingrave W. The nature of discharges and douches. The Lancet. 1902;17:1373–1375. [Google Scholar]
- 2.Grossan M. Irrigation of the child’s nose. Clin Pediat. 1974;13(3):229–231. doi: 10.1177/000992287401300306. [DOI] [PubMed] [Google Scholar]
- 3.Robert S. Zeiger Prospects for ancillary treatment of sinusitis in the 1990s. J Allergy Clin Immunol. 1992;90:478–495. doi: 10.1016/0091-6749(92)90173-Y. [DOI] [PubMed] [Google Scholar]
- 4.Shoseyov David, Bibi Haim, Shai Pintov, Shoseyov Nurit, Shazberg Gila, Hurvitz Haggit. Treatment with hypertonic saline versus normal saline nasal wash of paediatric chronic sinusitis. J Allergy Clin lmmunol. 1998;101:602–605. doi: 10.1016/S0091-6749(98)70166-6. [DOI] [PubMed] [Google Scholar]
- 5.Instruction Manual and General formation on Yogic Saline Nasal Cleansing Technique. The Jala-neti Booklet [cited 2005 Dec 30): (41screens). http://www.yoasanas/jala.pdf
- 6.Band BC, Mukherjee AL, Bang FB. Human nasal mucous flow rates. Johns Hopkins Med J. 1967;121:38–48. [Google Scholar]
- 7.Grossan M. A device for nasal irrigation. ANL. 1976;3:65–70. [PubMed] [Google Scholar]
- 8.Majima Y, Sakakura Y, Matsubara T, Murai S, Miyoshi Y. Mucociliary clearance in chronic sinusitis: related huma nasal clearance and in vitro bullfrog palate clearance. Biorheology. 1983;20(25):1–62. doi: 10.3233/bir-1983-20215. [DOI] [PubMed] [Google Scholar]
- 9.Dulfano MJ, Adler K, Wooten O. Primary properties of sputum. IV. Effects of 100 percent humidity and water mist. Am Rev Respir Dis. 1973;107:130–132. doi: 10.1164/arrd.1973.107.1.130. [DOI] [PubMed] [Google Scholar]
- 10.Rossman CCM, Lee RMKW, Forrest JB, Newhouse MT. Nasal ciliary ultrastructure and function in patients with primary ciliary dyskinesia with that in normal subjects and in subjects with various respiratory diseases. Am Rev Respir Dis. 1984;129:161–170. doi: 10.1164/arrd.1984.129.1.161. [DOI] [PubMed] [Google Scholar]
- 11.Johnson NT, Villalon M, Royce FH, Hard R, Verdugo Autoregulation of beat frequency in respiratory ciliated cells. Demonstrated by viscous loading. Am Rev Respir Dis. 1991;144:1091–1094. doi: 10.1164/ajrccm/144.5.1091. [DOI] [PubMed] [Google Scholar]
- 12.Hirata K. Dynamic viscoelasticity of nasal mucus from children with chronic sinusitis. Mic Med J. 1985;3(34):205–219. [Google Scholar]
- 13.Mangete EDO, David W, Blankson CD. Hypertonic saline solution for wound dressing. The Lancet. 1992;28(340):1351. doi: 10.1016/0140-6736(92)92533-L. [DOI] [PubMed] [Google Scholar]
- 14.Manning SC. Pediatric sinusitis. Otolaryngol Clin North Am. 1993;26(4):623–638. doi: 10.1016/S0030-6665(20)30795-7. [DOI] [PubMed] [Google Scholar]
- 15.Folkesson Hans G, Kheradmand Farrah, Matthay Michael A. The effect of salt water on alveolar epithelial barrier function. Am J Rcspir Crit Care Med. 1994;150:1555–1563. doi: 10.1164/ajrccm.150.6.7952614. [DOI] [PubMed] [Google Scholar]
- 16.Georgitis JW. Nasal hyperthermia and simple irrigation for perennial rhinitis. Changes in inflammatory mediators. Chest. 1994;106:1487–1492. doi: 10.1378/chest.106.5.1487. [DOI] [PubMed] [Google Scholar]
- 17.Daviskas E, Anderson SD, Gonda I, Eberl S, Meikle S, Seale JP, et al. Inhalation of hypertonic saline aerosol enhances mucociliary clearance in asthmatic and healthy subjects. Eur Respir J. 1996;9(4):725–732. doi: 10.1183/09031936.96.09040725. [DOI] [PubMed] [Google Scholar]